Abstract
Purpose
The prognosis of patients with pancreatic cancer remains poor, even after potentially curative R0 resection. This discrepancy may be due to the histopathological misclassification of R1 cases as curative resections (R0) in the past.
Materials and methods
To test this hypothesis, color coding of all resection margins and organ surfaces as part of a standardized histopathological workup was implemented and prospectively tested on 100 pancreatic head specimens.
Results
Thirty-five patients were excluded from the analysis owing to the pathohistological diagnosis; only pancreatic ductal adenocarcinoma, distal bile duct adenocarcinoma, and periampullary adenocarcinoma were included. Applying the International Union Against Cancer criteria, 32 cancer resections were classified R0 (49.2%), while 33 cases turned out to be R1 resections (50.8%). The mesopancreas was infiltrated in 22 of the 33 R1 resection specimens (66.6%). It proved to be the only site of tumor infiltration in 17 specimens (51.5%). Applying the Royal College of Pathologists’ criteria, 46 resections were classified R1 (70.8%). As expected, the mesopancreas again was the most frequent site of noncurative resection (n = 27; 58.7%).
Conclusion
Using the intensified histopathological workup for pancreatic head cancer specimens resulted in an increased rate of R1 resections and the mesopancreas represents the primary site for positive resection margins. Such results are of relevance for patients’ stratification in clinical trials.
Keywords: Pancreatic cancer, Mesopancreas, Histopathological workup, R1 resection
Introduction
Due to its dismal prognosis, pancreatic cancer is the fourth most common cause of cancer death in Europe and the USA. From a clinical point of view, resection status is one of the major factors influencing patient survival. Therefore, complete surgical resection of the primary tumor represents the only curative treatment option.
However, even patients with tumor-free margins (R0 resection) experience frequently local recurrence and distant metastases, which is in clear contrast to other solid tumors of the gastrointestinal tract. Consequently, more radical approaches have been evaluated, first described by Fortner and colleagues [3]. Even though there was initial indication of some survival benefit, follow-up studies have failed to confirm these promising results [9]. This raised the question as to whether such a discrepancy is caused, other than through incomplete lymphadenectomy and perineural invasion, by a misclassification of R1 resections as R0 resections [1]. According to the recent literature, the rates of noncurative resections range from 15% to 35% [12, 15, 23, 27], whereas postmortem examinations of pancreatic cancer patients revealed local recurrence rates approaching 100% [5, 7, 19, 21, 24]. This is supported by recent publications (Verbeke et al. [22] and Esposito et al. [2]) revealing that modified histopathological workup of pancreatic head carcinomas leads to R1 resection rates of 85% and 76%, respectively.
The aim of the present article was to develop an optimized and standardized histopathological workup and to test prospectively the hypothesis that current histopathological reports underestimate the proportion of R1 pancreatic head resections. Towards this goal, we firstly implemented color coding of the resection margins (RMs) and the organ surfaces. Secondly, we carefully reevaluated the different sites of R1 resections according to the color code and demonstrated that the mesopancreatic RM was the most frequent site of incomplete tumor resection.
Materials and methods
Retrospective data analysis
In order to test the hypothesis that an optimized and standardized histopathological workup increases the rate of R1 resections after pancreatic head resections, we first compared the rates of curative resections after conventional histopathological workup in our department. Therefore, we retrospectively identified all patients who had undergone pancreatic head resection, either through pylorus-preserving pancreaticoduodenectomy (PPPD) or Kausch–Whipple procedure due to malignant diseases, in the Department of General and Visceral Surgery between 1996 and 2005. During this period, all specimens were worked up by pathologists specializing in gastrointestinal pathology. The location, histological tumor type, size of tumor, and lymph node involvement were defined. Assessment of the RM included the common bile duct, the pancreatic transection margin, the duodenal and jejunal resection plane, and the anterior and posterior surface. Additionally, vascular, lymphatic, and perineural invasion were reported if present. Cases with macroscopic tumor residues at the surgical RM or the organ surface were defined as R2. If tumor cells at the surgical RM or the organ surface were only detectable microscopically, the resection was classified R1. A curative R0 resection was defined as a surgical RM or organ surface without tumor cell infiltration.
Establishing a modified histopathological workup and prospective data analysis
A modified and standardized histopathological workup was introduced in April 2006 and prospectively tested for 28 months until July 2008. Organ surfaces and RMs of the pancreatic head resection specimen were stained according to a well-defined five-color code (Fig. 1): the anterior (ventral) surface was painted black, the posterior (dorsal) surface white, the groove of the superior mesenteric vein (SMV) green, the pancreatic transection margin yellow, and the mesopancreas red. The mesopancreas was defined as the soft tissue between the superior mesenteric artery and the pancreatic parenchyma and contains lymphatic, nervous, and vascular structures. Since its identification is challenging, especially after formalin fixation, the mesopancreas was stained directly after removing the specimen from the situs, while the other parts were colored after formalin fixation for 24 to 36 h. All staining procedures were performed by the operating surgeon or by a surgeon present during the procedure.
Fig. 1.
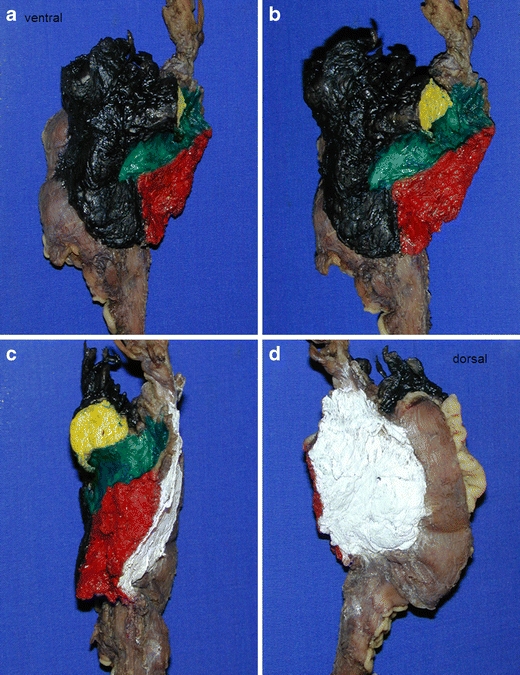
a–d Stained surfaces of pancreatic head resection specimen (black—ventral; white—dorsal; yellow—pancreatic RM; green—groove of superior mesenteric vein; red—mesopancreatic RM)
After fixation and staining, the RMs of the proximal duodenum/stomach, distal duodenum, the common bile duct, and if present any major vessel (SMV, portal vein) were identified and completely embedded. The specimen was serially sliced (0.5- to 1-cm slices) perpendicular to the mesopancreatic RM (Fig. 2a–c). The pancreatic RM and the mesopancreas were completely embedded. Several samples were taken from the tumor with relation to the anterior and posterior surface. The distance between the tumor and each colored surface or resection margin was measured microscopically and documented in the pathohistological report. Histological classification (tumor type, grade of malignancy, pathological tumor–node–metastasis) was carried out according to the current World Health Organization and International Union Against Cancer (UICC) criteria [26]. According to the UICC criteria, the operation was considered as potentially curative (R0) if the RMs and organ surfaces were free of tumor cells, whereas histopathologically verified tumor cell infiltration was defined as R1 resection. In cases of macroscopically visible tumor tissue, the resection was classified R2. Applying the definition of The Royal College of Pathologists (RCP) [13], the specimens were classified R1 if tumor cells were within 1 mm of the RM. Histopathological inclusion criteria were diagnosis of either pancreatic ductal adenocarcinoma (PDAC), distal bile duct adenocarcinomas (DBD), or periampullary adenocarcinoma (PAC).
Fig. 2.
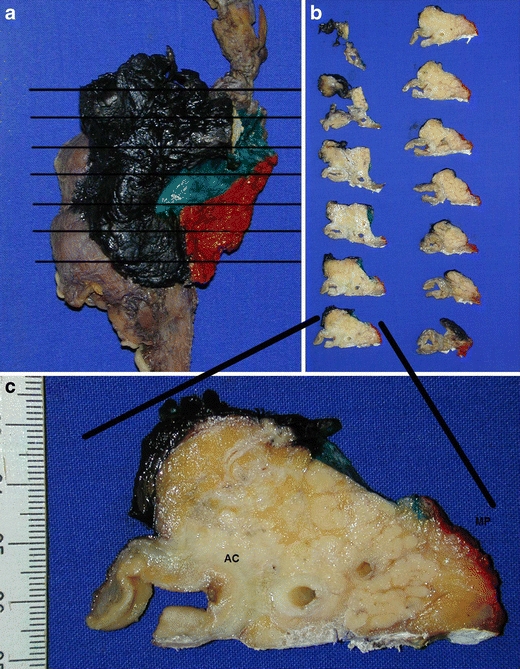
Section planes indicated at resection specimen (a). Individual slices (b) and magnification of one representative slice (c). AC indicates the adenocarcinoma, MP the mesopancreas
Surgical procedures
The vast majority of pancreatic head resections were performed as PPPD. All resection procedures were performed by two experienced surgeons (BMG, HB). Since an extended lymphadenectomy does not necessarily improve patient outcome, we rather intended to achieve oncological radicality through the extended excision of perivascular tissue around the superior mesenteric artery (SMA). To achieve this goal, the SMA was approached caudal to the region of the uncinate process, where a distinct fascia separates the uncinate from the mesocolon. Then, the SMA was isolated laterally right up to the vessel, and all tissues between the artery and the pancreatic parenchyma were resected. Attention was paid not to dissect it entirely from the surrounding mesenteric plexus to avoid postoperative diarrhea (see Fig. 3). Subsequently, the peripancreatic tissue was dissected up to the portal vein. Lymph node dissection was performed up to the hepatoduodenal ligament laterally to the portal vein. Where there was evidence of tumor infiltration, the SMV was partially resected and reconstructed either by end-to-end anastomosis or insertion of a venous graft. Finally, the posterior surface of the pancreatic head specimen was assessed macroscopically for its integrity.
Fig. 3.
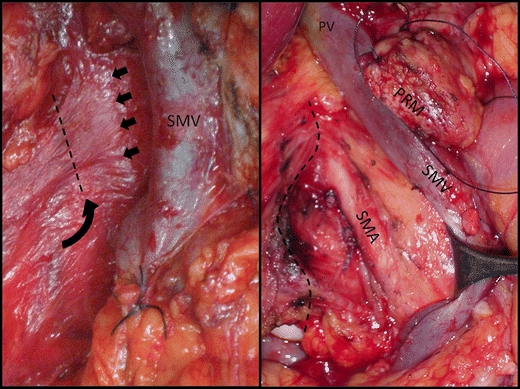
Intraoperative view before (left) and after resection of the mesopancreas (right). Small arrows point to the superior mesenteric artery; large arrow indicates the resection line; dashed line indicates dissection plane (left; SMV—superior mesenteric vein; SMA—superior mesenteric artery; PV—portal vein)
Results
In order to compare the rates of curative and noncurative resections in our department to the published data, we retrospectively identified 115 patients with malignant pancreatic head tumors who had undergone either PPPD or a Kausch–Whipple procedure between 1996 and 2005 (n = 115). For 89 of these 115 patients (77.4%), the operation could be considered potentially curative, whereas the RMs of 26 cancer specimens were positive (22.6%).
In April 2006, we introduced the modified and standardized histopathological workup and applied it prospectively until July 2008. During this 28-month period, 100 consecutively resected pancreatic head specimens were processed according to this protocol. Only five patients underwent a Kausch–Whipple procedure: three patients as a consequence of advanced disease, one owing to inflammatory changes of the tissue, and one owing to the intraoperative detection of a synchronous gastric neoplasia. The remaining 95 patients were treated with PPPD. For 17 patients, the operation included partial or complete resection of the SMV. The vena cava was partially removed once. None of the 100 patients died within 30 days after surgery. A 79-year-old patient who underwent head resection for ductal adenocarcinoma developed endocarditis with consecutive mitral valve regurgitation. He required replacement of the mitral valve but died postoperatively as a result of the cardiac procedure. The remaining 99 patients were discharged from hospital.
After definitive histopathological assessment, 35 patients were excluded from this analysis, owing to histopathological diagnosis as listed in Table 1.
Table 1.
Pancreatic head specimens excluded from analysis
| No. | Nonmalignant or borderline | No. | Malignant |
|---|---|---|---|
| 7 | Chronic pancreatitis | 5 | Neuroendocrine tumor |
| 4 | Autoimmune pancreatitis | 4 | Metastases to the pancreatic head |
| 2 | Periampullary adenoma | 1 | Duodenal adenocarcinoma |
| 2 | Periampullary adenomyoma | 1 | Acinar cell carcinoma |
| 2 | Serous cystadenoma | 1 | Non-Hodgkin lymphoma |
| 2 | Intraductal papillary mucinous neoplasia (IPMN) | ||
| 1 | Mucinous cystadenoma | ||
| 1 | Duodenitis | ||
| 1 | Simple pancreatic cyst | ||
| 1 | Duodenal diverticulum | ||
| 23 | Total | 12 | Total |
Therefore, 65 pancreatic head resections with a malignant tumor were analyzed further (PAC, n = 7; DBD, n = 12; PDAC, n = 46). Applying the UICC criteria, 32 cancers were curatively (R0) resected (49.2%), while 33 cases turned out to be R1 resections (50.8%; Table 2). Seven R1 resections revealed tumor infiltration in two stained areas. Interestingly, the mesopancreas was the only site of infiltration in 17 of these R1 specimens (51.5%). In another five cases, infiltration of the mesopancreas with additional involvement of the SMV or the pancreatic transection margin was discovered. In all, the mesopancreas was determined as being the most frequent site with residual tumor mass by far (n = 22, 56.4%). The groove of the SMV (n = 1), the anterior (n = 2) and posterior surface (n = 1), the pancreatic transection margin (n = 4), and the proximal duodenum (n = 2) were only infiltrated infrequently in the final histological diagnosis. SMV margins were infiltrated in seven of the 17 specimens including partial or complete SMV resection. Applying the definitions of the RCP, an additional set of 13 specimens would have to be considered as R1 resections, resulting in a total percentage of 70.8% of noncurative operations. As expected, the total number of affected areas increased from 39 to 83, involving the mesopancreas (n = 27) and the anterior (n = 18) and the posterior (n = 13) surface most often (Table 2).
Table 2.
Histopathological and resection classification data
| All cancers | PDAC | DBD | PAC | |||||
|---|---|---|---|---|---|---|---|---|
| UICC | RCP | UICC | RCP | UICC | RCP | UICC | RCP | |
| Resection | ||||||||
| R0 | 32 (49.2%) | 19 (29.2%) | 17 (37.0%) | 8 (17.4%) | 10 (83.3%) | 7 (58.3%) | 5 (71.4%) | 4 (57.1%) |
| R1/R2 | 33 (50.8%) | 46 (70.8%) | 29 (63.0%) | 38 (82.6%) | 2 (16.7%) | 5 (41.7%) | 2 (28.6%) | 3 (42.9%) |
| Site of R1 | ||||||||
| Mesopancreas | 22 (56.4%) | 27 (32.5%) | 19 (57.6%) | 24 (34.3%) | 1 (25.0%) | 1 (11.1%) | 2 (100%) | 2 (50.0%) |
| Pancreatic transection margin | 4 (10.3%) | 11 (13.3%) | 3 (9.1%) | 10 (14.3%) | 1 (25.0%) | 1 (11.1%) | 0 | 0 |
| Anterior | 2 (5.1%) | 18 (21.7%) | 2 (6.1%) | 15 (21.4%) | 0 | 1 (11.1%) | 0 | 2 (50.0%) |
| Posterior | 1 (2.6%) | 13 (15.7%) | 1 (3.0%) | 11 (15.7%) | 0 | 2 (22.2%) | 0 | 0 |
| Groove of SMV | 1 (2.6%) | 4 (4.8%) | 1 (3.0%) | 2 (2.9%) | 0 | 2 (22.2%) | 0 | 0 |
| SMV (n = 17) | 7 (17.9%) | 8 (9.6%) | 5 (15.2%) | 6 (8.6%) | 2 (50.0%) | 2 (22.2%) | 0 | 0 |
| Duodenum oral | 2 (5.1%) | 2 (2.4%) | 2 (6.1%) | 2 (2.9%) | 0 | 0 | 0 | 0 |
| Number of infiltrated sites | ||||||||
| 1 | 26 (78.8%) | 22 (47.8%) | 25 (86.2%) | 18 (47.4%) | 0 | 2 (40%) | 2 (100%) | 2 (66.7%) |
| 2 | 7 (21.2%) | 14 (30.4%) | 4 (13.8%) | 11 (28.9%) | 2 (100%) | 2 (40%) | 0 | 1 (33.3%) |
| 3 | 0 | 8 (17.4%) | 0 | 7 (18.4%) | 0 | 1 (20%) | 0 | 0 |
| 4 | 0 | 1 (2.2%) | 0 | 1 (2.6%) | 0 | 0 | 0 | 0 |
| 5 | 0 | 1 (2.2%) | 0 | 1 (2.6%) | 0 | 0 | 0 | 0 |
| Total | 39 | 83 | 33 | 70 | 4 | 9 | 2 | 4 |
| T1 | 2 (3.1%) | 2 (4.3%) | 0 | 0 | ||||
| T2 | 1 (1.5%) | 0 | 0 | 1 (14.3%) | ||||
| T3 | 50 (76.9%) | 43 (93.5%) | 6 (50%) | 1 (14.3%) | ||||
| T4 | 12 (18.5%) | 1 (2.2%) | 6 (50%) | 5 (71.4%) | ||||
| N0 | 12 (18.5%) | 7 (15.2%) | 4 (33.3%) | 1 (14.3%) | ||||
| N1 | 53 (81.5%) | 39 (84.8%) | 8 (66.7%) | 6 (85.7%) | ||||
Resection of 13 PDAC and four DBD included an SMV resection
UICC International Union Against Cancer, RCP Royal College of Pathologists, SMV superior mesenteric vein, PDAC pancreatic ductal adenocarcinoma, DBD distal bile duct adenocarcinoma, PAC periampullary adenocarcinoma
PDAC represent 71% of all analyzed cancer specimens. Looking at each histopathological type, it became obvious that the number of R1 resections is much lower for DBD (16.7% or 41.7% applying UICC or RCP criteria) and PAC (28.6% or 42.9%), irrespective of the classification. Although the total number of R1 resected specimens is too small to draw definitive conclusions, it is noteworthy that the mesopancreas is infiltrated in two of the two R1 resected PAC.
Discussion
Cancer of the pancreatic head is one of the most malignant gastrointestinal tumors. Surgery is still considered to be the only potentially curative approach if complete resection is possible [6, 20, 23]. However, surgical resection in patients with localized pancreatic cancer is still underused [14]. Retrospective analyses of data from patients treated in our department between 1996 and 2005 revealed a 5-year survival rate of 20% for R0 patients, which is in agreement with the literature, even though some authors deny the existence of 5-year survivors [4]. With respect to the classification of the pancreatic head resections evaluated retrospectively, the percentage of R1 resections (22.6%) also mirrors the literature [12, 15, 23, 27]. These data appear to indicate the possible misclassification of R1 resections as R0.
Local recurrence and disseminated cancer spread dramatically impair the prognosis of patients with pancreatic head cancer. This is supported by postmortem examinations reporting a local recurrence rate approaching 100% [5, 7, 19, 21, 24]. Luettges et al. [8, 13] already stated in 1999 that tumor recurrence is primarily due to incomplete removal at the site of resection rather than to metastatic disease. They pointed out that the retroperitoneal RM has an influence on patient survival. However, it was in 2006 when Verbeke et al. [22] first reported an incomplete resection rate of 85% using a standardized and intensified workup. For the 54 pancreatic head resections, a color code was implemented to distinguish between the anterior, posterior, and SMV groove surface. Similar results were published by Esposito et al. [2] who reported an R1 resection rate of 76% in 111 PDAC. As part of their protocol, they color-coded the anterior, posterior, medial margin, and groove surface of the SMV, respectively, whereas the retroperitoneal RM was not investigated separately. The importance of the retroperitoneal resection margin was confirmed by Westgaard et al. [25] who thoroughly worked up 114 periampullary adenocarcinomas by perpendicular sectioning. The overall R1 resection rate was 35%, whereas the retroperitoneal resection margin was involved in 80% of the specimens. However, it should be pointed out that all three studies classified the specimens according to the definition of The Royal College of Pathologists. Since there do not exist any general guidelines about the definition of R1 resection, we primarily applied the UICC criteria, i.e., a curative resection was defined as there being no microscopic evidence of residual tumor at the RM. We found an R1 resection rate of 50.8%, which demonstrates that a high rate of R1 resections is not only based on the definition of margin positivity as tumor clearance of ≤1 mm.
Our R1 rate (using RCP criteria) was comparable to those from Verbeke et al. [22] and Esposito et al. [2]. Therefore, we could confirm that the number of noncurative resections is considerably higher when a modified and intensified histopathological workup is applied. Interestingly, Westgaard et al. [25] only investigated the transection margins of the pancreas and reached R1 rate of 45% for PDAC and 59% for DBD. The anterior or posterior surfaces of the pancreas were not part of the workup.
We identified the mesopancreas as the primary site of positive RMs. In total, 66.6% of those cancers resected noncuratively displayed infiltration of this structure. As pointed out by other authors [8, 25] the retroperitoneal RM is of great interest with regard to curative resection. Interestingly, there is no exact definition of the retroperitoneal RM. Some consider the complete posterior surface of the pancreas as retroperitoneal margin, while others use the term to describe just the area of sharp dissection, similar to what we call mesopancreatic RM. Esposito et al. [2] defined medial and posterior soft tissue margins to acknowledge the importance of the region. This diversity of definitions impairs a meaningful comparison of RMs. Therefore, we introduced the term “mesopancreatic RM” to describe the dissection margin in the peripancreatic fatty tissue behind the pancreatic head and lateral to the mesenteric artery. It was chosen because of its anatomical origin and therapeutic implication. The tissue between the pancreatic parenchyma and the SMA consists of fatty tissue and contains blood and lymphatic vessels, as well as lymph nodes draining the pancreatic head and the uncinate. Additionally, nerve fibers are located in the mesopancreas innervating the pancreatic parenchyma. In this context, these structures should be defined as mesopancreas although the peritoneal attachment, which is a requisite to the existence of a “meso” [10], was lost during embryological development owing to duodenal rotation. The mesopancreas rises from the embryological mesentery attaching the pancreatic bud to the abdominal wall. This leads to the consequence that the mesopancreas must be resected and removed completely in its integrity down to the mesenteric artery. Based on the embryological development and according to our experience, the pancreatic tissue is not directly adjacent to the mesenteric artery but connected by a delicate meshwork of connective tissue rich in nerve fibers (mesenteric plexus). This layer should be separated close to the mesopancreas to prevent the complications of postoperative diarrhea.
As Verbeke and colleagues demonstrated [22], intensive embedding of resected tissue increases the rate of R1 resections. However, infiltration of the mesopancreas may have been misinterpreted in the past as a consequence of a cancer-induced fibrosis or disseminated cancer cells. Therefore, RMs in their integrity and numerous samples from the tumor with relation to the surfaces of the pancreas were embedded as part of this modified and standardized protocol.
It is widely accepted that only an R0 resection is considered as a curative approach and stratification for resection status is routinely performed in clinical trials such as in the CONKO-001 trial. Numerous trials failed to show significant differences in patients’ treatment which could possibly be due to the misinterpretation of the resection status based on the lack of a standardized workup [17]. In general, R1 resections rates of about 20% are reported [11, 16, 18, 27]. However, one can speculate that in these trials the low R1 resection rates are due to a conventional pathohistological workup. Being aware of the crucial importance of assessing the resection rate an intensified workup is obligatory in trials such as CONKO-005 and CONKO-006. Considering the mesopancreas as a structure guiding relevant vessels for lymphatic and blood drainage of the pancreatic head and the uncinate, it may be hypothesized that tumor cells drain into the lymphatic and blood vessels during manipulation of the pancreatic head (e.g., Kocher’s maneuver). As in the treatment of colorectal cancer, a no-touch technique would diminish this potential influence, resulting in the need to resect the mesopancreas along the superior mesenteric artery first.
Based on our data, we propose a standardized histopathological workup for pancreatic head cancer specimens, which may represent a more accurate assessment of curative and noncurative resection rates. As a consequence of this modified protocol, we demonstrate that the mesopancreas is a frequent site for positive resection margins, which has potential therapeutic implications and should be considered in clinical trials when stratifying patients into R0 and R1 resection classifications. Owing to morphological changes during formalin fixation, it is of upmost importance to color the mesopancreatic RM directly after surgical resection. We strongly believe that the complete and meticulous surgical resection of the mesopancreas as the structure to the right of the mesenteric artery must become the standard surgical approach in pancreatic head resection.
Acknowledgment
The authors thank J. Eggert and L. Schroeter for technical support.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Buchler MW, Kleeff J, Friess H. Surgical treatment of pancreatic cancer. J Am Coll Surg. 2007;205:S81–S86. doi: 10.1016/j.jamcollsurg.2007.06.332. [DOI] [PubMed] [Google Scholar]
- 2.Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess H, Schirmacher P, Buchler MW. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 2008;15:1651–1660. doi: 10.1245/s10434-008-9839-8. [DOI] [PubMed] [Google Scholar]
- 3.Fortner JG. Regional resection of cancer of the pancreas: a new surgical approach. Surgery. 1973;73:307–320. [PubMed] [Google Scholar]
- 4.Gudjonsson B. Survival statistics gone awry: pancreatic cancer, a case in point. J Clin Gastroenterol. 2002;35:180–184. doi: 10.1097/00004836-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Hishinuma S, Ogata Y, Tomikawa M, Ozawa I, Hirabayashi K, Igarashi S. Patterns of recurrence after curative resection of pancreatic cancer, based on autopsy findings. J Gastrointest Surg. 2006;10:511–518. doi: 10.1016/j.gassur.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Jarufe NP, Coldham C, Mayer AD, Mirza DF, Buckels JA, Bramhall SR. Favourable prognostic factors in a large UK experience of adenocarcinoma of the head of the pancreas and periampullary region. Dig Surg. 2004;21:202–209. doi: 10.1159/000079346. [DOI] [PubMed] [Google Scholar]
- 7.Kayahara M, Nagakawa T, Ueno K, Ohta T, Takeda T, Miyazaki I. An evaluation of radical resection for pancreatic cancer based on the mode of recurrence as determined by autopsy and diagnostic imaging. Cancer. 1993;72:2118–2123. doi: 10.1002/1097-0142(19931001)72:7<2118::AID-CNCR2820720710>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 8.Luttges J, Vogel I, Menke M, Henne-Bruns D, Kremer B, Kloppel G. The retroperitoneal resection margin and vessel involvement are important factors determining survival after pancreaticoduodenectomy for ductal adenocarcinoma of the head of the pancreas. Virchows Arch. 1998;433:237–242. doi: 10.1007/s004280050242. [DOI] [PubMed] [Google Scholar]
- 9.Michalski CW, Kleeff J, Wente MN, Diener MK, Buchler MW, Friess H. Systematic review and meta-analysis of standard and extended lymphadenectomy in pancreaticoduodenectomy for pancreatic cancer. Br J Surg. 2007;94:265–273. doi: 10.1002/bjs.5716. [DOI] [PubMed] [Google Scholar]
- 10.Morgado PJ. Total mesorectal excision: a misnomer for a sound surgical approach. Dis Colon Rectum. 1998;41:120–121. doi: 10.1007/BF02236909. [DOI] [PubMed] [Google Scholar]
- 11.Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine F, Falconi M, Pederzoli P, Pap A, Spooner D, Kerr DJ, Buchler MW. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350:1200–1210. doi: 10.1056/NEJMoa032295. [DOI] [PubMed] [Google Scholar]
- 12.Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C, Gutberlet K, Kettner E, Schmalenberg H, Weigang-Koehler K, Bechstein WO, Niedergethmann M, Schmidt-Wolf I, Roll L, Doerken B, Riess H. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267–277. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- 13.The Royal College of Pathologists . Standards and minimum datasets for reporting cancers. Minimum dataset for the histopathological reporting of pancreatic, ampulla of Vater and bile duct carcinoma. London: The Royal College of Pathologists; 2002. [Google Scholar]
- 14.Riall TS, Lillemoe KD. Underutilization of surgical resection in patients with localized pancreatic cancer. Ann Surg. 2007;246:181–182. doi: 10.1097/SLA.0b013e31811eaa2c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richter A, Niedergethmann M, Sturm JW, Lorenz D, Post S, Trede M. Long-term results of partial pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head: 25-year experience. World J Surg. 2003;27:324–329. doi: 10.1007/s00268-002-6659-z. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, Baumgardner JA, Cummings OW, Jacobson LE, Broadie TA, Canal DF, Goulet RJ, Jr, Curie EA, Cardenes H, Watkins JM, Loehrer PJ, Lillemoe KD, Madura JA. Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg. 2004;139:718–725. doi: 10.1001/archsurg.139.7.718. [DOI] [PubMed] [Google Scholar]
- 17.Smeenk HG, van Eijck CH, Hop WC, Erdmann J, Tran KC, Debois M, van Cutsem E, van Dekken H, Klinkenbijl JH, Jeekel J. Long-term survival and metastatic pattern of pancreatic and periampullary cancer after adjuvant chemoradiation or observation: long-term results of EORTC trial 40891. Ann Surg. 2007;246:734–740. doi: 10.1097/SLA.0b013e318156eef3. [DOI] [PubMed] [Google Scholar]
- 18.Sohn TA, Yeo CJ, Cameron JL, Koniaris L, Kaushal S, Abrams RA, Sauter PK, Coleman J, Hruban RH, Lillemoe KD. Resected adenocarcinoma of the pancreas—616 patients: results, outcomes, and prognostic indicators. J Gastrointest Surg. 2000;4:567–579. doi: 10.1016/S1091-255X(00)80105-5. [DOI] [PubMed] [Google Scholar]
- 19.Sperti C, Pasquali C, Piccoli A, Pedrazzoli S. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg. 1997;21:195–200. doi: 10.1007/s002689900215. [DOI] [PubMed] [Google Scholar]
- 20.Stojadinovic A, Brooks A, Hoos A, Jaques DP, Conlon KC, Brennan MF. An evidence-based approach to the surgical management of resectable pancreatic adenocarcinoma. J Am Coll Surg. 2003;196:954–964. doi: 10.1016/S1072-7515(03)00010-3. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi S, Ogata Y, Miyazaki H, Maeda D, Murai S, Yamataka K, Tsuzuki T. Aggressive surgery for pancreatic duct cell cancer: feasibility, validity, limitations. World J Surg. 1995;19:653–659. doi: 10.1007/BF00294750. [DOI] [PubMed] [Google Scholar]
- 22.Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232–1237. doi: 10.1002/bjs.5397. [DOI] [PubMed] [Google Scholar]
- 23.Wagner M, Redaelli C, Lietz M, Seiler CA, Friess H, Buchler MW. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004;91:586–594. doi: 10.1002/bjs.4484. [DOI] [PubMed] [Google Scholar]
- 24.Westerdahl J, Andren-Sandberg A, Ihse I. Recurrence of exocrine pancreatic cancer-local or hepatic? Hepatogastroenterology. 1993;40:384–387. [PubMed] [Google Scholar]
- 25.Westgaard A, Tafjord S, Farstad IN, Cvancarova M, Eide TJ, Mathisen O, Clausen OP, Gladhaug IP. Resectable adenocarcinomas in the pancreatic head: the retroperitoneal resection margin is an independent prognostic factor. BMC Cancer. 2008;8:5. doi: 10.1186/1471-2407-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wittekind C, Klimpfinger M, Sobin LH. UICC: TNM Atlas. Illustrierter Leitfaden zur TNM/pTNM-Klassifikation maligner Tumoren. Berlin: Springer; 2005. [Google Scholar]
- 27.Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, Hruban RH, Ord SE, Sauter PK, Coleman J, Zahurak ML, Grochow LB, Abrams RA. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997;226:248–257. doi: 10.1097/00000658-199709000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]


