Abstract
A dedifferentiated liposarcoma of the retroperitoneum is an extremely rare tumor. A 51-year old man was admitted to our department because a retroperitoneal mass was seen on abdominal computed tomography at another hospital. Computed tomography of the abdomen and magnetic resonance imaging showed a large pelvic mass located in the right hemipelvis, and it was pushing the right ureter and invading the right kidney, duodenum, colon and inferior vena cava. The patient underwent right radical nephrectomy, pylorus preserving pancreatoduodenectomy, right hemicolectomy and artificial blood vessel replacement for the inferior vena cava. The histopathological diagnosis was dedifferentiated liposarcoma and the patient was free from recurrence on the computed tomography that was done 6 months after the operation.
Keywords: Dedifferentiation, Liposarcoma, Retroperitoneum
Introduction
Liposarcoma is the most common malignant tumor in the retroperitoneal soft tissue, and this tumor is classified according to the amount of lipid inside the cells, the mucoid lipid and the degree of cell differentiation. This tumor is classified into the well differentiated, myxoid, round cell, pleomorphic and dedifferentiated types (1), and the pleomorphic type is known to be the most common type. The dedifferentiated liposarcoma refers to a condition in which well and poorly differentiated liposarcoma and non-lipomatous sarcoma coexist in one tumor. This type has a vague prognosis compared to other types of sarcoma, and making the histological diagnosis can be difficult.
Dedifferentiated liposarcoma commonly develops in the retroperitoneum, limbs, testis and spermatic cord, yet there are only a few such case reports from Korea (2,3), and retroperitoneal liposarcoma is quite rare.
We report here on a case of primary dedifferentiated liposarcoma in the retroperitoneum.
Case Report
A 51-year-old asymptomatic male patient was referred to our hospital with the retroperitoneal tumor that was incidentially detected by abdominal ultrasonography during a routine medical check. His vital signs were normal on the physical examination, and a solid non-tender mass was palpable in the right hypogastric area. The blood tests, including the blood cell count (CBC), showed no abnormal findings except for a slight leukocytosis (10,700/mm3).
The patient had been on insulin treatment for 2 years to control his blood sugar.
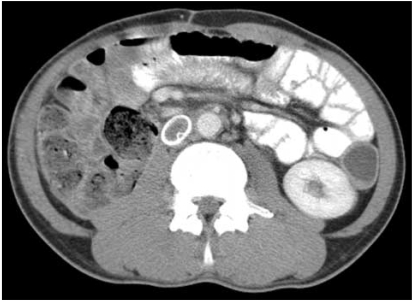
Abdomino-pelvic CT scans showed a huge mass in the retroperitoneum, with suspicious infiltration into the right kidney, the duodenum, the inferior vena cava and the ascending colon, but there were no enlarged lymph nodes (Fig. 1). Magnetic resonance imaging (MRI) gave no additional information (Fig. 2).
Fig. 1.
CT of the abdomen shows a huge fat containing mass in the retroperitoneum. The right kidney, duodenum, inferior vena cava and pancreas are adhered to the mass.
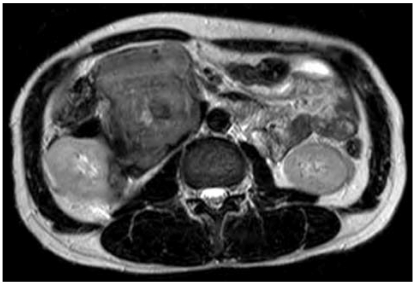
Fig. 2.
MRI of the abdomen shows a huge solid soft tissue mass.
The fine needle aspiration biopsy report suggested the possibility of sarcoma. On laparotomy for radical excision, a huge mass covering from the midriff to the aorta via the bottom side of the kidney was discovered. The mass had severe synechia with the right kidney, duodenum, ascending colon, inferior vena cava and pancreas, so he received retroperitoneal tumor excision and radical nephrectomy, ascending colectomy, artificial blood vessel replacement for the inferior vena cava and pancreatoduodenectomy. The mass measured 15 × 12 × 7 cm and it weighed 2.8 kg; the mass was mutinodular and covered with a capsule. The incisional surface was very hard and the tumor displayed different sized areas of necrosis and calcification. The mass had infiltrated into the surrounding organs, including the right kidney, duodenum, pancreas, ascending colon and inferior vena cava (Fig. 3).
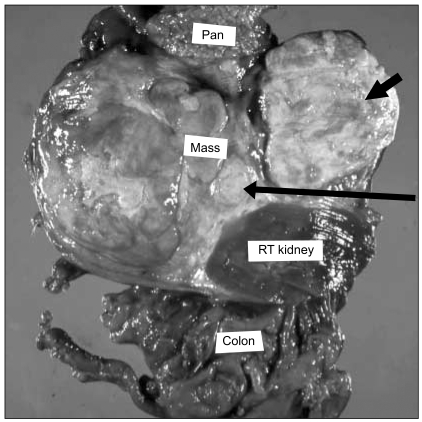
Fig. 3.
On sectioning, the tumor mass shows a poorly circumscribed solid cut surface with multifocal necrosis, calcification and discrete intratumoral nodules of varying sizes. The right kidney is partially encased and the mass has grossly infiltrated the surrounding duodenum (thick arrow), the inferior vena cava wall (thin arrow), the pancreas and the colon.
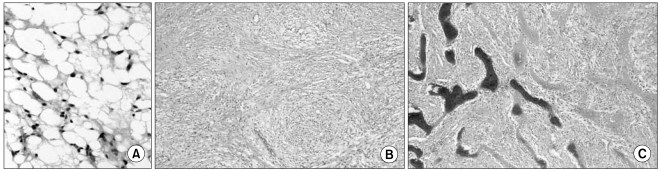
Microscopic examination revealed malignant fusiform cells and dedifferentiated liposarcoma, and this was accompanied with mucoid malignant fibrous histiocytoma coexisting with multicentric metaplastic ossification, with neither lymph node metastasis nor involvement of the resection margin (Fig. 4).
Fig. 4.
The tumor consisted of a few components. (A) Well-differentiated liposarcoma area (H&E, ×400), (B) a fibrosarcomatous area (H&E, ×200) and (C) myxoid and neural whirling-like spindle cell nodules with multifocal metaplastic ossification (H&E, ×200).
The postoperative course was relatively uneventful until 20 days after the surgery, when right upper quadrant abdominal pain developed with elevated amylase (203 IU/l, normal: 28~100 IU/L) and lipase (4,077 IU/l, normal: 13~60 IU/l) levels. Antibiotic treatment was started under the diagnosis of acute pancreatitis, and four days afterward, the patient's symptoms were much relieved and the laboratory findings improved (the amylase level: 65 IU/l and the lipase level: 354 IU/l). There was neither recurrence nor metastasis on the follow-up CT that was done 6 months after surgery (Fig. 5).
Fig. 5.
The follow-up CT taken six months after the operation shows no evidence of recurrence.
Discussion
A retroperitoneal tumor often develops in people in their 40's to 50's, and especially in men, but it is a very rare tumor that accounts for less than 0.2% of all types of malignant tumors. Based on its histological features, liposarcoma was initially classified into four subtypes: the well differentiated, myxoid, round cell and pleomorphic types. Evans introduced dedifferentiated liposarcoma later in 1979, so now there are five subtypes (4). The feature of dedifferentiated liposarcoma is the histological coexistence of well to poorly differentiated liposarcoma and non-lipomatous differentiated areas (5).
As the mass grows, there is usually no initial subjective symptoms, and making the diagnosis is often difficult until the tumor reaches a great size to cause symptoms of pressure. Complete surgical removal is often difficult and the tumor tends to recur, which make it hard to treat. Our case also did not have symptoms, and the mass was found when performing an abdominal ultrasound exam on a routine medical examination, and then the patient sought medical attention. The main symptom of a retroperitoneal tumor is abdominal discomfort. If the tumor reaches a very large size, it exerts pressure to the surrounding organs, and the patent may experience abdominal distention and pain. The size of dedifferentiated liposarcoma has been reported to range from 2 to 80 cm, and the tumor in our patient measured 15 × 12 × 7 cm.
Surgery or biopsy is the most reliable method for making the diagnosis of retroperitoneal tumors, and, chest x-ray, abdominal xray, ultrasound, CT, and MRI are most commonly used for radiologic examination. Transversion of the kidney and ureter and/or compression of the urinary bladder by compressing tumor may be seen on the excretory urography. Adipose tissue (below 30 HU), soft tissue (34~76 HU) and the tissue with borderline density can be observed on CT. On MRI, the most dedifferentiated component of dedifferentiated liposarcomas is undifferentiated high-grade pleomorphic sarcoma or ibrosarcoma. These areas typically have nonspecific findings, low to intermediate signal intensity on T1-weighted MR images and intermediate to high signal intensity on T2-weighted MR images.
For treatment, complete removal of retroperitoneal sarcoma is the most effective point and radical complete surgical removal has a remarkable effect on the survival rate. However, there are many cases with limited resectability because of the tumor being too big or there is invasion to organs around it or adhesion with the great vessels. The rate of complete removal is 50% on average (15~78%) (6). Radiation therapy or additional chemotherapy can be considered for the poorly differentiated sarcoma that is more than more than 10 cm in size or for the cases of incomplete removal. In this current case, although there was infiltration to the right kidney, duodenum, inferior vena cava, ascending colon and pancreas, it was fortunate that complete removal was possible with clear resection margins, and no additional treatment was recommended.
When making the diagnosis of liposarcoma, the subtypes of the sarcoma are closely related to the prognosis, so the histologic examination is important. Dedifferentiated liposarcoma has a worse prognosis than other subtypes because it has a higher risk of local recurrence and distant metastasis.
It ahs been recently noted that patients with retroperitoneal tumors have a lower survival rate compared to those with tumor in other parts of body, so the anatomic site of tumor is recognized as an important prognosis factor. When performing surgery, completeness of removal is also another prognosis factor that has a large impact on survival and the recurrence rate (7). Other than that, there are reports saying that a positive incisional surface is other element that has an impact on local recurrence, and receuurence is seen for 27~29% of the completely incised tumors (8). This case has not shown recurrence for six months after the surgery and the patient is undergoing regular follow-up check-ups.
References
- 1.Antinori A, Antonacci V, Magistrelli P. Giant retroperitoneal liposarcoma. Am J Surg. 2002;184:56–57. doi: 10.1016/s0002-9610(02)00880-2. [DOI] [PubMed] [Google Scholar]
- 2.Moon WS, Jeong MJ, Lee DG, Choi HY, Kim SH. Dedifferentiated liposarcoma of the retroperitoneum: a case report. Korean J Pathol. 1993;27:296–298. [Google Scholar]
- 3.Cho YJ, Chun HJ, Park DK, Kim YB, Koh DW, Choung RS, et al. A case of dedifferentiated liposarcoma of retroperitoneum. Korean J Med. 2002;62:552–556. [Google Scholar]
- 4.Evans HL. Liposarcomas: a study of 55 cases with a reassessment of its classification. Am J Surg Pathol. 1979;3:507–523. doi: 10.1097/00000478-197912000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Tateishi U, Hasegawa T, Beppu Y, Satake M, Moriyama N. Primary dedifferentiated liposarcoma of the retroperitoneum. Prognostic significance of computed tomography and magnetic resonance imaging features. J Comput Assist Tomogr. 2003;27:799–804. doi: 10.1097/00004728-200309000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Malkowicz SB. Urologic oncology. 1st ed. Philadelphia: Saunders; 1997. Retroperitoneal tumors: diagnosis, staging, surgery, management, and prognosis; pp. 539–557. [Google Scholar]
- 7.Henricks WH, Chu YC, Goldblum JR, Weiss SW. Dedifferentiated liposarcoma: a clinicopathologic analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol. 1997;21:271–281. doi: 10.1097/00000478-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 8.McCormick D, Mentzel T, Beham A, Fletcher CD. Dedifferentiated liposarcoma. Clinicopathologic analysis of 32 cases suggesting a better prognostic subgroup among pleomorphic sarcomas. Am J Surg Pathol. 1994;18:1213–1223. doi: 10.1097/00000478-199412000-00004. [DOI] [PubMed] [Google Scholar]