Summary
Background
Stents are an alternative treatment to carotid endarterectomy for symptomatic carotid stenosis, but previous trials have not established equivalent safety and efficacy. We compared the safety of carotid artery stenting with that of carotid endarterectomy.
Methods
The International Carotid Stenting Study (ICSS) is a multicentre, international, randomised controlled trial with blinded adjudication of outcomes. Patients with recently symptomatic carotid artery stenosis were randomly assigned in a 1:1 ratio to receive carotid artery stenting or carotid endarterectomy. Randomisation was by telephone call or fax to a central computerised service and was stratified by centre with minimisation for sex, age, contralateral occlusion, and side of the randomised artery. Patients and investigators were not masked to treatment assignment. Patients were followed up by independent clinicians not directly involved in delivering the randomised treatment. The primary outcome measure of the trial is the 3-year rate of fatal or disabling stroke in any territory, which has not been analysed yet. The main outcome measure for the interim safety analysis was the 120-day rate of stroke, death, or procedural myocardial infarction. Analysis was by intention to treat (ITT). This study is registered, number ISRCTN25337470.
Findings
The trial enrolled 1713 patients (stenting group, n=855; endarterectomy group, n=858). Two patients in the stenting group and one in the endarterectomy group withdrew immediately after randomisation, and were not included in the ITT analysis. Between randomisation and 120 days, there were 34 (Kaplan-Meier estimate 4·0%) events of disabling stroke or death in the stenting group compared with 27 (3·2%) events in the endarterectomy group (hazard ratio [HR] 1·28, 95% CI 0·77–2·11). The incidence of stroke, death, or procedural myocardial infarction was 8·5% in the stenting group compared with 5·2% in the endarterectomy group (72 vs 44 events; HR 1·69, 1·16–2·45, p=0·006). Risks of any stroke (65 vs 35 events; HR 1·92, 1·27–2·89) and all-cause death (19 vs seven events; HR 2·76, 1·16–6·56) were higher in the stenting group than in the endarterectomy group. Three procedural myocardial infarctions were recorded in the stenting group, all of which were fatal, compared with four, all non-fatal, in the endarterectomy group. There was one event of cranial nerve palsy in the stenting group compared with 45 in the endarterectomy group. There were also fewer haematomas of any severity in the stenting group than in the endarterectomy group (31 vs 50 events; p=0·0197).
Interpretation
Completion of long-term follow-up is needed to establish the efficacy of carotid artery stenting compared with endarterectomy. In the meantime, carotid endarterectomy should remain the treatment of choice for patients suitable for surgery.
Funding
Medical Research Council, the Stroke Association, Sanofi-Synthélabo, European Union.
Introduction
Carotid endarterectomy became the treatment of choice for patients with recently symptomatic, severe carotid artery stenosis after the publication of results from large randomised trials that compared endarterectomy with best medical treatment alone.1–3 The potential benefit of endovascular treatment (angioplasty with or without stenting) as an alternative to carotid endarterectomy was first highlighted by the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS).4 This trial showed that endovascular treatment largely avoided the main complications of the endarterectomy incision (namely cranial nerve injury and severe haematoma). However, the rate of stroke or death within 30 days after treatment was high in both groups. Since completion of CAVATAS, stenting has largely replaced angioplasty, and stents and protection devices specifically designed for the carotid artery have been introduced. Two large randomised trials comparing use of carotid stenting with endarterectomy for symptomatic stenosis have subsequently published short-term outcomes and longer term results.5–8 The Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) trial in symptomatic patients did not show non-inferiority of stenting compared with endarterectomy within 30 days after treatment and was stopped early for reasons of futility and cost.6 The Endarterectomy versus Stenting in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) trial was stopped early because of a significantly lower rate of periprocedural stroke or death in the endarterectomy group than in the stenting group.5 We report the short-term results of the International Carotid Stenting Study (ICSS), a randomised trial comparing stenting versus endarterectomy for recently symptomatic carotid artery stenosis.
Methods
Study centres and participants
ICSS is an international, multicentre, open, randomised controlled trial designed to compare the safety and long-term efficacy of carotid stenting and endarterectomy. The protocol was published in 20049 and is publically available on the trial website. ICSS was approved by the Northwest Multicentre Research Ethics Committee in the UK and participating centres had to obtain site-specific approval from their local ethics committees. All patients provided written informed consent.
Participating centres had a team of investigators consisting of at least one neurologist or physician with an interest in stroke, a surgeon with experience in endarterectomy, and a physician or surgeon with expertise in carotid angiography, angioplasty, and stenting. All centres were required to hold regular multidisciplinary meetings between the investigators to discuss the management of patients with carotid stenosis. Investigators submitted their curriculum vitae and audit data that documented satisfactory training and results of carotid treatment to the credential committee. Centres were then enrolled as either experienced or supervised centres on the recommendation of the committee. To qualify as experienced, a centre had to have a surgeon who had done at least 50 carotid operations (ten or more cases per year) and a physician or surgeon who had done a minimum of 50 stenting procedures, with at least ten cases in the carotid artery. Centres not fulfilling these criteria joined as supervised centres and their trial procedures had to be proctored by an outside surgeon or interventionist, appointed by the trial steering committee, until the proctor was satisfied that the centre was proficient in undertaking the procedure. Supervised centres were promoted to experienced centres after randomisation and treatment of 20 cases within the trial if their results were deemed acceptable by the proctor and the credential committee.
Patients were eligible for enrolment if they were older than 40 years of age and had symptomatic atheromatous carotid artery stenosis measured as more than 50% by the North American Symptomatic Carotid Endarterectomy Trial criteria2 (or non-invasive equivalent) deemed to require treatment. Symptoms attributable to the randomised artery needed to have occurred within 12 months before randomisation.
Non-invasive imaging of the carotid artery, including duplex ultrasound, was acceptable for study entry. Catheter angiography before randomisation was not required. Exclusion criteria included major stroke without useful recovery of function, previous carotid endarterectomy or stenting in the randomised artery, contraindications for either treatment, and planned coronary artery bypass grafting or other major surgery.
At randomisation, patients had to be deemed suitable for both surgery and stenting by the investigators, who also had to be uncertain which of the two treatments was the best option for the patient. Patients unsuitable for stenting because of tortuous anatomy proximal or distal to the stenosis, visible thrombus, proximal common carotid artery stenosis, or internal carotid artery pseudo-occlusion were excluded, as were patients unsuitable for endarterectomy because of the distal site of the stenosis, a rigid neck, or risk factors for surgical complications. No record was kept of patients screened who were ineligible or treated outside the trial. It was recommended that patients randomised to stenting after non-invasive investigation, in which subsequent angiography before stenting showed one or more exclusion criteria, should have the procedure abandoned and be treated by surgery, if appropriate, or medical care alone. A similar approach was taken in patients randomised to surgery.
Randomisation and masking
Eligible patients were randomly assigned in a 1:1 ratio to receive carotid artery stenting or carotid endarterectomy by use of a computerised service provided by Oxford Clinical Trials Service Unit staff who were not involved in other parts of the trial. The allocated treatment was communicated to investigators or one of their research team by telephone or fax after they provided baseline data for the patient. Randomisation was stratified by centre with minimisation for sex, age, contralateral occlusion, and side of the randomised artery. Investigators were kept masked about the randomisation program to prevent them anticipating the next assignment. Patients and individuals who delivered the interventions were not masked to treatment assignment. Patients were followed up by independent clinicians who were not masked to treatment assignment but who were not directly involved in delivering the randomised treatment. Adjudication of outcomes was blinded. Apart from the trial statistician and the data monitoring committee, all investigators, including the chief investigator, remained masked to the results of the trial until after recruitment was completed.
Procedures
Carotid stenting or endarterectomy was deemed initiated if the patient had been given general or local anaesthetic in preparation for the intervention, even if the procedure was subsequently abandoned before stent deployment or endarterectomy. Stents and other devices used for carotid stenting were chosen at the discretion of the interventionist but had to have a CE mark. The protocol recommended that a cerebral protection device should be used whenever the local investigator thought that one could be used safely, but this was not mandatory. A combination of aspirin and clopidogrel to cover stenting procedures was recommended. Use of heparin and atropine or similar agent during the procedure was mandatory. Surgeons were free to use standard or eversion endarterectomy. The use of local or general anaesthesia, shunts, and patches was left to the discretion of the surgeon.
Outcome events and trial safety
The protocol specified that patients should be seen before randomisation and then followed up 30 days after treatment, 6 months after randomisation, and then once a year after randomisation by a clinician who was not involved in the revascularisation procedure. At every visit, levels of impairment were assessed with the modified Rankin scale. Outcome events were reported in detail to the central office by the local neurologist or stroke physician. Major outcome events were submitted to an independent external adjudicator, who was masked to treatment allocation and who determined the cause, severity, and duration of the event. If this assessment differed from the initial assessment, a second external adjudicator reviewed the event and any differences were resolved by consensus.
The primary analysis specified in the protocol was the difference between groups in long-term rate of fatal or disabling stroke in any territory. Long-term was defined as 3 years and therefore data are not yet available for this analysis. Here, we report the first secondary analysis specified in the protocol: the differences in mortality and morbidity between groups within 30 days of carotid treatment. The main endpoint for this analysis was defined before analysis as any stroke, death, or procedural myocardial infarction. Secondary endpoints of particular interest were any stroke, any stroke or death, any stroke or procedural death, disabling stroke or death, and all-cause death. Events relating to the various components of the main endpoint, cranial nerve palsies, and haematomas requiring surgery, transfusion, or extended hospital stay, were analysed.
Stroke was defined as a rapidly developing clinical syndrome of focal disturbance of cerebral function lasting more than 24 h or leading to death with no apparent cause other than that of vascular origin. Stroke was classified as fatal if death attributed to stroke occurred within 30 days of onset of stroke. Stroke or cranial nerve palsy were classified as disabling if there was an increase in the Rankin score to 3 or more, attributable to the event at 30 days after onset. The remaining non-fatal strokes were classified as non-disabling. Myocardial infarction was defined by the presence of two of the following three criteria: specific cardiac enzymes more than twice the upper limit of normal; history of chest discomfort for at least 30 min; or the development of specific abnormalities (eg, Q waves) on a standard 12-lead electrocardiograph. Death or myocardial infarction was defined as procedural if it occurred within 30 days of stenting or endarterectomy. Transient ischaemic attack was defined as an acute disturbance of focal neurological function with symptoms lasting less than 24 h attributed to cerebrovascular disease, but was not included as an outcome event in the analyses reported here.
The rate of reported events at individual centres was monitored at the central office. The independent data monitoring committee met on a regular basis to review the accumulating data and to monitor trial safety.
Statistical analysis
A large difference in outcomes between the stenting and endarterectomy groups was not expected and the sample size was calculated to provide a reasonable estimate of the treatment effect. A sample size of 1500 patients from experienced centres was chosen on the basis that this would allow a 95% CI to be measured with a width of ±3·3 percentage points for the difference in risk of disabling stroke or death between treatment groups, based on an average of 12·5% of patients having the outcome. We also calculated that this sample size would allow a 95% CI to be measured with a width ±3·0 percentage points for the secondary short-term outcome of 30-day stroke, death, or procedural myocardial infarction, on the basis of an average of 10% of patients having the outcome.
Because some patients did not receive their allocated treatment and the timing of treatment after randomisation varied, we undertook two main analyses: an intention-to-treat (ITT) analysis of all events occurring up to 120 days after randomisation and a per-protocol analysis of the procedural risk within 30 days of allocated treatment. All main analyses combined patients from experienced and supervised centres.
The ITT analysis included all randomised patients and compared those allocated to stenting with those allocated to endarterectomy, irrespective of whether they received their allocated treatment or not. All events between randomisation and 120 days were included in the ITT analysis, irrespective of whether they occurred within 30 days of treatment or not. This analysis therefore compared the initial policy of referral for stenting with referral for endarterectomy in terms of outcome over 120 days. The period of 120 days was chosen because most patients should have had their treatment within 3 months of randomisation and their 30-day post-treatment follow-up appointment within 4 months after randomisation.
Patients with less than 120 days of follow-up and without an event were censored on the date of last follow-up. Censoring was assumed to be non-informative—ie, a censored patient was assumed to have the same risk of an outcome event as those who had complete 120-day follow-up. Kaplan-Meier methods were used to estimate 120-day probabilities of an event and subsequently the absolute risk difference between the two treatment groups and corresponding 95% CIs. Cox proportional hazard methods were used to calculate the relative difference between treatment groups (hazard ratio, HR) and 95% CIs with endarterectomy as the reference group. Log-rank tests were used to compare the two survival curves.
The 30-day per-protocol analysis of the procedural risk included only patients in whom the allocated treatment was initiated as their first ipsilateral revascularisation procedure. Patients who received the alternative revascularisation procedure as their first treatment (cross-overs), or who received no revascularisation treatment were excluded from this analysis. All outcome events occurring within 30 days after initiation of the first allocated treatment were included. We included every patient in whom the allocated treatment was initiated in the per-protocol analysis, even if the date of treatment was more than 120 days after randomisation, or if the treatment was aborted after initiation. This per-protocol analysis therefore compared the 30-day procedural risks of the two treatments in those patients in whom the allocated procedure was completed or initiated. Binomial regression methods were used to estimate the 30-day absolute risk differences and relative risk ratios together with 95% CIs. χ2 tests were used to test for differences between the two treatment groups.
Several predefined exploratory subgroup analyses were undertaken to investigate whether the relative treatment effect for the 120-day ITT short-term composite outcome of stroke, death, or procedural myocardial infarction differed across various patient groups. Interaction tests were done with Cox proportional hazard models. All analyses were done with Stata release 11, apart from the meta-analysis, which was done with ReviewManager version 5.0. This study is registered, number ISRCTN25337470.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or the writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
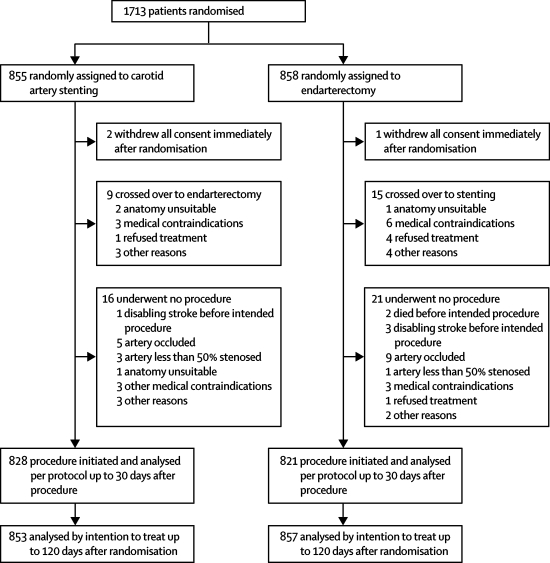
Figure 1 shows the trial profile. Between May, 2001, and October, 2008, 1713 patients from 50 academic centres in Europe, Australia, New Zealand, and Canada were enrolled and randomised. Three patients (stenting group, two; endarterectomy group, one) withdrew consent immediately after randomisation and were excluded from the ITT analysis. 751 (88%) of 853 patients assigned to carotid stenting and 760 (89%) of 857 patients assigned to endarterectomy were randomised at centres classified as experienced. Table 1 shows baseline characteristics of study participants.
Figure 1.
Trial profile
Data for the number of patients screened for eligibility were not recorded.
Table 1.
Baseline characteristics of patients
| Stenting group (n=853) | Endarterectomy group (n=857) | ||
|---|---|---|---|
| Age (years) | 70 (9) | 70 (9) | |
| Sex (male) | 601 (70%) | 606 (71%) | |
| Vascular risk factors | |||
| Treated hypertension | 587 (69%) | 595 (69%) | |
| Systolic blood pressure (mm Hg) | 147 (24) | 146 (24) | |
| Diastolic blood pressure (mm Hg) | 79 (12) | 78 (13) | |
| Cardiac failure | 23 (3%) | 47 (5%) | |
| Angina in past 6 months | 83 (10%) | 77 (9%) | |
| Previous myocardial infarction | 151 (18%) | 156 (18%) | |
| Previous CABG | 109 (13%) | 116 (14%) | |
| Atrial fibrillation | 57 (7%) | 59 (7%) | |
| Other cardiac embolic source | 19 (2%) | 16 (2%) | |
| Type 2 diabetes mellitus | 134 (16%) | 147 (17%) | |
| Type 1 diabetes mellitus | 50 (6%) | 40 (5%) | |
| Peripheral artery disease | 139 (16%) | 136 (16%) | |
| Current smoker | 205 (24%) | 198 (23%) | |
| Ex-smoker | 408 (48%) | 424 (49%) | |
| Treated hyperlipidaemia | 522 (61%) | 562 (66%) | |
| Cholesterol (mmol/L) | 4·8 (1·3) | 4·9 (1·3) | |
| Degree of symptomatic carotid stenosis* | |||
| 50–69% | 92 (11%) | 76 (9%) | |
| 70–99% | 761 (89%) | 781 (91%) | |
| Degree of contralateral stenosis* | |||
| <50% | 565 (66%) | 561 (65%) | |
| 50–69% | 128 (15%) | 142 (17%) | |
| 70–99% | 105 (12%) | 110 (13%) | |
| Occluded | 49 (6%) | 37 (4%) | |
| Unknown | 6 (1%) | 7 (1%) | |
| Most recent ipsilateral event† | |||
| Amaurosis fugax | 148 (17%) | 142 (17%) | |
| Transient ischaemic attack | 273 (32%) | 303 (35%) | |
| Ischaemic hemispheric stroke | 393 (46%) | 376 (44%) | |
| Retinal infarction | 26 (3%) | 23 (3%) | |
| Unknown | 13 (2%) | 13 (2%) | |
| Event <6 months before randomisation | 826 (97%) | 816 (95%) | |
| Event 6–12 months before randomisation‡ | 27 (3%) | 36 (4%) | |
| Multiple ipsilateral symptoms before randomisation | 330 (39%) | 317 (37%) | |
| Ipsilateral stroke before most recent ipsilateral event | 131 (15%) | 106 (12%) | |
| Modified Rankin score at randomisation | |||
| 0–2 | 756 (89%) | 744 (87%) | |
| 3–5§ | 81 (9%) | 99 (12%) | |
| Unknown | 16 (2%) | 14 (2%) | |
Data are number (%) or mean (SD). CABG=coronary artery bypass graft.
Degree of stenosis measured by North American Symptomatic Carotid Endarterectomy Trial2 method at randomisation centre.
If two events were reported on the same day, the more serious of the two was counted (stroke>retinal infarction>transient ischaemic attack>amaurosis fugax).
In three patients the event was more than 12 months before randomisation and in two the date was unknown.
Some Rankin scores of 3 or more were caused by non-stroke disability.
Most patients had their allocated treatment initiated (stenting group, n=828; endarterectomy group, n=821). Nine patients allocated to stenting crossed over to surgery without an attempt at the procedure and a further 16 had no attempted ipsilateral endarterectomy or stenting procedure (figure 1). 15 patients allocated to endarterectomy crossed over to stenting without an attempt at endarterectomy and 21 had no attempted ipsilateral procedure.
Monitoring of adverse events led to concern about the stenting results of two investigators at supervised centres. These investigators were stopped from treating further patients within the trial and their centres were suspended from randomisation. All the patients allocated to stenting (n=11, five with disabling stroke or death) or endarterectomy during the same time period (n=9, one with fatal stroke) at these centres were included in the analyses. One of the two centres subsequently restarted randomisation with a different investigator performing stenting.
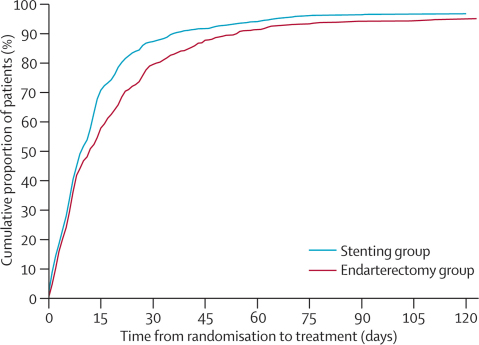
Figure 2 shows the delay from randomisation to first initiated ipsilateral treatment in the per-protocol analysis. Median delay from randomisation to treatment was shorter in the stenting group than in the endarterectomy group, as was the delay from most recent ipsilateral event to treatment (table 2).
Figure 2.
Time between randomisation and treatment
Cumulative number of patients in whom allocated treatment was initiated per protocol plotted as a proportion of the total number randomised in each group (vertical axis), against the delay between the dates of randomisation and treatment (horizontal axis). Only allocated per-protocol treatment dates were counted.
Table 2.
Time from randomisation and from most recent ipsilateral event to allocated treatment
| Stenting group (n=828) | Endarterectomy group (n=821) | p value* | ||
|---|---|---|---|---|
| Time from randomisation to treatment (days) | 9 (5–17) | 11 (5–24) | <0·0001 | |
| ≤14 | 578 (70%) | 469 (57%) | .. | |
| >14 | 250 (30%) | 352 (43%) | .. | |
| Time from most recent event to treatment (days) | 35 (15–82) | 40 (18–87) | 0·013 | |
| ≤14 | 205 (25%) | 151 (18%) | .. | |
| >14 | 623 (75%) | 668 (81%) | .. | |
Data are number (%) or median (IQR) in the per-protocol analysis. Three patients in the endarterectomy group were randomised more than 12 months after onset of symptoms. The date of the most recent event was unknown in two patients (endarterectomy group).
Mann-Whitney U test.
Of the 828 patients in whom stenting was initiated as allocated, 64 (8%) had their procedure aborted before the insertion of a stent (38 procedures were aborted because of difficulty gaining access to the stenosis, 15 were aborted because of the finding of an occluded artery, one patient had a fatal stroke, one patient had fatal myocardial infarction before completion of treatment, two had other medical complications, and further investigation in seven patients showed the artery to be <50% stenosed). Of the 62 patients whose stenting procedure was aborted after initiation and who did not have a fatal event, 37 went on to have an ipsilateral endarterectomy, whereas 25 continued with best medical care only. Only two of the 821 patients whose allocated endarterectomy was initiated had their procedure aborted (one patient had an allergic reaction during general anaesthesia; the other became distressed and the endarterectomy had to be abandoned). Both patients subsequently had ipsilateral stenting.
The following stents were each used in 10% or more of the 764 patients in whom stents were inserted: Carotid Wallstent (Boston Scientific), Precision (Cordis), and Protégé (EV3). The following were each used in less than 10% of patients: Acculink (Guidant), Xact (Abbott), Smart (Cordis), Cristallo Ideale (Invatec), Exponent (Medtronic), Next Stent (Boston Scientific). Protection devices were known to have been used in 593 (72%) of 828 patients. The following protection devices were each used in 10% or more of the patients in whom stenting was attempted: FilterWire EZ (Boston Scientific), Angioguard (Cordis), Spider FX (EV3), and Emboshield (Abbott). A range of other protection devices were each used in less than 5% of patients. In 27 patients, it was not clear whether or not a protection device was used.
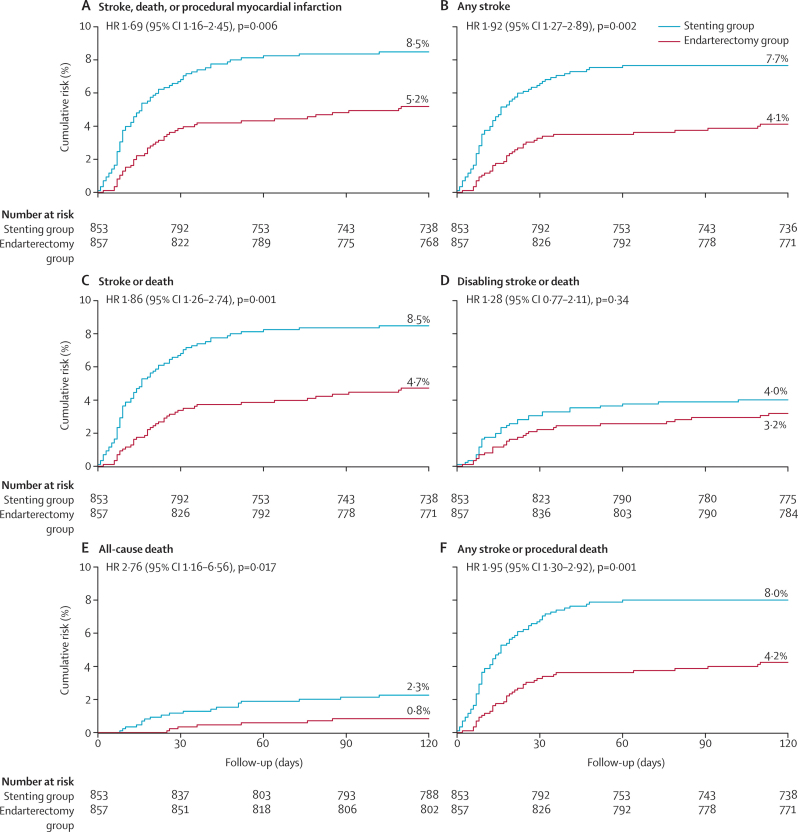
In the ITT analysis, between randomisation and 120 days, there was no significant difference in the rate of disabling stroke or death between groups (stenting group, 4·0% vs endarterectomy group, 3·2%; table 3).
Table 3.
Outcome measures within 120 days of randomisation (intention-to-treat population)
| Stenting group (n=853) | Endarterectomy group (n=857) | Hazard ratio (95% CI) | Risk difference, % (95% CI) | p value* | |
|---|---|---|---|---|---|
| Stroke, death or procedural myocardial infarction | 72 (8·5%) | 44 (5·2%) | 1·69 (1·16 to 2·45) | 3·3% (0·9 to 5·7) | 0·006 |
| Any stroke | 65 (7·7%) | 35 (4·1%) | 1·92 (1·27 to 2·89) | 3·5% (1·3 to 5·8) | 0·002 |
| Any stroke or death | 72 (8·5%) | 40 (4·7%) | 1·86 (1·26 to 2·74) | 3·8% (1·4 to 6·1) | 0·001 |
| Any stroke or procedural death | 68 (8·0%) | 36 (4·2%) | 1·95 (1·30 to 2·92) | 3·8% (1·5 to 6·0) | 0·001 |
| Disabling stroke or death | 34 (4·0%) | 27 (3·2%) | 1·28 (0·77 to 2·11) | 0·8% (−0·9 to 2·6) | 0·34 |
| All-cause death | 19 (2·3%) | 7 (0·8%) | 2·76 (1·16 to 6·56) | 1·4% (0·3 to 2·6) | 0·017 |
Data are number of first events (Kaplan-Meier estimate at 120 days). Risk differences are calculated from Kaplan-Meier estimates at 120 days.
Log-rank test.
The risk of stroke, death, or procedural myocardial infarction 120 days after randomisation was significantly higher in patients in the stenting group than in patients in the endarterectomy group (8·5% vs 5·2%), representing an estimated 120-day absolute risk difference of 3·3% (95% CI 0·9–5·7) with an HR in favour of surgery of 1·69 (1·16–2·45, log-rank p=0·006; figure 3, table 3). Most outcome events in the stent and endarterectomy groups occurred within 30 days of the first ipsilateral procedure (61 of 72 events vs 31 of 44 events). A few events occurred after randomisation but before the date of treatment (two patients vs one patient), or in patients who had no attempted ipsilateral procedure (three patients vs six patients), or more than 30 days after treatment but within 120 days of randomisation (six patients vs six patients).
Figure 3.
Kaplan-Meier estimates of cumulative incidence of various outcome measures
Data were analysed by intention to treat. The numbers above the end of the lines are the incidence estimates at 120 days after randomisation. HR=hazard ratio.
Compared with endarterectomy, allocation to stenting had a greater 120-day risk of the outcome measures of any stroke, any stroke or death, any stroke or procedural death, and all-cause death (table 3). Most strokes within 120 days of randomisation were ipsilateral to the treated carotid artery and most were ischaemic (table 4). There were very few haemorrhagic strokes with only two patients in whom the cause of the stroke was uncertain. The observed treatment effect was largely driven by the higher number of non-disabling strokes in the stenting group, most of which had symptoms lasting for more than 7 days. There was an excess of fatal strokes in the stenting group compared with the surgery group, but little difference in the number of patients with disabling stroke within 120 days of randomisation.
Table 4.
Number of outcome events between randomisation and 120 days in the intention-to-treat (ITT) analysis and between initiation of treatment and 30 days after treatment in the per-protocol analysis
|
ITT analysis (events up to 120 days after randomisation) |
Per-protocol analysis (events between 0 days and 30 days after treatment) | |||||
|---|---|---|---|---|---|---|
| Stenting group (n=853) | Endarterectomy group (n=857) | Stenting group (n=828) | Endarterectomy group (n=821) | |||
| Any stroke | 65* | 35 | 58* | 27 | ||
| Ipsilateral stroke | 58 | 30 | 52 | 25 | ||
| Ischaemic stroke | 63 | 28 | 56 | 21 | ||
| Haemorrhagic stroke | 3 | 5 | 2 | 5 | ||
| Uncertain cause | 0 | 2 | 0 | 1 | ||
| Non-disabling stroke | 39 | 14 | 36 | 11 | ||
| Lasting fewer than 7 days | 9† | 5‡ | 8† | 5‡ | ||
| Lasting more than 7 days | 31 | 9 | 29 | 6 | ||
| Disabling stroke | 17§ | 20 | 14 | 14 | ||
| Fatal stroke | 9 | 2 | 8 | 3 | ||
| Procedural myocardial infarction | 3 | 4 | 3 | 5 | ||
| Non-fatal myocardial infarction | 0 | 4 | 0 | 5¶ | ||
| Fatal myocardial infarction | 3 | 0 | 3 | 0 | ||
| Death unrelated to stroke or myocardial infarction | 7 | 5 | 1 | 1 | ||
| Cranial nerve palsy | 1‖ | 45 | 1‖ | 45 | ||
| Disabling cranial nerve palsy | 1‖ | 1 | 1‖ | 1 | ||
| Haematoma | 31 | 50 | 30 | 50 | ||
| Severe haematoma** | 9 | 28 | 8 | 28 | ||
Data are number of first events of each type. See text for definition of per protocol.
In two patients this was a retinal infarction. One patient had both an ischaemic and a haemorrhagic stroke.
One patient had a subsequent fatal myocardial infarction and one patient also had a non-disabling stroke that lasted for more than 7 days.
One patient had a subsequent disabling stroke.
Two patients subsequently died of a cause unrelated to stroke or myocardial infarction.
One patient had a non-fatal myocardial infarction within 30 days of the first procedure, which was undertaken more than 120 days after randomisation. This myocardial infarction was therefore excluded from the ITT analysis (which stopped at 120 days) but was included in the per-protocol 30-day analysis that included all first ipsilateral allocated procedures.
The cranial nerve palsy in this patient in the stenting group, which was initiated but aborted, occurred after endarterectomy done within 30 days of the stenting procedure.
Severe haematoma was defined as one that required surgical evacuation or blood transfusion, or resulted in extended hospital stay.
The per-protocol analysis included 1649 patients (stenting group, n=828; endarterectomy group, n=821). Results for 30-day procedural risk mirrored the results of the intention-to-treat analysis. Risk of stroke, death, or procedural myocardial infarction was higher in the stenting group than in the endarterectomy group (30-day risk 7·4% vs 4·0%; risk difference [RD] 3·3%, 95% CI 1·1–5·6; risk ratio [RR] 1·83, 1·21–2·77, χ2 p=0·003; table 5). Risk of any stroke or death up to 30 days after treatment remained significantly higher in patients in whom stenting was initiated than in patients with surgery initiated, but there was no significant difference in the risk of disabling stroke or death between treatment groups. There were more fatal strokes in the stenting group than in the endarterectomy group (eight vs three), but difference in the risk of death alone was no longer significant (table 5). 43 (74%) of 58 strokes in the stenting group and 12 (44%) of 27 in the endarterectomy group occurred on the day of the procedure.
Table 5.
Outcome measures between initiation of treatment and 30 days after treatment (per-protocol analysis)
| Stenting group (n=828) | Endarterectomy group (n=821) | Risk ratio (95% CI) | Risk difference, % (95% CI) | p value* | |
|---|---|---|---|---|---|
| Stroke, death, or myocardial infarction | 61 (7·4%) | 33 (4·0%) | 1·83 (1·21 to 2·77) | 3·3% (1·1 to 5·6) | 0·003 |
| Any stroke | 58 (7·0%) | 27 (3·3%) | 2·13 (1·36 to 3·33) | 3·7% (1·6 to 5·8) | 0·001 |
| Any stroke or death | 61 (7·4%) | 28 (3·4%) | 2·16 (1·40 to 3·34) | 4·0% (1·8 to 6·1) | 0·0004 |
| Disabling stroke or death | 26 (3·1%) | 18 (2·2%) | 1·43 (0·79 to 2·59) | 0·9% (−0·6 to 2·5) | 0·23 |
| Procedural death | 11† (1·3%) | 4 (0·5%) | 2·73 (0·87 to 8·53) | 0·8% (−0·1 to 1·8) | 0·072 |
Data are number of first events (%). See text for definition of per protocol.
χ2 test.
One patient had a fatal stroke but died more than 30 days after the procedure. The event is therefore counted in the fatal stroke outcome but not in the procedural death outcome.
Few procedural myocardial infarctions were recorded (three in the stenting group, all of which were fatal, compared with five in the endarterectomy group). Cranial nerve palsies were almost completely avoided by stenting (table 4; RR 0·02, 95% CI 0·00–0·16, p<0·0001). The one cranial nerve palsy recorded in the stenting group occurred as a complication of an endarterectomy done within 30 days of stenting. This patient and one additional patient in the endarterectomy group required percutaneous endoscopic gastrostomy feeding as a result of the cranial nerve palsies, which were classified as disabling. There were also fewer haematomas of any severity in the stenting group than in the endarterectomy group (table 4; RR 0·59, 0·38–0·93, p=0·0197), and fewer severe haematomas requiring surgical intervention, blood transfusion, or extended hospital stay (table 4; RR 0·28, 0·13–0·62, p=0·0007).
A post-hoc sensitivity analysis was undertaken to examine if the results of the per-protocol analysis were affected by inclusion of patients in whom the allocated procedure was initiated but not completed. Exclusion of the 64 patients allocated to stenting and two patients allocated to endarterectomy in whom the procedures were aborted after initiation—ie, including only patients in whom the allocated procedure was completed as planned—made little difference to the results (30-day risk of stroke, death, or procedural myocardial infarction 7·6% in the stenting group vs 4·0% in the endarterectomy group; RD 3·6%, 95% CI 1·3–5·9; RR 1·88, 1·24–2·86, p=0·002).
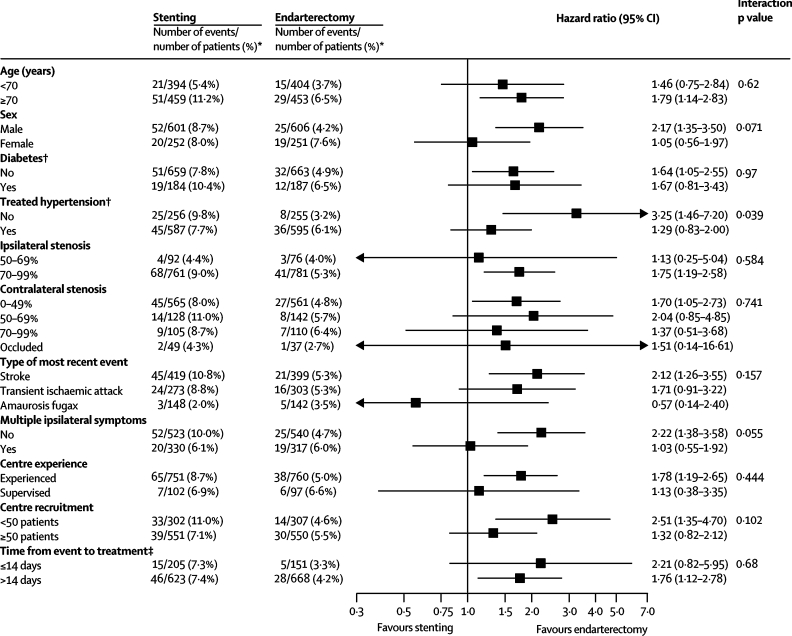
We undertook exploratory analyses of the composite outcome of stroke, death, or procedural myocardial infarction for predefined subgroups (figure 4). These analyses suggested that carotid stenting might have a similar risk to endarterectomy in women, but that the intervention was more hazardous than endarterectomy in men. The difference was mainly caused by a higher risk of stroke, death, or procedural myocardial infarction in women assigned to endarterectomy than in men (7·6% vs 4·2%). However, the difference between the hazard ratios comparing the risk of stenting with endarterectomy in men and women only reached borderline significance (interaction p=0·071). Stenting was more hazardous, and endarterectomy less hazardous, in patients without treated hypertension at baseline than in patients with treated hypertension (figure 4).
Figure 4.
Subgroup analysis to compare the rates of stroke, death, or procedural myocardial infarction in different subgroups
Subgroups are defined according to baseline characteristics and analysed by intention to treat up to 120 days after randomisation, apart from time from event to treatment, which is analysed per protocol. p values are associated with treatment-covariate interaction tests. *Data are number of events of first stroke, death, or procedural myocardial infarction within 120 days of randomisation/number of patients (Kaplan-Meier estimate at 120 days). †Patients with missing information were excluded from the analysis. ‡Time from the most recent ipsilateral event before randomisation to the date of treatment, analysed per protocol for 30-day procedural events only (results are relative risk and 95% CI at 30 days after treatment).
There was also a suggestion that patients allocated to the stenting group had a similar risk of stroke, death, or procedural myocardial infarction to those allocated to endarterectomy after multiple ipsilateral symptoms, but compared with patients with only one event before randomisation, the difference in the hazard ratios only reached borderline significance (interaction p=0·055). There was no evidence that the relative increase in the hazard of an event in the stenting group compared with the endarterectomy group differed significantly across any other subgroups.
Discussion
Short-term results from this randomised controlled trial show that carotid endarterectomy is safer than carotid stenting for treatment of patients with symptomatic carotid artery stenosis. Patients allocated to stenting had a 3·3% higher risk of stroke, death, or procedural myocardial infarction within 120 days of randomisation in the ITT analysis. In the per-protocol analysis, the rate of any stroke or death within 30 days of treatment in the stenting group was more than twice the rate recorded in the endarterectomy group. The difference between groups in the per-protocol analysis was mainly attributable to an excess of non-disabling stroke in the stenting group compared with the endarterectomy group, but there were also more fatal strokes and fatal myocardial infarctions in the stenting group. By contrast, the numbers of disabling strokes in the two groups were identical and the rate of disabling stroke or death was not significantly different between groups.
Most strokes within 30 days of treatment were ipsilateral to the treated artery and most were ischaemic. Despite the recommended use of combined antiplatelet therapy with aspirin and clopidogrel before stenting and for 1 month afterwards, plus use of heparin during the procedure, there were only two haemorrhagic strokes within 30 days of stenting compared with five after endarterectomy, suggesting that dual antiplatelet therapy in this setting is safe. However, this antithrombotic regimen did not reduce ischaemic stroke sufficiently in the stenting group.
The balance of risk in favour of surgery caused by an excess of non-disabling stroke in the stenting group might be seen as partly offset by the fact that endarterectomy was associated with more cranial nerve injuries and more severe haematomas than was stenting. However, the long-term outcome of non-disabling stroke might be worse than that of non-disabling cranial nerve palsy. A recent systematic review has highlighted the increased risk of dementia associated with recurrent stroke10 and the long-term consequences of the non-disabling strokes in our study might only become evident with further follow-up, which will include measures of disability and quality of life.
Patients who received a stent had a shorter wait from most recent stroke or transient ischaemic attack to treatment than did those who received endarterectomy, but even so only 25% of patients in the stenting group were treated within 14 days of symptoms, compared with 18% of those in the endarterectomy group. However, there was no difference in the risks of stenting compared with endarterectomy whether or not patients were treated within 14 days of symptoms or later. Several strokes occurred before treatment was initiated (five vs seven) and several patients developed asymptomatic carotid artery occlusion before treatment (five vs nine), emphasising the importance of treating carotid stenosis as soon as possible after symptoms.
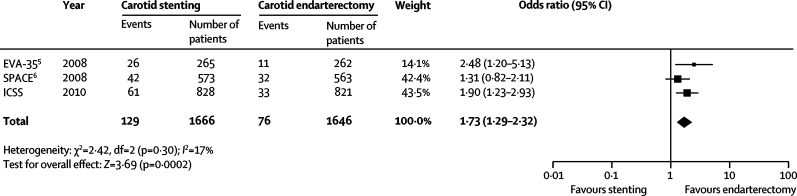
The results of our study are consistent with those seen in previous randomised trials.11 A new analysis of events occurring within 30 days of treatment in CAVATAS also showed an excess of minor strokes in patients assigned to endovascular treatment compared with those assigned to endarterectomy, with no difference in rates of disabling stroke or death.12 CAVATAS used outdated techniques and few patients had stents inserted. The first multicentre randomised trial of carotid stenting with modern devices designed for the carotid artery, the Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy (SAPPHIRE) trial, mostly recruited patients with asymptomatic stenosis at high risk for endarterectomy.13 Therefore, the trial's findings, which suggested that stenting was not inferior to endarterectomy, cannot be directly compared with our results. The EVA-3S and SPACE trials recruited only symptomatic patients and had similar protocols to our trial.5,6 We have therefore combined the published 30-day safety data from EVA-3S, SPACE, and ICSS in a meta-analysis (figure 5). The summary statistic strongly favours carotid endarterectomy (odds ratio for stroke, death, or myocardial infarction within 30 days after the procedure 1·73, 95% CI 1·29–2·32). One further large randomised trial, the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST), has completed recruitment, but has not yet published any safety data.14
Figure 5.
Meta-analysis comparing safety of carotid artery stenting with endarterectomy in the recent carotid stenting trials
Odds ratio for any stroke, death, or procedural myocardial infarction within 30 days of treatment in the three recent trials of carotid artery stenting versus endarterectomy including only symptomatic patients. Analysis is based on published results of per-protocol data. The large diamond represents the odds ratio and 95% CI of the combined data. The summary estimate statistic was calculated by use of a Mantel-Haenszel fixed-effect model; the centre of the diamond is the point estimate, and its width the 95% CI. EVA-3S=Endarterectomy versus Stenting in Patients with Symptomatic Severe Carotid Stenosis. SPACE=Stent-Protected Angioplasty versus Carotid Endarterectomy. ICSS=International Carotid Stenting Study.
Since CAVATAS was completed, there has been a reduction in risk of adverse outcomes associated with endovascular treatment, but the risk associated with endarterectomy has reduced to a greater extent. The risk of stroke, death, or procedural myocardial infarction in the stenting group of our trial is similar to the risk associated with carotid endarterectomy that was reported in the European Carotid Surgery Trial (ECST) in 1998.1 By contrast, the risk of stroke, death, or procedural myocardial infarction after endarterectomy in our trial and in EVA-3S was approximately half that reported in ECST. This reduction in risk probably reflects improved anaesthetic and surgical techniques, and improved medical treatment before surgery. The low rate of myocardial infarction in our trial is consistent with improved medical treatment before surgery.
Our results are applicable to the current practice of carotid stenting at most vascular centres. The participating centres were representative of academic centres with substantial experience of treating carotid stenosis and needed to show a high standard of practice before they could join the trial. Our results could be criticised in that the experience of the interventionists in carotid stenting was less than that of the surgeons in carotid endarterectomy. However, the risk of outcome events associated with stenting was lower in inexperienced, supervised centres than in more experienced centres (figure 4) and there was no significant difference in the excess hazard of stenting compared with endarterectomy between supervised and experienced centres or between centres recruiting more or less than 50 patients; therefore, inexperience cannot explain our results. The EVA-3S trial also showed no differences in the outcomes favouring endarterectomy related to the experience of the interventionists or the number of procedures done within the trial.5
There are several possible explanations for the excess of non-disabling stroke seen in the stenting group compared with the endarterectomy group. Investigators who undertook follow-up assessments were not masked to treatment allocation, leading to the possibility of ascertainment bias of minor events. A post-analysis audit has confirmed that all but 77 patients were seen for follow-up by a neurologist or stroke physician, or by research nurses or practitioners supervised by a neurologist, not directly involved in the revascularisation procedures. A sensitivity analysis excluding the 77 patients seen for follow-up by a surgeon only, provided similar results to those of the full analysis (data not shown), making it unlikely that biased reporting affected the results. We were concerned that some short-lived events might be missed in surgical patients operated on under general anaesthesia and returned to surgical wards, whereas these events might not be missed in endovascular patients treated under local anaesthesia. However, this hypothesis is an unlikely explanation of our results, since most of the excess non-disabling strokes associated with stents lasted for more than 7 days. The conclusion that the excess in non-disabling stroke cannot be explained by bias is supported by the results of a blinded MRI subanalysis of this trial.15 This subanalysis showed a significantly higher proportion of patients with new ischaemic lesions on MRI in the stenting group than in the endarterectomy group (50% vs 17%, adjusted odds ratio 5·21, 95% CI 2·78–9·79, p<0·0001).
The most likely explanation for the excess risk of non-disabling stroke associated with stenting is that it is related to instrumentation of the carotid stenosis, given that most strokes occurred on the day of treatment. Selection of patients could be important in keeping the risks of instrumentation to a minimum. Future analyses of our trial will investigate anatomical and clinical risk factors for procedural stroke, as well as the effects of stent design and protection devices.
Our exploratory analyses suggested that carotid stenting might have a similar risk to endarterectomy in women, but that the intervention was more hazardous than endarterectomy in men. However, the difference between the hazard ratios comparing stenting with endarterectomy in women and men did not reach statistical significance. The difference seemed to be largely explained by a higher risk of outcome events associated with endarterectomy in women than in men. The increased risk associated with endarterectomy in women is a consistent feature of most large studies and was also seen in the EVA-3S trial,8 in the pooled analysis of the major carotid endarterectomy trials,16 and in a systematic review of the published series.17 Stenting seemed to be more hazardous, and endarterectomy less hazardous, in patients without treated hypertension at baseline than in patients with treated hypertension, but the reasons remain unclear. However, a systematic review of predictors of stroke and death caused by carotid endarterectomy showed a similar increase in risk of stroke or death associated with hypertension (HR 1·82, 95% CI 1·37–2·41, p<0·0001) in accordance with our findings.18
Our results suggest that carotid endarterectomy should remain the treatment of choice for symptomatic patients with severe carotid stenosis suitable for surgery. Most patients had no complications from either procedure. Thus, some patients might still opt for stenting after being presented with the available evidence, especially if they have a strong preference for avoiding surgery. Since outcomes in the stenting group were similar to those reported after carotid endarterectomy in previous trials that compared surgery with best medical treatment alone, stenting is also likely to be better than no revascularisation in patients unwilling or unable to have surgery because of medical or anatomical contraindications.
The aim of treatment for carotid stenosis is long-term prevention of stroke. The EVA-3S and SPACE studies showed little difference between carotid stenting and endarterectomy groups in the rates of ipsilateral non-perioperative stroke occurring more than 30 days after treatment, but the length of follow-up in these studies was restricted to a maximum of 4 years and 2 years, respectively.7,8 CAVATAS had a longer follow-up period and reported a higher 8-year rate of non-perioperative stroke in patients who received endovascular treatment (21·1%) than in patients who received surgery (15·4%; HR 1·66, 95% CI 0·99–2·80).12 Most of the divergence occurred more than 2 years after randomisation, which might be partly explained by a higher incidence of restenosis after endovascular treatment than after endarterectomy.19 However, CAVATAS included only a small proportion of patients treated by use of a stent, and the long-term rate of restenosis after stent insertion remains uncertain. Follow-up is therefore continuing in ICSS and further data will become available from the trial in due course.
Acknowledgments
Acknowledgments
This study was funded by grants from the Medical Research Council, the Stroke Association, Sanofi-Synthélabo, and the European Union. MMB's Chair in Stroke Medicine is supported by the Reta Lila Weston Trust for Medical Research. JE and RLF are supported by a grant from Medical Research Council. LHB was supported by grants from the Swiss National Science Foundation (PBBSB-116873) and the University of Basel. This work was undertaken at University College London Hospital/University College London, which received a proportion of funding from the Department of Health's National Institute for Health Research Biomedical Research Centres funding scheme.
Contributors
JE wrote the first draft of the manuscript. JD undertook the statistical analyses. RLF maintained the database and undertook database queries. LHB contributed to the analysis. All the authors listed in the writing committee made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; and also contributed to drafting the article or revising it critically for important intellectual content. The committee members and the remaining investigators listed at participating centres made contributions to the conception and design or acquisition of data. MMB had the final responsibility for the analyses and the manuscript content as the chief investigator of ICSS.
International Carotid Stenting Study investigators
Writing committee: Jörg Ederle (Department of Brain Repair and Rehabilitation, UCL Institute of Neurology, University College London, UK) Joanna Dobson (Medical Statistics Unit, Department of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, UK), Roland L Featherstone (Department of Brain Repair and Rehabilitation, UCL Institute of Neurology, University College London, UK), Leo H Bonati (Department of Brain Repair and Rehabilitation, UCL Institute of Neurology, University College London, UK), H Bart van der Worp (Department of Neurology, Rudolf Magnus Institute of Neuroscience, University Medical Centre Utrecht, Netherlands), Gert J de Borst (Department of Vascular Surgery, University Medical Centre Utrecht, Netherlands), T Hauw Lo (Department of Radiology, University Medical Centre Utrecht, Netherlands), Peter Gaines (Sheffield Vascular Institute, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK), Paul J Dorman (Department of Neurology, Newcastle General Hospital, Newcastle upon Tyne, UK), Sumaira Macdonald (Department of Radiology, Freeman Hospital, Newcastle upon Tyne, UK), Philippe A Lyrer (Department of Neurology and Stroke Unit, University Hospital Basel, Basel University, Switzerland), Johanna M Hendriks (Department of Vascular Surgery, Erasmus Medical Center, Rotterdam, Netherlands), Charles McCollum (Cardiovascular Medicine, School of Biomedicine, Manchester Academic Health Science Centre, University of Manchester, Manchester, UK), Paul J Nederkoorn (Department of Neurology, Academic Medical Centre, University of Amsterdam, Netherlands), Martin M Brown (Department of Brain Repair and Rehabilitation, UCL Institute of Neurology, University College London, UK). Steering Committee: A Algra, J Bamford (chair), J Beard, M Bland, A W Bradbury, M M Brown (chief investigator), A Clifton, P Gaines, W Hacke, A Halliday, I Malik, J L Mas, A J McGuire, P Sidhu, G Venables. Credential committee: A Bradbury, M M Brown, A Clifton, P Gaines. Data Monitoring Committee: R Collins, A Molyneux, R Naylor, C Warlow (chair). Outcome Event Adjudication Committee: J M Ferro, D Thomas. Central office staff at UCL Institute of Neurology: L H Bonati, L Coward, J Dobson (trial statistician), J Ederle, R F Featherstone (trial manager), H Tindall, D J H McCabe, A Wallis. Participating centres (number of enrolled patients per centre; local investigators): Australia Austin Health, Heidelberg (46; M Brooks, B Chambers [principal investigator], A Chan, P Chu, D Clark, H Dewey, G Donnan, G Fell, M Hoare, M Molan, A Roberts, N Roberts). Box Hill Hospital (Monash University), Melbourne (25; B Beiles, C Bladin [principal investigator], C Clifford, G Fell, M Grigg, G New). Monash Medical Centre, Clayton (26; R Bell, S Bower, W Chong, M Holt, A Saunder, P G Than [principal investigator]). Princess Alexandra Hospital, Brisbane (48; S Gett, D Leggett, T McGahan [principal investigator], J Quinn, M Ray, A Wong, P Woodruff). Repatriation General Hospital, Daw Park, Adelaide (6; R Foreman, D Schultz [principal investigator], R Scroop, B Stanley). Royal Melbourne Hospital, Melbourne (57; B Allard, N Atkinson, W Cambell, S Davies [principal investigator], P Field, P Milne, P Mitchell, B Tress, B Yan). Royal Hobart Hospital, Hobart (18; A Beasley, D Dunbabin, D Stary, S Walker [principal investigator]). Belgium Antwerp University Hospital, Antwerp (10; P Cras, O d'Archambeau, J M H Hendriks [principal investigator], P Van Schil). A Z St Blasius, Dendermonde (5; M Bosiers [principal investigator], K Deloose, E van Buggenhout). A Z Sint Jan Brugge-Oostende, Campus Brugge, Brugges (18; J De Letter, V Devos, J Ghekiere, G Vanhooren [principal investigator]). Cliniques Universitaires St Luc, Bruxelles (1; P Astarci, F Hammer, V Lacroix, A Peeters [principal investigator], R Verhelst). Imelda Ziekenhuis, Bonheiden (3; L DeJaegher [principal investigator], A Peeters, J Verbist). Canada CHUM Notre-Dame Hospital, Montreal (30; J-F Blair, J L Caron, N Daneault, M-F Giroux, F Guilbert, S Lanthier, L-H Lebrun, V Oliva, J Raymond, D Roy [principal investigator], G Soulez, A Weill). Foothills Medical Centre, Calgary (4; M Hill [principal investigator], W Hu, M Hudion, W Morrish, G Sutherland, J Wong). Finland Helsinki University Central Hospital, Helsinki (33; A Albäck, H Harno, P Ijäs, M Kaste [principal investigator], M Lepäntalo, S Mustanoja, T Paananen, M Porras, J Putaala, M Railo, T Sairanen, L Soinne, A Vehmas, P Vikatmaa). Germany Otto von Guericke University, Magdeburg (9; M Goertler [principal investigator], Z Halloul, M Skalej). Ireland Beaumont Hospital, Dublin (4; P Brennan, C Kelly, A Leahy, J Moroney [principal investigator], J Thornton). Netherlands Academic Medical Centre, Amsterdam (56; M J W Koelemay, P J Nederkoorn [principal investigator], J A A Reekers, Y B W E M Roos). Erasmus Medical Centre, Rotterdam (75; J M Hendriks, P J Koudstaal [principal investigator], P M T Pattynama, A van der Lugt, L C van Dijk, M R H M van Sambeek, H van Urk, H J M Verhagen). Haga Teaching Hospitals, The Hague (45; C M A Bruijninckx, S F de Bruijn, R Keunen, B Knippenberg, A Mosch [principal investigator], F Treurniet, L van Dijk, H van Overhagen, J Wever). Isala Klinieken, Zwolle (14; F C de Beer, J S P van den Berg [principal investigator], B A A M van Hasselt, D J Zeilstra). Medical Centre Haaglanden, The Hague (3; J Boiten [principal investigator], J C A de Mol van Otterloo, A C de Vries, G J Lycklama a Nijeholt, B F W van der Kallen). UMC St Radboud, Nijmegen (13; J D Blankensteijn, F E De Leeuw, L J Schultze Kool [principal investigator], J A van der Vliet). University Medical Centre, Utrecht (270; G J de Borst, G A P de Kort, L J Kapelle [principal investigator], T H Lo, W P Th M Mali, F Moll, HB van der Worp, H Verhagen). New Zealand Auckland City Hospital, Auckland (40; P A Barber, R Bourchier, A Hill, A Holden, J Stewart [principal investigator]). Norway Rikshospitalet University Hospital, Oslo (16; S J Bakke [principal investigator], K Krohg-Sørensen, M Skjelland, B Tennøe). Poland Institute of Psychiatry and Neurology (2nd Department of Neurology & Department of Neuroradiology) and Medical University of Warsaw (2nd Department of General, Vascular and Oncological Surgery), Warsaw (20; P Bialek, Z Biejat, W Czepiel, A Czlonkowska [principal investigator], A Dowzenko, J Jedrzejewska, A Kobayashi, M Lelek, J Polanski). Slovenia University Medical Centre, Ljubljana (12; J Kirbis, Z Milosevic, B Zvan [principal investigator]). Spain Hospital Clinic, Barcelona (18; J Blasco, A Chamorro [principal investigator], J Macho, V Obach, V Riambau, L San Roman). Parc Taulí Sabadell Hospital, Barcelona (33; J Branera, D Canovas [principal investigator], Jordi Estela, A Gimenez Gaibar, J Perendreu). Sweden Malmö University Hospital, Malmö (67; K Björses, A Gottsater [principal investigator], K Ivancev, T Maetzsch, B Sonesson). Sodersjukhuset, Stockholm (55; B Berg, M Delle, J Formgren, P Gillgren, T-B Kall, P Konrad [principal investigator], N Nyman, R Takolander). The Karolinska Institute, Stockholm (5; T Andersson, J Malmstedt, M Soderman, C Wahlgren, N Wahlgren [principal investigator]). Switzerland Centre Hospitalier Universitaire Vaudois, Lausanne (12; S Binaghi, L Hirt, P Michel [principal investigator], P Ruchat). University Hospital Basel, Basel (94; L H Bonati, S T Engelter, F Fluri, L Guerke, A L Jacob, E Kirsch, P A Lyrer [principal investigator], E-W Radue, P Stierli, M Wasner, S Wetzel). University Hospital of Geneva, Geneva (16; C Bonvin, A Kalangos, K Lovblad, N Murith, D Ruefenacht, R Sztajzel [principal investigator]). UK Addenbrookes Hospital, Cambridge (5; N Higgins, P J Kirkpatrick, P Martin [principal investigator]). K Varty Birmingham Heartlands Hospital, Birmingham (11; D Adam, J Bell, A W Bradbury, P Crowe, M Gannon, M J Henderson, D Sandler, R A Shinton [principal investigator], J M Scriven, T Wilmink). Lancashire Teaching Hospitals NHS Trust, Preston (2; S D'Souza, A Egun, R Guta, S Punekar, D M Seriki [principal investigator], G Thomson). Liverpool Royal Infirmary (21) and the Walton Centre, Liverpool (7; J A Brennan, T P Enevoldson, G Gilling-Smith [principal investigator], D A Gould, P L Harris, R G McWilliams, H-C Nasser, R White). Manchester Royal Infirmary, Manchester (2; K G Prakash, F Serracino-Inglott, G Subramanian [principal investigator], J V Symth, M G Walker). Newcastle Acute Hospitals NHS Foundation Trust, Newcastle upon Tyne (108; M Clarke, M Davis, S A Dixit, P Dorman [principal investigator], A Dyker, G Ford, A Golkar, R Jackson, V Jayakrishnan, D Lambert, T Lees, S Louw, S Macdonald, A D Mendelow, H Rodgers, J Rose, G Stansby, M Wyatt). North Bristol NHS Trust, Frenchay Hospital, Bristol (13; T Baker, N Baldwin [principal investigator], L Jones, D Mitchell, E Munro, M Thornton). Royal Free Hospital, London (1; D Baker, N Davis, G Hamilton [principal investigator], D McCabe, A Platts, J Tibballs). Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield (151; J Beard, T Cleveland, D Dodd, P Gaines, R Lonsdale, R Nair, A Nassef, S Nawaz, G Venables [principal investigator]). St George's University of London and St George's NHS Healthcare Trust, London (58; A Belli, A Clifton, G Cloud, A Halliday, H Markus [principal investigator], R McFarland, R Morgan, A Pereira, A Thompson). St Mary's Hospital, Imperial College Healthcare NHS Trust, London (13; J Chataway [principal investigator], N Cheshire, R Gibbs, M Hammady, M Jenkins, I Malik, J Wolfe). University College London Hospitals NHS FoundationTrust, London (51; M Adiseshiah, C Bishop, S Brew, J Brookes, M M Brown [principal investigator], R Jäger, N Kitchen). University Hospital of South Manchester, Wythenshawe, Manchester (58; R Ashleigh, S Butterfield, G E Gamble, C McCollum [principal investigator], A Nasim, P O'Neill, J Wong). Western Infirmary, Glasgow (5; R D Edwards, K R Lees, A J MacKay, J Moss [principal investigator], P Rogers).
Conflicts of interest
PG holds a research grant from Gore Medical and has a consultant and proctorship agreement with Boston Scientific. SM holds consultancy agreements with CR Bard and WL Gore. All other authors have no relevant conflicts of interest to declare.
Correspondence to: Prof Martin M Brown, Institute of Neurology, University College London, Box 6, The National Hospital for Neurology and Neurosurgery, Queen Square, London WC1N 3BG, UK m.brown@ion.ucl.ac.uk
References
- 1.European Carotid Surgery Trialists' Collaborative Group Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–1387. [PubMed] [Google Scholar]
- 2.Barnett HJ, Taylor DW, Eliasziw M. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415–1425. doi: 10.1056/NEJM199811123392002. [DOI] [PubMed] [Google Scholar]
- 3.Rothwell PM, Eliasziw M, Gutnikov SA, for the Carotid Endarterectomy Trialists' Collaboration Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet. 2003;361:107–116. doi: 10.1016/s0140-6736(03)12228-3. [DOI] [PubMed] [Google Scholar]
- 4.CAVATAS investigators Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001;357:1729–1737. [PubMed] [Google Scholar]
- 5.Mas JL, Chatellier G, Beyssen B. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355:1660–1671. doi: 10.1056/NEJMoa061752. [DOI] [PubMed] [Google Scholar]
- 6.The SPACE Collaborative Group 30 day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised non-inferiority trial. Lancet. 2006;368:1239–1247. doi: 10.1016/S0140-6736(06)69122-8. [DOI] [PubMed] [Google Scholar]
- 7.Eckstein HH, Ringleb P, Allenberg JR. Results of the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study to treat symptomatic stenoses at 2 years: a multinational, prospective, randomised trial. Lancet Neurol. 2008;7:893–902. doi: 10.1016/S1474-4422(08)70196-0. [DOI] [PubMed] [Google Scholar]
- 8.Mas JL, Trinquart L, Leys D, for the EVA-3S investigators Endarterectomy Versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) trial: results up to 4 years from a randomised, multicentre trial. Lancet Neurol. 2008;7:885–892. doi: 10.1016/S1474-4422(08)70195-9. [DOI] [PubMed] [Google Scholar]
- 9.Featherstone RL, Brown MM, Coward LJ. International carotid stenting study: protocol for a randomised clinical trial comparing carotid stenting with endarterectomy in symptomatic carotid artery stenosis. Cerebrovasc Dis. 2004;18:69–74. doi: 10.1159/000078753. [DOI] [PubMed] [Google Scholar]
- 10.Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8:1006–1018. doi: 10.1016/S1474-4422(09)70236-4. [DOI] [PubMed] [Google Scholar]
- 11.Ederle J, Featherstone RL, Brown MM. Percutaneous transluminal angioplasty and stenting for carotid artery stenosis. Cochrane Database Syst Rev. 2007;4 doi: 10.1002/14651858.CD000515.pub3. CD000515. [DOI] [PubMed] [Google Scholar]
- 12.Ederle J, Bonati LH, Dobson J, on behalf of the CAVATAS investigators Endovascular treatment with angioplasty or stenting versus endarterectomy in patients with carotid artery stenosis in the Carotid And Vertebral Artery Transluminal Angioplasty Study (CAVATAS): long-term follow-up of a randomised trial. Lancet Neurol. 2009;8:898–907. doi: 10.1016/S1474-4422(09)70228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yadav JS, Wholey MH, Kuntz RE. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351:493–501. doi: 10.1056/NEJMoa040127. [DOI] [PubMed] [Google Scholar]
- 14.Lal BK, Brott TG. The Carotid Revascularization Endarterectomy vs Stenting Trial completes randomization: lessons learned and anticipated results. J Vasc Surg. 2009;50:1224–1231. doi: 10.1016/j.jvs.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonati LH, Jongen LM, Haller S, for the ICSS-MRI study group New ischaemic brain lesions on MRI after stenting or endarterectomy for symptomatic carotid stenosis: a substudy of the International Carotid Stenting Study (ICSS) Lancet Neurol. 2010 doi: 10.1016/S1474-4422(10)70057-0. published online Feb 26. [DOI] [PubMed] [Google Scholar]
- 16.Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ, for the Carotid Endarterectomy Trialists Collaboration Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet. 2004;363:915–924. doi: 10.1016/S0140-6736(04)15785-1. [DOI] [PubMed] [Google Scholar]
- 17.Bond R, Rerkasem K, Cuffe R, Rothwell PM. A systematic review of the associations between age and sex and the operative risks of carotid endarterectomy. Cerebrovasc Dis. 2005;20:69–77. doi: 10.1159/000086509. [DOI] [PubMed] [Google Scholar]
- 18.Rothwell PM, Slattery J, Warlow CP. Clinical and angiographic predictors of stroke and death from carotid endarterectomy: systematic review. BMJ. 1997;315:1571–1577. doi: 10.1136/bmj.315.7122.1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonati LH, Ederle J, McCabe DJ, on behalf of the CAVATAS investigators Long-term risk of carotid restenosis in patients randomly assigned to endovascular treatment or endarterectomy in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): long-term follow-up of a randomised trial. Lancet Neurol. 2009;8:908–917. doi: 10.1016/S1474-4422(09)70227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]