Abstract
Foot-and-mouth disease virus (FMDV) continues to be a significant economic problem worldwide. Control of the disease involves the use of killed-virus vaccines, a control measure developed decades ago. After natural infection, the primary site of replication of FMDV is the pharyngeal area, suggesting that a mucosal immune response is the most effective. Humoral immunity to killed-virus vaccination induces antibodies that can prevent the clinical disease but not local infection. Determining whether infection or vaccination stimulates IgA-mediated local immunity depends on the method of analysis. Different assays have been described to analyze the quality of antibody responses of cattle and swine to FMDV, including indirect double-antibody sandwich enzyme-linked immunosorbent assay (IDAS-ELISA) and antibody capture assay-ELISA (ACA-ELISA). We tested these assays on swine and show that vaccinated animals had FMDV-specific IgM and IgG but no IgA in either serum or saliva. After the infection, both assays detected FMDV-specific IgM, IgG, and IgA in serum. Notably, serum IgA was more readily detected using the ACA-ELISA, whereas IgA was not detected in saliva with this assay. FMDV-specific IgA antibodies were detected in saliva samples using the IDAS-ELISA. These data show that parenterally administered, killed-virus vaccine does not induce a mucosal antibody response to FMDV and illuminates limitations and appropriate applications of the two ELISAs used to measure FMDV-specific responses. Further, the presence of the IgA antivirus in serum correlates with the presence of such antibodies in saliva.
Foot-and-mouth disease virus (FMDV) continues to be a significant economic problem worldwide. In FMDV-free countries, an outbreak of the virus freezes the export of all animal products, causing significant loss of revenue to the livestock industry. Eradication of the disease from areas of endemicity involves the use of killed-virus vaccines, a control measure developed decades ago. The vaccine offers clinical protection against FMDV, but it does not prevent virus excretion or the establishment of latency after challenge infection (14). Recovery from FMDV and protection from reinfection are associated predominantly with the presence of circulating neutralizing antibody (20, 25, 32).
Transmission of FMDV between animals is primarily via oral-pharyngeal exposure from contaminated feed and aerosols emitted from infected animals. This has led to a particular interest in the local, mucosal immune response to FMDV infection in the pharynx since, following exposure, this region is the most common site for primary virus replication (30, 36). Unfortunately, analysis of mucosal immunity has essentially been limited to assessment of immunoglobulin A (IgA) responses to FMDV infection of swine. Alternatively, the virus can gain direct entry into the skin through cuts or abrasions, particularly during infection of swine, as reviewed by Alexandersen and colleagues (2). The latter route of viral entry is more common in swine than in other susceptible species.
The role of T cells in stimulating B cell proliferation and subsequent differentiation to high-affinity antibody production in the swine response to FMDV is of particular interest. In the response of other species to different pathogens, it has been clearly demonstrated that both Th1 and Th2 responses contribute to effective immunity and clearance of pathogens (4, 26, 28, 33, 34). Manipulating vaccine formulations to target immune responses will be useful for FMDV prophylactics in swine and cattle, but the present knowledge of immune responses in these species offers little insight into the importance of the Th1/Th2 paradigm in effective antiviral immunity. Thus, extrapolating the Th1/Th2 paradigm of mice to swine is problematic.
In mice, the B cell switch from IgM to IgG2b antibody secretion is mediated by Th1 cytokines, specifically, gamma interferon (IFN-γ), whereas Th2 cytokines, including interleuken-4 (IL-4), IL-5, IL-13, and transforming growth factor β (TGF-β), accompany class switch to IgG1, IgG3, IgE, and IgA. However, IgG1 and IgG2b are not homologous immunoglobulins among distantly related mammals since speciation preceded subclass diversification (13, 23).
Further complicating our understanding of antibody responses in pigs is the fact that there are six subclasses of porcine IgG, five of which occur in at least two allelic forms (13). IgG1 is transcribed predominately in fetal and adult swine but not in the ileal Peyer's patches and mesenteric lymph nodes of fetal and neonatal piglets, where IgG3 predominates (11). IgG2 is poorly transcribed in all tissues of fetal and neonatal piglets. IgG3, the primordial porcine IgG, is most 5′ in the CH locus and, based on sequences motifs, is best equipped to activate complement and bind to Fcγ receptors (13, 17a). Currently, only two monoclonal antibodies (MAbs) that are described as specific for IgG1 and IgG2 are available. Based on preliminary results, anti-IgG1 is quite likely IgG1 specific, whereas the anti-IgG2 MAb likely recognizes an infraclass group that includes IgG2, IgG4, and IgG6. Since purified forms of IgG4 and IgG6 are not yet available, this has yet to be tested.
There are other factors that complicate understanding antibody responses to viral infection of mucosal surfaces in swine. In their studies on the distribution of antibody-containing cells, Bianchi and colleagues recognized differential reactivities among anti-porcine IgA MAb, which they suggested might reflect different IgA subclasses, as in humans (3). At nearly the same time, the porcine Cα gene was cloned and was shown to occur in two allelic forms, one of which was missing 4 amino acids of the hinge due to a splice accepter site mutation (5, 6). Sera from swine homozygous for IgAa and IgAb were exchanged to show that the MAbs generated by Bianchi and colleagues differentially recognized the two allotypic variants (29). The distribution of the two allotypes appears to be founder and breed associated, with IgAa occurring in the highest frequency (29).
The study reported here focuses on the mucosal antibody response of swine and utilizes isotype-specific reagents in two different, sensitive enzyme-linked immunosorbent assays (ELISAs). The comparison of assays for determination of the quality of antibody responses to FMDV addresses the limitations of presently available reagents. We tested for antibody responses in serum and saliva at 7, 14, or 21 days postvaccination (dpv) with a single dose of vaccine and compared the responses to those resulting from direct inoculation of pigs or following contact transmission of infection. FMDV-specific IgA, IgM, and IgG antibodies were readily detected in serum after infection, and IgA was detected in the saliva of the same animals. However, following vaccination, there were IgM and IgG responses in serum but no IgA antibodies in serum or saliva. These results illuminate the need to develop alternative FMDV vaccines designed for more efficient mucosal delivery and the induction of a mucosal IgA response that is predicted to yield better control of FMDV in an outbreak.
MATERIALS AND METHODS
Experimental design and animals.
All vaccine trials and live-virus challenges in pigs were reviewed and approved by the Plum Island Animal Disease Center's Animal Care and Use Committee before initiation of these studies. Eighteen Yorkshire pigs weighing 25 to 30 kg were used for the study and housed together in one room measuring 6 by 6 m. Vaccinated animals were inoculated with the inactivated, purified O1 Manisa strain of FMDV in a double-oil emulsion (provided by T. Doel, Merial Animal Health, Pirbright, Surrey, United Kingdom), previously described in a bovine vaccination/challenge study (18). The estimated potency was consistent with a vaccine consisting of three 50% protective doses (PD50), and the vaccine was administered at the manufacturer's recommended dose of 1.0 ml per animal (half of a bovine dose), intramuscularly in the neck. Vaccinations were staggered to allow simultaneous challenge of all pigs. Five animals were vaccinated 21 days before challenge (animals 51, 52, 53, 54, and 55, named group −21), and five animals were vaccinated 7 days before challenge (animals 56, 57, 58, 59, and 60, named group −7). Three pigs were used as a source of direct-contact virus (pigs 61, 62, and 63, named the direct-inoculation [DI] group) by means of intradermal inoculation of 100,000 PFU of pig-derived O1 Manisa in two sites in the heel bulb. The five remaining animals were used as nonvaccinated controls (pigs 64, 65, 66, 67, and 68, named the direct-contact [DC] group). One animal (pig 61) was euthanized at 7 days postchallenge (dpc) due to severity of lesions; therefore, no results for antibodies are shown for this particular animal.
Sample collection.
Serum and saliva were collected weekly from dpc −21 to 28 for antibody detection. Whole blood was collected in heparin at 0, 1, 2, 3, 4, 5, 6, and 7 dpc for virus isolation.
Clinical assessment.
Records of the sites on the animals showing vesicles were prepared each day, and a vesicle score was calculated by summing the following: one point for each affected digit, one point for vesicles on the tongue, one point for vesicles on the snout, one point for vesicles on the lower lip, and one point for vesicles on the carpal or tarsal area of one or more legs. A maximum lesion score of 20 was possible. Once a vesicle appeared at a site, the site was scored “positive” on all subsequent days, even if the vesicles at that site had begun to heal.
Virus isolation and quantification.
The presence of virus in whole-blood samples was measured by a standard plaque assay with BHK-21 cells (22).
FMDV-neutralizing antibodies from serum.
Serum samples were heat inactivated (56°C, 30 min) and used for microtiter neutralization assay on BHK-21 cells. Serial dilutions of serum were incubated with a virus dose of 100 50% tissue culture infective doses (TCID50) of FMDV O1 Manisa for 1 h at 37°C and then transferred to preformed monolayers of BHK-21 cells and incubated at 37°C for 48 to 72 h. Cytopathic effect (CPE) was used to determine the endpoint titers, which were calculated as the reciprocal of the last serum dilution to neutralize 100 TCID50 of virus in 50% of the wells.
Specificity of antiporcine IgA antibodies.
Porcine IgAa and IgAb were purified from late-phase colostrum samples obtained from sows homozygous for IgAa and IgAb, respectively, using previously described methods; their purity was confirmed by SDS-PAGE (8, 24). The protein concentration of each preparation was determined by absorbance at 280 nm using an absorbance coefficient of 1.36 (1 cm, 0.1%). The functional or active concentration was determined by the recognition of immobilized IgAa and IgAb by biotinylated polyclonal anti-IgA reagents. Within the titration range for both allotypic variants, two different concentrations of immobilized IgAa and IgAb (60 ng and 30 ng, respectively) were selected for all subsequent tests. These were then used as targets for detection by the various anti-porcine MAb and polyclonal antibodies (PAbs) listed in Table 1. The dilution of each MAb tested was optimized so that the activities of different MAbs could be compared on the same microtiter plates (Table 1).
TABLE 1.
Anti-porcine IgA MAbs and PAbs tested
| Reagent | Species | Source | Dilution used | IgA concn (ng) | Specificity |
|---|---|---|---|---|---|
| M1459 | Mouse | Klaus Nielsen | 1:10,000 | 60 | Neutral |
| 30 | Neutral | ||||
| M1450 | Mouse | Klaus Nielsen | 1:10,000 | 60 | IgAa biased |
| 30 | IgAa biased | ||||
| M1457 | Mouse | Klaus Nielsen | 1:10,000 | 60 | IgAb biased |
| 30 | IgAb biased | ||||
| MCA638 | Mouse | Serotec | 1:200 | 60 | Neutral |
| 30 | Neutral | ||||
| 28.8.1 | Mouse | Andre Bianchi | 1:2,000 | 60 | IgAa biased |
| 30 | IgAa biased | ||||
| 27.9.1 | Mouse | Andre Bianchi | 1:5,000 | 60 | IgAa biased |
| 30 | IgAa biased | ||||
| KAK 5376 | Rabbit | Francek Klobasa | 1:40,000 | 60 | Neutral |
| 30 | Neutral | ||||
| KAK 6272 | Rabbit | Francek Klobasa | 1:150 | 60 | Neutral |
| 30 | Neutral | ||||
| ZAK 141 | Goat | Francek Klobasa | 1:5,000 | 60 | Neutral |
| 30 | Neutral | ||||
| ZAK 71 | Goat | Francek Klobasa | 1:40,000 | 60 | Neutral |
| 30 | Neutral |
MAbs bound to immobilized IgAa and IgAb were detected using goat anti-mouse IgG conjugated to alkaline phosphatase (AP; Sigma product number A2429) followed by para-nitrophenyl phosphate (AP substrate) at 1 mg/ml. The detection of immobilized IgAa and IgAb by various biotinylated PAbs to porcine IgA was visualized using ExtrAvidin AP (Sigma-Aldrich product number E2636). Biotinylation of the gamma globulin fraction of the polyclonal antisera was done using N-hydroxysuccinimide ester-polyethyleneoxide-biotin according to the instructions of the manufacturer (Pierce Chemical, Rockford, IL).
Isotype-specific antibody immunoassay for FMDV.
The IgM, IgA, and total IgG responses to the virus were determined by two specific antibody immunoassays. The first of these uses a sandwich-based system in which FMDV was captured by a rabbit anti-FMDV O1 Manisa antiserum (Institute for Animal Health, Pirbright, United Kingdom), diluted to 1:4,000 in carbonate-bicarbonate buffer (pH 9.6) and adsorbed on Immulon 2 microtiter plates (Dynatech Corp., Chantilly, VA) at 50 μl/well (see Fig. S1A in the supplemental material). This procedure for virus immobilization avoids adsorption-induced conformational change and the adsorption of culture medium proteins along with the virus (21). After 4 washes with PBS-T (0.05% Tween 20 in phosphate-buffered saline [PBS]), plates were blocked for 1 h at 37°C with blocking buffer (10% normal horse serum [Sigma, St. Louis, MO] in PBS-T) in a shaking incubator. Preparations of inactivated FMDV from infected fibroblasts (BHK-21 cells) that were captured in this manner were then used as the solid-phase antigen. Serum/saliva samples were tested for FMDV-specific IgM, IgA, and total IgG antibodies. After incubation of the samples and appropriate washing steps, the bound swine antibodies were detected using either goat anti-swine IgM or goat anti-swine IgG directly conjugated to horseradish peroxidase (product number 04-14-03 or 04-14-02, respectively; KPL, Gaithersburg, MD) or a mouse monoclonal anti-swine IgA (clone K61 1B4, product number MCA638; Serotec, Raleigh, NC) that was subsequently detected using goat anti-mouse IgG directly conjugated with horseradish peroxidase (product number 04-18-02 from KPL). This ELISA format has been previously described as an isotype-specific indirect double-antibody sandwich ELISA (IDAS-ELISA) (35). In the interest of consistency with the published data, we have retained this nomenclature.
The second assay used the same mouse MAb described above but in an assay configuration previously described by van Zaane and colleagues as the isotype-specific antibody capture assay-ELISA (ACA-ELISA) (35). In this configuration, Immulon 2 microtiter plates were coated with sheep anti-mouse IgG (product number AAC10P from Serotec) diluted 1:200 in coating buffer (carbonate-bicarbonate, pH 9.6) at 50 μl/well (see Fig. S1B in the supplemental material). After 4 washes with PBS-T, the plates were blocked as described above, washed, and subsequently incubated with monoclonal mouse anti-swine IgA (the same antibodies used above). After washing of the plates, the samples, serum or saliva, from vaccinated and/or infected swine were added. After appropriate washing steps, the virus was added and subsequently detected using rabbit anti-FMDV O1 Manisa hyperimmune antiserum (Institute for Animal Health, Pirbright, United Kingdom) diluted to 1:4,000. The rabbit antibody was detected using goat polyclonal anti-rabbit IgG conjugated with peroxidase.
An optical density at 450 nm (OD450)/OD570 ratio of 0.1 was selected as a background cutoff for both ELISAs based on analysis of negative controls and results from prevaccination/infection samples. Results for both ELISAs are expressed as OD450/OD570 ratios at a single dilution: 1/100 for serum samples and 1/5 for saliva samples. These working dilutions were selected after titration assays were performed in parallel with both ELISAs, with dilutions from 1/25 to 1/400,000 for serum or 1/1 to 1/400,000 for saliva samples. When samples were analyzed by IDAS-ELISA, the OD450/OD570 ratio of the selected dilutions was directly related with the titer (the last dilution that showed an OD450/OD570 ratio above the cutoff). The ACA-ELISA did not yield endpoint values because the dilution curves had multiple slopes, possibly related to an intraisotype competition (see Fig. S1 in the supplemental material for a diagram of comparative ELISAs).
Statistical analysis.
The general linear model of statistical analysis implemented in the SAS 9.1 package (SAS Institute Inc., Cary, NC) was used to test the significant differences among treatment groups. If the P value of the test was equal to or smaller than 0.05, the differences among the groups were declared significant and Tukey's Studentized range test was used to detect the differences between the groups.
RESULTS
Viremia and clinical signs.
Naïve animals inoculated directly in the heel bulb with FMDV showed clear signs of disease by 1 dpc, characterized by formation of vesicles, with a peak clinical score of 19 to 20 out of a maximum of 20 (Table 2). Virus in blood was isolated at 1 dpc, and the peak of viremia for these animals was at 2 dpc (Table 3). A second cohort of animals became infected by direct contact with the directly inoculated, infected pigs. These animals also showed clear signs of FMD, with vesicles detected as early as 3 dpc, with a peak lesion score of 16 to 18 out of 20 by 4 to 6 dpc (Table 2). In these contact-infected animals, viremia followed the pattern of the needle-inoculated animals, with an expected delay of 48 h (Table 3).
TABLE 2.
Clinical score for FMD
| Group | Pig | Clinical score at dpce: |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| −21a | 51 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 52 | 0 | 0 | 1 | 1 | 1 | 4 | 5 | 5 | |
| 53 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 3 | |
| 54 | 0 | 0 | 0 | 0 | 2 | 7 | 10 | 13 | |
| 55 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| −7b | 56 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 5 |
| 57 | 0 | 0 | 0 | 0 | 0 | 2 | 4 | 5 | |
| 58 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | |
| 59 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |
| 60 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| DIc | 61 | 0 | 1 | 13 | 19 | 19 | 19 | 19 | 19 |
| 62 | 0 | 1 | 15 | 20 | 20 | 20 | 20 | 20 | |
| 63 | 0 | 1 | 17 | 18 | 19 | 19 | 19 | 19 | |
| DCd | 64 | 0 | 0 | 0 | 1 | 16 | 18 | 18 | 18 |
| 65 | 0 | 0 | 0 | 6 | 18 | 18 | 18 | 18 | |
| 66 | 0 | 0 | 0 | 1 | 14 | 16 | 16 | 16 | |
| 67 | 0 | 0 | 0 | 3 | 13 | 17 | 18 | 18 | |
| 68 | 0 | 0 | 0 | 12 | 16 | 15 | 16 | 16 | |
Animals were vaccinated on dpc −21 (infected by direct contact with directly inoculated animals).
Animals were vaccinated on dpc −7 (infected by direct contact with directly inoculated animals).
Animals were directly inoculated on the day of challenge.
Naïve animals infected by direct contact with directly inoculated animals.
Clinical scores were calculated as numbers of vesicles on each toe (4 per foot, with a potential score of 16), in the mouth or on the lips, on the tongue, on the snout, and elsewhere, for a maximum score of 20, on the indicated day postchallenge of directly inoculated animals.
TABLE 3.
Viremia
| Group | Pig | No. of PFU/ml on dpce: |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| −21a | 51 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 |
| 52 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| 53 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| 54 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| 55 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| −7b | 56 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 |
| 57 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| 58 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| 59 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| 60 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | <0.7 | |
| DIc | 61 | <0.7 | 4.1 | 5.6 | <0.7 | <0.7 | <0.7 | ND | ND |
| 62 | <0.7 | 4.2 | 5.8 | <0.7 | <0.7 | <0.7 | ND | ND | |
| 63 | <0.7 | 4.2 | 5.9 | 1.7 | <0.7 | <0.7 | ND | ND | |
| DCd | 64 | <0.7 | <0.7 | <0.7 | 3.5 | 5.7 | 2.4 | <0.7 | <0.7 |
| 65 | <0.7 | <0.7 | <0.7 | 2.2 | 4.0 | 2.2 | <0.7 | <0.7 | |
| 66 | <0.7 | <0.7 | <0.7 | 2.1 | 4.5 | <0.7 | <0.7 | <0.7 | |
| 67 | <0.7 | <0.7 | <0.7 | 3.4 | 4.3 | <0.7 | <0.7 | <0.7 | |
| 68 | <0.7 | <0.7 | <0.7 | 4.5 | 2.3 | <0.7 | <0.7 | <0.7 | |
Animals were vaccinated on dpc −21 (infected by direct contact with directly inoculated animals).
Animals were vaccinated on dpc −7 (infected by direct contact with directly inoculated animals).
Animals were directly inoculated on the day of challenge.
Naïve animals were infected by direct contact with directly inoculated animals.
Day postchallenge of directly inoculated animals. ND, not determined.
Of the animals vaccinated 21 days before natural infection by contact as the challenge, 2 out of 5 animals (pigs 51 and 55) were protected, with no detectable clinical signs and no virus isolated from their blood for 7 days after contact. The 3 remaining animals (pigs 52, 53, and 54) did not show virus in their blood, and few lesions were detected (clinical scores were 3, 5, and 13, respectively). Of the animals challenged 7 dpv, only 1 of 5 animals (pig 60) was protected, having no clinical signs or viremia for 7 days after contact. The 4 remaining animals (pigs 56, 57, 58, and 59) had low clinical scores of 1, 2, 5, and 5, respectively (Table 2). As with the other vaccinated group, there was no virus isolated from the blood of any of these animals over the 7-day sampling period.
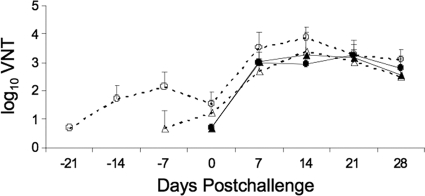
Serum neutralizing antibody response following vaccination and infection.
Serum samples from animals vaccinated 21 days before challenge with killed-virus vaccine showed rising titers of neutralizing antibodies, peaking at 14 dpv (dpc −7 in Fig. 1). Within the group vaccinated 7 days before challenge, animal 57 did not show any neutralizing antibody titer, but the other 4 animals had detectable titers on the day of challenge. In other studies, samples were taken on days 1 through 4 postvaccination and were uniformly negative, as were samples from days 1 through 4 postchallenge from all naïve animals, regardless of whether they were directly inoculated or infected by contact. No correlation was detected between serum neutralizing titer and protection from clinical disease, and all animals showed increasing titers of neutralizing antibody after challenge, peaking at 14 dpc (Fig. 1). These data indicate that animals protected from the development of clinical disease were not protected from infection. The subclinical infection results in production of viral antigen, which boosts the serum neutralizing antibody response.
FIG. 1.
Mean serum-neutralizing antibody responses in swine following vaccination and challenge with FMDV O Manisa. Three pigs were directly inoculated (closed circles) and used as donors for challenge of groups of 5 pigs that were vaccinated at −21(open circles) or −7 (open triangles) dpc and to 5 naïve pigs (contact inoculated, closed triangles). VNT, virus-neutralizing titer.
Specificity of Ig isotype ELISAs used in this study.
A complicating factor in understanding the antibody response of swine to FMDV is the limitation of the reagents available to determine the quality of the antibody response. MAbs reactive with each of the six porcine IgG subclasses (12, 13) are not available; only two MAbs designated anti-IgG1 and anti-IgG2 are currently available. In addition, the analysis of the IgA antibody used required further analysis of specificity.
Before using the porcine IgG subclass-specific MAbs in studies of FMDV, we tested their specificity in several ways since in preliminary tests, inconsistent results in ACA-ELISA and IDAS-ELISA were obtained. First, we used three MAbs, anti-IgG1, anti-IgG2, and anti-IgA, to capture their target Igs from serum. Then we used the same MAbs as detection antibodies for the Igs that had been captured. We found that anti-IgG1 recognized Igs captured by all three MAbs, whereas anti-IgG2 appeared to be specific for the Ig that had been captured with anti-IgG2 antibody and did not recognize Igs captured by anti-IgG1. Therefore, we did not use the monoclonal anti-IgG1 or anti-IgG2 antibodies in these analyses. Anti-IgA proved to be specific by the same criterion and when tested using purified pan porcine IgG and purified IgA.
In a separate study, these anti-porcine IgG MAbs were tested against porcine-camelid chimeric Igs constructed from the gene sequences of a number of the porcine IgG subclasses and allotypic variants (J. E. Butler, S. Muylderman, P. Boyd, and J. K. Lunney, unpublished). These tests confirmed that anti-IgG2 did not recognize any known IgG1 variant, whereas anti-IgG1 was weakly cross-reactive with several subclass chimeric Igs and was biased to the IgG1b allotype. However, since purified forms of all six subclasses and their allotypes are currently unavailable, the full specificity of these two MAbs to swine IgG remains unknown. Therefore, we relied on a polyclonal antibody (PAb) to IgG throughout the study.
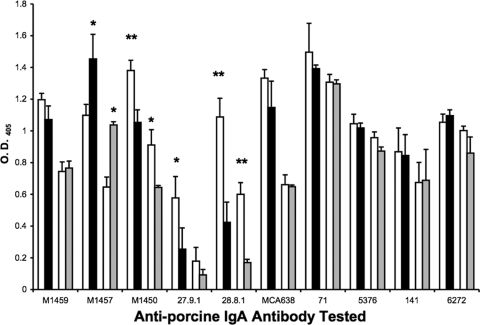
Since anti-IgA proved to be specific in these tests of specificity, our concern was then for allotype bias. Further assessment of the specificity of IgA reagents confirmed evidence of allotype bias by MAbs and raised the possibility that data obtained in immunoassays might be biased by the particular MAbs and PAbs for porcine IgAa and IgAb used in our studies. Figure 2 compares the relative specificities of six anti-porcine MAb and four PAb reagents at two different concentrations of immobilized IgAa and IgAb. The reagents are described in Table 1. Allotype bias was evaluated by two-tailed Student t tests. Four MAbs to IgA (M1457, M1450, 27.9.1, and 28.8.1) were biased in one or the other direction, although 27.9.1 was not significantly biased when tested against IgAa and IgAb at 30 ng. The mean values shown in Fig. 2 are from independently prepared triplicate dilutions. Monoclonal antibodies M1459 from the Centre for Veterinary Biologics (CVB) at the National Veterinary Services Laboratory (NVSL), APHIS, U.S. Department of Agriculture (USDA) (Ames, IA), and MCA638 from Serotec (Raleigh, NC) show no allotype bias in their reactivities for two different concentrations of immobilized IgAa and IgAb. However, there was a 50-fold difference in useful concentration/dilution, indicating that the Serotec product is supplied in a highly diluted form (Table 1). The criterion for allotype bias is based on the premise that since PAbs are comprised of many antibodies that recognize different epitopes, bias will be reduced compared to that of MAbs that theoretically recognize only one epitope. This premise is supported by the empirical results obtained with four different PAbs (Table 1; Fig. 2). Based on these specificity tests, we analyzed the IgA anti-FMDV response of vaccinated and challenged animals using the Serotec monoclonal antibody to IgA (clone K61 1B4, Serotec product number MCA638).
FIG. 2.
The allotype specificity of six MAbs and four PAbs raised against porcine IgA tested against IgAa (open bars) and IgAb (black bars) immobilized at 60 ng per well or IgAa (open bars) and IgAb (gray bars) immobilized at 30 ng per well. *, P < 0.04; **, P < 0.006 (two-tailed Student t test results).
Serum IgM and IgG responses to FMDV following infection or vaccination and challenge.
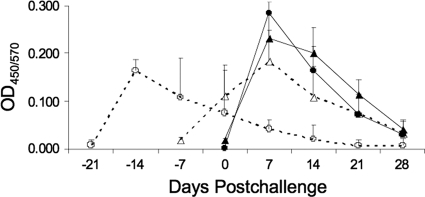
Analysis of the serum IgM response to FMDV was carried out using the IDAS-ELISA. The data in Fig. 3 illustrate that IgM anti-FMDV peaked in all animals from all treatment groups at 7 dpv (day −14 relative to the live-virus challenge) as well as at 7 dpc in the naïve controls. As expected, the mean signal for IgM from serum samples taken from animals vaccinated 21 days before challenge decreased after 7 dpv and was not affected by exposure to virus, even though one of these animals exhibited clinical signs of disease. The boost in the IgM response in the animals challenged at day 7 was also expected, as the IgM response had yet to peak and there was a new exposure to FMDV antigens. By 28 dpc, IgM antibody was diminishing in a normal pattern in all groups.
FIG. 3.
Mean serum IgM antibody responses in swine following vaccination and challenge with FMDV O Manisa. Three pigs were directly inoculated (closed circles) and used as donors for challenge of groups of 5 pigs that were vaccinated at −21 (open circles) or −7 (open triangles) dpc and to 5 naïve pigs (contact inoculated; closed triangles).
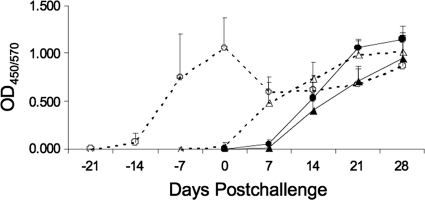
Analysis of the serum IgG anti-FMDV antibody response shows that no animals had IgG at 7 dpv for vaccinated animals or 7 dpc for nonvaccinated controls (dpc −14, 0, or 7 in Fig. 4). Rising titers of IgG were detected by day 14 following inoculation or vaccination in animals not challenged at 7 dpv and continued rising at day 21 for all groups whether vaccinated, directly infected, or infected by contact with animals presenting with disease. Following challenge, the animals vaccinated 7 days previously showed a rising titer of IgG anti-FMDV. Contrarily, the animals challenged 21 dpv showed a flat IgG response pattern, indicating a lack of further exposure to antigen. This includes the three animals that showed clinical signs of disease (numbers 52, 53, and 54 in Table 2). This result is consistent with the observation that none of the vaccinated animals had detectable viremia and therefore little or no viral antigen to stimulate a boost in the antibody response.
FIG. 4.
Mean serum IgG antibody responses in swine following vaccination and challenge with FMDV O Manisa. Three pigs were directly inoculated (closed circles) and used as donors for challenge of groups of 5 pigs that were vaccinated at −21 (open circles) or −7 (open triangles) dpc and to 5 naïve pigs (contact inoculated; closed triangles).
IgA anti-FMDV antibody responses.
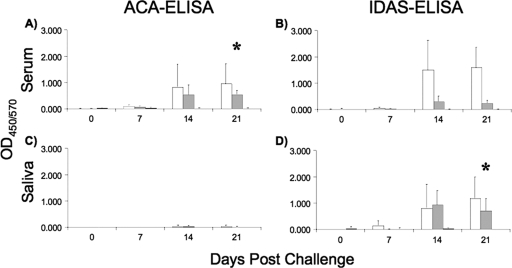
The IgA response to FMDV vaccination and infection illustrates the complexity of analyzing these responses. Serum IgA was not detectable in the vaccinated groups by either ELISA methodology when samples taken before challenge were analyzed (Fig. 5A and B). Following virus exposure, the IgA anti-FMDV response was very low at 7 dpc in all groups regardless of the assay used (Fig. 5A and B). Contrarily, all nonvaccinated animals exhibited an IgA anti-FMDV response detectable in serum samples by 14 dpc using either assay. Interestingly, the difference in IgA levels reached statistical significance when vaccinated animals were compared at 21 dpv and both groups of naïve animals were compared at 21 dpc (P = 0.001) but only in the ACA-ELISA (Fig. 5A). Further, the same differential comparison of the day 14 samples was nearly significant (P = 0.068) (Fig. 5A) by the ACA-ELISA. When the same set of serum samples were assayed with the IDAS-ELISA, the results differed. Here, animals directly inoculated with FMDV had an IgA anti-FMDV response at both 14 and 21 dpc, significantly more than that of either contact-exposed or vaccinated animals (P = 0.0026 and 0.0001, respectively) (Fig. 5B). However, there were no significant differences between contact-exposed animals and vaccinated animals on either day 14 or day 21 (Fig. 5B).
FIG. 5.
Mean serum and saliva IgA antibody responses in swine following vaccination and challenge with FMDV O Manisa. Three pigs were directly inoculated (white bars) and used as donors for challenge of groups of 5 pigs (contact inoculated, gray bars) or vaccinated at −21 dpc (black bars). Porcine IgA was detected with mouse monoclonal anti-IgA (Serotec product number MCA638). * denotes differences with statistical significance when vaccinated animals were compared at 21 dpv and both groups of naïve animals were compared at 21 dpc (P = 0.001 for panel A and P = 0.023 for panel D).
Results with saliva samples add to the understanding of the antibody response using these different assays, both in previous reports and in the present study. As in the sera, no IgA anti-FMDV was detected in the saliva by either method of ELISA before the challenge (Fig. 5C and D). Unlike with the sera, the ACA-ELISA detected only minimal levels of IgA in the saliva of the infected animals (Fig. 5C). However, the IDAS-ELISA detected salivary IgA anti-FMDV starting at 7 or 14 dpc, regardless of whether animals were infected by direct inoculation or contact transmission. These animals produced more IgA in their saliva than the vaccinated animals at day 14, with differences being significant only between the contact and vaccinated groups. The difference in IgA levels reached statistical significance when we compared vaccinated animals at 21 dpv and both groups of naïve animals at 21 dpc (P = 0.023) (Fig. 5D).
Following the challenge of vaccinated animals, there was a barely detectable IgA anti-FMDV response in either serum or saliva. This was predicted, as both vaccinated groups had very mild disease and no detectable viremia following challenge. Therefore, there was very little antigen available in vaccinated animals to drive the switch to an IgA anti-FMDV response. The IgA anti-FMDV response was detected only in the naïve, infected animals. Detection in serum requires the ACA-ELISA format, whereas detection in saliva was seen only in the IDAS-ELISA format. Importantly, in all animals where IgA anti-FMDV was detected in saliva, it was also detected in serum.
DISCUSSION
Historically, the prediction of protection against infection with FMDV correlates with the presence of serum neutralizing antibody. Many exceptions to this have been reported, highlighting the need to understand more about the immune response to FMDV. Even within the more narrow analysis of the humoral response to the virus, there is still minimal understanding of the details of the development of anti-FMDV antibody responses in different lymphoid tissues and the circulation leading to control of the disease by antibodies. For example, neutralizing antibody titers are used to correlate humoral immune responses and protection against infection, but little is known about the role of nonneutralizing antibodies in the antiviral response. Further, the majority of available data derives from studies where animals are challenged with FMDV by needle inoculation. Certainly, this allows for control of the challenge dose and consistent induction of clinical disease, but natural infection is by contact with contaminated feed or bedding and, most often, actively infected animals shedding virus.
The results of the contact challenge of vaccinated pigs presented here show that vaccinated animals were only partially protected, as 3 of 5 animals in the group vaccinated 21 days prior to virus challenge and 4 of 5 animals in the group vaccinated 7 days prior to challenge developed clinical symptoms of disease. Clearly, all vaccinated animals showed delayed clinical signs, a reduced clinical score when disease developed, and no detection of virus in their blood. By comparison, naïve animals had a rapid onset of disease, high clinical scores, and high levels of viremia as a result of the same exposure to virus. Serum neutralizing antibodies were detected in all but one of the vaccinated animals before contact with infected animals, and it should be noted that relative levels of neutralizing antibody did not correlate with levels of clinical disease.
The lack of protection could be related to the severe challenge in our study, as the different vaccinated and naïve groups were housed together for the duration of the experiment. This resulted in an overwhelming challenge from the unprotected pigs rechallenging the vaccinated pigs, as these animals shed high levels of FMDV. For instance, a milliliter of vesicular fluid can contain 106 to 108 infectious viral particles. The concept of overwhelming challenge has been cited for swine (P. Barnett et al., unpublished) and cattle (15) and is particularly relevant with regard to high-density farming practices. The lack of protection may also be related to the insufficient immune response after vaccination, particularly at a mucosal level, as discussed by Eblé et al. (17). If natural introduction of virus is via oral infection in swine during a contact transmission, FMDV-specific antibody in oral secretions such as saliva should then be critical to protection against infection.
A central objective of this study was to develop a better understanding of the mucosal antibody response. Because of the limited reagents available to determine antibody isotypes, we did not analyze IgG subtypes and limited our analysis to the IgA response in serum and saliva.
Results presented here indicate that analysis of different samples, for at least the IgA isotype of the antibody, requires use of the appropriate assay. For IgA anti-FMDV in serum, the ACA-ELISA, which first captures all of a given isotype of an antibody, is the most accurate analysis. Saliva and likely nasal samples are most accurately assayed for IgA anti-FMDV by the IDAS-ELISA, capturing all of the FMDV-specific antibody and determining IgA in that population. Given what we know from analysis of human antibody responses relative to the presence of IgA in different fluids, these results are consistent. Small concentrations of IgA in serum require the capture of all the IgA first, followed by analysis for the FMDV-specific antibodies among those proteins. IgG interference in the detection of serum IgA antibodies in an IDAS-ELISA format has been previously demonstrated (7). The dominance of IgA in mucosal secretions means that interisotype inhibition of IgA detection using an IDAS-ELISA format is inconsequential.
For this study, a very important result to be emphasized is that if there is a detectable IgA anti-FMDV response in serum, then there is also one in saliva, and if IgA anti-FMDV is detectable in saliva, it is also detectable in serum. Our data clearly show a strong correlation between the results of ACA-ELISA in sera and IDAS-ELISA in saliva (with an r2 of 0.82). Therefore, these results indicate that collection of only serum samples and analysis by ACA-ELISA allow for a representative analysis of the IgA anti-FMDV response in pigs. This differs in part with previously published data for which investigators used only a single assay for IgA response and did not compare the two assays (1, 16, 27, 31). This is strong support for the idea that local IgA responses in swine also cause elevation of serum IgA responses. This has also been observed in colonized piglets (10) and more recently in isolator piglets infected with swine influenza (J. E. Butler, K. M. Lager, Z. Bergman, and X.-Z. Sun, unpublished). Similar results were also obtained with rabbits immunized through inhalation of ovalbumin (9) and by studies of sheep showing that IgA produced in the respiratory tract makes a major contribution to serum IgA levels (19).
Intramuscular vaccination with inactivated FMDV in double-oil emulsion induced no IgA response in serum or saliva regardless of the assay employed, making this result very clear. After infection, IgA was detected in serum with both ELISAs; however, only the assay that captured all IgA antibody and determined the anti-FMDV within that (the ACA-ELISA) yielded statistically significant differences. Saliva samples had a different result, with all saliva samples testing negative for IgA anti-FMDV. The assay that analyzes all anti-FMDV antibodies in a sample, the IDAS-ELISA, showed a strong IgA anti-FMDV response in infected animals and no IgA anti-FMDV in saliva of vaccinated animals. This is an example of the intraisotype competition due to the presence of larger amounts of IgA in saliva; since there is little antibody of other isotypes in the saliva, the interisotype competition does not affect the assay. In order to detect these antibodies, they need to be concentrated by reactivity with the virus as they are in the IDAS-ELISA, and then they can be detected with isotype-specific reagents. Capturing all IgA from a saliva sample creates a condition where only a diminishingly small part of the antibody present is reactive with FMDV.
As previously reported (16), our results show that intramuscular inoculation with killed-virus vaccine does not induce an IgA response. This highlights the need to further understand the development of the immune response to this virus as we confront the design of new, rapid-action vaccines for FMDV. As the primary component of countermeasures deployed in response to outbreaks of FMDV, vaccines targeting induction of a mucosal IgA response are predicted to be highly effective considering that the pharynx is the main site of primary replication for FMDV. Such vaccines are likely to yield better control of FMDV spread in an outbreak and increase the likelihood of using these vaccines and limiting the impact of future outbreaks.
Supplementary Material
Acknowledgments
We thank Lindsey Banigan (University of Delaware) for assistance in the animal studies. We also thank Xiu Zhu Sun of the Department of Microbiology, University of Iowa College of Medicine, for his assistance in specificity analysis of the different anti-IgA reagents. Finally, we acknowledge the Laboratory Animal Resources group at Plum Island Animal Disease Center for their professional work.
This work was supported by grant CRIS 1940-32000-042, USDA (W.T.G.), and a reimbursable agreement with the Agricultural Research Service, USDA, and the Department of Homeland Security (agreement 60-1940-4-0027). J. M. Pacheco was the recipient of a Plum Island Animal Disease Center Research Participation Program fellowship, administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy (DOE) and the USDA.
Footnotes
Published ahead of print on 27 January 2010.
Supplemental material for this article may be found at http://cvi.asm.org/.
REFERENCES
- 1.Abu Elzein, E. M., and J. R. Crowther. 1981. Detection and quantification of IgM, IgA, IgG1 and IgG2 antibodies against foot-and-mouth disease virus from bovine sera using an enzyme-linked immunosorbent assay. J. Hyg. (Lond.) 86:79-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexandersen, S., Z. Zhang, A. I. Donaldson, and A. J. Garland. 2003. The pathogenesis and diagnosis of foot-and-mouth disease. J. Comp. Pathol. 129:1-36. [DOI] [PubMed] [Google Scholar]
- 3.Bianchi, A. T., H. W. Moonen-Leusen, P. J. van der Heijden, and B. A. Bokhout. 1995. The use of a double antibody sandwich ELISA and monoclonal antibodies for the assessment of porcine IgM, IgG and IgA concentrations. Vet. Immunol. Immunopathol. 44:309-317. [DOI] [PubMed] [Google Scholar]
- 4.Boom, W. H., L. Liebster, A. K. Abbas, and R. G. Titus. 1990. Patterns of cytokine secretion in murine leishmaniasis: correlation with disease progression or resolution. Infect. Immun. 58:3863-3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown, W. R., and J. E. Butler. 1994. Characterization of a C alpha gene of swine. Mol. Immunol. 31:633-642. [DOI] [PubMed] [Google Scholar]
- 6.Brown, W. R., I. Kacskovics, B. A. Amendt, N. B. Blackmore, M. Rothschild, R. Shinde, and J. E. Butler. 1995. The hinge deletion allelic variant of porcine IgA results from a mutation at the splice acceptor site in the first C alpha intron. J. Immunol. 154:3836-3842. [PubMed] [Google Scholar]
- 7.Butler, J. E., Y. Heo, P. Adams, and H. B. Richerson. 1990. The antigen-limited nature of microtiter ELISAs requires partial depletion of IgG to permit reliable determination of rabbit serum IgA antibody activity. Mol. Immunol. 27:319-325. [DOI] [PubMed] [Google Scholar]
- 8.Butler, J. E., F. Klobasa, and E. Werhahn. 1981. The differential localization of IgA, IgM and IgG in the gut of suckled neonatal piglets. Vet. Immunol. Immunopathol. 2:53-65. [DOI] [PubMed] [Google Scholar]
- 9.Butler, J. E., H. B. Richerson, P. A. Swanson, M. T. Suelzer, and W. C. Kopp. 1983. Carrier requirement for development of acute experimental hypersensitivity pneumonitis in the rabbit. Int. Arch. Allergy Appl. Immunol. 71:74-82. [DOI] [PubMed] [Google Scholar]
- 10.Butler, J. E., P. Weber, M. Sinkora, J. Sun, S. J. Ford, and R. K. Christenson. 2000. Antibody repertoire development in fetal and neonatal piglets. II. Characterization of heavy chain complementarity-determining region 3 diversity in the developing fetus. J. Immunol. 165:6999-7010. [DOI] [PubMed] [Google Scholar]
- 11.Butler, J. E., and N. Wertz. 2006. Antibody repertoire development in fetal and neonatal piglets. XVII. IgG subclass transcription revisited with emphasis on new IgG3. J. Immunol. 177:5480-5489. [DOI] [PubMed] [Google Scholar]
- 12.Butler, J. E., N. Wertz, N. Deschacht, and I. Kacskovics. 2009. Porcine IgG: structure, genetics, and evolution. Immunogenetics 61:209-230. [DOI] [PubMed] [Google Scholar]
- 13.Butler, J. E., Y. Zhao, M. Sinkora, N. Wertz, and I. Kacskovics. 2009. Immunoglobulins, antibody repertoire and B cell development. Dev. Comp. Immunol. 33:321-333. [DOI] [PubMed] [Google Scholar]
- 14.Doel, T. R. 2003. FMD vaccines. Virus Res. 91:81-99. [DOI] [PubMed] [Google Scholar]
- 15.Donaldson, A. I., and R. P. Kitching. 1989. Transmission of foot-and-mouth disease by vaccinated cattle following natural challenge. Res. Vet. Sci. 46:9-14. [PubMed] [Google Scholar]
- 16.Eblé, P. L., A. Bouma, M. G. de Bruin, F. van Hemert-Kluitenberg, J. T. van Oirschot, and A. Dekker. 2004. Vaccination of pigs two weeks before infection significantly reduces transmission of foot-and-mouth disease virus. Vaccine 22:1372-1378. [DOI] [PubMed] [Google Scholar]
- 17.Eblé, P. L., A. Bouma, K. Weerdmeester, J. A. Stegeman, and A. Dekker. 2007. Serological and mucosal immune responses after vaccination and infection with FMDV in pigs. Vaccine 25:1043-1054. [DOI] [PubMed] [Google Scholar]
- 17a.Eguchi-Ogawa, T., X.-Z. Sun, N. Wertz, H. Uenishi, F. Puimi, P. Chardon, K. Wells, G. J. Tobin, and J. E. Butler. Antibody repertoire development in fetal and neonatal piglets. XI. The relationship of VDJ usage and the genomic organization of the variable heavy chain locus. J. Immunol., in press. [DOI] [PubMed]
- 18.Golde, W. T., J. M. Pacheco, H. Duque, T. Doel, B. Penfold, G. S. Ferman, D. R. Gregg, and L. L. Rodriguez. 2005. Vaccination against foot-and-mouth disease virus confers complete clinical protection in 7 days and partial protection in 4 days: use in emergency outbreak response. Vaccine 23:5775-5782. [DOI] [PubMed] [Google Scholar]
- 19.Gorin, A. B., and J. Gould. 1979. Immunoglobulin synthesis in the lungs and caudal mediastinal lymph node of sheep. J. Immunol. 123:1339-1342. [PubMed] [Google Scholar]
- 20.Graves, J. H., P. D. McKercher, and J. J. Callis. 1972. Foot-and-mouth disease vaccine: influence of the vaccine virus subtype on neutralizing antibody and resistance to disease. Am. J. Vet. Res. 33:765-768. [PubMed] [Google Scholar]
- 21.Herrmann, J. E., R. M. Hendry, and M. F. Collins. 1979. Factors involved in enzyme-linked immunoassay of viruses and evaluation of the method for identification of enteroviruses. J. Clin. Microbiol. 10:210-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hierholzer, J. C., and R. A. Killington. 1996. Virus isolation and quantitation, p. 25-46. In B. W. Mahy and H. O. Kangro (ed.), Virology methods manual. Academic Press, Inc., San Diego, CA.
- 23.Kehoe, J. M., and J. D. Capra. 1974. Nature and significance of immunoglobulin subclasses. N. Y. State J. Med. 74:489-491. [PubMed] [Google Scholar]
- 24.Klobasa, F., F. Habe, E. Werhahn, and J. E. Butler. 1985. Changes in the concentrations of serum IgG, IgA and IgM of sows throughout the reproductive cycle. Vet. Immunol. Immunopathol. 10:341-353. [DOI] [PubMed] [Google Scholar]
- 25.McCullough, K. C., F. De Simone, E. Brocchi, L. Capucci, J. R. Crowther, and U. Kihm. 1992. Protective immune response against foot-and-mouth disease. J. Virol. 66:1835-1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moran, T. M., H. Park, A. Fernandez-Sesma, and J. L. Schulman. 1999. Th2 responses to inactivated influenza virus can be converted to Th1 responses and facilitate recovery from heterosubtypic virus infection. J. Infect. Dis. 180:579-585. [DOI] [PubMed] [Google Scholar]
- 27.Mulcahy, G., C. Gale, P. Robertson, S. Iyisan, R. D. DiMarchi, and T. R. Doel. 1990. Isotype responses of infected, virus-vaccinated and peptide-vaccinated cattle to foot-and-mouth disease virus. Vaccine 8:249-256. [DOI] [PubMed] [Google Scholar]
- 28.Müller, I., J. A. Garcia-Sanz, R. Titus, R. Behin, and J. Louis. 1989. Analysis of the cellular parameters of the immune responses contributing to resistance and susceptibility of mice to infection with the intracellular parasite, Leishmania major. Immunol. Rev. 112:95-113. [DOI] [PubMed] [Google Scholar]
- 29.Navarro, P., R. K. Christensen, P. Weber, M. Rothschild, G. Ekhardt, and J. E. Butler. 2000. Porcine IgA allotypes are not equally transcribed or expressed in heterozygous swine. Mol. Immunol. 37:653-664. [DOI] [PubMed] [Google Scholar]
- 30.Pacheco, J. M., J. Arzt, and L. L. Rodriguez. 2010. Early events in the pathogenesis of foot-and-mouth disease in cattle after controlled aerosol exposure. Vet. J. 183:46-53. [DOI] [PubMed] [Google Scholar]
- 31.Parida, S., J. Anderson, S. J. Cox, P. V. Barnett, and D. J. Paton. 2006. Secretory IgA as an indicator of oro-pharyngeal foot-and-mouth disease virus replication and as a tool for post vaccination surveillance. Vaccine 24:1107-1116. [DOI] [PubMed] [Google Scholar]
- 32.Salt, J. S., G. Mulcahy, and R. P. Kitching. 1996. Isotype-specific antibody responses to foot-and-mouth disease virus in sera and secretions of “carrier” and “non-carrier” cattle. Epidemiol. Infect. 117:349-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sher, A., R. T. Gazzinelli, I. P. Oswald, M. Clerici, M. Kullberg, E. J. Pearce, J. A. Berzofsky, T. R. Mosmann, S. L. James, and H. C. Morse III. 1992. Role of T-cell derived cytokines in the downregulation of immune responses in parasitic and retroviral infection. Immunol. Rev. 127:183-204. [DOI] [PubMed] [Google Scholar]
- 34.Sieling, P. A., and R. L. Modlin. 1994. Cytokine patterns at the site of mycobacterial infection. Immunobiology 191:378-387. [DOI] [PubMed] [Google Scholar]
- 35.van Zaane, D., and J. Ijzerman. 1984. Monoclonal antibodies against bovine immunoglobulins and their use in isotype-specific ELISAs for rotavirus antibody. J. Immunol. Methods 72:427-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang, Z. D., and R. P. Kitching. 2001. The localization of persistent foot and mouth disease virus in the epithelial cells of the soft palate and pharynx. J. Comp. Pathol. 124:89-94. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.