Abstract
In the first 6 months of the H1N1 swine-origin influenza virus (S-OIV) pandemic, the vast majority of infections were relatively mild. It has been postulated that mutations in the viral genome could result in more virulent viruses, leading to a more severe pandemic. Mutations E627K and D701N in the PB2 protein have previously been identified as determinants of avian and pandemic influenza virus virulence in mammals. These mutations were absent in S-OIVs detected early in the 2009 pandemic. Here, using reverse genetics, mutations E627K, D701N, and E677G were introduced into the prototype S-OIV A/Netherlands/602/2009, and their effects on virus replication, virulence, and transmission were investigated. Mutations E627K and D701N caused increased reporter gene expression driven by the S-OIV polymerase complex. None of the three mutations affected virus replication in vitro. The mutations had no major impact on virus replication in the respiratory tracts of mice and ferrets or on pathogenesis. All three mutant viruses were transmitted via aerosols or respiratory droplets in ferrets. Thus, the impact of key known virulence markers in PB2 in the context of current S-OIVs was surprisingly small. This study does not exclude the possibility of emergence of S-OIVs with other virulence-associated mutations in the future. We conclude that surveillance studies aimed at detecting S-OIVs with increased virulence or transmission should not rely solely on virulence markers identified in the past but should include detailed characterization of virus phenotypes, guided by genetic signatures of viruses detected in severe cases of disease in humans.
The new H1N1 swine-origin influenza virus (S-OIV) recently emerged to cause the first influenza pandemic in 40 years (2). The S-OIV presumably emerged from pigs, as its genome was shown to consist of six gene segments of “triple-reassortant” swine viruses and two of “Eurasian lineage” swine viruses (9). The start of the S-OIV pandemic has been relatively mild, with a clinical spectrum ranging from mild upper respiratory tract illness to sporadic cases of severe pneumonia leading to acute respiratory distress syndrome (22). As of 15 November 2009, worldwide, more than 206 countries have reported laboratory-confirmed cases of S-OIV infection, including over 6,770 deaths (32).
In previous influenza pandemics, such as the Spanish influenza pandemic of 1918 and the Hong Kong influenza pandemic of 1968, a first wave of cases of relatively mild illnesses was followed by more severe subsequent waves (29). The reason for this increased severity has remained largely unknown, but one possible explanation could be that the pandemic viruses required further adaptation to the human host, resulting in the emergence of viruses that were more virulent than those of the first wave. Such adaptive changes could occur by gene reassortment between cocirculating influenza A viruses or by mutation.
In the past decade, determinants of influenza A virus virulence have been mapped using reverse genetics with a variety of pandemic, epidemic, and zoonotic influenza viruses. Mutations affecting virulence and host range have frequently been mapped to hemagglutinin (HA) and neuraminidase (NA) in relation to their interaction with sialic acids, the virus receptors on host cells (11, 18, 30). Nonstructural protein 1 (NS1) has been implicated in the virulence of highly pathogenic avian influenza (HPAI) virus H5N1 and the 1918 H1N1 virus, as the NS1 proteins of these viruses were shown to act as strong antagonists of the interferon pathways (10, 25). Furthermore, the polymerase genes, in particular the PB2 gene, have been shown to be important determinants of virulence in the HPAI H5N1 and H7N7 viruses and of transmission in the 1918 H1N1 virus (11, 21, 31). One of the most commonly identified virulence markers to date is E627K in PB2. The glutamic acid (E) residue is found generally in avian influenza viruses, while human viruses have a lysine (K), and this mutation has been described as a determinant of the host range in vitro (28). When avian viruses lacking the E627K substitution were passaged in mice, the viruses acquired the mutation spontaneously upon a single passage (15, 17). In the HPAI H5N1 and H7N7 viruses, E627K was shown to be the prime determinant of pathogenesis in mice (11, 21, 23). Given that all human and many zoonotic influenza viruses of the last century contained 627K (1), it was surprising that the S-OIV had 627E.
Additionally, the aspartate (D)-to-asparagine (N) mutation at position 701 of PB2, which was shown to compensate for the absence of E627K, has also not been detected in S-OIV (27). This D701N mutation has previously been shown to expand the host range of avian H5N1 to mice and humans (3, 15) and to increase virus transmission in guinea pigs (27). Thus, S-OIV was the first known human pandemic virus with 627E and 701D, and it has been speculated that S-OIV could mutate into a more virulent form by acquiring one of these mutations, or both.
On 8 May 2009, the detection of another mutation in the PB2 gene of S-OIV, an E-to-glycine (G) mutation at position 667, was reported (http://www.promedmail.org/pls/apex/f?p=2400:1000, archive no. 20090508.1722). It has previously been suggested that the E667G substitution in PB2 of HPAI H5N1 virus was under positive selection and possibly played a role in sustainable transmission in humans (14).
On 28 September 2009, detection of the E627K mutation in PB2 of S-OIVs of two individuals in the Netherlands was reported (http://www.promedmail.org/pls/apex/f?p=2400:1000, archive no. 20090928.3394) and raised concern about the possible enhanced replication of the S-OIV in humans, possibly associated with increased virulence. To date, the D701N mutation in PB2 has not been reported in any of the S-OIVs sequenced, and additional viruses with mutation E627K have not been recorded, either. In contrast, viruses with E677G have been reported from the United States, Canada, Germany, the United Kingdom, Norway, and France, according to the public sequence databases.
Here, the effects of the E627K, D701N, and E677G mutations in the PB2 genes of S-OIVs was investigated using genetically engineered influenza viruses based on a prototype S-OIV, A/Netherlands/602/2009. Polymerase activity was measured in minigenome assays in human 293T cells, virus replication was analyzed in Madin-Darby Canine kidney (MDCK) cells, virulence was tested in mouse and ferret models, and transmission by aerosols or respiratory droplets was tested in ferrets. In contrast to the earlier assumptions based on experience with other influenza A viruses, S-OIVs with E627K, D701N, or E677G in PB2 did not show a marked increase in virulence or transmission compared to the wild-type virus.
MATERIALS AND METHODS
Cells and viruses.
MDCK cells were cultured in Eagle's minimal essential medium (EMEM) (Lonza, Breda, Netherlands) supplemented with 10% fetal calf serum (FCS), 100 IU/ml penicillin, 100 μg/ml streptomycin, 2 mM glutamine, 1.5 mg/ml sodium bicarbonate (Cambrex), 10 mM HEPES (Lonza), and nonessential amino acids (MP Biomedicals Europe, Illkirch, France). 293T cells were cultured in Dulbecco's modified Eagle's medium (DMEM) (Lonza) supplemented with 10% FCS, 100 IU/ml penicillin, 100 mg/ml streptomycin, 2 mM glutamine, 1 mM sodium pyruvate, and nonessential amino acids.
Influenza virus A/Netherlands/602/09 was isolated from the first patient with S-OIV infection in the Netherlands (20). All eight gene segments of this virus were amplified by reverse transcription-PCR, cloned in a modified version of the bidirectional reverse-genetics plasmid pHW2000 (5, 12), and subsequently used to generate recombinant virus by reverse genetics as described elsewhere (5). The mutations of interest (E627K, E677G, and D701N) were introduced into the PB2 gene using the QuikChange multisite-directed mutagenesis kit (Stratagene, Leusden, Netherlands) according to the instructions of the manufacturer, resulting in recombinant viruses NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N. The presence of each mutation was confirmed by sequencing.
Virus titrations.
Virus titers in nasal and throat swabs, homogenized organ samples, or samples for replication curves were determined by endpoint titration in MDCK cells. MDCK cells were inoculated with 10-fold serial dilutions of each sample, washed 1 h postinoculation (p.i.) with phosphate-buffered saline (PBS), and grown in 200 μl of infection medium, consisting of EMEM supplemented with 100 U/ml penicillin, 100 μg/ml streptomycin, 2 mM glutamine, 1.5 mg/ml sodium bicarbonate, 10 mM HEPES, nonessential amino acids, and 20 μg/ml trypsin (Lonza). Three days after inoculation, the supernatants of inoculated cell cultures were tested for agglutinating activity using turkey erythrocytes as an indicator of virus replication in the cells. Infectious-virus titers were calculated from 4 (homogenized tissues and swabs) or 5 (samples from replication curves) replicates by the method of Spearman and Karber (13).
Minigenome assays.
A model viral RNA (vRNA), consisting of the firefly luciferase open reading frame flanked by the noncoding regions (NCRs) of segment 8 of influenza A virus, under the control of a T7 RNA polymerase promoter was used for minigenome assays (4). The reporter plasmid (0.5 μg) was transfected into 293T cells in 6-well plates, along with 0.5 μg of each of the pHW2000 plasmids encoding PB2, PB1, PA, and NP; 1 μg of pAR3132 expressing T7 RNA polymerase (6); and 0.02 μg of the Renilla luciferase expression plasmid pRL (Promega, Leiden, Netherlands) as an internal control. Twenty-four hours after transfection, luminescence was measured using a Dual-Glo Luciferase Assay System (Promega) according to the instructions of the manufacturer in a TECAN Infinite F200 machine (Tecan Benelux bv, Giessen, Netherlands). Relative light units (RLU) were calculated as the ratio of firefly and Renilla luciferase luminescences.
Replication curves.
Multicycle replication curves were generated by inoculating MDCK cells at a multiplicity of infection (MOI) of 0.01 50% tissue culture infectious dose (TCID50) per cell. One hour after inoculation, at time point 0, the cells were washed once with PBS, and fresh infection medium was added. The supernatants were sampled at 6, 12, 24, and 48 h postinfection, and the virus titers in these supernatants were determined by means of endpoint titration in MDCK cells.
Animal experiments.
All animal studies were approved by an independent animal ethics committee. All experiments were performed under animal biosafety level 3+ conditions.
Groups of six 5-week-old female BALB/c mice were inoculated intranasally with 5 × 104 TCID50 of NL602, NL602/PB2-627K, NL602/PB2-677G, or NL602/PB2-701N, and their bodyweights, as an indicator of disease, were recorded daily until 14 days p.i. In a second experiment, three animals from each group were euthanized at 3 and 6 days p.i., and their lungs were collected and subsequently homogenized for virus titration. Virus titers were determined by endpoint titration in MDCK cells.
The ferret model to test the pathogenicity and transmission of S-OIV was described previously (20). To study pathogenesis, groups of six influenza virus-seronegative 6-month-old female ferrets (Mustella putorius furo) were inoculated intranasally with 106 TCID50 of NL602, NL602/PB2-627K, NL602/PB2-677G, or NL602/PB2-701N divided over both nostrils (2 × 250 μl). We had previously found that this virus dose of S-OIV was not lethal to ferrets and allowed the assessment of quantitative differences in virus replication (20). Throat and nasal swabs were collected daily to determine virus excretion from the upper respiratory tract. The animals were observed for clinical symptoms and weighed daily as an indicator of disease. Three animals from each group were euthanized at 3 and 7 days p.i., and the nasal turbinates, trachea, lungs, liver, spleen, kidney, colon, and brain were collected to study virus distribution.
In the transmission experiment, four female ferrets, individually housed in transmission cages, were inoculated intranasally with 106 TCID50 of NL602, NL602/PB2-627K, NL602/PB2-677G, or NL602/PB2-701N divided over both nostrils (2 × 250 μl). At 1 day p.i., four naïve ferrets were individually placed in a transmission cage adjacent to an inoculated ferret, separated by two stainless steel grids to allow airflow from the inoculated to the naive ferret but to prevent direct contact and fomite transmission. Nasal and throat swabs were collected at 0, 1, 2, 3, 5, and 7 days p.i. from inoculated ferrets and at 0, 1, 2, 3, 5, and 7 days postexposure (p.e.) for the naïve animals. The inoculated ferrets were euthanized at 7 days p.i., and naive ferrets that were found positive by reverse transcription-PCR (7) at 7 days p.e. were also euthanized. Naïve animals that remained negative for virus excretion throughout the experiment were euthanized at 15 days p.e., and a blood sample was collected for serology. The virus titers in the collected swabs and tissue homogenates were determined by means of endpoint titration in MDCK cells.
RESULTS
Minigenome assays.
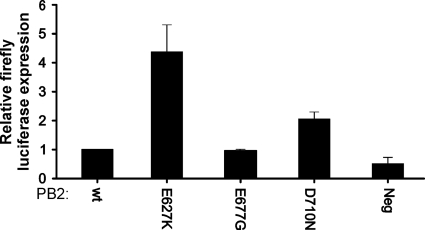
Minigenome assays were used to study the effects of three amino acid substitutions in the PB2 gene, E627K, E677G, and D701N, on the activity of the influenza virus polymerase complex. These assays employ a model vRNA consisting of the firefly luciferase open reading frame flanked by the NCRs of segment 8 of influenza A virus (4). Upon cotransfection of the vRNA reporter construct with plasmids expressing the influenza virus PB2, PB1, PA, and NP proteins, negative-sense vRNA is copied to positive-sense cRNA and mRNA, and the firefly luciferase protein is expressed. A plasmid that constitutively expresses Renilla luciferase was cotransfected as an internal control to standardize the transfection efficiency and sample processing. Introduction of the E627K and D701N mutations in PB2 yielded expression levels of the reporter protein that were 4.4- and 2.0-fold higher, respectively, than in experiments with the wild-type PB2 (Fig. 1). Introduction of the E677G mutation into PB2 did not result in altered expression levels of the reporter protein. Thus, introduction of the E627K and D701N mutations, known to be responsible for adaptation to replication in humans, resulted in elevated polymerase activity in vitro.
FIG. 1.
Activity of the NL602 polymerase complex with wild type (wt) PB2, PB2-E627K, PB2-E677G, and PB2-D701N in minigenome assays. Firefly luciferase was expressed from a synthetic viral RNA when the influenza virus polymerase complex was present. The luminescence of the firefly luciferase reporter was standardized using a plasmid constitutively expressing Renilla luciferase protein to correct for differences in transfection efficiencies and sample processing. Relative luminescence was calculated as the percent relative light units (firefly luciferase/Renilla luciferase), and the fold difference in reporter protein expression was calculated with the wild-type polymerase complex as a reference. Averages and standard deviations from two independent experiments performed in duplicate are shown. Neg, negative control.
Replication kinetics.
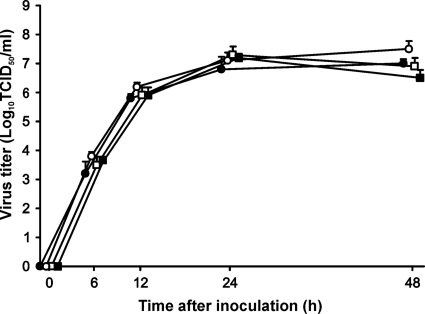
The multicycle replication kinetics of wild-type and PB2 mutant viruses were studied in vitro. To this end, recombinant viruses with and without the mutations in PB2 were generated in 293T cells by reverse genetics, and virus stocks were propagated and titrated in MDCK cells. Subsequently, MDCK cells were infected at an MOI of 0.01, after which the supernatants were harvested at fixed time points and the viral titers were determined in MDCK cells. The replication kinetics of the wild-type virus and the three mutant viruses were similar, with a maximum difference in the virus titer of 0.5 log10 TCID50, which is not statistically significant (Fig. 2).
FIG. 2.
Replication kinetics of NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses in MDCK cells. MDCK cells were inoculated with 0.01 TCID50/cell of the NL602 (closed circles), NL602/PB2-627K (open circles), NL602/PB2-677G (closed squares), and NL602/PB2-701N (open squares) viruses, and supernatant samples were harvested 6, 12, 24, and 48 h later. The supernatant samples were titrated in MDCK cells. Geometric mean titers and standard deviations were calculated from two independent experiments.
Mouse experiments.
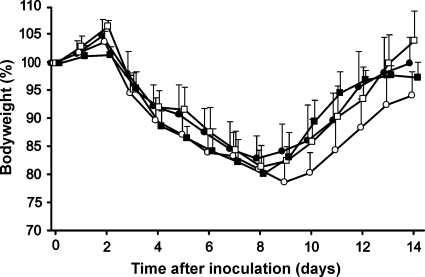
To study pathogenesis in mice, groups of five or six BALB/c mice were inoculated intranasally with 5 × 104 TCID50 of each virus and weighed daily as an indicator of disease. Mice in all four groups lost body weight at approximately the same rate in the first 8 days p.i. One out of five and two out of six animals inoculated with NL602/PB2-627K or NL602/PB2-677G, respectively, showed more than 25% bodyweight loss at 8 days p.i. and were euthanized for ethical reasons. In the week following 8 days p.i., the body weights of all remaining mice returned to normal levels. Mice inoculated with NL602/PB2-627K showed a 2-day delay in this recovery compared to mice inoculated with the other viruses in the study (Fig. 3).
FIG. 3.
Weight loss of BALB/c mice inoculated with NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses. Mean bodyweights and standard deviations were calculated as percentages of bodyweight compared to bodyweight at the time of inoculation for each group inoculated with NL602 (closed circles), NL602/PB2-627K (open circles), NL602/PB2-677G (closed squares), and NL602/PB2-701N (open squares) viruses.
In a second experiment, groups of six mice were inoculated intranasally with 5 × 104 TCID50 of NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N. The lung virus titers were determined at 3 and 6 days p.i. by titration of lung homogenates in MDCK cells. Lung virus titers for the NL602/PB2-627K- and NL602/PB2-677G-inoculated groups were approximately 0.5 log10 TCID50 higher than for the NL602- and NL602/PB2-701N-inoculated groups at 3 days p.i.. At 6 days p.i., the lung virus titers for the NL602/PB2-677G group were 0.7 log10 TCID50 higher than for the NL602 group (Table 1). Although there were small differences between the groups inoculated with the wild-type and mutant viruses, these differences were not statistically significant.
TABLE 1.
Virus titers in the lungs of BALB/c mice inoculated with NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses
| Time after inoculation (days) | Virus titer (log10 TCID50/g of tissue)a |
|||
|---|---|---|---|---|
| NL602 | NL602/PB2-627K | NL602/PB2-677G | NL602/PB2-701N | |
| 3 | 6.0 ± 0.3 | 6.4 ± 0.5 | 6.5 ± 0.4 | 6.0 ± 0.3 |
| 6 | 4.9 ± 0.3 | 4.9 ± 0.2 | 5.6 ± 0.8 | 5.3 ± 0.4 |
Geometric mean titers ± standard deviations are given.
Pathogenesis experiments in ferrets.
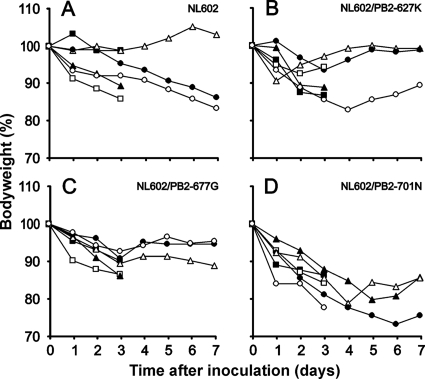
Groups of six ferrets were inoculated intranasally with 106 TCID50 of NL602, NL602/PB2-627K, NL602/PB2-677G, or NL602/PB2-701N. The animals were weighed daily as an indicator of disease. The mean maximum weight loss, referring to the day on which this mean weight loss for each group of ferrets was highest, was 7% for animals inoculated with the NL602 virus. Animals inoculated with NL602/E627K or NL602/PB2-677G had mean maximum weight losses of 9% and 11%, respectively (Fig. 4). Animals inoculated with NL602/PB2-701N experienced the highest mean weight loss, which was reached at 6 days p.i., in contrast to the peak in weight loss for animals inoculated with the other viruses, which was reached at 3 days p.i. Over the first 3 days, a statistically significant difference was observed in weight loss in animals inoculated with NL602/PB2-701N compared to NL602-inoculated animals as calculated from the “area under the curve” (Mann-Whitney; P = 0.026). These results suggest a more virulent phenotype for the NL602/PB2-701N virus, or at least slower recovery upon inoculation with the virus. However, no marked differences were observed for other clinical parameters, such as lethargy, sneezing, ruffled fur, interest in food, and runny nose, between the four groups of ferrets.
FIG. 4.
Weight loss of ferrets inoculated with NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses. Bodyweight is depicted as percentage of bodyweight at time of inoculation. Data are shown for individual animals until the animals were euthanized at 3 or 7 days p.i.
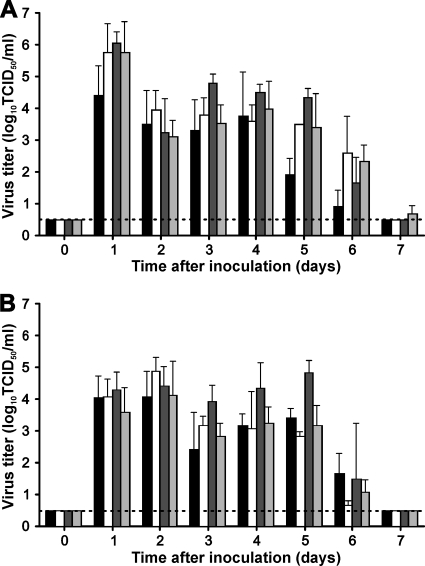
Nose and throat swabs were collected from inoculated animals daily, and virus titers were determined by endpoint titration in MDCK cells. Infectious-virus shedding was demonstrated from 1 day p.i. onward and continued until 6 days p.i. in both the noses and the throats of ferrets inoculated with each of the four viruses (Fig. 5). Overall, only minor differences in virus shedding between the different groups were observed. The total amount of virus shed from the throat and nose during the first 3 days, as calculated from the area under the curve, was higher in animals inoculated with NL602/PB2-627K and NL602/PB2-677G than in animals inoculated with NL602 (Mann-Whitney; P = 0.041 and P = 0.020 for throat swabs, respectively; P = 0.041 for nose swabs of both groups). However, during the entire 1-week period, differences in virus shedding were minimal and did not reach statistical significance, except for slightly higher virus shedding in the throat for animals inoculated with NL602/PB2-677G (Mann-Whitney; P = 0.033).
FIG. 5.
Virus shedding from the upper respiratory tract of ferrets inoculated with NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses. Virus detection in throat swabs (A) and nose swabs (B) is indicated for NL602 (black bars), NL602/PB2-627K (white bars), NL602/PB2-677G (dark-gray bars), and NL602/PB2-701N (light-gray bars). Geometric mean titers for positive samples are displayed, and the error bars indicate the standard deviations. The lower limits of detection are indicated by the dotted lines.
At 3 and 7 days p.i., three ferrets from each group were euthanized, and the nasal turbinates, trachea, lungs, brain, liver, spleen, kidney, and colon were collected for virological examination. Parts of the collected tissues were homogenized, and virus titers were determined by titration in MDCK cells. Virus was detected in the respiratory tracts (nasal turbinates, trachea, and lungs) at 3 days p.i. in 3/3 animals that were inoculated with the NL602 and NL602/PB2-701N viruses (Table 2) and in 2/3 animals inoculated with NL602/PB2-677G and NL602/PB2-627K. At 7 days p.i., no virus was detected in animals inoculated with NL602/PB2-627K, whereas in the groups inoculated with NL602, NL602/PB2-677G, and NL602/PB2-701N, in two, one, or three animals, respectively, virus was detected in the respiratory tract (Table 2). Virus titers in the respiratory tract at 3 and 7 days p.i. were similar for all groups of ferrets. Virus was not detected in any of the organs outside the respiratory tract for these animals.
TABLE 2.
Virus titers in the respiratory tracts of ferrets inoculated with NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses
| Tissue | Virus titer (log10 TCID50/g tissue)a |
|||||||
|---|---|---|---|---|---|---|---|---|
| 3 days p.i. |
7 days p.i. |
|||||||
| NL602 | NL602 627K | NL602 677G | NL602 701N | NL602 | NL602 627K | NL602 677G | NL602 701N | |
| NT | 6.9 ± 0.3 (3/3) | 7.2 ± 0.6 (3/3) | 6.8 ± 0.5 (3/3) | 6.7 ± 0.6 (3/3) | 4.4 ± 0.7 (2/3) | ND | 6.8 (1/3) | 4.9 ± 1.3 (3/3) |
| Trachea | 5.0 ± 0.7 (3/3) | 4.4 ± 1.0 (3/3) | 5.3 ± 0.5 (2/3) | 5.1 ± 1.0 (3/3) | 2.4 (1/3) | ND | ND | 2.1 (1/3) |
| Lung | 5.6 ± 0.9 (3/3) | 5.4 ± 0.7 (2/3) | 4.8 ± 0.3 (2/3) | 4.9 ± 1.1 (3/3) | 1.5 (1/3) | ND | ND | ND |
Geometric mean titers of positive samples ± standard deviations are given, and the numbers of positive animals are indicated in parentheses. ND, not detected. The detection levels for nasal turbinates (NT), trachea, and lung were <1.5, <1.5, and <1 log10 TCID50/g tissue, respectively.
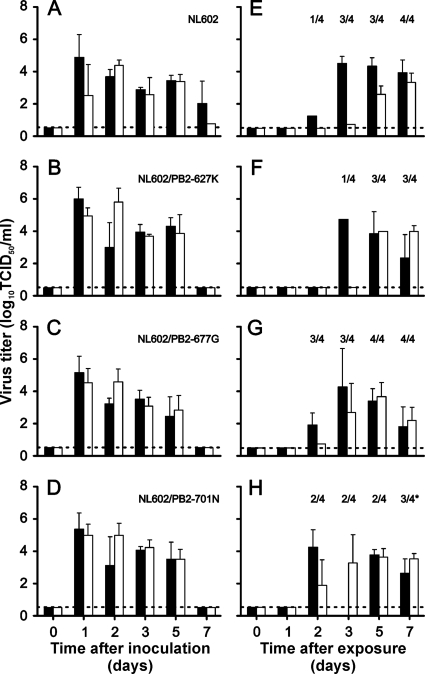
Transmission experiments in ferrets.
Aerosol or respiratory droplet transmission of the NL602 and mutant viruses was tested in the ferret model. Four individually housed ferrets were inoculated with each virus, and naïve animals were placed in a cage adjacent to each inoculated ferret at 1 day p.i. The experimental setup was designed to prevent direct contact or carryover of cage bedding but to allow airflow, thereby permitting transmission via aerosols or respiratory droplets. The inoculated ferrets started to shed virus at 1 day p.i., with virus titers up to 106 TCID50/ml in throat and nose swabs (Fig. 6). The naïve ferrets became infected as a result of aerosol or respiratory droplet transmission 2 or 3 days p.e. In the naïve animals, virus was detected in two (NL602/PB2-701N), three (NL602/PB2-627K), or four (NL602 and NL602/PB2-677G) out of four animals. In addition, one animal that was placed adjacent to a ferret inoculated with NL602/PB2-701N seroconverted in the course of the experiment, despite the fact that infectious-virus shedding was not demonstrated in the nose or throat during the first week.
FIG. 6.
Transmission of NL602, NL602/PB2-627K, NL602/PB2-677G, and NL602/PB2-701N viruses by aerosol or respiratory droplets in ferrets. Virus titers in throat (black bars) and nose (white bars) swabs are displayed for inoculated (A to D) and exposed (E to H) ferrets. The geometric mean titers of positive samples are displayed, and the error bars indicate the standard deviations. The number of positive contact animals per day is depicted. The asterisk indicates that one ferret was negative for virus shedding but seroconverted to influenza A virus nucleoprotein in the course of the experiment. The lower limits of detection are indicated by the dotted lines.
DISCUSSION
Here, using recombinant viruses generated with reverse genetics, the impact of three amino acid substitutions in PB2 on S-OIV replication, pathogenesis in animal models, and transmission was evaluated. The E627K and D701N substitutions were previously shown to be important for adaptation of avian influenza viruses to the human host, and the E627K and E677G substitutions were detected recently in patients with S-OIV infection. In vitro, the E627K and D701N amino acid substitutions in PB2 of S-OIV resulted in enhanced minigenome reporter expression compared to the wild-type PB2, but not in enhanced replication kinetics in MDCK cells. This apparent discrepancy between the minigenome reporter assay and the in vitro virus replication assay may be related to the different parameters under investigation; whereas mRNA synthesis and reporter protein expression is the primary readout in minigenome assays, for efficient virus replication, a proper balance between the syntheses of cRNA, vRNA, and mRNA is required.
In a mouse model, slightly elevated levels of virus replication were detected at 3 days p.i. in the lungs of animals inoculated with NL602/PB2-627K, and these animals showed a 2-day delay in regaining bodyweight. Mice inoculated with NL602/PB2-677G had slightly elevated levels of virus replication in the lungs at both 3 and 6 days p.i., which was not reflected by changes in bodyweight. In the ferret model, animals inoculated with the NL602/PB2-701N virus lost significantly more bodyweight than ferrets inoculated with the other viruses. Although this could suggest more severe disease, it should be noted that variation in bodyweight loss was relatively high between individual ferrets (Fig. 4). The groups of ferrets were too small to detect statistically significant differences after 3 days p.i., when only 3 animals remained in the experiment. Major differences between the four groups of ferrets were not observed for other clinical parameters, such as lethargy, sneezing, ruffled fur, interest in food, and runny nose. This was in agreement with the virus titers in the respiratory tracts of inoculated animals, which were largely comparable for all groups. Minor variations in virus shedding, however, were also observed in ferrets; in throat swab samples, higher levels of virus shedding were detected for each of the PB2 mutants at 5 and 6 days p.i., and virus shedding from the throat was higher for animals inoculated with NL602/PB2-677G throughout the time course of this experiment.
It is unclear which of these observations has implications for infections of humans with S-OIVs. It is possible that S-OIVs with mutations in PB2 would also result in differences in virus replication in the human upper or lower respiratory tract and perhaps in differences in pathogenesis and transmission. However, from the accumulated data, we conclude that none of the tested mutations in PB2 had a major impact on the virulence of A/Netherlands/602/2009 in mice and ferrets. Certainly, for E627K and D701N, this was in contrast to our expectations, because a large impact of these mutations was observed in the context of other influenza viruses in mice and ferrets. In mice infected with HPAI A/Netherlands/219/2003 (H7N7) virus, PB2 E627K was the main determinant of pathogenicity, related to >1,000-fold differences in lung virus titers (21). Adaptation of A/Equine/London/1416/73 (H7N7) to mice resulted, among others, in an E627K substitution in PB2, leading to 1,000-fold-increased virulence of the virus as measured by the dose lethal to 50% of infected mice (MLD50) (26). The PB2 E627K mutation was also the main determinant of differences in pathogenicity of 1997 HPAI H5N1 viruses, in which the MLD50 changed >1,000-fold upon introduction of the mutation (11). In HPAI H5N1 viruses isolated from ducks in China, D701N was the main determinant of pathogenesis in the mouse model (15). The pathogenicity of a variant of A/seal/Massachusetts/1/1980 (H7N7) that is highly pathogenic to mice, SC35, was also determined in part by D701N in PB2 (8). Thus, the mouse model seems appropriate for testing the effects of both E627K and D701N in PB2, yet in the context of A/Netherlands/602/2009 (S-OIV), there was no such marked effect of these mutations on pathogenesis.
Ferrets are generally considered a more suitable animal model for influenza A virus infections in humans because they are susceptible to natural infection and develop respiratory disease and lung pathology similar to those of humans when suffering from seasonal, avian, or pandemic influenza virus infections (16). Ferrets have also been used previously to map determinants of influenza virus pathogenicity and transmission to the PB2 gene (24, 31). However, there was no major effect on pathogenesis and transmission of A/Netherlands/602/2009 from any of the three PB2 mutations tested. Transmission was detected in 3 or 4 out of 4 animals that were placed adjacent to animals inoculated with viruses containing the PB2 mutations. For comparison, NL602 was transmitted to 4 out of 4 animals. The ferret transmission model was designed as a qualitative model for virus transmission via aerosols or respiratory droplets. With the limited number of animals in this experiment, quantitative information on virus transmission, with statistical support, could not be obtained. Therefore, we merely conclude from the experiment that the S-OIVs with and without mutations in PB2 were all transmitted via aerosols or respiratory droplets.
The polymerase complex of the S-OIV originated from triple-reassortant swine viruses, the PB2 gene of which is of avian origin and entered pigs around 1998 (9, 33). The fact that this avian-origin PB2 gene did not significantly benefit from the substitutions E627K and D701N for enhanced replication in mammals suggests that other mutations in the polymerase complex can compensate. It will be important to map which genetic changes in the polymerase complex of S-OIV facilitate efficient replication in mammalian cells in the absence of E627K and D701N in PB2, as this may reveal yet-unidentified virulence or host adaptation markers of influenza A virus. A recent study suggested a role for a PB2 SR polymorphism present in S-OIV, since mutation of this SR polymorphism to the consensus G590Q591 sequence resulted in reduced polymerase activity in human cells in vitro (19). Animal experiments are needed to elucidate the role of SR polymorphisms in vivo.
Although the PB2 mutations tested did not increase the pathogenicity of S-OIV in our experiments, it cannot be concluded that they will not affect virulence in the future. Because the mutations did not impair replication and transmission significantly, they could reemerge in the future in a different viral genetic background in which they could possibly give rise to more virulent strains. The present study implies that surveillance activities should not remain limited to known virulence factors but should include studies to search for new virulence markers. Surveillance studies should additionally focus on genetic signatures in S-OIVs that are associated with severe disease in humans and on the testing of mutations in several pathogenesis models, as described here.
More research is also needed to test the effects of additional known virulence markers in the polymerase genes or, for instance, in the HA, NA, NS1, or PB1-F2 protein. Furthermore, altered virulence of S-OIV may result not only from mutation, but also upon gene reassortment with contemporary seasonal H1N1 and H3N2 viruses, which could result in enhanced virulence and transmission. Further laboratory investigations and enhanced surveillance activities to detect the emergence of new S-OIV genotypes and phenotypes are needed to determine their importance for public health and to identify a potential need for intensification of surveillance.
Acknowledgments
We thank Geert van Amerongen, Dennis de Meulder, Dennis Akkermans, and Robert Dias-D'Ullois for technical assistance.
This work was financed through NIAID-NIH contract HHSN266200700010C.
Footnotes
Published ahead of print on 3 February 2010.
REFERENCES
- 1.Chen, G. W., S. C. Chang, C. K. Mok, Y. L. Lo, Y. N. Kung, J. H. Huang, Y. H. Shih, J. Y. Wang, C. Chiang, C. J. Chen, and S. R. Shih. 2006. Genomic signatures of human versus avian influenza A viruses. Emerg. Infect. Dis. 12:1353-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dawood, F. S., S. Jain, L. Finelli, M. W. Shaw, S. Lindstrom, R. J. Garten, L. V. Gubareva, X. Xu, C. B. Bridges, and T. M. Uyeki. 2009. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 360:2605-2615. [DOI] [PubMed] [Google Scholar]
- 3.de Jong, M. D., C. P. Simmons, T. T. Thanh, V. M. Hien, G. J. Smith, T. N. Chau, D. M. Hoang, N. V. Chau, T. H. Khanh, V. C. Dong, P. T. Qui, B. V. Cam, Q. H. Do, Y. Guan, J. S. Peiris, N. T. Chinh, T. T. Hien, and J. Farrar. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Wit, E., V. J. Munster, D. van Riel, W. E. P. Beyer, G. F. Rimmelzwaan, T. Kuiken, A. D. M. E. Osterhaus, and R. A. M. Fouchier. 2010. Molecular determinants of adaptation of highly pathogenic avian influenza H7N7 viruses to efficient replication in the human host. J. Virol. 84:1597-1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Wit, E., M. I. Spronken, T. M. Bestebroer, G. F. Rimmelzwaan, A. D. Osterhaus, and R. A. Fouchier. 2004. Efficient generation and growth of influenza virus A/PR/8/34 from eight cDNA fragments. Virus Res. 103:155-161. [DOI] [PubMed] [Google Scholar]
- 6.Dunn, J. J., B. Krippl, K. E. Bernstein, H. Westphal, and F. W. Studier. 1988. Targeting bacteriophage T7 RNA polymerase to the mammalian cell nucleus. Gene 68:259-266. [DOI] [PubMed] [Google Scholar]
- 7.Fouchier, R. A., T. M. Bestebroer, S. Herfst, L. Van Der Kemp, G. F. Rimmelzwaan, and A. D. Osterhaus. 2000. Detection of influenza A viruses from different species by PCR amplification of conserved sequences in the matrix gene. J. Clin. Microbiol. 38:4096-4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabriel, G., B. Dauber, T. Wolff, O. Planz, H. D. Klenk, and J. Stech. 2005. The viral polymerase mediates adaptation of an avian influenza virus to a mammalian host. Proc. Natl. Acad. Sci. U. S. A. 102:18590-18595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garten, R. J., C. T. Davis, C. A. Russell, B. Shu, S. Lindstrom, A. Balish, W. M. Sessions, X. Xu, E. Skepner, V. Deyde, M. Okomo-Adhiambo, L. Gubareva, J. Barnes, C. B. Smith, S. L. Emery, M. J. Hillman, P. Rivailler, J. Smagala, M. de Graaf, D. F. Burke, R. A. Fouchier, C. Pappas, C. M. Alpuche-Aranda, H. Lopez-Gatell, H. Olivera, I. Lopez, C. A. Myers, D. Faix, P. J. Blair, C. Yu, K. M. Keene, P. D. Dotson, Jr., D. Boxrud, A. R. Sambol, S. H. Abid, K. St George, T. Bannerman, A. L. Moore, D. J. Stringer, P. Blevins, G. J. Demmler-Harrison, M. Ginsberg, P. Kriner, S. Waterman, S. Smole, H. F. Guevara, E. A. Belongia, P. A. Clark, S. T. Beatrice, R. Donis, J. Katz, L. Finelli, C. B. Bridges, M. Shaw, D. B. Jernigan, T. M. Uyeki, D. J. Smith, A. I. Klimov, and N. J. Cox. 2009. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science 325:197-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geiss, G. K., M. Salvatore, T. M. Tumpey, V. S. Carter, X. Wang, C. F. Basler, J. K. Taubenberger, R. E. Bumgarner, P. Palese, M. G. Katze, and A. Garcia-Sastre. 2002. Cellular transcriptional profiling in influenza A virus-infected lung epithelial cells: the role of the nonstructural NS1 protein in the evasion of the host innate defense and its potential contribution to pandemic influenza. Proc. Natl. Acad. Sci. U. S. A. 99:10736-10741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatta, M., P. Gao, P. Halfmann, and Y. Kawaoka. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293:1840-1842. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karber, G. 1931. Beitrag zur kollektiven behandlung pharmakologischer reihenversuche. Exp. Pathol. Pharmakol. 162:480-483. [Google Scholar]
- 14.Lam, T. T., C. C. Hon, O. G. Pybus, S. L. Kosakovsky Pond, R. T. Wong, C. W. Yip, F. Zeng, and F. C. Leung. 2008. Evolutionary and transmission dynamics of reassortant H5N1 influenza virus in Indonesia. PLoS Pathog. 4:e1000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li, Z., H. Chen, P. Jiao, G. Deng, G. Tian, Y. Li, E. Hoffmann, R. G. Webster, Y. Matsuoka, and K. Yu. 2005. Molecular basis of replication of duck H5N1 influenza viruses in a mammalian mouse model. J. Virol. 79:12058-12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maher, J. A., and J. DeStefano. 2004. The ferret: an animal model to study influenza virus. Lab. Anim. 33:50-53. [DOI] [PubMed] [Google Scholar]
- 17.Mase, M., N. Tanimura, T. Imada, M. Okamatsu, K. Tsukamoto, and S. Yamaguchi. 2006. Recent H5N1 avian influenza A virus increases rapidly in virulence to mice after a single passage in mice. J. Gen. Virol. 87:3655-3659. [DOI] [PubMed] [Google Scholar]
- 18.Matsuoka, Y., D. E. Swayne, C. Thomas, M. A. Rameix-Welti, N. Naffakh, C. Warnes, M. Altholtz, R. Donis, and K. Subbarao. 2009. Neuraminidase stalk length and additional glycosylation of the hemagglutinin influence the virulence of influenza H5N1 viruses for mice. J. Virol. 83:4704-4708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehle, A., and J. A. Doudna. 2009. Adaptive strategies of the influenza virus polymerase for replication in humans. Proc. Natl. Acad. Sci. U. S. A. 106:21312-21316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Munster, V. J., E. de Wit, J. M. van den Brand, S. Herfst, E. J. Schrauwen, T. M. Bestebroer, D. van de Vijver, C. A. Boucher, M. Koopmans, G. F. Rimmelzwaan, T. Kuiken, A. D. Osterhaus, and R. A. Fouchier. 2009. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science 325:481-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Munster, V. J., E. de Wit, D. van Riel, W. E. Beyer, G. F. Rimmelzwaan, A. D. Osterhaus, T. Kuiken, and R. A. Fouchier. 2007. The molecular basis of the pathogenicity of the Dutch highly pathogenic human influenza A H7N7 viruses. J. Infect. Dis. 196:258-265. [DOI] [PubMed] [Google Scholar]
- 22.Perez-Padilla, R., D. de la Rosa-Zamboni, S. Ponce de Leon, M. Hernandez, F. Quinones-Falconi, E. Bautista, A. Ramirez-Venegas, J. Rojas-Serrano, C. E. Ormsby, A. Corrales, A. Higuera, E. Mondragon, J. A. Cordova-Villalobos, and the International Working Group on Influenza. 2009. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N. Engl. J. Med. 361:680-689. [DOI] [PubMed] [Google Scholar]
- 23.Rigoni, M., K. Shinya, A. Toffan, A. Milani, F. Bettini, Y. Kawaoka, G. Cattoli, and I. Capua. 2007. Pneumo- and neurotropism of avian origin Italian highly pathogenic avian influenza H7N1 isolates in experimentally infected mice. Virology 364:28-35. [DOI] [PubMed] [Google Scholar]
- 24.Salomon, R., J. Franks, E. A. Govorkova, N. A. Ilyushina, H. L. Yen, D. J. Hulse-Post, J. Humberd, M. Trichet, J. E. Rehg, R. J. Webby, R. G. Webster, and E. Hoffmann. 2006. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. J. Exp. Med. 203:689-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seo, S. H., E. Hoffmann, and R. G. Webster. 2002. Lethal H5N1 influenza viruses escape host anti-viral cytokine responses. Nat. Med. 8:950-954. [DOI] [PubMed] [Google Scholar]
- 26.Shinya, K., S. Watanabe, T. Ito, N. Kasai, and Y. Kawaoka. 2007. Adaptation of an H7N7 equine influenza A virus in mice. J. Gen. Virol. 88:547-553. [DOI] [PubMed] [Google Scholar]
- 27.Steel, J., A. C. Lowen, S. Mubareka, and P. Palese. 2009. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 5:e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Subbarao, E. K., W. London, and B. R. Murphy. 1993. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 67:1761-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taubenberger, J. K., A. H. Reid, and T. G. Fanning. 2000. The 1918 influenza virus: a killer comes into view. Virology 274:241-245. [DOI] [PubMed] [Google Scholar]
- 30.Tumpey, T. M., T. R. Maines, N. Van Hoeven, L. Glaser, A. Solorzano, C. Pappas, N. J. Cox, D. E. Swayne, P. Palese, J. M. Katz, and A. Garcia-Sastre. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655-659. [DOI] [PubMed] [Google Scholar]
- 31.Van Hoeven, N., C. Pappas, J. A. Belser, T. R. Maines, H. Zeng, A. Garcia-Sastre, R. Sasisekharan, J. M. Katz, and T. M. Tumpey. 2009. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc. Natl. Acad. Sci. U. S. A. 106:3366-3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WHO. 2009. Influenza A (H1N1), update 75. WHO, Geneva, Switzerland. http://www.who.int/csr/don/2009_11_20a/en/index.html.
- 33.Zhou, N. N., D. A. Senne, J. S. Landgraf, S. L. Swenson, G. Erickson, K. Rossow, L. Liu, K. Yoon, S. Krauss, and R. G. Webster. 1999. Genetic reassortment of avian, swine, and human influenza A viruses in American pigs. J. Virol. 73:8851-8856. [DOI] [PMC free article] [PubMed] [Google Scholar]