Abstract
Cytotoxicity and proliferation capacity are key functions of antiviral CD8 T cells. In the present study, we investigated a series of markers to define these functions in virus-specific CD8 T cells. We provide evidence that there is a lack of coexpression of perforin and CD127 in human CD8 T cells. CD127 expression on virus-specific CD8 T cells correlated positively with proliferation capacity and negatively with perforin expression and cytotoxicity. Influenza virus-, cytomegalovirus-, and Epstein-Barr virus/human immunodeficiency virus type 1-specific CD8 T cells were predominantly composed of CD127+ perforin−/CD127− perforin+, and CD127−/perforin− CD8 T cells, respectively. CD127−/perforin− and CD127−/perforin+ cells expressed significantly more PD-1 and CD57, respectively. Consistently, intracellular cytokine (gamma interferon, tumor necrosis factor alpha, and interleukin-2 [IL-2]) responses combined to perforin detection confirmed that virus-specific CD8 T cells were mostly composed of either perforin+/IL-2− or perforin−/IL-2+ cells. In addition, perforin expression and IL-2 secretion were negatively correlated in virus-specific CD8 T cells (P < 0.01). As previously shown for perforin, changes in antigen exposure modulated also CD127 expression. Based on the above results, proliferating (CD127+/IL-2-secreting) and cytotoxic (perforin+) CD8 T cells were contained within phenotypically distinct T-cell populations at different stages of activation or differentiation and showed different levels of exhaustion and senescence. Furthermore, the composition of proliferating and cytotoxic CD8 T cells for a given antiviral CD8 T-cell population appeared to be influenced by antigen exposure. These results advance our understanding of the relationship between cytotoxicity, proliferation capacity, the levels of senescence and exhaustion, and antigen exposure of antiviral memory CD8 T cells.
Cytotoxic CD8 T cells are a fundamental component of the immune response against viral infections and mediate an important role in immunosurveillance (7, 10, 55), and the induction of vigorous CD8 T-cell responses after vaccination is thought to be a key component of protective immunity (37, 41, 49, 50, 58, 60, 69). Cytotoxic CD8 T cells exert their antiviral and antitumor activity primarily through the secretion of cytotoxic granules containing perforin (pore-forming protein) and several granule-associated proteases, including granzymes (Grms) (5, 15, 20, 44). Several studies have recently advanced the characterization of the mechanism of granule-dependent cytotoxic activity and performed a comprehensive investigation of the content of cytotoxic granules in human virus-specific CD8 T cells (2, 19, 29, 44, 53).
Heterogeneous profiles of cytotoxic granules have been identified in different virus-specific memory CD8 T cells and associated with distinct differentiation stages of memory CD8 T cells (2, 19, 29, 44). Furthermore, we have observed a hierarchy among the cytotoxic granules in setting the efficiency of cytotoxic activity and demonstrated that perforin (and to a lesser extent GrmB) but not GrmA or GrmK were associated with cytotoxic activity (29). Recently, a novel mechanism of perforin-dependent granule-independent CTL cytotoxicity has also been demonstrated (45).
Major advances in the characterization of antigen (Ag)-specific CD4 and CD8 T cells have been made recently and have aimed at identifying functional profiles that may correlate with protective CD8 T-cell responses (1, 3, 4, 12, 13, 24, 28, 36-38, 40, 41, 49, 50, 56-58, 60, 64, 68). In particular, the functional characterization of antigen-specific T cells was mainly performed on the basis of (i) the pattern of cytokines secreted (i.e., gamma interferon [IFN-γ], tumor necrosis factor alpha [TNF-α], interleukin-2 [IL-2], or macrophage inflammatory protein 1β [MIP-1β]), (ii) the proliferation capacity, and (iii) the cytotoxic capacity (13, 28, 59). Of note, degranulation activity (i.e., CD107a mobilization following specific stimulation) has been used as a surrogate marker of cytotoxic activity (11, 13).
The term “polyfunctional” has been used to define T-cell immune responses that, in addition to typical effector functions such as secretion of IFN-γ, TNF-α, or MIP-1β and cytotoxic activity (measured by the degranulation capacity), comprise distinct T-cell populations able to secrete IL-2 and retain proliferation capacity (13, 28, 49, 50). Some evidence indicates that a hallmark of protective immune responses is the presence of polyfunctional T-cell responses (59). Furthermore, the ability to secrete IL-2 was shown to be linked to proliferation capacity, and both factors have been associated with protective antiviral immunity (13, 28, 49, 50). Although a lack of correlation between degranulation activity and GrmB expression was reported in mice (65), the relationship between degranulation activity and perforin expression has never been comprehensively investigated in mice and in humans.
The private α chain of the IL-7 receptor (IL-7Rα, also called CD127) has been suggested to selectively identify CD8 T cells that will become long-lived memory cells (6, 34, 36). Moreover, it was shown in mice (34, 36) and humans (14, 48, 63) that the CD127high memory-precursor CD8 T cells produced IL-2 in contrast to CD127low effector CD8 T cells. Of interest, CD127 expression has also been shown to correlate with Ag-specific proliferation capacity in mice (34, 36). A similar correlation was observed in humans, although only for polyclonal stimulations (48). With the exception of studies performed in HIV-1 infection, where an association between CD127 expression and HIV-1 viremia has been shown (21, 22, 42, 48, 54), very limited information is available on the CD127 expression in human virus-specific CD8 T cells other that HIV-1.
Although cytotoxic activity and proliferation capacity are key components of the antiviral cellular immune response, the relationship between these functions has been only investigated in nonprogressive HIV-1 infection (46), where these two functions were shown to be related. However, it still remains to be determined whether these functions are mediated by the same or by different T-cell populations.
In the present study, we performed a comprehensive characterization of virus-specific CD8 T-cell responses against HIV-1, cytomegalovirus (CMV), Epstein Barr virus (EBV), and influenza virus (Flu) in order to (i) analyze the degree of concordance between degranulation activity and perforin/Grm expression; (ii) identify the relevance of CD127 in identifying virus-specific CD8 T cells endowed with proliferation capacity; (iii) delineate the relationship between proliferation capacity, cytotoxic activity, activation/differentiation stage, and level of exhaustion of CD8 T cells; and (iv) determine the influence of antigen exposure in shaping the functional composition of virus-specific CD8 T cells.
Our data indicate that cytotoxic (as defined by perforin expression) and proliferating (as defined by CD127 expression or IL-2 secretion) virus-specific CD8 T cells are contained within distinct CD8 T-cell populations. Furthermore, the proportion of proliferating and cytotoxic T cells within a given virus-specific CD8 T-cell population appears to be influenced by antigen exposure. These results advance our understanding of the relationship between cytotoxicity, proliferative capacity, differentiation stage, and Ag exposure of memory CD8 T cells.
MATERIALS AND METHODS
Study groups.
Twenty-nine subjects with progressive chronic HIV-1 infection were investigated prior to their enrollment in clinical trials, including antiviral therapy with nucleoside and protease inhibitors (9). In patients with chronic HIV-1 infection, at baseline (prior to the initiation of antiviral therapy), the CD4 T-cell counts were (means ± the standard errors [SE]) 790 ± 241 cells/μl and plasma viremia was 4.39 ± 043 log10 HIV-1 RNA copies/ml. In addition, blood from 51 HIV-negative subjects was obtained either from the local blood bank (Lausanne, Switzerland) or from lab coworkers. Of note, the Flu-, EBV-, and CMV-specific CD8 T-cell responses shown here were only characterized in HIV-seronegative subjects. These studies were approved by the Institutional Review Board of the Centre Hospitalier Universitaire Vaudois.
Synthetic peptides and peptide MHC class I tetramer complexes.
All of the peptides used in the present study were purified by high-pressure liquid chromatography (>80% purity). HIV-1-, Flu-, CMV-, and EBV-derived peptides are listed in the supplemental material (part 1). HLA-A2-GILGFVFTL (Flu), HLA-A2-GLCTLVAML (EBV), HLA-B8-RAKFKQLL (EBV), HLA-B8-FLRGRAYGL (EBV), HLA-B7-RPPIFIRRL (EBV), HLA-A2-NLVPMVATV (CMV), HLA-B7-TPRVTGGGAM (CMV), HLA-A2-SLYNTVATL (HIV), HLA-B7-GPGHKARVL (HIV), HLA-B8-EIYKRWII (HIV), and HLA-A2-ILKEPVHGV (HIV) peptide-major histocompatibility complex (MHC) class I tetramer complexes were purchased from Beckman Coulter (Fullerton, CA).
Antibodies.
The following antibodies were used in different combinations. CD8-PerCPCy5.5, CD8-PB, CD4-PerCPCy5.5, CD4-fluorescein isothiocyanate (FITC), CD3-APCCy7, CD14-PB, CD45RA-PECy5, GrmB-AF700, CD107a-PECy5, PD-1-FITC, IFN-γ-FITC, IFN-γ-allophycocyanin (APC), TNF-α-PECy7, TNF-α-FITC, and IL-2-phycoerythrin (PE) were purchased from Becton Dickinson (BD, San Diego, CA); CD4-ECD was from Beckman Coulter (Fullerton, CA); perforin-FITC (clone B-D48) was from Diaclone (Besançon, France); GrmA-PB and perforin-APC were from Biolegend (San Diego, CA); CD127-PECy7 and PD-1-APC were from eBioscience, Inc. (San Diego, CA); CCR7-FITC and CD127-APC were from R&D Systems (Minneapolis, MN); CD57-PECy5 was from Abcam (Cambridge, United Kingdom); CD3-Qdot655 was from Invitrogen (Carlsbad, CA); GrmK-FITC was from Santa Cruz Biotechnology (Santa Cruz, CA); and CD4-AF700 and CD19-PB were from VWR International (Arlington Heights, IL).
Ex vivo analysis of virus-specific CD8 T cells.
Cryopreserved blood mononuclear cells (1 × 106 to 2 × 106) were stained with appropriately titered peptide-MHC class I tetramer complexes at 4°C for 15′ in Ca2+-free media. The cells were then washed and either permeabilized (Cytofix/Cytoperm; BD) and stained at room temperature for 20 min with GrmK, GrmA, GrmB, perforin, CD45RA, CD127, and CD8 or directly stained at 4° for 20 min with CD3, CD8, CD45RA, CD127, CCR7, PD-1, or CD57. Then, the cells were fixed with CellFix (BD), acquired on an LSRII SORP (4 lasers), and analyzed by using FlowJo 8.8.2 (Treestar, Inc., Ashland, OR) and SPICE 4.2.3 (developed by Mario Roederer, Vaccine Research Center, National Institute of Allergy and Infectious Disease, National Institutes of Health). The number of lymphocyte-gated events ranged between 6 × 105 and 106 in the flow cytometry experiments.
Degranulation activity (CD107a mobilization).
Cryopreserved blood mononuclear cells (1 × 106 to 2 × 106) were stimulated for 6 h in 1 ml of complete medium (RPMI plus 10% fetal bovine serum) in the presence of Golgiplug and Golgistop (1 μl/ml; BD), αCD28 antibody (0.5 μg/ml, BD), αCD107a (pretitered volume; BD), and 1 μg of peptide/ml as described previously (27). Staphyloccal enterotoxin B (SEB) stimulation (200 ng/ml) served as a positive control. At the end of the stimulation period, cells were washed, stained for dead cells by using the violet Live/Dead stain kit (Invitrogen), permeabilized (Cytofix/Cytoperm; BD), and then stained at room temperature for 20 min with CD3, CD4, CD8, CD19, CD14, and IFN-γ. Cells were then fixed, acquired on an LSRII SORP and analyzed by using FlowJo 8.8.2. The number of lymphocyte-gated events ranged between 6 × 105 and 106 in the flow cytometry experiments. With regard to the criteria of positivity of the intracellular cytokine staining (ICS), the background in the unstimulated controls never exceeded 0.03%. For an ICS result to be considered positive, there had to be more than 0.05% cytokine-positive cells after subtraction of the background.
Perforin ICS assay.
Cryopreserved blood mononuclear cells (1 × 106 to 2 × 106) were stimulated for 6 h in 1 ml of complete medium (RPMI plus 10% fetal bovine serum) in the presence of Golgiplug (1 μl/ml; BD), αCD28 (0.5 μg/ml; BD), and 1 μg of peptide/ml as described previously (27). SEB stimulation (200 ng/ml) served as a positive control. At the end of the stimulation period, cells were washed, stained for dead cells by using an Aqua Live/Dead stain kit (Invitrogen), permeabilized (Cytofix/Cytoperm), and then stained at room temperature for 20 min with CD3, CD4, CD8, IFN-γ, TNF-α, IL-2, and perforin (clone B-D48). The cells were then fixed, acquired on an LSRII SORP, and analyzed by using FlowJo 8.8.2 and SPICE 4.2.3. The number of lymphocyte-gated events ranged between 6 × 105 and 106 in the flow cytometry experiments. With regard to the criteria for ICS positivity, the background in the unstimulated controls never exceeded 0.03%. For an ICS result to be considered positive, there had to be more than 0.05% cytokine-positive cells after subtraction of the background.
Ex vivo proliferation assay.
Cryopreserved blood mononuclear cells (106 in 1 ml of complete medium) were cultured in the presence of anti-CD28 (0.5 μg/ml, BD), 20 UI of IL-2 (Proleukin; Novartis International, Basel, Switzerland) and 1 μg of peptide/ml as described previously (27, 68). At day 7, the cells were harvested, stained with appropriately titered peptide-MHC class I tetramer complexes at 37°C for 15 min, and then permeabilized (Cytofix/Cytoperm) and stained at room temperature for 20 min with GrmK, GrmA, GrmB, perforin, CD45RA, CD127, and CD8. The cells were then acquired on an LSRII SORP (four lasers) and analyzed by using FlowJo 8.8.2 and SPICE 4.2.3. For the 5,6-carboxyfluorescein diacetate succinimidyl ester (CFSE) dilution assay, overnight-rested cryopreserved blood mononuclear cells were washed twice, resuspended at 106/ml in phosphate-buffered saline, and incubated for 7 min at 37°C with 0.25 μM CFSE (Molecular Probes) as described previously (68). The reaction was then quenched with 1 volume of fetal calf serum, and the cells were washed, stained with CD127 and CD8, sorted as CD8+ CD127− and CD8+ CD127+ with a FACS-ARIA (BD), and cultured in the presence of αCD28 antibody (0.5 μg/ml; BD) and 1 μg of peptide/ml. SEB stimulation (40 ng/ml) served as a positive control.
Chromium release assay.
T2 cells were used as target cells in standard 51Cr release assays as described previously (25). 51Cr labeling and pulsing with cognate peptide (or an irrelevant HIV peptide for control) was performed for 1 h at 37°C. A total of 2,500 target cells were aliquoted into microtiter plates. Cryopreserved CD4- and CD19-depleted CD8 T cells were added to the targets at 50:1, 25:1, 12:1, and 6:1 ratios. Assay plates were incubated 4 h at 37°C and 5% CO2 before harvesting. The percent specific 51Cr release was calculated from the following equation: [(experimental release − spontaneous release)/(maximum release − spontaneous release)] × 100.
Statistical analysis.
Statistical significance (P values) of the results was calculated by using a two-tailed Student t test with either Excel (Microsoft, Redmond, WA) or SPICE 4.2.3. A two-tailed P value of <0.05 was considered significant. The correlations among variables were tested by simple regression analysis.
RESULTS
Degranulation activity and profile of cytotoxic granules distribution in virus-specific CD8 T cells.
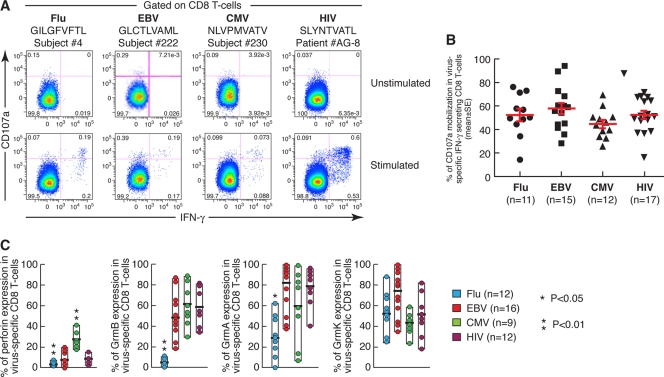
Blood mononuclear cells from four subjects containing CD8 T cells specific to Flu (GILGFVTL)-, EBV (GLCTLVAML)-, CMV (NLVPMVATV)-, and HIV-1 (SLYNTVATL)-derived peptides restricted by HLA-A2 were stimulated with the cognate peptides and stained with CD3, CD8, CD107a, and IFN-γ antibodies. The proportion of virus-specific IFN-γ-secreting CD8 T cells able to degranulate, i.e., that were CD107a positive, was comparable and in the range of 50%, regardless of the virus specificity (Fig. 1A). The extensive analysis performed on 55 virus-specific CD8 T-cell responses confirmed that degranulation activity was not significantly different among Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells (Fig. 1B). A trend toward statistical significance (P = 0.047) was only observed in the degranulation activity between EBV- and CMV-specific CD8 T cells. Of note, we have recently determined the profiles of cytotoxic granules distribution in Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells detected by peptide-HLA tetramer complexes. The analysis was limited to perforin, GrmA, GrmB, and GrmK since monoclonal antibodies are not available for GrmH and M. We observed that perforin and, to a lesser extent, GrmB correlated with cytotoxic activity, whereas GrmA and GrmK did not (29). Since the level of degranulation activity was similar in Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells (Fig. 1A and B), we compared the degranulation activity with the GrmB, GrmA, and GrmK content and in particular with perforin expression, since it is the most relevant marker of cytotoxic CD8 T cells. As summarized in Fig. 1C, perforin expression, unlike degranulation activity, was very heterogeneous between the different virus-specific CD8 T cells and was below 15% in Flu-, EBV-, and HIV-1-specific CD8 T cells. GrmB, GrmA, and GrmK were expressed at similar levels in HIV-1-, CMV-, and EBV-infected cells, while less GrmB (P < 0.01) and GrmA (P < 0.05) expression was observed in Flu-specific CD8 T cells (Fig. 1C).
FIG. 1.
Degranulation activity and cytotoxic granules content of virus-specific CD8 T cells. (A) Flow cytometry profiles of the degranulation activity of CD8 T cells measured by CD107a mobilization after stimulation with Flu-, EBV-, CMV-, or HIV-1-derived peptides. (B) Cumulative data (means ± the SE) of the proportion of CD107a+ cells among IFN-γ-secreting CD8 T cells after Ag-specific stimulation. At least 600,000 live-gated events were acquired. With regard to the criteria of positivity of the ICS, the background in the unstimulated controls never exceeded 0.03%. An ICS to be considered positive had to have >0.05% cytokine-positive cells after subtraction of the background. (C) Perforin and GrmB, GrmA, and GrmK expression in virus-specific CD8 T cells. Asterisks indicate significant differences (*, P < 0.05; **, P < 0.01) of a given virus-specific CD8 T-cell response versus all of the others. At least 600,000 live-gated events were acquired.
These data indicate that degranulation activity and perforin expression are not correlated. Thus, unlike perforin expression, degranulation activity does not necessarily identify cytotoxic CD8 T cells.
Relationship between CD127 expression and CD8 T-cell proliferation.
In mice, CD127 expression has been associated with proliferation capacity, while CD127− effector CD8 T cells proliferated poorly ex vivo (34, 36). Furthermore, in humans, the proliferation capacity of CD8 T cells was also associated with CD127 expression following polyclonal stimulation (48). Of interest, a previous report has shown a tendency of higher proliferative potential of sorted CD127+ versus CD127− CMV-specific CD8 T cells (63).
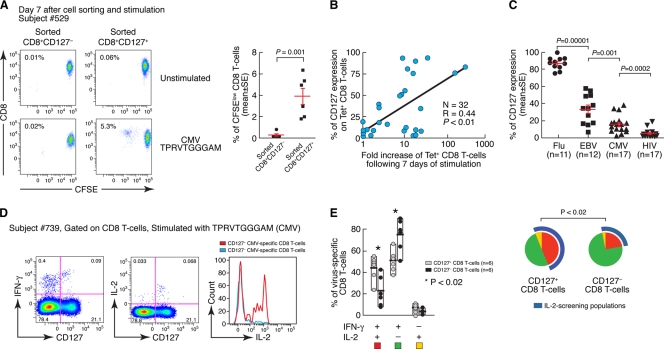
It was thus of interest to determine whether CD127 expression defined populations of Ag-specific CD8 T cells endowed with proliferation capacity in humans. For this purpose, CD8+ CD127− and CD8+ CD127+ T cells were sorted (purity > 95%), stained with CFSE and stimulated for 7 days with virus-derived peptides. As shown in the representative example in Fig. 2A, CD8 T-cell proliferation was mostly restricted to the CD127+ CD8 T-cell population after stimulation with the CMV-derived peptide TPRVTGGGAM. The higher CD8 T-cell proliferation capacity of Ag-specific CD127+ cells compared to CD127− cells was confirmed in six additional subjects (Fig. 2A), and the differences were statistically significant (P = 0.001). Furthermore, a significant positive correlation (P < 0.01) was observed between the levels of CD127 expression on virus-specific CD8 T cells and the subsequent in vitro expansion (i.e., fold increase) of virus-specific CD8 T cells after 7 days of culture (Fig. 2B).
FIG. 2.
Correlation between CD127 expression, proliferation capacity, and IL-2 production. (A) CD8+ CD127− and CD8+ CD127+ T cells were sorted (purity > 95%), stained with CFSE, and stimulated for 7 days with the CMV-derived peptide TPRVTGGGAM. Flow cytometry profiles show CFSE dilution in the two sorted populations after 7 days in vitro stimulation. Cumulative data of the percentage (means ± the SE) of proliferating (CFSElow) CD8+ CD127− and CD8+ CD127+ sorted T-cell populations after stimulation with CMV-, EBV-, or Flu-derived peptides. The data were obtained in six separate experiments. (B) Correlation between the percentage of CD127-expressing virus-specific CD8 T cells prior stimulation with the cognate peptides and the proliferation capacity (fold increase) of virus-specific CD8 T cells after 7 days of in vitro stimulation. The data were obtained by pooling 32 virus-specific CD8 T-cell stimulations. (C) Percentages of CD127 expression on Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells. (D) Flow cytometry profiles showing combinations of CD127 expression with IFN-γ- or IL-2-secreting CD8 T cells after stimulation with a CMV peptide (left panels). The right panel shows overlaid histograms of the distribution of IL-2-secreting CD8 T cells on CMV-specific (i.e., IFN-γ-secreting) CD127− and CD127+ CD8 T cells. (E) Cumulative data on the distribution of IFN-γ- and/or IL-2-secreting CD8 T cells on CD127− and CD127+ CD8 T cells. Of note, these data include HIV-1-specific CD8 T-cell responses from a patient treated at the time of the acute infection who underwent spontaneous treatment interruption and with an undetectable viremia (<5 HIV-1 RNA copies/μl of plasma) at the time of the analysis. Combinations of IFN-γ and IL-2 are shown on the x axis, whereas the percentage of virus-specific CD8 T cells is shown on the y axis. The pie charts summarize the data, and each slice corresponds to the proportion of virus-specific CD8 T cells positive for a certain combination of T-cell functions. In the pie charts, the blue line indicates functional subsets positive for IL-2.
Finally, CD127 expression in Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells showed significant differences between the distinct virus-specific CD8 T-cell responses (all P < 0.001; Fig. 2C). Of interest, the distribution of CD127 expression mirrored the ability to secrete IL-2 in the different virus-specific CD8 T-cell responses, i.e., Flu > EBV > CMV > HIV-1 (68). This observation further strengthened the relationship between CD127 expression and proliferation capacity since the presence of IL-2-secreting CD8 T cells was consistently associated with Ag-specific proliferation capacity (4, 8, 31, 32, 35, 66, 68).
Of note, we investigated the correlation between CD127 expression and IL-2 secretion in a panel of antiviral CD8 T-cell responses. For these purposes, peripheral blood mononuclear cells were stimulated with the cognate peptides and stained with antibodies to IFN-γ, IL-2, CD3, CD4, CD8, and CD127. We found that virus-specific CD127+ CD8 T cells secreted significantly more IL-2 (P < 0.02) than CD127− CD8 T cells (Fig. 2D and E). Virus-specific CD8 T cells secreting both IFN-γ and IL-2 were significantly enriched in the CD127+ population, whereas single IFN-γ-secreting CD8 T cells (i.e., IL-2 negative) were mostly contained (P < 0.02) within the CD127− population (Fig. 2D and E). These observations were consistent with previous studies showing that, after polyclonal stimulation, CD127high CD8 T cells secreted IL-2, whereas CD127neg did not (48).
In agreement with previous observations, these data indicated that CD127 is a relevant marker of cells endowed with proliferation capacity and IL-2 secretion in virus-specific human CD8 T cells.
Combination of CD127 and perforin expression and association with the activation/differentiation stage.
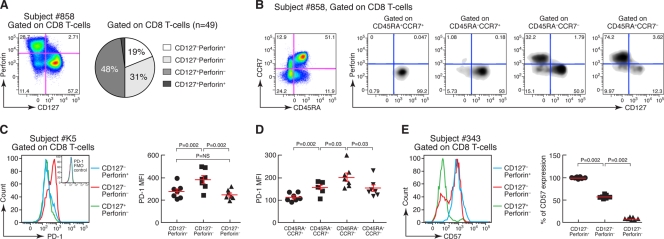
Since perforin and CD127 represent relevant markers of CD8 T cells endowed with cytotoxic or proliferation capacity, respectively, we analyzed the simultaneous distribution of these two markers on CD8 T cells. As shown in Fig. 3A, the combination of CD127 and perforin identified three phenotypically distinct populations of CD8 T cells, i.e., CD127+ perforin−, CD127− perforin−, and CD127− perforin+ cells, which is consistent with the findings of a previous study (16). We confirmed this finding in 48 additional subjects (Fig. 3A).
FIG. 3.
Combination of CD127 and perforin expression, association with T-cell differentiation, and PD-1 and CD57 expression. (A) Representative flow cytometry profile and cumulative data showing that the combination of CD127 and perforin identified three distinct populations of CD8 T cells, i.e., CD127+ perforin−, CD127− perforin−, and CD127− perforin+. (B) Polychromatic flow cytometry assay combining CD8, perforin, and CD127, together with CD45RA and CCR7. Shown is the distribution of CD127 and perforin on the four populations defined by CD45RA and CCR7. This experiment is representative of five independent assays on five distinct subjects. (C) PD-1 expression on CD127+ perforin−, CD127− perforin−, and CD127− perforin+ CD8 T-cell populations. A representative histogram plot and cumulative data ( n = 7) are shown. PD-1 FMO control (for fluorescence minus one) was used to confirm the accuracy of PD-1 expression. (D) Cumulative data of PD-1 expression (MFI) on CD45RA+ CCR7+, CD45RA− CCR7+, CD45RA− CCR7−, and CD45RA+ CCR7− CD8 T-cell populations (n = 8). (E) CD57 expression on CD127+ perforin−, CD127− perforin−, and CD127− perforin+ CD8 T-cell populations. A representative histogram plot and cumulative data (n = 7) are shown. MFI, mean fluorescence intensity.
We then investigated the differentiation stage of these distinct CD8 T-cell populations. For this purpose, blood mononuclear cells were stained with CD45RA and CCR7, allowing the distinction between naive T cells (N; CD45RA+ CCR7+), T central memory cells (TCM; CD45RA− CCR7+), T effector memory cells (TEM; CD45RA− CCR7−), and terminally differentiated effector T cells (TET; CD45RA+ CCR7−). Several studies have shown that the expression of CD45RA and CCR7 defined functionally distinct T-cell populations and a pattern of differentiation going from N to TCM to TEM and then to TET cells (8, 18, 57). Naive and TCM were almost exclusively composed of CD127+ perforin− CD8 T cells (Fig. 3B). TEM contained a majority of CD127+ perforin− CD8 T cells but also some CD127− perforin− CD8 T cells and about one-third of CD127− perforin+ CD8 T cells and the majority of TET consisted of CD127− perforin+ CD8 T cells (Fig. 3B). The example shown in Fig. 3B is representative of five independent experiments. Thus, consistent with previous studies, there was a progressive loss of CD127 expression and a progressive increase of perforin expression associated with T-cell differentiation (4, 19, 29, 48, 64). Therefore, these data are consistent with the higher proliferation capacity of TCM and the higher cytotoxic activity of TEM and TET cells (26).
As recently shown in several studies, programmed death 1 (PD-1) is upregulated on exhausted cells (23, 51, 62) and was demonstrated to be significantly associated with reduced expression of perforin and decreased T-cell proliferation (67). Along this line, we measured PD-1 expression on the different CD8 T-cell populations defined by CD127 and perforin. We observed higher PD-1 expression on CD127− perforin− T cells compared to CD127+ perforin− and CD127− perforin+ T cells (both P = 0.002; Fig. 3C). Furthermore, since the highest proportion of CD127− perforin− was found in TEM (i.e., CD45RA− CCR7−) we measured PD-1 expression in the different CD8 T-cell populations defined by CD45RA and CCR7. Consistent with our previous observations, we observed that PD-1 expression was higher in TEM compared to TCM or TET (both P = 0.03; Fig. 3D). These results are consistent with similar observations obtained with other differentiation markers (51, 62).
Finally, CD57 expression on CD8 T cells is associated with proliferation incompetence and replicative senescence (17). Thus, we measured CD57 expression on the different CD8 T-cell populations defined by CD127 and perforin and observed that CD57 was almost negative (i.e., <10%), intermediate (i.e., ca. 50%) and positive (i.e., >90%) in CD127+ perforin−, CD127− perforin−, and CD127− perforin+ CD8 T-cell populations, respectively (all P = 0.002; Fig. 3E). These results are consistent with recent studies investigating the association between CD57 and perforin (19) or PD-1 (52).
Combined expression of CD127 and perforin on virus-specific CD8 T cells.
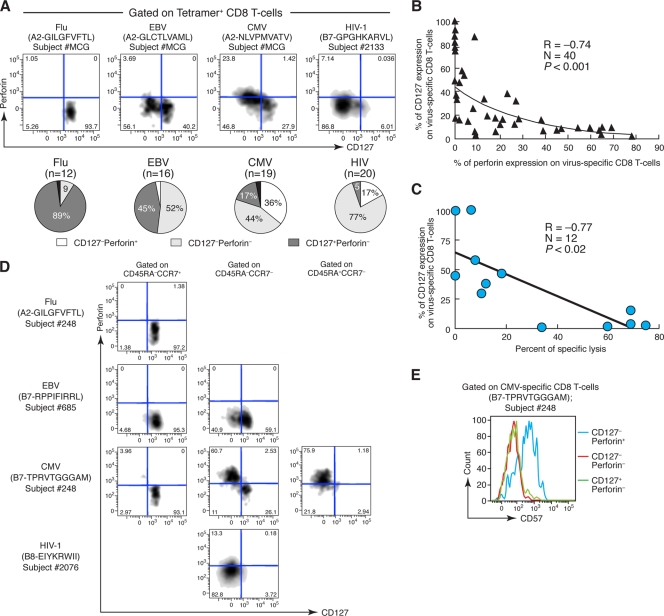
Having established the association between CD127 expression and proliferation capacity on one hand and between perforin expression and cytotoxic activity on the other hand, we then analyzed the distribution of these markers on a panel of Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells. Flu-specific CD8 T cells were mostly (>80%) CD127+ perforin− (Fig. 4A). The majority (>50%) of EBV-specific CD8 T cells were CD127− perforin−, but CD127+ perforin− CD8 T cells were also present (Fig. 4A). CMV-specific CD8 T cells were heterogeneous and rather equally distributed between all three populations (Fig. 4A). Finally, the majority (>75%) of HIV-1-specific CD8 T cells were CD127− perforin−, but a few CD127− perforin+ CD8 T cells were also present (Fig. 4A). The distinct profiles of virus-specific CD8 T-cell populations were significantly different (all P < 0.0001). Furthermore, the analysis of a large number of subjects confirmed that perforin and CD127 expression were significantly negatively correlated when Flu-, EBV-, and CMV-specific CD8 T cells were comparatively analyzed (n = 40, R = −0.74, P < 0.001, Fig. 4B). A negative correlation was also observed between CD127 expression on virus-specific CD8 T-cell responses and the percentage of specific lysis (n = 12, R = −0.77, P < 0.02, Fig. 4C).
FIG. 4.
Combination of CD127 and perforin expression, association with T-cell differentiation and CD57 expression on virus-specific CD8 T cells. (A) Representative examples and cumulative data of perforin and CD127 expression on Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells (identified by peptide-HLA tetramer complexes). (B) Inverse correlation between the percentages of perforin and CD127 expression on CMV-, EBV-, and Flu-specific CD8 T cells. (C) Inverse correlation between the percentage of CD127 expression and the percentage of specific lysis of virus-specific CD8 T-cell responses. (D) Polychromatic flow cytometry analysis combining perforin and CD127, together with CD45RA and CCR7, in virus-specific CD8 T cells. Representative examples of the distribution of CD127 and perforin on the populations defined by CD45RA and CCR7 in Flu-, EBV-, CMV-, and HIV-1-specific CD8 T-cell responses are shown. This experiment is representative of four independent experiments. (E) Representative example of CD57 expression on CMV-specific CD127+ perforin−, CD127− perforin−, and CD127− perforin+ CD8 T-cell populations.
Taken together, these data indicate a divergent expression of perforin and CD127 on virus-specific CD8 T cells.
It was then of interest to investigate whether the distribution of virus-specific CD8 T cells within the different populations defined by the expression of CD127 and perforin was associated to the stage of differentiation (defined by the expression of CCR7 and CD45RA), as previously shown for bulk CD8 T cells (Fig. 3B). As shown in Fig. 4D, Flu-, EBV-, and CMV-specific TCM (CD45RA− CCR7+) CD8 T cells were mostly (>90%) contained within the CD127+ perforin− population. EBV-, CMV-, and HIV-1-specific TEM (CD45RA− CCR7−) CD8 T cells contained a majority of CD127+ perforin− T cells but also some CD127− perforin− T cells and some CD127− perforin+ T cells (Fig. 4D). Finally, the majority (>75%) of CMV-specific TET (CD45RA+ CCR7−) CD8 T cells were CD127− perforin+ (Fig. 4D). The examples shown are representative of four independent experiments. Thus, these data indicated a progressive loss of CD127 expression and a progressive increase in perforin expression associated with T-cell differentiation in virus-specific CD8 T cells (4, 19, 29, 48, 64), which is consistent with the higher proliferation capacity of TCM cells and the higher cytotoxic activity of TEM and TET cells (26).
We then analyzed PD-1 expression within the different populations of virus-specific CD8 T cells defined by the expression of CD127 and perforin. PD-1 expression was significantly higher on CD127− perforin− T cells and on TEM, and the latter finding was consistent with the fact that the highest proportion of CD127− perforin− was observed in TEM (Fig. 3B). However, as mentioned above, the representation of these three populations was extremely heterogeneous in Ag-specific CD8 T cells. The data shown in Fig. 4A indicate that the totality of Flu-specific CD8 T cells were CD127+ perforin−, the large majority of EBV-specific CD8 T cells were also CD127+ perforin−, almost the totality of HIV-1-specific CD8 T cells were CD127− perforin−, and only CMV-specific CD8 T cells contained relevant fractions of the three populations defined by the expression of CD127 and perforin. Furthermore, CMV-specific CD8 T cells were previously shown to express very low levels of PD-1 (23, 62). Therefore, while the analysis of bulk CD8 T cells allowed us to analyze the distribution of PD-1 in the three cell populations defined by CD127 and perforin, this analysis was not possible in virus-specific CD8 T cells due to the highly heterogeneous and substantially different representation of the distinct CD8 T-cell populations. Therefore, it is difficult to compare the results obtained in bulk CD8 T-cell populations to those in Ag-specific CD8 T cells.
Finally, we measured CD57 expression on the different virus-specific CD8 T-cell populations defined by CD127 and perforin and observed that CD57 was mostly expressed by the CD127− perforin+ CD8 T-cell populations (Fig. 4E). This observation was confirmed on a large number (n = 13) of virus-specific CD8 T-cell responses (P = 0.002). These data are consistent with recent studies investigating the association between CD57 and perforin (19) or PD-1 (52) and further support the findings that CD127− perforin+ cell populations contain senescent CD8 T cells with very limited proliferation capacity (17).
Modulation of CD127 expression profiles upon Ag exposure.
We and others have recently demonstrated that Ag exposure substantially influence the phenotypic and functional (based on cytokine secretion) profiles of CD8 T cells (28, 30, 32, 61). More recently, we have shown that Ag reexposure of virus-specific CD8 T cells for 7 days in vitro induced major changes in the cytotoxic granule profiles (particularly increase in perforin and GrmB) and was associated with the acquisition of cytotoxic activity (29). Along the same lines, we investigated the influence of Ag exposure on CD127 expression. Thus, Flu-, EBV-, CMV-, and HIV-1-specific CD8 T cells were analyzed for CD127 expression directly ex vivo and then after 7 days of in vitro stimulation with cognate peptides (see the supplemental material, part 2). Interestingly, Flu-specific (HLA-A2-GILGFVFTL) CD8 T cells dramatically shifted from CD127+ to CD127− after Ag reexposure in vitro (see the supplemental material, part 2). These findings were confirmed on a larger number of subjects, and they not only pertain to Flu-specific CD8 T cells but also to EBV- and CMV-specific CD8 T cells (both P < 0.002; supplemental material, part 2). Of note, CD127 downregulation was observed in HIV-1-specific CD8 T cells despite the weak ex vivo level of expression (see the supplemental material, part 2). This is consistent with the lack of proliferation capacity of HIV-1-specific CD8 T cells (43, 68) and the lack of CD127 expression (Fig. 2C and 4A) (48).
Combination of perforin expression and cytokine secretion on CMV-specific CD8 T cells.
The presence of IL-2-secreting CD8 T cells and also CD4 T cells was consistently associated with Ag-specific proliferation capacity (8, 31, 32, 35, 61, 68). Thus, we assessed the combined expression of IL-2 and perforin on Ag-specific CD8 T cells.
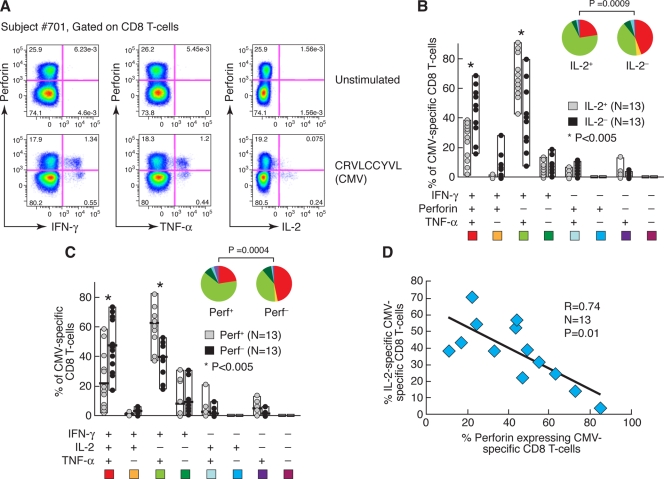
In order to analyze the combination of perforin expression and the pattern of cytokine secretion by virus-specific CD8 T cells, we took advantage of the availability of the anti-perforin antibody clone B-D48, which recognizes multiple forms of perforin. These include the uncleaved form of perforin, which is not directly secreted upon stimulation and is therefore suitable for ICS assays (33). Moreover, this form of perforin has been recently demonstrated to mediate a granule-independent mechanism of cytotoxicity (45). We thus performed conventional ICS on CMV-specific CD8 T-cell responses and stained the cells for a viability marker, CD3, CD8, CD4, a panel of cytokines (i.e., IFN-γ, TNF-α, and IL-2), and perforin. As shown for subject 701 after stimulation with the CMV-derived peptide CRVLCCYVL, a large proportion (>70%) of IFN-γ- and TNF-α-secreting CD8 T cells also expressed perforin, whereas the majority (>70%) of IL-2-secreting CD8 T cells were perforin negative (Fig. 5A). The divergent expression of perforin and IL-2 was then confirmed in the analysis of multiple functions mediated by CMV-specific CD8 T cells. When CMV-specific CD8 T cells were analyzed based on the ability to secrete IL-2 (Fig. 5B), the majority of IL-2-secreting CD8 T cells were composed of cells secreting IFN-γ and TNF-α but not containing perforin, whereas the majority of IL-2-negative CD8 T cells were composed of cells positive for IFN-γ, TNF-α and perforin (P = 0.0009). Along the same line, when CMV-specific CD8 T cells were analyzed based on perforin expression (Fig. 5C), the majority of perforin-positive CD8 T cells were composed of cells secreting IFN-γ and TNF-α but not IL-2, whereas the majority of perforin-negative CD8 T cells were composed of cells secreting IFN-γ, TNF-α, and IL-2 (P = 0.0004). Finally, a significant negative correlation (P = 0.01) was observed between the proportion of CMV-specific CD8 T cells expressing perforin or secreting IL-2, further underscoring the discordance between these functions (Fig. 5D).
FIG. 5.
Association between perforin expression and IL-2 secretion on CMV-specific CD8 T-cell responses. (A) Representative example of perforin expression and IFN-γ, TNF-α, and IL-2 secretion on CMV-specific CD8 T cells. (B) Analysis of perforin, IFN-γ, and TNF-α expression on IL-2-negative and IL-2-positive CMV-specific CD8 T-cell subsets. (C) Analysis of IL-2, IFN-γ,and TNF-α on perforin-negative and perforin-positive CMV-specific CD8 T-cell subsets. (D) Correlation between the proportion of CMV-specific CD8 T cells expressing perforin or secreting IL-2. In panels B and C, all of the possible combinations of the different markers are shown on the x axis, whereas the percentage of CMV-specific CD8 T cells is shown on the y axis. The pie charts summarize the data, and each slice corresponds to the proportion of CMV-specific CD8 T cells positive for a certain combination of T-cell functions.
DISCUSSION
In the present study, we have taken advantage of the combined use of multiparameter phenotypic and functional flow cytometry in order to determine the relationship between differentiation stage and antigen exposure with respect to key functions of CD8 T cells such as proliferation capacity and cytotoxic activity, which have been shown to be important in protective antiviral immunity. The central strategy of the study was to use CD127 and perforin as phenotypic and functional markers to define populations of virus-specific CD8 T cells. With regard to the characterization of virus-specific cytotoxic CD8 T cells, we have clearly shown the lack of correlation between degranulation activity and perforin expression, which was shown to be the primary marker of cytotoxic CD8 T cells (29). In this regard, a discrepancy between degranulation activity and GrmB expression has already been reported in mice (65).
With regard to the proliferation capacity, we have shown that, in addition to IL-2 secretion, which is a functional marker, CD127 is associated qualitatively and quantitatively with the presence of cells endowed with higher proliferation capacity. Interestingly, levels of CD127 expression followed the same trend as the proportion of IL-2-secreting CD8 T cells (68) within the same models of virus-specific CD8 T-cell responses. CD127 expression was almost absent in HIV-1-specific CD8 T cells, higher in EBV- and CMV-specific CD8 T cells, and the highest in Flu-specific CD8 T cells (68). Of interest, we also showed that virus-specific CD127+ CD8 T cells secreted significantly more IL-2 than CD127− CD8 T cells. These observations were also consistent with previous studies showing that CD127high CD8 T cells secreted IL-2, whereas CD127neg CD8 T cells did not (48). Overall, we believe that these results indicate that CD127+ CD8 T cells have greater intrinsic proliferation potential compared to CD127− CD8 T cells due to the high proportion of IL-2-secreting CD8 T cells contained within this population. Furthermore, the proportion of viable cells was lower in cultures containing CD127− CD8 T cells than in those containing CD127+ CD8 T cells (data not shown). The results also showed a certain degree of heterogeneity in the proliferation capacity of CD127+ CD8 T cells (Fig. 2B). Although we do not have a formal demonstration, it is conceivable to speculate that the observed heterogeneity may in part be explained by the size of the memory CD8 T-cell population (larger CD8 T-cell populations have generally an advantage to better expand), by the affinity for the cognate epitope and/or by the efficiency of the different peptides to induce Ag-specific proliferation.
With regard to the phenotype of virus-specific CD8 T cells, we have previously shown that both Flu- and HIV-1 (from progressors)-specific CD8 T cells are similar, i.e., almost exclusively composed of CD45RA− CCR7− T cells, whereas CMV-, EBV-, and HIV-1 (from long-term nonprogressors)-specific CD8 T cells also include a significant proportion of CD45RA+ CCR7− cells (28, 29, 68). The data provided here indicate that, in contrast to the CD45RA and CCR7 combination, CD127 is a marker that enables to discriminate between Flu- and HIV-1-specific CD8 T cells since CD127 was expressed on >80% and <10% of Flu- and HIV-1-specific CD8 T cells, respectively. Thus, CD127 expression is a key marker to distinguish between different models of virus-specific CD8 T cells and, more importantly, is a relevant marker of cells endowed with proliferation capacity.
Of interest, the combination of CD127 and perforin identified three CD8 T-cell populations. The distribution within the three T-cell populations defined by CD127 and perforin expression revealed substantial differences between the distinct virus-specific CD8 T-cell responses. Flu-specific CD8 T cells were mostly CD127+ perforin−, EBV- and CMV-specific CD8 T cells were heterogeneous with variable proportions of CD127+ perforin− and CD127− perforin+ cells, and the large majority of HIV-1-specific CD8 T cells were CD127− perforin−. Moreover, PD-1 expression was higher in CD127− perforin− cells, i.e., the population with reduced proliferation and cytotoxic potential, a finding consistent with the anergic state and reduced functionality associated with PD-1 expression (39). Along the same line, CD45RA− CCR7− T cells were was the dominant population of the CD127− perforin− CD8 T-cell populations which expressed high levels of PD-1 and which contained most HIV-1-specific CD8 T cells (18). Furthermore, CD57 expression, which is associated with proliferation incompetence and replicative senescence (17), was virtually negative in CD127+ perforin− CD8 T cells and was highest in CD127− perforin+ CD8 T cells, consistent with the fact that this T-cell population contains mostly the terminally differentiated CD45RA+ CCR7− T cells.
Moreover, the lack of coexpression of perforin and CD127 suggested a divergence between cytotoxic activity and proliferation capacity. Consistent with this model, we observed a negative correlation between CD127 expression and cytotoxic activity. Furthermore, we also report here a divergence between perforin expression and IL-2 secretion in virus-specific CD8 T cells. This observation further strengthens the divergent model between cytotoxic activity and proliferation capacity since the presence of IL-2-secreting CD8 T cells and also CD4 T cells was consistently associated with Ag-specific proliferation capacity (8, 31, 32, 35, 61, 68).
Of note, we previously showed that Ag exposure influenced the profiles of cytotoxic granules, including perforin and GrmB, GrmA, and GrmK; that perforin expression was induced in vitro after stimulation; and that these changes were associated with the acquisition of direct cytotoxic activity (29). Along the same line, we show here that Ag exposure induced a downregulation of CD127 on virus-specific CD8 T cells, which is consistent with previous studies (16, 48, 54, 63). Thus, the likely scenario suggested by these data is that after stimulation, T cells endowed with proliferation capacity (i.e., CD127+/IL-2 secreting, as found in Flu-, EBV-, and CMV-specific T cells) will expand, downregulate CD127, reduce IL-2 secretion, upregulate perforin, and acquire cytotoxic activity, whereas HIV-1-specific T cells from progressors (i.e., mostly CD127− cells) do not expand and consequently do not acquire cytotoxic activity. Interestingly, in nonprogressive HIV-1 infection, virus-specific CD8 T cells expressed significant amount of CD127 (in the range observed in CMV and EBV infection), expanded, upregulated perforin and GrmB, and acquired cytotoxic activity upon stimulation (data not shown), findings consistent with the original observations from Connors and coworkers (46, 47).
Furthermore, the composition of proliferating and cytotoxic CD8 T cells for a given antiviral CD8 T-cell population appeared to be influenced by antigen exposure (or recent activation). This model does not apply to HIV-1 chronic and progressive infection, where the high levels of antigen load and the persistence of the chronic stimulation cause severe T-cell dysfunction (23, 51, 62). The results in the present study should be taken into account for a correct monitoring and evaluation of the cytotoxic capacity of CD8 T cells induced by candidate vaccines. Based on our results, the levels of cytotoxic granules expression and the lack of detection of cytotoxic function are not necessarily the result of an underlying defect but rather reflect Ag exposure following natural virus infection, virus reactivation in chronic infections, and the associated activation/differentiation stages of memory CD8 T cells.
In conclusion, the data reported here demonstrate that proliferation and cytotoxic activities are mediated by different phenotypically defined virus-specific CD8 T-cell populations. These phenotypically distinct T-cell populations are associated with different degrees of senescence and exhaustion, and the balance between proliferating and cytotoxic populations of virus-specific CD8 T cells appears to be influenced by Ag exposure. Overall, these results are instrumental for optimizing the monitoring of antiviral CD8 T-cell responses induced by natural infections and/or vaccination regimens.
Supplementary Material
Acknowledgments
Research conducted as part of the Poxvirus T-Cell Vaccine Discovery Consortium and the Vaccine Immune Monitoring Consortium under the Collaboration for AIDS Vaccine Discovery with support from the Bill and Melinda Gates Foundation. This study was also supported by Swiss National Science Foundation Research grant FN-310000-116342 and by the Swiss Vaccine Research Institute.
Footnotes
Published ahead of print on 3 February 2010.
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1.Ahmed, R., and D. Gray. 1996. Immunological memory and protective immunity: understanding their relation. Science 272:54-60. [DOI] [PubMed] [Google Scholar]
- 2.Appay, V., P. R. Dunbar, M. Callan, P. Klenerman, G. M. Gillespie, L. Papagno, G. S. Ogg, A. King, F. Lechner, C. A. Spina, S. Little, D. V. Havlir, D. D. Richman, N. Gruener, G. Pape, A. Waters, P. Easterbrook, M. Salio, V. Cerundolo, A. J. McMichael, and S. L. Rowland-Jones. 2002. Memory CD8+ T cells vary in differentiation phenotype in different persistent virus infections. Nat. Med. 8:379-385. [DOI] [PubMed] [Google Scholar]
- 3.Appay, V., D. F. Nixon, S. M. Donahoe, G. M. Gillespie, T. Dong, A. King, G. S. Ogg, H. M. Spiegel, C. Conlon, C. A. Spina, D. V. Havlir, D. D. Richman, A. Waters, P. Easterbrook, A. J. McMichael, and S. L. Rowland-Jones. 2000. HIV-specific CD8+ T cells produce antiviral cytokines but are impaired in cytolytic function. J. Exp. Med. 192:63-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Appay, V., R. A. van Lier, F. Sallusto, and M. Roederer. 2008. Phenotype and function of human T lymphocyte subsets: consensus and issues. Cytometry A 73:975-983. [DOI] [PubMed] [Google Scholar]
- 5.Ashton-Rickardt, P. G. 2005. The granule pathway of programmed cell death. Crit. Rev. Immunol. 25:161-182. [DOI] [PubMed] [Google Scholar]
- 6.Bachmann, M. F., R. R. Beerli, P. Agnellini, P. Wolint, K. Schwarz, and A. Oxenius. 2006. Long-lived memory CD8+ T cells are programmed by prolonged antigen exposure and low levels of cellular activation. Eur. J. Immunol. 36:842-854. [DOI] [PubMed] [Google Scholar]
- 7.Barry, M., and R. C. Bleackley. 2002. Cytotoxic T lymphocytes: all roads lead to death. Nat. Rev. Immunol. 2:401-409. [DOI] [PubMed] [Google Scholar]
- 8.Bart, P. A., A. Harari, and G. Pantaleo. 2006. Clinical studies of experimental vaccines. Curr. Opin. HIV AIDS 1:286-293. [DOI] [PubMed] [Google Scholar]
- 9.Bart, P. A., G. P. Rizzardi, G. Tambussi, J. P. Chave, A. G. Chapuis, C. Graziosi, J. M. Corpataux, N. Halkic, J. Y. Meuwly, M. Munoz, P. Meylan, W. Spreen, H. McDade, S. Yerly, L. Perrin, A. Lazzarin, and G. Pantaleo. 2000. Immunological and virological responses in HIV-1-infected adults at early stage of established infection treated with highly active antiretroviral therapy. AIDS 14:1887-1897. [DOI] [PubMed] [Google Scholar]
- 10.Berke, G. 1995. The CTL's kiss of death. Cell 81:9-12. [DOI] [PubMed] [Google Scholar]
- 11.Betts, M. R., J. M. Brenchley, D. A. Price, S. C. De Rosa, D. C. Douek, M. Roederer, and R. A. Koup. 2003. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J. Immunol. Methods 281:65-78. [DOI] [PubMed] [Google Scholar]
- 12.Betts, M. R., and A. Harari. 2008. Phenotype and function of protective T-cell immune responses in HIV. Curr. Opin. HIV AIDS 3:349-355. [DOI] [PubMed] [Google Scholar]
- 13.Betts, M. R., M. C. Nason, S. M. West, S. C. De Rosa, S. A. Migueles, J. Abraham, M. M. Lederman, J. M. Benito, P. A. Goepfert, M. Connors, M. Roederer, and R. A. Koup. 2006. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107:4781-4789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boettler, T., E. Panther, B. Bengsch, N. Nazarova, H. C. Spangenberg, H. E. Blum, and R. Thimme. 2006. Expression of the interleukin-7 receptor alpha chain (CD127) on virus-specific CD8+ T cells identifies functionally and phenotypically defined memory T cells during acute resolving hepatitis B virus infection. J. Virol. 80:3532-3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bots, M., and J. P. Medema. 2006. Granzymes at a glance. J. Cell Sci. 119:5011-5014. [DOI] [PubMed] [Google Scholar]
- 16.Boutboul, F., D. Puthier, V. Appay, O. Pelle, H. Ait-Mohand, B. Combadiere, G. Carcelain, C. Katlama, S. L. Rowland-Jones, P. Debre, C. Nguyen, and B. Autran. 2005. Modulation of interleukin-7 receptor expression characterizes differentiation of CD8 T cells specific for HIV, EBV, and CMV. AIDS 19:1981-1986. [DOI] [PubMed] [Google Scholar]
- 17.Brenchley, J. M., N. J. Karandikar, M. R. Betts, D. R. Ambrozak, B. J. Hill, L. E. Crotty, J. P. Casazza, J. Kuruppu, S. A. Migueles, M. Connors, M. Roederer, D. C. Douek, and R. A. Koup. 2003. Expression of CD57 defines replicative senescence and antigen-induced apoptotic death of CD8+ T cells. Blood 101:2711-2720. [DOI] [PubMed] [Google Scholar]
- 18.Champagne, P., G. S. Ogg, A. S. King, C. Knabenhans, K. Ellefsen, M. Nobile, V. Appay, G. P. Rizzardi, S. Fleury, M. Lipp, R. Forster, S. Rowland-Jones, R. P. Sekaly, A. J. McMichael, and G. Pantaleo. 2001. Skewed maturation of memory HIV-specific CD8 T lymphocytes. Nature 410:106-111. [DOI] [PubMed] [Google Scholar]
- 19.Chattopadhyay, P. K., M. R. Betts, D. A. Price, E. Gostick, H. Horton, M. Roederer, and S. C. De Rosa. 2009. The cytolytic enzymes granzyme A, granzyme B, and perforin: expression patterns, cell distribution, and their relationship to cell maturity and bright CD57 expression. J. Leukoc. Biol. 85:88-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chowdhury, D., and J. Lieberman. 2008. Death by a thousand cuts: granzyme pathways of programmed cell death. Annu. Rev. Immunol. 26:389-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colle, J. H., J. L. Moreau, A. Fontanet, O. Lambotte, M. Joussemet, J. F. Delfraissy, and J. Theze. 2006. CD127 expression and regulation are altered in the memory CD8 T cells of HIV-infected patients: reversal by highly active anti-retroviral therapy (HAART). Clin. Exp. Immunol. 143:398-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Colle, J. H., J. L. Moreau, A. Fontanet, O. Lambotte, M. Joussemet, S. Jacod, J. F. Delfraissy, and J. Theze. 2006. Regulatory dysfunction of the interleukin-7 receptor in CD4 and CD8 lymphocytes from HIV-infected patients: effects of antiretroviral therapy. J. Acquir. Immune. Defic. Syndr. 42:277-285. [DOI] [PubMed] [Google Scholar]
- 23.Day, C. L., D. E. Kaufmann, P. Kiepiela, J. A. Brown, E. S. Moodley, S. Reddy, E. W. Mackey, J. D. Miller, A. J. Leslie, C. DePierres, Z. Mncube, J. Duraiswamy, B. Zhu, Q. Eichbaum, M. Altfeld, E. J. Wherry, H. M. Coovadia, P. J. Goulder, P. Klenerman, R. Ahmed, G. J. Freeman, and B. D. Walker. 2006. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature 443:350-354. [DOI] [PubMed] [Google Scholar]
- 24.Doherty, P. C., and J. P. Christensen. 2000. Accessing complexity: the dynamics of virus-specific T-cell responses. Annu. Rev. Immunol. 18:561-592. [DOI] [PubMed] [Google Scholar]
- 25.Dutoit, V., V. Rubio-Godoy, P. Y. Dietrich, A. L. Quiqueres, V. Schnuriger, D. Rimoldi, D. Lienard, D. Speiser, P. Guillaume, P. Batard, J. C. Cerottini, P. Romero, and D. Valmori. 2001. Heterogeneous T-cell response to MAGE-A10(254-262): high avidity-specific cytolytic T lymphocytes show superior antitumor activity. Cancer Res. 61:5850-5856. [PubMed] [Google Scholar]
- 26.Geginat, J., A. Lanzavecchia, and F. Sallusto. 2003. Proliferation and differentiation potential of human CD8+ memory T-cell subsets in response to antigen or homeostatic cytokines. Blood 101:4260-4266. [DOI] [PubMed] [Google Scholar]
- 27.Harari, A., C. Cellerai, F. B. Enders, J. Kostler, L. Codarri, G. Tapia, O. Boyman, E. Castro, S. Gaudieri, I. James, M. John, R. Wagner, S. Mallal, and G. Pantaleo. 2007. Skewed association of polyfunctional antigen-specific CD8 T-cell populations with HLA-B genotype. Proc. Natl. Acad. Sci. U. S. A. 104:16233-16238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harari, A., V. Dutoit, C. Cellerai, P. A. Bart, R. A. Du Pasquier, and G. Pantaleo. 2006. Functional signatures of protective antiviral T-cell immunity in human virus infections. Immunol. Rev. 211:236-254. [DOI] [PubMed] [Google Scholar]
- 29.Harari, A., F. B. Enders, C. Cellerai, P. A. Bart, and G. Pantaleo. 2009. Distinct profiles of cytotoxic granules in memory CD8 T cells correlate with function, differentiation stage, and antigen exposure. J. Virol. 83:2862-2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harari, A., and G. Pantaleo. 2008. HIV-1-specific immune response. Adv. Pharmacol. 56:75-92. [DOI] [PubMed] [Google Scholar]
- 31.Harari, A., S. Petitpierre, F. Vallelian, and G. Pantaleo. 2004. Skewed representation of functionally distinct populations of virus-specific CD4 T cells in HIV-1-infected subjects with progressive disease: changes after antiretroviral therapy. Blood 103:966-972. [DOI] [PubMed] [Google Scholar]
- 32.Harari, A., F. Vallelian, P. R. Meylan, and G. Pantaleo. 2005. Functional heterogeneity of memory CD4 T-cell responses in different conditions of antigen exposure and persistence. J. Immunol. 174:1037-1045. [DOI] [PubMed] [Google Scholar]
- 33.Hersperger, A. R., G. Makedonas, and M. R. Betts. 2008. Flow cytometric detection of perforin upregulation in human CD8 T cells. Cytometry A 11:1050-1057. [DOI] [PubMed] [Google Scholar]
- 34.Huster, K. M., V. Busch, M. Schiemann, K. Linkemann, K. M. Kerksiek, H. Wagner, and D. H. Busch. 2004. Selective expression of IL-7 receptor on memory T cells identifies early CD40L-dependent generation of distinct CD8+ memory T-cell subsets. Proc. Natl. Acad. Sci. U. S. A. 101:5610-5615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iyasere, C., J. C. Tilton, A. J. Johnson, S. Younes, B. Yassine-Diab, R. P. Sekaly, W. W. Kwok, S. A. Migueles, A. C. Laborico, W. L. Shupert, C. W. Hallahan, R. T. Davey, Jr., M. Dybul, S. Vogel, J. Metcalf, and M. Connors. 2003. Diminished proliferation of human immunodeficiency virus-specific CD4+ T cells is associated with diminished interleukin-2 (IL-2) production and is recovered by exogenous IL-2. J. Virol. 77:10900-10909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaech, S. M., J. T. Tan, E. J. Wherry, B. T. Konieczny, C. D. Surh, and R. Ahmed. 2003. Selective expression of the interleukin 7 receptor identifies effector CD8 T cells that give rise to long-lived memory cells. Nat. Immunol. 4:1191-1198. [DOI] [PubMed] [Google Scholar]
- 37.Kaech, S. M., E. J. Wherry, and R. Ahmed. 2002. Effector and memory T-cell differentiation: implications for vaccine development. Nat. Rev. Immunol. 2:251-262. [DOI] [PubMed] [Google Scholar]
- 38.Kagi, D., B. Ledermann, K. Burki, R. M. Zinkernagel, and H. Hengartner. 1996. Molecular mechanisms of lymphocyte-mediated cytotoxicity and their role in immunological protection and pathogenesis in vivo. Annu. Rev. Immunol. 14:207-232. [DOI] [PubMed] [Google Scholar]
- 39.Kaufmann, D. E., and B. D. Walker. 2008. Programmed death-1 as a factor in immune exhaustion and activation in HIV infection. Curr. Opin. HIV AIDS 3:362-367. [DOI] [PubMed] [Google Scholar]
- 40.Klenerman, P., and A. Hill. 2005. T cells and viral persistence: lessons from diverse infections. Nat. Immunol. 6:873-879. [DOI] [PubMed] [Google Scholar]
- 41.Lanzavecchia, A., and F. Sallusto. 2005. Understanding the generation and function of memory T-cell subsets. Curr. Opin. Immunol. 17:326-332. [DOI] [PubMed] [Google Scholar]
- 42.Lecuroux, C., I. Girault, F. Boutboul, A. Urrutia, C. Goujard, L. Meyer, O. Lambotte, M. L. Chaix, V. Martinez, B. Autran, M. Sinet, and A. Venet. 2009. Antiretroviral therapy initiation during primary HIV infection enhances both CD127 expression and the proliferative capacity of HIV-specific CD8+ T cells. AIDS 13:1649-1658. [DOI] [PubMed]
- 43.Lichterfeld, M., D. E. Kaufmann, X. G. Yu, S. K. Mui, M. M. Addo, M. N. Johnston, D. Cohen, G. K. Robbins, E. Pae, G. Alter, A. Wurcel, D. Stone, E. S. Rosenberg, B. D. Walker, and M. Altfeld. 2004. Loss of HIV-1-specific CD8+ T-cell proliferation after acute HIV-1 infection and restoration by vaccine-induced HIV-1-specific CD4+ T cells. J. Exp. Med. 200:701-712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lieberman, J. 2003. The ABCs of granule-mediated cytotoxicity: new weapons in the arsenal. Nat. Rev. Immunol. 3:361-370. [DOI] [PubMed] [Google Scholar]
- 45.Makedonas, G., P. P. Banerjee, R. Pandey, A. R. Hersperger, K. B. Sanborn, G. A. Hardy, J. S. Orange, and M. R. Betts. 2009. Rapid up-regulation and granule-independent transport of perforin to the immunological synapse define a novel mechanism of antigen-specific CD8+ T-cell cytotoxic activity. J. Immunol. 182:5560-5569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Migueles, S. A., A. C. Laborico, W. L. Shupert, M. S. Sabbaghian, R. Rabin, C. W. Hallahan, D. Van Baarle, S. Kostense, F. Miedema, M. McLaughlin, L. Ehler, J. Metcalf, S. Liu, and M. Connors. 2002. HIV-specific CD8+ T-cell proliferation is coupled to perforin expression and is maintained in nonprogressors. Nat. Immunol. 3:1061-1068. [DOI] [PubMed] [Google Scholar]
- 47.Migueles, S. A., C. M. Osborne, C. Royce, A. A. Compton, R. P. Joshi, K. A. Weeks, J. E. Rood, A. M. Berkley, J. B. Sacha, N. A. Cogliano-Shutta, M. Lloyd, G. Roby, R. Kwan, M. McLaughlin, S. Stallings, C. Rehm, M. A. O'Shea, J. Mican, B. Z. Packard, A. Komoriya, S. Palmer, A. P. Wiegand, F. Maldarelli, J. M. Coffin, J. W. Mellors, C. W. Hallahan, D. A. Follman, and M. Connors. 2008. Lytic granule loading of CD8+ T cells is required for HIV-infected cell elimination associated with immune control. Immunity 29:1009-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Paiardini, M., B. Cervasi, H. Albrecht, A. Muthukumar, R. Dunham, S. Gordon, H. Radziewicz, G. Piedimonte, M. Magnani, M. Montroni, S. M. Kaech, A. Weintrob, J. D. Altman, D. L. Sodora, M. B. Feinberg, and G. Silvestri. 2005. Loss of CD127 expression defines an expansion of effector CD8+ T cells in HIV-infected individuals. J. Immunol. 174:2900-2909. [DOI] [PubMed] [Google Scholar]
- 49.Pantaleo, G., and A. Harari. 2006. Functional signatures in antiviral T-cell immunity for monitoring virus-associated diseases. Nat. Rev. Immunol. 6:417-423. [DOI] [PubMed] [Google Scholar]
- 50.Pantaleo, G., and R. A. Koup. 2004. Correlates of immune protection in HIV-1 infection: what we know, what we don't know, what we should know. Nat. Med. 10:806-810. [DOI] [PubMed] [Google Scholar]
- 51.Petrovas, C., J. P. Casazza, J. M. Brenchley, D. A. Price, E. Gostick, W. C. Adams, M. L. Precopio, T. Schacker, M. Roederer, D. C. Douek, and R. A. Koup. 2006. PD-1 is a regulator of virus-specific CD8+ T-cell survival in HIV infection. J. Exp. Med. 203:2281-2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Petrovas, C., B. Chaon, D. R. Ambrozak, D. A. Price, J. J. Melenhorst, B. J. Hill, C. Geldmacher, J. P. Casazza, P. K. Chattopadhyay, M. Roederer, D. C. Douek, Y. M. Mueller, J. M. Jacobson, V. Kulkarni, B. K. Felber, G. N. Pavlakis, P. D. Katsikis, and R. A. Koup. 2009. Differential association of programmed death-1 and CD57 with ex vivo survival of CD8+ T cells in HIV infection. J. Immunol. 183:1120-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pipkin, M. E., and J. Lieberman. 2007. Delivering the kiss of death: progress on understanding how perforin works. Curr. Opin. Immunol. 19:301-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rehr, M., J. Cahenzli, A. Haas, D. A. Price, E. Gostick, M. Huber, U. Karrer, and A. Oxenius. 2008. Emergence of polyfunctional CD8+ T cells after prolonged suppression of human immunodeficiency virus replication by antiretroviral therapy. J. Virol. 82:3391-3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Russell, J. H., and T. J. Ley. 2002. Lymphocyte-mediated cytotoxicity. Annu. Rev. Immunol. 20:323-370. [DOI] [PubMed] [Google Scholar]
- 56.Sallusto, F., J. Geginat, and A. Lanzavecchia. 2004. Central memory and effector memory T-cell subsets: function, generation, and maintenance. Annu. Rev. Immunol. 22:745-763. [DOI] [PubMed] [Google Scholar]
- 57.Sallusto, F., D. Lenig, R. Forster, M. Lipp, and A. Lanzavecchia. 1999. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401:708-712. [DOI] [PubMed] [Google Scholar]
- 58.Seder, R. A., and R. Ahmed. 2003. Similarities and differences in CD4+ and CD8+ effector and memory T-cell generation. Nat. Immunol. 4:835-842. [DOI] [PubMed] [Google Scholar]
- 59.Seder, R. A., P. A. Darrah, and M. Roederer. 2008. T-cell quality in memory and protection: implications for vaccine design. Nat. Rev. Immunol. 8:247-258. [DOI] [PubMed] [Google Scholar]
- 60.Sprent, J., and C. D. Surh. 2002. T-cell memory. Annu. Rev. Immunol. 20:551-579. [DOI] [PubMed] [Google Scholar]
- 61.Tilton, J. C., M. R. Luskin, A. J. Johnson, M. Manion, C. W. Hallahan, J. A. Metcalf, M. McLaughlin, R. T. Davey, Jr., and M. Connors. 2007. Changes in paracrine interleukin-2 requirement, CCR7 expression, frequency, and cytokine secretion of human immunodeficiency virus-specific CD4+ T cells are a consequence of antigen load. J. Virol. 81:2713-2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Trautmann, L., L. Janbazian, N. Chomont, E. A. Said, S. Gimmig, B. Bessette, M. R. Boulassel, E. Delwart, H. Sepulveda, R. S. Balderas, J. P. Routy, E. K. Haddad, and R. P. Sekaly. 2006. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nat. Med. 12:1198-1202. [DOI] [PubMed] [Google Scholar]
- 63.van Leeuwen, E. M., G. J. de Bree, E. B. Remmerswaal, S. L. Yong, K. Tesselaar, I. J. ten Berge, and R. A. van Lier. 2005. IL-7 receptor alpha chain expression distinguishes functional subsets of virus-specific human CD8+ T cells. Blood 106:2091-2098. [DOI] [PubMed] [Google Scholar]
- 64.van Lier, R. A., I. J. ten Berge, and L. E. Gamadia. 2003. Human CD8+ T-cell differentiation in response to viruses. Nat. Rev. Immunol. 3:931-939. [DOI] [PubMed] [Google Scholar]
- 65.Wolint, P., M. R. Betts, R. A. Koup, and A. Oxenius. 2004. Immediate cytotoxicity but not degranulation distinguishes effector and memory subsets of CD8+ T cells. J. Exp. Med. 199:925-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Younes, S. A., B. Yassine-Diab, A. R. Dumont, M. R. Boulassel, Z. Grossman, J. P. Routy, and R. P. Sekaly. 2003. HIV-1 viremia prevents the establishment of interleukin 2-producing HIV-specific memory CD4+ T cells endowed with proliferative capacity. J. Exp. Med. 198:1909-1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang, J. Y., Z. Zhang, X. Wang, J. L. Fu, J. Yao, Y. Jiao, L. Chen, H. Zhang, J. Wei, L. Jin, M. Shi, G. F. Gao, H. Wu, and F. S. Wang. 2007. PD-1 up-regulation is correlated with HIV-specific memory CD8+ T-cell exhaustion in typical progressors but not in long-term nonprogressors. Blood 109:4671-4678. [DOI] [PubMed] [Google Scholar]
- 68.Zimmerli, S. C., A. Harari, C. Cellerai, F. Vallelian, P. A. Bart, and G. Pantaleo. 2005. HIV-1-specific IFN-γ/IL-2-secreting CD8 T cells support CD4-independent proliferation of HIV-1-specific CD8 T cells. Proc. Natl. Acad. Sci. U. S. A. 102:7239-7244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zinkernagel, R. M., M. F. Bachmann, T. M. Kundig, S. Oehen, H. Pirchet, and H. Hengartner. 1996. On immunological memory. Annu. Rev. Immunol. 14:333-367. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.