Abstract
The proportion of laboratory-confirmed Japanese encephalitis (JE) virus (JEV) infections was compared to the number of JE cases reported on the basis of seasonality and the clinical symptoms of hospitalized patients in Guizhou Province, China, between April and November 2006. Of the 1,837 patients with reported JE, 1,382 patients in nine prefectures were investigated. JE was confirmed in 1,210 of 1,382 (87.6%) patients by a JEV-specific immunoglobulin M (IgM) antibody-capture enzyme-linked immunosorbent assay (MAC-ELISA), heminested reverse transcriptase PCR, and virus isolation. Two strains of JEV belonging to genotype 1 were isolated. Other viral pathogens responsible for encephalitis, including echovirus, mumps virus, herpes simplex virus, and cytomegalovirus, were identified in 67 of 172 (38.9%) JE-negative cases. On the basis of the distribution of the laboratory-confirmed JE cases from different hospitals according to the Chinese administrative division, which included hospitals at the provincial, city, county, and township levels, county hospitals detected the highest number of JE cases (81.8%), whereas township hospitals detected the smallest number of JE cases (1.4%). Provincial and city hospitals had the highest and lowest rates of accuracy of providing a clinical diagnosis of JE, as confirmed by laboratory testing (91.8% and 76.7%, respectively). This study demonstrates that laboratory confirmation improves the accuracy of diagnosis of JE and that an enhanced laboratory capacity is critical for JE surveillance as well as the identification of other pathogens that cause encephalitic syndromes with clinical symptoms similar to those caused by JEV infection.
Japanese encephalitis (JE) virus (JEV), a mosquito-borne pathogen of the family Flavivirus (genus Flaviviridae), is the most common cause of epidemic and endemic viral encephalitis in Asia, with the disease being more severe in young children (1, 10). JE is widespread throughout Southeast Asia, the western Pacific region, Australasia (4, 5, 8), and China. There are an estimated 35,000 to 50,000 cases of JE reported annually. Twenty to 30% of JE patients present with neurological and mental sequelae, and there are approximately 10,000 JE-related deaths each year (1). Before 1996, there were 8,000 to 10,000 JE cases annually in China, and these cases accounted for >80% of the worldwide total (16). Since the introduction of the JE vaccine in China, the incidence of JE has decreased, with only 5,097 JE cases being reported from China in 2005 (19). Despite the use of the JE vaccine, JEV infection is still the primary cause of viral encephalitis and continues to be a pressing public health problem in China (19, 20).
A clinical JE case reporting system has been in place in China since 1951. JE cases and epidemic outbreaks have occurred in all provinces except Xinjiang, Tibet, and Qinghai (23). The reported incidence of JE decreased from 0.9489 to 0.3898 per 100,000 population between 2000 and 2005. Five provinces (Guizhou, Sichuan, Chongqing, Henan, and Yunnan) have reported the most JE cases, with children under the age of 15 being affected the most often (3, 20, 24). Although the incidence rate of JE has decreased since 2000, the hilly province of Guizhou has the highest annual incidence of JE in China; there were 1,230 and 1,038 reported cases of JE in 2004 and 2005, respectively, accounting for over 20% of the total in China (14).
Surveillance for JE in China has consisted of reporting of suspected or clinically diagnosed cases in hospital settings. Seasonality, vaccine status, and clinical tests are factors in the diagnosis of JE; but laboratory confirmation has not been part of routine surveillance activities. We wanted to analyze the accuracy of diagnosis of JE in Guizhou Province and determine the effect of laboratory testing on enhancing the detection of JE cases, as laboratory-based surveillance has been shown to be important for determining the actual JE disease burden (29).
The JEV immunoglobulin M (IgM)-capture enzyme-linked immunosorbent assay (MAC-ELISA) is highly sensitive and relatively specific and is therefore the main method used to diagnose JEV infections. However, even by the use of this assay, few reported JE cases in the southwestern provinces of China, especially Guizhou Province, are confirmed by serological testing. In 2004, only 251 of 1,230 reported cases were analyzed by the JEV MAC-ELISA, and 188 of those (74.9%) were JEV IgM positive (14). No data regarding other pathogens known to cause viral encephalitis in Guizhou Province were available.
In the present study, we tested serum and cerebrospinal fluid (CSF) specimens collected from 1,382 JE cases reported from Guizhou Province during 2006 by the JEV MAC-ELISA. In addition, 64 CSF specimens underwent nucleic acid detection testing in order to enhance the sensitivity of detection. The 172 samples with negative results for JEV were further tested by IgM ELISAs for eight other viral etiologies. The proportion of laboratory-confirmed JE cases among all reported JE cases was analyzed by test method, the Chinese administrative division of the hospital, and the JE incidence region within Guizhou Province. We found evidence of a mixed etiological spectrum and identified several factors that may affect assessment of the actual JE disease burden.
MATERIALS AND METHODS
Patients and case definition.
A total of 1,837 patients with JE (including patients with suspected JE and those meeting the clinical JE case definition; age range, 1 month to 70 years) were reported in Guizhou Province between April and November 2006. The urban or rural residence of the patient was not considered in the definition or analysis.
For the purposes of this study, a reported JE case was defined as a suspected or a clinically confirmed case of JE that was not confirmed in the laboratory. A suspected case was defined as a hospitalized patient with fever who was ill during the defined JE epidemic season (from June to October) and who had three or more of the following symptoms: vomiting, headache, focalized or generalized seizure, coma, lethargy, motor deficit, and neck rigidity. A total of 1,105 suspected JE cases were reported in Guizhou Province between April and November 2006.
A clinically confirmed JE case was defined as a patient who met the suspected JE case definition and who had clinical laboratory results of CSF pleocytosis (>10 white blood cells/mm3), an elevated protein concentration (>40 mg/dl), and a normal glucose concentration. Seven hundred thirty-two clinically confirmed JE cases were reported in Guizhou Province between April and November 2006.
A laboratory-confirmed JE case was defined as a suspected or clinically confirmed reported JE case for which there was laboratory confirmation by the presence of JEV-specific IgM in a single CSF or serum sample, detection of JEV RNA in CSF by a heminested reverse transcriptase PCR (hnRT-PCR), or the isolation and identification of JEV from CSF.
Specimens.
Specimens were collected from 1,382 of the hospitalized reported JE cases in nine prefectures in Guizhou Province (from north to south): Zunyi (ZY), Bijie (BJ), Tongren (TR), Liupanshui (LPS), Guiyang (GY), Qianxinan (QXN), Anshun (AS), Qiannan (QN), and Qiandongnan (QDN). Both serum and CSF samples were obtained from 185 patients. Only serum was obtained from 1,089 patients, and only CSF was obtained from the remaining 108 patients. Specimens were collected from the 1,382 cases within the first 3 days of illness onset in 325 (23.5%) patients, from 3 to 14 days in 1,006 (72.8%) patients, and at >14 days in 51 (3.7%) patients. Specimens were stored at −80°C and were transported on dry ice to the Department of Viral Encephalitis and Arbovirus, Institute for Viral Disease Control and Prevention (IVDCP), China Center for Disease Control and Prevention (CDC), Beijing, China, for testing.
Serological testing.
All the serum and CSF specimens were screened for JEV-specific IgM by the MAC-ELISA with a JEV IgM-capture ELISA kit (Shanghai B&C Biological Technology Co., Ltd., Shanghai, China). The JEV IgM-negative serum samples were tested by the use of ELISA IgM kits (Virion/Serion Co., Wurzburg, Germany) for other viral encephalitis pathogens, including echovirus (ECHOV), coxsackievirus (COXV), Epstein-Barr virus (EBV), mumps virus, herpes simplex virus (HSV) type 1 (HSV-1), HSV-2, varicella-zoster virus (VZV), cytomegalovirus (CMV), and measles virus. All operations were done in accordance with the manufacturer's instructions. All testing was carried out at the Department of Viral Encephalitis and Arbovirus, IVDCP, China CDC.
Molecular biological testing.
Sixty-four of the 293 CSF specimens met the criteria for molecular testing by hnRT-PCR, as follows: (i) specimen collection was within 3 days of illness onset, (ii) the specimen had been appropriately stored and shipped at −80°C, and (iii) the volume of the specimen remaining after serological testing was completed was sufficient. Briefly, RNA was extracted by using a QIAamp viral RNA extraction kit (Qiagen, Valencia, CA), in accordance with the manufacturer's protocol, and the first strands of cDNA were produced by using Ready-To-Go You-Prime First-Strand beads (Amersham Pharmacia Biotech, Piscataway, NJ), as described in the manual accompanying the bead kit. The prM gene of JEV was amplified by hnRT-PCR (21, 22). One positive control and one negative control were included in the reactions, and the use of procedures to avoid contamination was strictly enforced. All operations were carried out according to the manufacturer's specifications.
Virus isolation and identification.
Of the 64 CSF specimens examined by hnRT-PCR, 45 had a sufficient volume for virus isolation. An aliquot of 200 μl of each CSF specimen was diluted in 1 ml Eagle's minimum essential medium (MEM; Sigma, St. Louis, MO) and inoculated onto confluent BHK-21 cell monolayers in a T25 flask. After adsorption for 1 h at 37°C, fresh medium was added and the cells were incubated at 37°C in 5% CO2. The cells were checked daily for a cytopathic effect (CPE). At a 70% CPE, the culture supernatants were harvested and the cellular debris was removed by centrifugation at 12,000 rpm. The supernatants were stored at −80°C until they were tested for JEV by hnRT-PCR. Neighbor-joining phylogenetic analysis was performed by using the genotypes of the JEV strains determined on the basis of the nucleotide sequences, and neighbor-joining treesAu: Insertion of @0082neighbor-joining trees@0083 correct to specify “constructed”? were constructed by using the MEGA program (version 4).
Diagnostic criteria.
A viral pathogen was regarded as etiologic when one of the following criteria was met: (i) virus-specific IgM antibodies were present in serum and/or CSF, (ii) virus was isolated from CSF, or (iii) viral RNA was detected in CSF by hnRT-PCR.
Statistical analysis.
Significance was assessed by Pearson's χ2 analysis with the SPSS program (version 11.5; SPSS Inc., Chicago, IL).
RESULTS
Analysis of epidemic of reported JE cases in Guizhou Province in 2006.
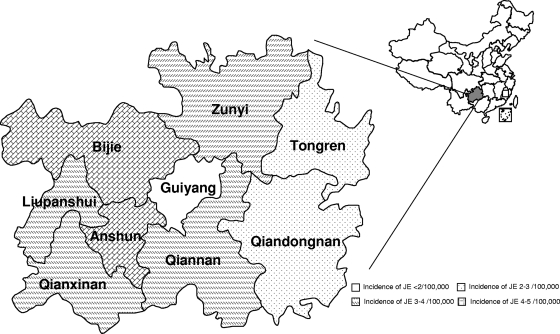
The nine prefectures were classified into four groups, according to the JE incidence rate. The incidence rate was derived from data on the epidemic of JE cases reported to the China CDC in 2006: GY, the capital of Guizhou Province, was in group 1 (JE incidence rate, <2/100,000 population); the eastern prefectures of TR and QDN were in group 2 (JE incidence rate, 2 to 3/100,000 population); most of the prefectures, including LPS, ZY, QXN, and QN, belonged to group 3 (JE incidence rate, 3 to 4/100,000 population); and AS and BJ were in group 4 (JE incidence rate, 4 to 5/100,000) (Fig. 1).
FIG. 1.
(Right panel) Location of Guizhou Province in China. (Left panel) Background incidence rate of reported JE cases in nine prefectures within Guizhou Province.
The hospitals involved in this study were classified into the four administrative divisions in China: provincial, city, county, and township hospitals. Provincial hospitals provide medical services for the whole province, while city hospitals mainly serve people within the prefecture, county hospitals mainly serve people within the county, and township hospitals serve as health care centers within the township. Patients with more serious illnesses in county hospitals are mostly transferred to a city hospital and/or a provincial hospital. In general, the provincial hospital is more comprehensive and capable, followed by the city, county, and township hospitals.
Specimen collection.
The overall specimen collection rate was 75.2% (1,382/1,837 specimens) (Table 1). In seven prefectures, the collection rate exceeded 86%. By comparison, the rate in ZY was 74.1% and that in BJ was 47.8%.
TABLE 1.
Specimen collection from reported JE patients in Guizhou Province, 2006
| JE incidence group no. | Prefecture | No. of reported JE cases | No. of specimens collected from cases | Specimen collection rate (%) |
|---|---|---|---|---|
| 1 | GY | 44 | 43 | 97.7 |
| 2 | TR | 110 | 108 | 98.2 |
| QDN | 145 | 128 | 88.3 | |
| 3 | LPS | 171 | 158 | 92.4 |
| ZY | 290 | 215 | 74.1 | |
| QXN | 177 | 155 | 87.6 | |
| QN | 172 | 151 | 87.8 | |
| 4 | AS | 195 | 169 | 86.7 |
| BJ | 533 | 255 | 47.8 | |
| Total | 1,837 | 1,382 | 75.2 |
Laboratory diagnosis.
There were 1,382 hospitalized patients enrolled in the study. These patients met the case definition of suspected or clinically confirmed JE, and serum and/or CSF was obtained from each patient. Of the 1,382 patients, 1,210 (87.6%) had laboratory-confirmed JE: 1,186 (98.0%) by the JEV MAC-ELISA (1,013 of 1,089 serum samples, 54 of 108 CSF samples, 119 of 185 serum/CSF samples) and 24 (2.0%) by hnRT-PCR only (10 of 108 CSF samples, 14 of 185 serum/CSF samples). The JE positivity rates in the different prefectures ranged from 74.4% (GY) to 94.3% (LPS) (Table 2).
TABLE 2.
Laboratory diagnosis of JE in reported JE patients in Guizhou Province, 2006a
| JE incidence group no. | Prefecture | No. of reported cases | No. of the following samples with the indicated result: |
Total no. of JE-positive cases | Rate of positivity (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S, ELISA+ | CSF |
Serum or CSF |
|||||||||||||
| ELISA+ | ELISA+/RT-PCR− | ELISA−/RT-PCR+ | ELISA+/RT-PCR+ | S, ELISA+ | CSF, ELISA+ | S/CSF, ELISA+ | S/CSF, ELISA+/RT-PCR− | S/CSF, ELISA−/RT-PCR+ | S/CSF, ELISA+/RT-PCR+ | ||||||
| 1 | GY | 43 | 32 | 32 | 74.4 | ||||||||||
| 2 | TR | 108 | 78 | 2 | 2 | 2 | 2 | 3 | 89 | 82.4 | |||||
| QDN | 128 | 113 | 113 | 88.3 | |||||||||||
| 3 | LPS | 158 | 100 | 14 | 1 | 1 | 2 | 27 | 2 | 2 | 149 | 94.3 | |||
| ZY | 215 | 189 | 1 | 190 | 88.4 | ||||||||||
| QXN | 155 | 72 | 6 | 3 | 1 | 6 | 1 | 31 | 5 | 5 | 130 | 83.9 | |||
| QN | 151 | 131 | 2 | 133 | 88.1 | ||||||||||
| 4 | AS | 169 | 111 | 10 | 1 | 2 | 22 | 3 | 1 | 150 | 88.8 | ||||
| BJ | 255 | 187 | 12 | 3 | 3 | 14 | 1 | 3b | 1 | 224 | 87.8 | ||||
| Total | 1,382 | 1,013 | 42 | 3 | 10 | 9 | 8 | 1 | 98 | 3 | 14 | 9 | 1,210 | 87.6 | |
Abbreviations: S, serum; CSF, cerebrospinal fluid; +, positive; −, negative; ELISA, JEV-specific IgM detection by MAC-ELISA with a JEV IgM-capture ELISA kit; RT-PCR, molecular testing by hnRT-PCR.
JEV was isolated from two of these three samples.
Of the 64 CSF specimens tested by hnRT-PCR, 48 cases were confirmed to be JE: 6 with positive JEV MAC-ELISA results alone and negative hnRT-PCR results, 24 with negative JEV MAC-ELISA results but positive hnRT-PCR results, and 18 with positive results by both the JEV MAC-ELISA and hnRT-PCR (Tables 2 and 3).
TABLE 3.
Results of JE diagnosis by JEV MAC-ELISA and RT-PCR
| RT-PCR result | No. of specimens with the following JEV MAC-ELISA result: |
||
|---|---|---|---|
| + | − | Total | |
| + | 18 | 24 | 42 |
| − | 6 | 16 | 22 |
| Total | 24 | 40 | 64 |
Virus was isolated from 2 of 45 CSF specimens for which a sufficient volume for testing remained (data not shown). Background analysis showed that the CSF sample from one patient (an 8-year-old male; the CSF sample was collected 3 days after the onset of illness) was JEV IgM positive, whereas the serum and CSF samples from the other patient (a 2-year-old female; serum and CSF were collected 5 and 4 days after the onset of illness, respectively) were JEV IgM negative. Neither patient had been vaccinated against JEV. The viral isolates were identified as JEV genotype 1 by phylogenetic analysis (data not shown).
One hundred seventy-two JE-negative serum specimens were tested for IgM antibodies against other etiological agents. Other viral pathogens were identified in 67 (38.9%) specimens. Mumps virus was the most common pathogen, accounting for 58.2% (39/67), followed by ECHOV (8/67, 11.9%), HSV (6/67, 9.0%), COXV (2/67, 3.0%), and CMV (1/67, 1.5%). No patient tested positive for EBV, VZV, or measles virus. Testing for IgM antibodies revealed several cases of infection with more than one virus: six cases (8.9%) of mumps virus and HSV infections and five cases of ECHOV and COXV infections (7.5%) (data not shown). The average rate of detection of all other pathogens was 4.8% (67/1,382). Non-JEV infections accounted for 12.4% of the cases diagnosed overall; the highest frequency (25.6%) occurred in GY, and the lowest (5.7%) occurred in LPS. The frequencies in the other regions ranged from 10% to 17% (Table 4).
TABLE 4.
Laboratory detection of other pathogens in reported JE patients in Guizhou Province, 2006
| JE incidence group no. | Prefecture | Total no. of cases tested | JE-negative cases |
Laboratory diagnosis |
||||
|---|---|---|---|---|---|---|---|---|
| Negative |
||||||||
| No. | Rate (%) | No. | Rate (%) | No. | Rate (%) | |||
| 1 | GY | 43 | 11 | 25.6 | 3 | 7.0 | 8 | 18.6 |
| 2 | TR | 108 | 19 | 17.6 | 12 | 11.1 | 7 | 6.5 |
| QDN | 128 | 15 | 11.7 | 9 | 7.0 | 6 | 4.7 | |
| 3 | LPS | 158 | 9 | 5.7 | 4 | 2.5 | 5 | 3.1 |
| ZY | 215 | 25 | 11.6 | 11 | 5.1 | 14 | 6.5 | |
| QXN | 155 | 25 | 16.1 | 6 | 3.9 | 19 | 12.3 | |
| QN | 151 | 18 | 11.9 | 8 | 5.3 | 10 | 6.6 | |
| 4 | AS | 169 | 19 | 11.2 | 7 | 4.1 | 12 | 7.1 |
| BJ | 255 | 30 | 11.8 | 7 | 2.7 | 24 | 9.4 | |
| Total | 1382 | 172 | 12.4 | 67 | 4.8 | 105 | 7.6 | |
Sex, age, and seasonal distribution.
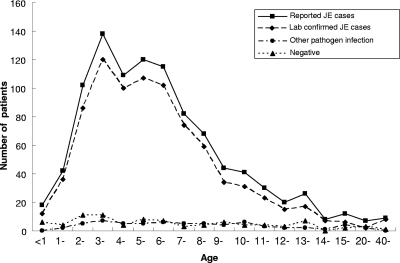
From the analysis of the 841 reported JE cases for which clinical data were available, among the patients with laboratory-confirmed JE, the number of males exceeded that of females by a ratio of 1.6:1. The group consisting of individuals ages <1 to 11 years accounted for 90% of the JEV-positive patients; this was concordant between hospitalized reported JE cases and laboratory-confirmed JE cases. No age range was associated with any of the JEV-negative cases with other viral etiologies (Fig. 2).
FIG. 2.
Age distribution of all reported JE cases, laboratory-confirmed JE cases, and other virus infections in Guizhou Province, 2006.
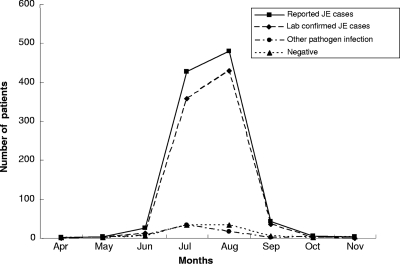
The seasonal distribution of the reported JE cases showed that the incidence of JE appeared to have a single epidemic peak spanning the months of July and August. Encephalitis caused by other viral pathogens did not show a clear seasonal distribution (Fig. 3).
FIG. 3.
Monthly distribution of all reported JE cases, laboratory-confirmed JE cases, and other virus infections in Guizhou Province, 2006.
Distribution of JE cases diagnosed in the laboratory.
In GY (JE incidence group 1), the percentage of laboratory-confirmed cases compared to the number of suspected or clinically confirmed reported JE cases was relatively low (74.4%) and differed significantly from the percentages of laboratory-confirmed JE cases in the other regions (χ2 = 20.92, P = 0.002) (Table 5). No significant difference was detected among the four incidence groups in Guizhou Province. The hospitals involved in this study were also classified into four different levels according to the Chinese administrative division and included provincial, city, county, and township hospitals. County hospitals detected 81.8% of the total laboratory-confirmed cases, with the highest and lowest rates being in QN (98.7%) and GY (44.2%), respectively. This was followed by city (12.4%), provincial (4.4%), and township (1.4%) hospitals (Table 5).
TABLE 5.
Distribution of laboratory-confirmed cases of JE in Guizhou Province, 2006
| JE incidence group no. | Prefecture | Total no. of cases tested | No. of cases (% positivity) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Province |
City |
County |
Town |
|||||||||||||||
| Total | JE | Infection with another pathogen | Negative | Total | JE | Infection with another pathogen | Negative | Total | JE | Infection with another pathogen | Negative | Total | JE | Infection with another pathogen | Negative | |||
| 1 | GY | 43 | 12 (27.9) | 9 (75.0) | 0 | 3 (25.0) | 12 (27.9) | 10 (83.3) | 0 | 2 (16.7) | 19 (44.2) | 13 (68.4) | 3 (15.8) | 3 (15.8) | 0 | 0 | 0 | 0 |
| 2 | TR | 108 | 3 (2.8) | 3 (100.0) | 0 | 0 | 5 (4.6) | 4 (80.0) | 0 | 1 (20.0) | 95 (87.9) | 79 (83.2) | 11 (11.6) | 5 (5.26) | 5 (4.6) | 3 (60.0) | 1 (20.0) | 1 (20.0) |
| QDN | 128 | Na | 5 (3.9) | 1 (20.0) | 2 (40.0) | 2 (40.0) | 123 (96.1) | 112 (91.1) | 7 (5.7) | 4 (3.3) | 0 | 0 | 0 | 0 | ||||
| 3 | LPS | 158 | N | 15 (9.5) | 12 (80.0) | 0 | 3 (20.0) | 141 (89.2) | 135 (95.7) | 4 (2.8) | 2 (1.4) | 2 (1.3) | 2 (100.0) | 0 | 0 | |||
| ZY | 215 | 40 (18.6) | 38 (95.0) | 0 | 2 (5.0) | 65 (30.2) | 56 (86.2) | 2 (3.1) | 7 (10.8) | 107 (49.8) | 93 (86.9) | 9 (8.4) | 5 (4.7) | 3 (1.4) | 3 (100.0) | 0 | 0 | |
| QXN | 155 | N | 29 (18.7) | 23 (79.3) | 2 (6.9) | 4 (13.8) | 123 (79.4) | 104 (84.5) | 4 (3.3) | 15 (12.2) | 3 (1.9) | 3 (100.0) | 0 | 0 | ||||
| QN | 151 | N | 2 (1.3) | 2 (100.0) | 0 | 0 | 149 (98.7) | 131 (87.9) | 8 (5.4) | 10 (6.7) | 0 | 0 | 0 | 0 | ||||
| 4 | AS | 169 | 1 (0.6) | 1 (100.0) | 0 | 0 | 21 (12.4) | 14 (66.7) | 3 (14.3) | 4 (19.0) | 145 (85.8) | 133 (91.7) | 4 (2.8) | 8 (5.5) | 2 (1.2) | 2 (100.0) | 0 | 0 |
| BJ | 255 | 5 (2.0) | 5 (100.0) | 0 | 0 | 18 (7.1) | 10 (55.6) | 1 (5.6) | 7 (38.9) | 228 (89.4) | 205 (89.9) | 6 (2.6) | 17 (7.5) | 4 (1.6) | 4 (100.0) | 0 | 0 | |
| Total | 1,382 | 61 (4.4) | 56 (91.8) | 0 | 5 (8.2) | 172 (12.4) | 132 (76.7) | 10 (5.8) | 30 (17.4) | 1,130 (81.8) | 1,005 (88.9) | 56 (5.0) | 69 (6.1) | 19 (1.4) | 17 (89.5) | 1 (5.3) | 1 (5.3) | |
N, there are no provincial hospitals in this area.
The accuracies of detection of the 1,382 suspected and clinically diagnosis JE cases, determined by laboratory confirmation, were 91.8%, 88.9%, and 89.5% in the provincial hospitals (there were no provincial hospitals in QDN, LPS, QXN, and QN), county hospitals, and township hospitals, respectively. In comparison, the accuracy of the clinical diagnosis was significantly lower in city hospitals (76.7%; χ2 = 31.41, P < 0.001); the lowest accuracy (20.0%) occurred in QDN. In GY, the rate of JE laboratory confirmation was lower in the provincial hospitals (75.0%) and county hospitals (68.4%) than in the other hospitals. The rate of detection of the other pathogens was higher in country hospitals in TR Prefecture (11.6%) than in the other regions (Table 5).
DISCUSSION
JE is an epidemic disease which occurs during the mosquito transmission season in the summer on mainland China. In previous studies conducted from 2000 to 2004, the number of cases reported between June and October accounted for over 92% of the total number of annual cases, with monthly distribution data showing a single peak spanning July and August (3). The incidence of JE steadily decreased after 1972 and since 1996 has remained at <1/100,000 population, which is at about the same time that JE vaccination became widely used in several eastern provinces in China (23).
A safe and effective live-attenuated JE vaccine made from strain SA14-14-2 is routinely administered nationwide in China (6, 26). Since 2007, the prevention and control of JE in China have been advanced through the integration of JE immunization into the Expanded Program of Immunization (EPI) on mainland China, especially in rural and poor areas, such as Guizhou Province. The EPI system is mainly aimed at children; however, the number of adult cases of JE being reported in China is increasing; for example, 86% of the patients in the Yuncheng JE outbreak were adults (22). Therefore, it is essential that laboratory confirmation of the diagnosis of cases hospitalized with suspected JE be implemented as part of surveillance activities in order to understand the true JE disease burden.
Guizhou Province is a poor, rural area with a hilly terrain located in southwestern China. From 1995 to 2004, it had the highest rate of JE epidemics and incidence (23). It has been hypothesized (4) that the incidence of JE in low-income areas such as Guizhou Province would be higher because of the lack of a surveillance system, personal protection, education about the disease and the mosquito vector, and financial resources. We wanted to look at the current incidence rate of JE in Guizhou Province using laboratory-based surveillance, as well as to determine the accuracy of reporting of JE cases.
We conducted our investigation during the summer JE epidemic season in Guizhou Province in 2006. Laboratory testing by virus isolation, a serological MAC-ELISA, and hnRT-PCR confirmed 87.6% of the reported JE cases. The JEV MAC-ELISA remains the dominant method for the laboratory confirmation of JE in China, and in our study, 98.0% of the cases were identified by the JEV MAC-ELISA. Although CSF was considered the best specimen for use for diagnostic testing, only 21.2% of the specimens referred in this study were CSF specimens. Of the 293 CSF specimens collected, 64 could be tested by molecular methods; 24 JE cases were confirmed by hnRT-PCR alone, and two JEV isolates were obtained. Among the 172 JE-negative cases, another viral encephalitis etiology was identified in 67 (38.9%). CMV particularly seems to be an important pathogen among this population (18, 28). JE was most often identified in children during July and August, whereas the non-JEV infections identified did not show these trends; these are similar to the results of previous studies (18, 28).
The reported JE cases from Guizhou Province largely comprised hospitalized patients meeting the suspected JE case definition. Analysis of the diagnostic accuracy rate at the different hospitals at the administrative division level showed that the rate of misdiagnosis was significantly higher in city hospitals than in provincial, county, or township hospitals. Guizhou Province is mountainous and economically underdeveloped and has a poor road system. Most patients with encephalitis are taken to county hospitals (81.8%), which are closer, rather than to provincial hospitals (4.4%) or city hospitals (12.4%), which are farther away. Few JE cases (1.4%) were seen at township-level hospitals. Because the doctors in the county hospitals had more contact with JE cases than those in the township or provincial hospitals, they are more familiar with the disease and, it might be assumed, have a higher rate of clinical diagnostic accuracy. Many of the cases in the provincial hospitals, especially in GY, were referred from other hospitals across the province, and their clinical symptoms were complex and serious, resulting in difficult diagnoses and a lower rate of confirmed JE cases. Other studies have also found that severe, rare, or unusual cases are more likely to be found at tertiary-care hospitals, such as Beijing Children's Hospital, than at other hospitals, where JE may be more likely to be diagnosed by clinicians familiar with the symptoms. Also, because there is no effective treatment for JE, patients at the county hospitals diagnosed with JE on the basis of their clinical symptoms would be less likely to be transferred to the tertiary-care provincial hospitals. Anecdotally, this phenomenon also appeared to be true in our study in GY, the capital of Guizhou Province.
Despite the comprehensive testing that is performed, a large proportion of encephalitis cases remain undiagnosed. Similarly, it was shown in a retrospective study at Beijing Children's Hospital that the etiology could be confirmed by serological and/or molecular biological testing in only 38.5% of cases (11).
The rates of acute encephalitis syndrome (AES) related to infection with JEV are about 30 to 40% in Vietnam, Cambodia, and India (9, 13, 15), where JE is an endemic disease. A separate study of acute undifferentiated fever in Thailand showed that about 14% of the cases were actually JE (25). An investigation into the viral etiology of acute childhood encephalitis in Beijing showed that 5.1% of the cases were caused by JEV (27). Given a sample collection rate of 75.2% (1,382 of 1,837 reported JE cases), we estimate that there were about 1,609 laboratory-confirmed cases of JE in Guizhou Province in 2006.
hnRT-PCR can increase the sensitivity of JE detection in very acute JE cases if CSF is collected within the first few days of illness, when IgM may not have reached levels detectable by the MAC-ELISA. However, molecular methods increase the cost of testing, and the CSF must be stored at −80°C immediately after collection to prevent viral RNA degradation. In addition it is more difficult to establish and maintain the technical skills necessary to conduct the testing in hospitals and public health laboratories. Virus isolation also requires a high-quality CSF specimen, which means that CSF should be collected in a timely manner and stored/shipped in liquid nitrogen and/or dry ice. It would not be possible to perform routine molecular testing for JE surveillance at most public health laboratories.
Two JEV isolates were found to be genotype 1. This is the first reported isolation of JEV genotype 1 from humans in China. JEV genotype 3 was first isolated from a human brain in Beijing in 1949 (7), and genotype 1 was first isolated from mosquitoes in Shanghai in 2001 (17). Since then, numerous genotype 1 JEV strains have been isolated from mosquitoes in other provinces; in addition, genotypes 1 and 3 have been found to cocirculate across mainland China (2, 21). Moreover, JEV genotypes 1 and 3 were detected simultaneously in CSF specimens from JE patients and from mosquitoes during the JE outbreak in Yuncheng Prefecture, Shanxi Province, in 2006, while no virus isolates were obtained during that outbreak (22). Further investigation and isolation of JEV are needed to determine the role of genotype 1 in JE outbreaks in China.
In this study, we looked at the accuracy of JE case reporting in Guizhou Province. JE cases were primarily identified from hospitalized patients with suspected and/or clinically diagnosed JE. The insight into the disease burden that it provides may be useful for the further development of a JE vaccination policy in China. This study indicates that the current JE surveillance system in China should be enhanced to include the laboratory confirmation of cases, and it is very important that the laboratory capacity be improved in these settings in order distinguish JE from encephalitis caused by infections with other viruses. To determine the true incidence of JE in China, a system that uses the JEV MAC-ELISA for the diagnosis of JE should be instituted in hospitals and local (county and/or prefecture) CDCs. In addition, in those provincial laboratories with a greater technical capacity, the use of molecular detection methods would increase the sensitivity of detection. Laboratory-based surveillance for JE among AES patients should also be enhanced, as it would facilitate the identification of cases of JE that might have been missed on the basis of other clinical definitions. In the future, we plan to focus on the etiologies of AES, especially JEV, in China.
Acknowledgments
We thank Barbara W. Johnson, Diagnostic & Reference Laboratory, Arbovirus Diseases Branch, Division of Vector-Borne Infectious Diseases, Centers for Disease Control and Prevention, Fort Collins, CO, for critical reading of the manuscript and helpful discussions about this paper.
This work was supported by a grant from the Ministry of Science and Technology of China (grant 2003BA712A08-01), a development grant from the State Key Laboratory for Infectious Disease Prevention and Control (grant 2008SKLID105), and the Japan Health Science Foundation (2002 to 2007).
Footnotes
Published ahead of print on 10 February 2010.
REFERENCES
- 1.Burke, D. S., and C. J. Leake 1988. Japanese encephalitis, p. 63-92. In T. P. Monath (ed.), Arboviruses: epidemiology and ecology, vol. 3. CRC Press, Boca Raton, FL. [Google Scholar]
- 2.Chen, D., H. Y. Wang, S. H. Fu, H. Song, J. Deng, Y. L. Yang, and G. D. Liang. 2005. Molecular characteristics of three new isolates of Japanese encephalitis virus in Fujian Province. Chin. J. Exp. Clin. Virol. 19:5-8. [PubMed] [Google Scholar]
- 3.Chen, Y. S., X. F. Liang, X. J. Wang, Y. X. Li, J. F. Yang, J. H. Li, Z. D. Yin, Y. S. Hu, and W. Lu. 2006. Epidemiological analysis of the Japanese encephalitis in China during 2000-2004. Chin. J. Vaccines Immunization 12:196-198. (In Chinese.) [Google Scholar]
- 4.Erlanger, T. E., S. Weiss, and J. Keiser. 2009. Past, present, and future of Japanese encephalitis. Emerg. Infect. Dis. 15:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanna, J. N., S. A. Ritchie, and D. A. Phillops. 1999. Japanese encephalitis in north Queensland, Australia. Med. J. Aust. 170:533-536. [DOI] [PubMed] [Google Scholar]
- 6.Hennessy, S., Z. Liu, T. F. Tsai, B. L. Strom, C. M. Wan, H. L. Liu, T. X. Wu, H. J. Yu, Q. M. Liu, N. Karabatson, W. B. Bilker, and S. B. Halstead. 1996. Effectiveness of live-attenuated Japanese encephalitis vaccine (SA14-14-2): a case-control study. Lancet 347:1583-1586. [DOI] [PubMed] [Google Scholar]
- 7.Huang, C. H., and Y. M. Wang. 1951. Epidemic encephalitis virus isolation and identification in Beijing. Chin. Med. J. 37:280-285. [Google Scholar]
- 8.Jeffrey, N. H., A. R. Scott, and A. P. Debra. 1995. An outbreak of Japanese encephalitis in the Torres Strait, Australia. Med. J. Aust. 165:256-260. [DOI] [PubMed] [Google Scholar]
- 9.Kabilan, L., S. Ramesh, S. Srinivasan, V. Thenmozhi, S. Muthukumaravel, and R. Rajendran. 2004. Hospital- and laboratory-based investigations of hospitalized children with central nervous system-related symptoms to assess Japanese encephalitis virus etiology in Cuddalore District, Tamil Nadu, India. J. Clin. Microbiol. 42:2813-2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knipe D. M., and P. M. Howley. Flaviviridae: the virus and their replication, p. 991-1029. In B. N. Fields (ed.), Fields virology, 4th ed. Lippincott-Raven, Philadelphia, PA.
- 11.Liu, C. Y., Q. L. Shen, and G. D. Liang. 2007. Epidemiological analysis of viral encephalitis in children hospitalized in Beijing Children's Hospital from 2002 to 2005. Chin. J. Pract. Pediatr. 22:498-501. [Google Scholar]
- 12.Reference deleted.
- 13.Lowry, P. W., D. H. Truong, L. D. Hinh, J. I. Ladinsky, N. Karabatsons, C. B. Cropp, D. Martin, and D. J. Gubler. 1995. Japanese encephalitis among hospitalized pediatric and adult patients with acute encephalitis syndrome in Hanoi, Vietnam. Am. J. Trop. Med. Hyg. 58:324-329. [DOI] [PubMed] [Google Scholar]
- 14.Song, C. F., Q. Tao, C. Yu, W. J. Jiang, J. Z. Zhou, and Z. X. Wang. 2006. Preventive control strategy and epidemiological analysis on Japanese encephalitis in Guizhou province during 1997-2004. Chin. J. Vector Biol. Control 17:90-92. [Google Scholar]
- 15.Srey, V. H., H. Sadones, S. Ong, M. Mam, C. Yim, S. Sor, P. Grosjean, and J. M. Reynes. 2002. Etiology of encephalitis syndrome among hospitalized children and adults in Takeo, Cambodia, 1999-2000. Am. J. Trop. Med. Hyg. 66:200-207. [DOI] [PubMed] [Google Scholar]
- 16.Tsai, F. T. 2000. New initiatives for the control of Japanese encephalitis by vaccination: minutes of a WHO/CVI meeting, Bangkok, Thailand, 13-15 October 1998. Vaccine 18(Suppl. 2):1-25. [DOI] [PubMed] [Google Scholar]
- 17.Wang, H. Y., S. H. Fu, X. Y. Li, H. Song, J. Deng, Y. L. Yang, and G. D. Liang. 2004. Isolation and identification of genotype I Japanese encephalitis virus in China. Chin. J. Microbiol. Immunol. 24:843-849. [Google Scholar]
- 18.Wang, H. Y., S. H. Fu, L. Wang, X. Y. Gao, Y. X. Li, Z. D. Yin, S. B. Zhang, X. F. Liang, S. Chutima, and G. D. Liang. 2008. Confirm diagnosis for Japanese encephalitis report cases in Shaanxi Province 2005-2006. Chin. J. Vaccines Immunization 12:118-120. (In Chinese.) [Google Scholar]
- 19.Wang, H., Y, Li, X. Liang, and G. Liang. 2009. Japanese encephalitis in mainland China. Jpn. J. Infect. Dis. 62:331-336. [PubMed] [Google Scholar]
- 20.Wang, H. Y., and G. D. Liang. 2003. Review: arbovirus in China in recent ten years. Chin. J. Public Health 19:473-476. [Google Scholar]
- 21.Wang, H. Y., T. Takasaki, S. H. Fu, X. H. Sun, H. L. Zhang, Z. X. Wang, Z. Y. Hao, J. K. Zhang, Q. Tang, A. Kotaki, S. Tajima, X. F. Liang, W. Z. Yang, I. Kurane, and G. D. Liang. 2007. Molecular epidemiological analysis of Japanese encephalitis virus (JEV) in China. J. Gen. Virol. 88:885-894. [DOI] [PubMed] [Google Scholar]
- 22.Wang, L. H., S. H. Fu, H. Y. Wang, X. F. Liang, J. X. Cheng, H. M. Jiang, G. L. Cai, X. W. Li, W. Y. Ze, X. J. Lv, H. Q. Wang, D. L. Zhang, Y. Feng, Z. D. Yin, X. H. Sun, T. J. Shui, M. H. Li, Y. X. Li, and G. D. Liang. 2007. Japanese encephalitis outbreak, Yuncheng, China, 2006. Emerg. Infect. Dis. 13:1123-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang, X. J., Y. Lu, Y. P. Zhang, Y. S. Chen, and X. F. Liang. 2004. Dynamic tendency of Japanese B encephalitis in China. Chin. J. Vaccines Immunization 10:302-304. [Google Scholar]
- 24.Wang, X. J., Y. P. Zhang, R. Z. Zhang, Y. S. Chen, and X. F. Liang. 2004. Analysis on epidemic trend of Japanese encephalitis during 1998-2002 in China. Chin. J. Vaccines Immunization 10:215-217. [Google Scholar]
- 25.Watt, G., and K. Jongsakul. 2003. Acute undifferentiated fever caused by infection with Japanese encephalitis virus. Am. J. Trop. Med. Hyg. 68:704-706. [PubMed] [Google Scholar]
- 26.Xin, Y. Y., G. M. Zhang, Y. P. Guo, J. Ao, and L. H. Min. 1988. Safety of a live attenuated Japanese encephalitis virus vaccine (SA14-14-2) for children. Am. J. Trop. Med. Hyg. 39:214-217. [DOI] [PubMed] [Google Scholar]
- 27.Xu, Y. H., R. G. Zhao, V. Sirkka, K. L. Shen, Y. T. Zhou, L. O. Magnius, W. Britta, and L. Annika. 1996. Viral etiology of acute childhood encephalitis in Beijing diagnosed by analysis of single samples. Pediatr. Infect. Dis. J. 15:1018-1024. [DOI] [PubMed] [Google Scholar]
- 28.Xu, Z. Q., S. H. Fu, Y. P. Zhang, X. L. Li, X. Y. Gao, L. Wang, Y. X. Cao, L. H. Xu, Y. Jin, Q. Tang, and G. D. Liang. 2008. Laboratory testing of specimens from patients with viral encephalitis from regions of China. Chin. J. Exp. Clin. Virol. 22:98-100. [PubMed] [Google Scholar]
- 29.Zhuang, Y., H. Wu, C. Yu, and Z. X. Wang. 2004. Epidemiological investigation and analysis of a Japanese encephalitis outbreak in Guizhou Province. Chin. J. Vector Biol. Control 15:473. [Google Scholar]