Abstract
Objective
To examine the prevalence of left ventricular hypertrophy (LVH) and LV remodeling patterns within Hispanic subgroups compared with non-Hispanic whites in the Multi-Ethnic Study of Atherosclerosis.
Background
Hispanics are the largest and fastest growing ethnic minority in the United States but there are no data on LVH and LV geometry among Hispanic subgroups.
Methods
Cardiac magnetic resonance imaging was performed in 4309 men and women aged 45 to 84 years without clinical cardiovascular disease. Hispanics were categorized into subgroups based on self-reported ancestry. LVH was defined as the upper 95th percentile of indexed LV mass in a reference normotensive, non-diabetic, non-obese population, and LV remodeling according to the presence/absence of LVH and abnormal/normal LV mass to LV end-diastolic volume ratio.
Results
Among Hispanic participants, 574 were of Mexican, 329 were of Caribbean, and 161 were of Central/South American origin. On unadjusted analysis, only Caribbean-origin Hispanics (PR 1.2 [95% CI, 1.03–1.4]) had greater prevalence of hypertension than non-Hispanic whites. Hispanic subgroups were more likely to have LVH than non-Hispanic whites after adjustment for hypertension and other covariates (Caribbean-origin Hispanics: OR 1.8 [95% CI 1.1–3.0]; Mexican-origin Hispanics: OR 2.2 [95% CI 1.4–3.3]; Central/South Americans: OR 1.5 [95% CI 0.7–3.1]). All Hispanic subgroups also had a higher prevalence of concentric and eccentric hypertrophy compared to non-Hispanic whites (P<0.001).
Conclusion
Caribbean-origin Hispanics had a higher prevalence of LVH and abnormal LV remodeling compared to non-Hispanic whites. A higher prevalence of LVH and abnormal LV remodeling was also observed among Mexican-origin Hispanics despite a lower prevalence of hypertension. Differences among Hispanic subgroups regarding LVH and LV remodeling should be taken into account when evaluating cardiovascular risk in this population.
Keywords: hypertension, hypertrophy, remodeling, epidemiology, Hispanics, magnetic resonance imaging
Hispanics are the largest minority ethnic group in the United States, numbering 46 million people or 16% of the U.S. population (1,2). Sixty-seven percent of Hispanics in the U.S. are of Mexican origin, 19% come from the Caribbean (principally from Puerto Rico, Cuba, and the Dominican Republic), and 14% originate from Central and South America (3,4). Indirect evidence suggests that the prevalence of hypertension differs among these Hispanic subgroups: the prevalence of hypertension was lower among Mexican-origin Hispanics than among non-Hispanic whites and non-Hispanic blacks in one cohort (5), whereas the prevalence of hypertension among Caribbean-origin Hispanics was higher and similar to that of non-Hispanic whites and blacks, respectively, in another (6,7).
Left ventricular hypertrophy (LVH), as defined by increased LV mass (LVM), is a marker of subclinical cardiovascular disease (CVD) and a powerful, independent predictor of CVD morbidity and mortality among Hispanics and non-Hispanics (8,9). Abnormal LV remodeling may also carry an incremental risk independent of LVH (10). Three abnormal LV remodeling patterns have been identified: concentric hypertrophy, eccentric hypertrophy, and concentric remodeling (11,12). Each pattern of LVM distribution appears to carry a different risk for cardiovascular events (13).
In addition to the prevalence of hypertension, Hispanic subgroups also differ with respect to ancestry/race,(14) socioeconomic factors,(15) dietary and lifestyle risk factors for CVD (2,16) which could influence increased LVM and LV remodeling differentially among Hispanic subgroups. The prevalence of LVM and LV remodeling across Hispanic subgroups remains unknown. We therefore examined the prevalence of LVH and LV remodeling patterns on cardiac magnetic resonance imaging (MRI) in Hispanic subgroups compared to non-Hispanic whites in the Multi-Ethnic Study of Atherosclerosis (MESA). We specifically hypothesized that Mexican-origin Hispanics would have similar a prevalence of increased LVM and abnormal LV remodeling compared to non-Hispanic whites; Caribbean-origin Hispanics would have a higher prevalence; and Central/South Americans would have intermediate values.
METHODS
The characteristics of subjects enrolled in MESA have been described elsewhere (17). Between July 2000 and September 2002, 6,814 men and women aged 45 to 84 years were enrolled from six U.S. communities (Baltimore; New York; Los Angeles; Forsyth County, North Carolina; Chicago; and St. Paul, Minnesota). Participants were recruited from four ethnic groups: non-Hispanic white, non-Hispanic black, Hispanic, and Chinese. Non-Hispanic white participants were recruited at all sites, non-Hispanic black participants were recruited at all sites except St. Paul, and Hispanic participants were recruited in New York, Los Angeles, and St. Paul. All participants were free of clinical cardiovascular disease at enrollment. Institutional review boards at all study centers approved the study protocol. Informed consent was obtained from every participant.
Baseline Examination
Demographic characteristics, including age, gender, educational attainment, medical history, medication, alcohol, and tobacco use were ascertained by questionnaire. Race and ethnicity were based on responses to questions modeled on the 2000 U.S. census. All participants who self-identified as Hispanics where categorized as Hispanic and were asked to further self-identify as Cuban, Dominican, Mexican, Puerto Rican, or Other Hispanic. Glucose, total and high-density lipoprotein cholesterol levels were measured after a 12-h fast. Presence of diabetes mellitus was based on self-reported physician diagnosis, use of insulin and/or oral hypoglycemic agent, or a fasting glucose value ≥126 mg/dL. Physical activity was self-reported as number of minutes per week spent in moderate or vigorous activities, which allowed for determination of metabolic equivalents/minutes/week of physical activity. Family annual income and education were each classified into 3 groups (<$20,000; $20,000–$49,999; and >$50,000) and (< high school; completed high school +/− some college; and completed college or more) respectively.
Blood Pressure and Hypertension Assessment
Resting blood pressure was measured using the Dinamap Monitor PRO 100 (Critikon, Tampa, FL) automated oscillometric device. Three measurements were obtained at one-minute intervals with the subject in the seated position with back and arm supported after five minutes of rest with an appropriate sized cuff, with the cuff at the level of the heart, using a standardized protocol. The average of the second and third measurements was recorded as the resting blood pressure. Hypertension was defined as a systolic blood pressure ≥ 140 mm Hg, a diastolic blood pressure ≥ 90 mm Hg, or currently taking medications for blood pressure control (18).
Cardiac MRI protocol
The reliability of the MRI readings has been previously reported (19). Myocardial volume was determined from the difference between epicardial and endocardial LV volumes calculated by modified Simpson’s rule. A series of LV end diastolic short axis images were created starting at the mitral annulus and advancing through the ventricle to apex at 10mm intervals. Papillary muscles were excluded from LVM analysis. LVM was calculated from the product of myocardial volume and specific gravity (1.05g/ml) as previously described (20).
Preliminary evaluation showed MRI measured LVM and volume indexed by body surface area, height2.7 or height1.9 did not fully remove the correlation of these measures with weight and/or height. Using an allometric approach (21,22), regression models for body size were derived from a reference sample of MESA participants without hypertension, diabetes mellitus, or obesity as previously described (22) so that the equation would reflect the normal physiology free from disease or obesity that might distort the relationship of height and weight and LVM. The index derived multiplied by 100 is equivalent to the percentage of the value predicted on the basis of height, weight and gender in a normal population. LVM was adjusted for body size by dividing 100*LVM by the predicted LVM based on height, weight and gender, as 100*LVM/(a * Height0.54 * Weight0.61) where a = 6.82 for women and 8.25 for men with mass in grams, height in meters, weight in kilograms. Similarly, the body size adjusted LV end-diastolic volume was computed as 100*LV*volume/(b*Height1.25*Weight0.43) where b = 10.0 for women and 10.5 for males and LV end diastolic volume is in milliliters. Body surface area was used to index LVM in a confirmatory analysis. Presence of LVH was defined by a percent-predicted LVM value greater than the 95th upper percentile estimated (from empirical cumulative distribution) separately for men and women.
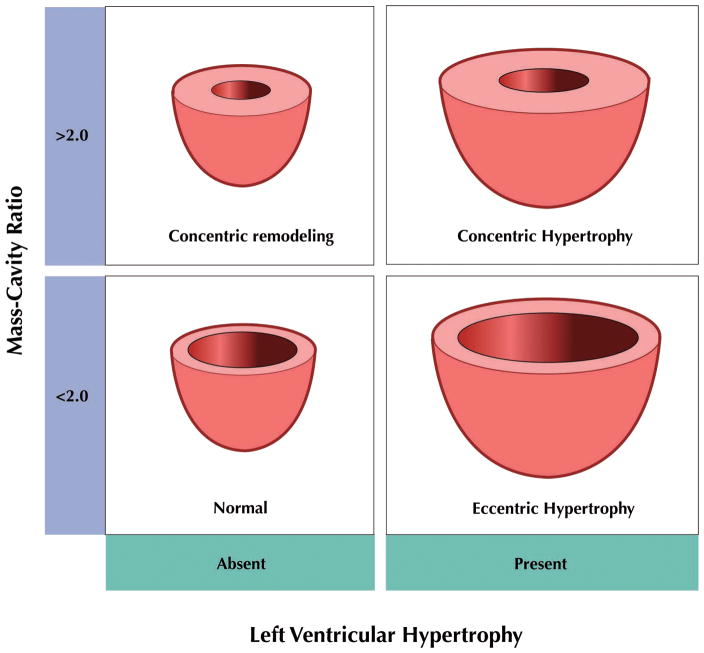
LV remodeling analysis was determined by unadjusted LVM/LV end-diastolic volume ratio [mass to cavity (M-C) ratio]. Geometric classification of LV architecture by echocardiography relies on measurement of relative wall thickness. The M-C ratio is conceptually the MRI equivalent of relative wall thickness. An abnormal M-C ratio was defined as an M-C ratio greater than the gender-specific 95th percentile of control subjects without the conditions described above. LV remodeling was classified into patterns of eccentricity: normal (normal LVM, normal M-C ratio), concentric remodeling (normal LVM, high M-C ratio), eccentric hypertrophy (high LVM, normal M-C ratio), and concentric hypertrophy (high LVM, high M-C ratio) as previously described (12). (Figure 1)
Figure 1. Diagram of left ventricular remodeling patterns based on left ventricular hypertrophy and left ventricular Mass.
Cavity ratio--Four types of left ventricular (LV) remodeling patterns are described based on presence/absence of LV hypertrophy (LVH) and the LV Mass/LV end-diastolic volume (M-C) ratio: normal with LVH absent and normal M-C ratio, concentric remodeling with LVH absent and increased M-C ratio, eccentric hypertrophy with LVH present and normal M-C ratio, and concentric hypertrophy with LVH present and increased M-C ratio. Partition value for elevated M-C ratio was 2.0.
Statistical Analysis
Hispanic subgroups were categorized based on self-report as Mexican- or Caribbean- (Dominican, Puerto Rican, or Cuban) origin Hispanic. Of the remainder identifying as ‘Other Hispanic’, 93% were born in Central or South America and were hence categorized as of Central/South American origin. Both non-Hispanic whites and non-Hispanic blacks were used as reference groups because Hispanics are often a mixture of these two racial groups; Asians were excluded from analyses. Distributions of risk factors, mean LVM, prevalence of LVH and ventricular remodeling categories were compared using Chi-square for categorical variables and ANOVA for continuous variables.
Because prevalence of hypertension was close to 50%, unadjusted and adjusted prevalence ratios (PR) and 95% confidence intervals (CI) were calculated by relative risk regression using SAS PROC GENMOD procedure with log-link and binomial error. Logistic regression analysis was used to assess the odds ratio (OR) and 95% CI of LVH and elevated M-C ratio among non-Hispanic whites, non-Hispanic blacks and each Hispanic subgroup. Multivariate linear regression models were based on LVM percent predicted as a continuous variable. To assess the relative contribution of different sets of covariates (potential confounders) on the LVH and M-C ratio differences observed, we compared estimates across a series of sequential adjustment models. Model 1 (adjusted for age and sex); in Model 2 socioeconomic factors (insurance, education, income) were added to model 1; Model 3 added metabolic factors (diabetic status, BMI, total and high-density lipoprotein cholesterol) to model 2; Model 4 added behavioral factors (physical activity, cigarette smoking) to model 3; Model 5 added systolic blood pressure, diastolic blood pressure, and use of antihypertensive medications to model 4. The relative proportion of risk explained by each set of factors was estimated as follows:
Statistical significance was defined as two-tailed P-value <0.05; no adjustment was made for multiple comparisons given the descriptive nature of this study but all major comparisons are reported (23).
RESULTS
Of 6814 MESA participants, 1810 lacked MRI measures, 653 were Asian and 42 did not provide information on Hispanic subgroup. Of the remaining 4309 included participants, 1064 were Hispanic: 574 (54%) of Mexican, 329 (31%) of Caribbean and 161 (15%) of Central/South American origin. Compared to participants without MRI, included participants were slightly younger, had lower average systolic blood pressure and body mass index (BMI) and were less likely to have hypertension or diabetes, as previously described (24). These differences were non-differential across Hispanic subgroups.
Demographics and Cardiac Risk Factors among Hispanic Subgroups
Age and gender distributions were similar across non-Hispanic whites, African-Americans and Hispanic subgroups; however, educational attainment, income, and the proportion with private insurance were lower for all Hispanic subgroups compared to both whites and African-Americans in this sample (Table 1). Mexican-origin Hispanics had a higher mean BMI than other Hispanic subgroups, similar to non-Hispanic blacks, and the greatest prevalence of diabetes and metabolic syndrome.
Table 1.
Baseline Characteristics by Race-Ethnicity and Hispanic Subgroup
| Non-Hispanic Whites N=1959 | Non-Hispanic Black N=1286 | Mexican-origin Hispanics N=574 | Caribbean-origin Hispanics N=329 | South or Central American N=161 | |
|---|---|---|---|---|---|
| Age, yrs | 62.1±10.1 | 61.6±9.9 | 60.7±10.1 | 59.4±10.2 | 60.5±10.1 |
| Gender M/F % | 47.3/52.7 | 45.5/54.5 | 52.3/47.7 | 49.2/50.8 | 42.2/57.8 |
| Education | |||||
| <high school | 4.1 | 10.3 | 43.7 | 42.3 | 37.3 |
| high school +/− some college | 42.9 | 54.4 | 48.6 | 45.6 | 47.2 |
| ≥Bachelor’s degree | 53.0 | 35.3 | 7.7 | 12.2 | 15.5 |
| Income | |||||
| ≤$20,000 | 10.1 | 20.2 | 35.6 | 38.5 | 43.0 |
| $20,000 to $49,999 | 31.8 | 40.7 | 46.2 | 43.1 | 41.8 |
| >$50,000 | 58.1 | 39.1 | 18.2 | 18.5 | 15.2 |
| Insurance Status % private | 81.5 | 75.1 | 55.8 | 63.8 | 50.9 |
| Diabetes % | 7.3 | 19.1 | 22.8 | 13.7 | 13.0 |
| Impaired fasting glucose, % | 23.4 | 25.7 | 29.8 | 30.5 | 32.3 |
| Metabolic Syndrome, % | 29.3 | 32.1 | 46.9 | 31.4 | 35.4 |
| BMI, kg/m2 | 27.3+/−4.7 | 29.4+/−5.2 | 29.5+/−4.7 | 28.3+/−4.2 | 28.2+/−4.4 |
| Current smoker, % | 12.8 | 19.4 | 14.1 | 18.5 | 13.0 |
| High-density lipoprotein cholesterol (mg/dl) | 52.5±15.8 | 53.1±15.6 | 46.5±12.9 | 48.4±13.0 | 50.1±13.5 |
| Exercise, metabolic equivalent/hour/week | 28.±37.4 | 31.3±50.9 | 22.7±35.3 | 24.7±31.6 | 19.2±31.7 |
| Current Alcohol use % | 72.0 | 51.0 | 49.5 | 49.9 | 48.1 |
| Systolic blood pressure, mm Hg | 122.4±20.3 | 130.7±21.4 | 126.4±22.7 | 125.4±20.4 | 125.0±19.8 |
| Diastolic blood pressure, mm Hg | 70.0±10.1 | 74.7±10.2 | 70.8±10.4 | 73.5±9.1 | 71.5±9.8 |
Values expressed as mean SD or percentage.
BMI – body mass index
Hypertension among Hispanic Subgroups
The prevalence of hypertension across Hispanic subgroups is shown in Table 2 in comparison to whites and non-Hispanic blacks. Non-Hispanic blacks had the highest prevalence of hypertension overall (unadjusted PR 1.6 [95% CI, 1.5–1.7] vs. whites) and Caribbean-origin Hispanics had the highest prevalence of hypertension among Hispanic subgroups (unadjusted PR 1.2 [95% CI, 1.03–1.4]). There were no significantly differences in hypertension prevalence between Central/South Americans (unadjusted PR 1.1 [95% CI, 0.9–1.4]) or Mexican-origin Hispanics (unadjusted PR 1.0 [95% CI, 0.9–1.1]) and non-Hispanic whites. After adjustment for age, gender, education, income, physical activity, BMI, current alcohol use, smoking, and diabetes, the prevalence of hypertension remained higher among non-Hispanic blacks (adjusted PR 1.05 [95% CI, 1.02–1.08]) and, of borderline statistical significance, among Caribbean-origin Hispanics (adjusted PR 1.05 [95% CI, 1.0.–1.10]) compared to non-Hispanic whites.
Table 2.
Hypertension and Left Ventricular Hypertrophy by Race-Ethnicity and Hispanics Subgroups
| Race-Ethnicity | Non-Hispanic Whites n=1959 | Non-Hispanic Black n=1286 | Mexican-origin Hispanics n=574 | Caribbean-origin Hispanics n=329 | South or Central American n=161 |
|---|---|---|---|---|---|
| % with Treated hypertension | 32.2 | 49.1 | 27.5 | 38.0 | 28.0 |
| % with Hypertension | 36.4 | 56.9 | 36.8 | 42.6 | 40.4 |
| LVM (g) | 143.7±38.3 | 157.7±41.6 | 148.9±38.5 | 146.0±37.1 | 137.7±37.0 |
| Indexed LVM (percent-predicted) | 101±17 | 107±21 | 106±19 | 107±18 | 105±20 |
| Indexed LVM (body surface area, g/m2) | 75.8±15.2 | 81.3±18.0 | 81.0±16.8 | 80.4±15.6 | 77.7±16.5 |
| M-C Ratio | 1.14±0.24 | 1.24±0.27 | 1.18±0.24 | 1.16±0.25 | 1.15±0.23 |
Crude prevalence rates are reported.
Values expressed as mean ± SD or percentage.
Hypertension was defined as blood pressure ≥140 mm Hg systolic or ≥90 mm Hg diastolic, or with treated hypertension.
Treated hypertension was defined as a history of a physician diagnosis of hypertension and taking antihypertensive medication.
LVH among Hispanic Subgroups
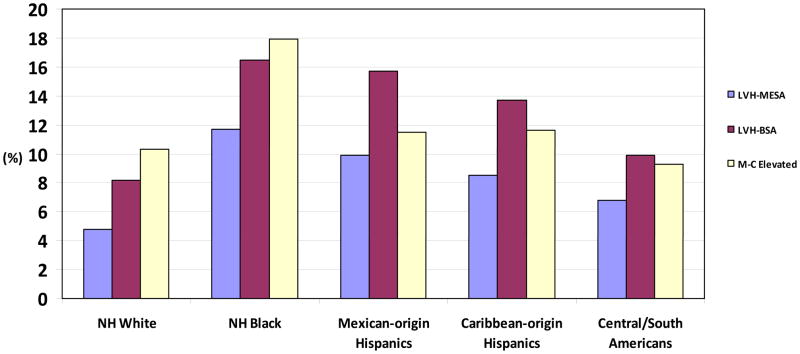
Despite the modest or absent differences in hypertension prevalence between Hispanics and non-Hispanic whites, all Hispanic subgroups had higher LVH prevalence than non-Hispanic whites (Table 2 and Figure 2). This result was not sensitive to indexing methodology (percent predicted or body surface area). There were weak but significant linear relationships between systolic blood pressure and LVM; Pearson r = 0.13–0.22 among the racial/ethnic subgroups; all p <0.01. Diastolic blood pressure was not correlated to LVM.
Figure 2. Prevalence of Left Ventricular Hypertrophy and elevated Mass-Cavity ratio by Race.
Ethnicity and Hispanic Subgroup--Different indexing methodologies for left ventricular hypertrophy (LVH) are presented including percent-predicted (LVH-MESA) and body surface area (LVH-BSA). M-C ratio = LVM/LV end-diastolic volume; partition value for elevated M-C ratio was 2.0.
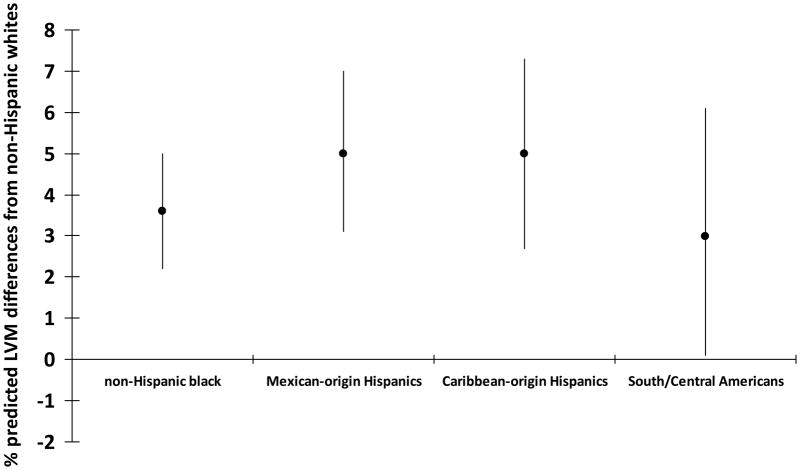
In age-sex adjusted models, Caribbean-origin Hispanics and Mexican-origin Hispanics had twice the odds of having LVH as non-Hispanic whites. Sequential adjustment for combined socioeconomic indices resulted with a 23% reduction in effect size versus only 10% among Caribbean-origin Hispanics and 12% among non-Hispanic blacks. Addition of metabolic covariates including BMI had minimal effects on the odds ratios for LVH among all Hispanics subgroups or non-Hispanic blacks. Additional adjustment for blood pressure reduced the odds of LVH for Caribbean-origin Hispanics and non-Hispanic blacks by 36% and 20% respectively (Table 3). After adjustment for all covariates, all Hispanic subgroups had a higher percent-predicted LVM compared to non-Hispanic whites, specifically 5.0 units larger for Mexican-origin Hispanics, 5.0 units larger for Caribbean-origin Hispanics, and 3.0 units larger for Central/South Americans. (Figure 3) A separate analysis substituting LVM indexed by body surface area in all our regression models yielded qualitatively similar results.
Table 3.
Odds Ratios of Left Ventricular Hypertrophy by Race-Ethnicity and Hispanic Subgroups after Sequential Adjustment for Covariates
| Non-Hispanic Whites n=1959 | Non-Hispanic Black n=1286 | Mexican-origin Hispanics n=574 | Caribbean-origin Hispanics n=329 | South or Central American n=161 | |
|---|---|---|---|---|---|
| Unadjusted | 1.0 | 2.6 (2.0–3.4) | 2.2 (1.5–3.1) | 1.8 (1.2–2.9) | 1.5 (0.8–2.8) |
| Model 1 (age and sex) | 1.0 | 2.7 (2.0–3.5) | 2.3 (1.6–3.2) | 2.0 (1.3–3.1) | 1.5 (0.8–2.9) |
| Model 2 (model 1+ socioeconomic factors) | 1.0 | 2.5 (2.0–3.5) | 2.0 (1.4–3.0) | 1.9 (1.2–3.1) | 1.2 (0.6–2.5) |
| Model 3 (model 2 + metabolic variables) | 1.0 | 2.5 (1.8–3.3) | 2.1 (1.4–3.1) | 1.9 (1.2–3.1) | 1.2 (0.6–2.6) |
| Model 4 (model 3 + behaviors) | 1.0 | 2.4 (1.8–3.2) | 2.2 (1.5–3.3) | 2.0 (1.2–3.2) | 1.3 (0.7–2.7) |
| Model 5 (model 4 + blood pressure variables) | 1.0 | 1.9 (1.4–2.6) | 2.2 (1.4–3.3) | 1.8 (1.1–3.0) | 1.5 (0.7–3.1) |
Socioeconomic factors are income, education, insurance
Metabolic variables include diabetic status, BMI, total and high-density lipoprotein cholesterol
Behaviors included are cigarette smoking and physical activity
Blood pressure includes systolic and diastolic blood pressure and use of antihypertensive medications
Figure 3. Left ventricular mass difference in means from non-Hispanic whites.
Multivariate regression modeling of left ventricular mass percent predicted as a continuous variable by Race-Ethnicity and Hispanic Subgroups
LV Geometry among Hispanic Subgroups
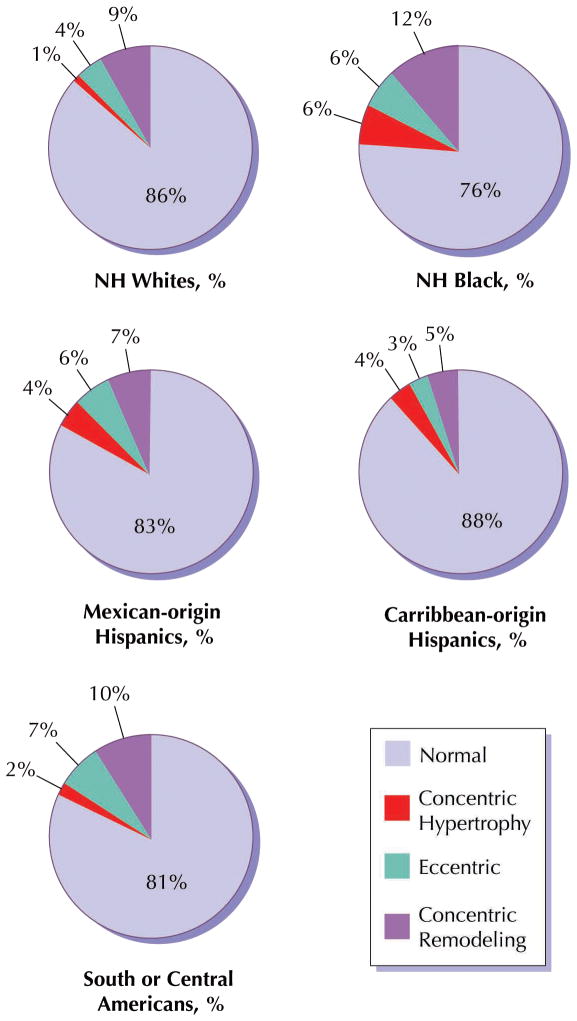
Compared to those with normal LV geometry, those with concentric hypertrophy were 53% more likely to be hypertensive with systolic and diastolic blood pressures 23.8 and 8.3mmHg higher respectively. All Hispanic subgroups had higher prevalence of concentric hypertrophy compared to non-Hispanic whites with Mexican-origin Hispanics having the highest prevalence similar to that of non-Hispanic blacks. Eccentric hypertrophy was most common among non-Hispanic blacks and all Hispanic subgroups compared to non-Hispanic whites. Among Hispanic subgroups, prevalence of concentric remodeling was not increased compared to non-Hispanic whites. (Figure 4) In contrast, only non-Hispanic blacks had a significantly increased risk for elevated M-C ratio compared to non-Hispanic whites. In sequential covariate adjustments or in the full multivariate model for LV remodeling the results did not change significantly except among non-Hispanic blacks. (Table 4) A separate analysis substituting LVM indexed by body surface area in all our regression models yielded qualitatively similar results.
Figure 4. Percent Breakdown of Four left ventricular remodeling patterns across Race.
Ethnicity and Hispanic Subgroup—Prevalence of abnormal remodeling patterns is higher among Hispanic subgroups compared to non-Hispanic whites (differences were significant at the p<0.0001 level).
Table 4.
Odds Ratios of Ventricular Remodeling (elevated M-C Ratio ≥95th percentile) by Race-Ethnicity and Hispanic Subgroup after Sequential Adjustment for Covariates
| Non-Hispanic Whites n=1959 | Non-Hispanic Black n=1286 | Mexican-origin Hispanics n=574 | Caribbean-origin Hispanics n=329 | South or Central American n=161 | |
|---|---|---|---|---|---|
| Unadjusted | 1.0 | 1.9 (1.6–2.3) | 1.1 (0.8–1.5) | 1.1 (0.8–1.7) | 0.9 (0.5–1.6) |
| Model 1 (age and sex) | 1.0 | 2.1 (1.7–2.6) | 1.2 (0.9–1.6) | 1.3 (0.9–1.9) | 1.0 (0.6–1.8) |
| Model 2 (model 1+ socioeconomic factors) | 1.0 | 1.9 (1.5–2.3) | 0.9 (0.7–1.3) | 1.0 (0.7–1.6) | 0.7 (0.4–1.3) |
| Model 3 (model 2 + metabolic variables) | 1.0 | 1.7 (1.3–2.1) | 0.8 (0.5–1.1) | 1.0 (0.7–1.5) | 0.6 (0.3–1.2) |
| Model 4 (model 3 + behaviors) | 1.0 | 1.7 (1.3–2.1) | 0.8 (0.6–1.1) | 1.0 (0.7–1.6) | 0.7 (0.4–1.2) |
| Model 5 (model 4 + blood pressure variables) | 1.0 | 1.4 (1.1–1.8) | 0.8 (0.6–1.2) | 0.9 (0.6–1.4) | 0.7 (0.4–1.3) |
Socioeconomic factors are income, education, insurance
Metabolic factors are BMI, diabetic Status, total and high-density lipoprotein cholesterol
Behaviors included are cigarette smoking and physical activity
Blood pressure variables include systolic and diastolic blood pressure and use of antihypertensive medications
DISCUSSION
We report an increased prevalence of LVH among Hispanic subgroups compared with non-Hispanic whites. Caribbean-origin Hispanics had a two-fold increased odds of LVH compared to non-Hispanic whites which was explained, in part due to an elevated prevalence of hypertension. Mexican-origin Hispanics had a similar two-fold increased odds of LVH compared to non-Hispanic whites despite no increase in the prevalence of hypertension. All Hispanic subgroups had a significantly higher prevalence of concentric and eccentric hypertrophy compared to non-Hispanic whites.
Heterogeneity of the Hispanic Population/Hispanic Subgroups
These data suggest that Hispanics are not monolithic with respect to cardiovascular risk but that different subgroups originating in different geographic areas of Latin America manifest significant differences in the distribution of LVH and the type of ventricular remodeling. This is concordant with other studies demonstrating that CVD risk factors and measures of subclinical atherosclerosis differ between Hispanic subgroups (25).
In the U.S. Hispanic population, heart disease and stroke are the leading cause of mortality.(26) LVH has been recognized as important for CV prognosis, (8) however, Hispanics remain understudied with regards to LVH and CV risk factors among their respective subgroups. Concerns about CVD among Hispanics may be muted by a perception that Hispanics are less susceptible to CVD than the general population. This perception, known as the “Hispanic Paradox,” contends that Hispanics have lower CV mortality risk than non-Hispanic whites,(27) but this hypothesis may not apply uniformly across subgroups of Hispanics. The ‘Hispanic Paradox’ has been contradicted in recent studies(28). Our findings demonstrate that Hispanics are a high CV risk group and highlight the fact that Hispanics subgroup differences need to be appreciated when considering CV risk.
LV Geometry among Hispanic Subgroups
Since increased LVM can be physiologic or pathologic, cardiac dimensions and remodeling must be considered. Concentric hypertrophy is associated with more adverse patterns of target organ damage than either eccentric hypertrophy or concentric remodeling(29,30). Koren, et al.(31) reported that hypertensive patients with concentric LVH had the highest risk of mortality followed by those with eccentric LVH and concentric remodeling. Caribbean-origin and Mexican-origin Hispanics, in particular had increased prevalence of concentric hypertrophy compared to non-Hispanic whites. In contrast, elevated M-C ratio alone was not significantly different among the Hispanic subgroups relative to non-Hispanic whites.
Differential Determinants of LVH among Hispanic Subgroups
The increased prevalence of LVH and abnormal LV remodeling among Mexican-origin Hispanics despite lower prevalence of hypertension is an interesting and unexpected finding. This may be related to elevated prevalence rates of obesity, diabetes, and metabolic syndrome observed in our cohort of Mexican-origin Hispanics. Diabetic patients without overt heart disease have been shown to have cardiac structural changes similar to those caused by LVH (32,33). Furthermore, many of those with diabetes or metabolic syndrome may not be diagnosed with hypertension even though their systolic blood pressure is above goal of 130/80mmHg.
It is not surprising that significant differences in LVH existed despite modest differences in hypertension prevalence since LVH has several determinants besides blood pressure or established hypertension. Furthermore, changes in LVM can occur in the setting of changes in adrenergic state, such as with psychosocial stress, despite overt changes in blood pressure (34). Adjustment for socioeconomic covariates accounted for a fraction of the odds of having LVH among Mexican-origin Hispanics. Socioeconomic indices may be better reflectors of changes in blood pressure over the life course accounting for unmeasured behavioral factors as well as levels of psychosocial stress (7).
While disparities regarding hypertension awareness, control, treatment rates among non-Hispanic blacks and whites may be making steps to being eliminated,(35) the same may not hold true for Hispanics and their respective subgroups (5). In our cohort, Mexican-origin Hispanics had significantly lower levels of hypertension treatment than non-Hispanic whites and other Hispanic subgroups. This may be related to issues of access to care, patient-physician relationships or medication adherence and would affect levels of target organ damage in this Hispanic subgroup despite lower hypertension prevalence.
The role of acculturation in the development of hypertension and LVH among Hispanics is conflicting and poorly studied. In some studies, acculturation seemed to be a strong predictor of hypertension,(36) although other studies of Mexican-origin Hispanics showed that the process of acculturation was not a major predictor (37).
Genetic Ancestry as a Potential Determinant of LVH among Hispanic Subgroups
Latin American populations originated as a result of the Spanish conquest of the Americas and subsequent admixture between Native American, European, and West African individuals. Caribbean-origin Hispanic and Mexican-origin Hispanic populations are genetically and culturally very different even if both are considered to be Hispanic. Genetic admixture studies in samples of Hispanics in the western and southwestern U.S. reflect mostly European and Native American admixture (38). Hispanics in the eastern and northeast U.S. conform more closely to predominating European and West African admixture (39). Given a higher proportion of West African ancestry, Caribbean-origin Hispanics may be more salt sensitive thus affecting their prevalence of hypertension, LVH and abnormal LV remodeling (40). Whether geographic ancestral origins contribute to the differential distribution of disease among Hispanic subgroups remains to be studied.
Limitations
Although population-based, MESA is not a representative sample of the U.S. Hispanic population due to its design and the exclusion of those with prevalent cardiovascular disease. Furthermore, the sample who completed MRI were healthier that the overall cohort. Hence our sample represents a lower risk group compared with the entire community, which is likely to have underestimated the burden of LVH in the Hispanic population. Blood pressure measurements used in this analysis were recorded at a single office visit, which may affect the estimate of hypertension prevalence and the ability to adjust for lifetime experience of hypertension. We indexed LVM using body surface area as well as allometric scaling, which is the methodology best supported by the current literature (21). Both models yielded qualitatively similar results. We used percent-predicted LVM as our measure of heart size to remove the effect of the normal physiologic relation of body size and heart size and allow for a more sensitive measure of differences between the racial/ethnic groups that is independent of their different body size characteristics. However, LVM differences in our race-ethnic groups may be due in part to residual confounding by body size. Unmeasured variables may account for some of the observed differences. For example, Hispanic subgroup classification may be a surrogate for other psychosocial factors that may have contributed to these disparities. Virtually all Caribbean-origin Hispanics came from the East Coast sites and a large proportion Mexican-origin Hispanics came from the West Coast sites. Whether or not this differential distribution caused any potential for confounding by site and thus bias in our analyses is unclear.
Conclusions
To our knowledge, this is the first comparative analysis of Hispanic subgroups in a single cohort. We demonstrate differential prevalence of hypertension, LVH and abnormal LV remodeling across Hispanic subgroups, which illustrates the heterogeneity of the Hispanic population. Efforts are warranted to better recognize, understand and address differences among Hispanic ethnic groups to prevent CVD events in this large subset of the U.S. population.
Acknowledgments
Funding sources:
This research was supported by contracts N01-HC-95159 and N01-HC-95168 from the National Heart, Lung, and Blood Institute.
Dr. Rodriguez is supported by the Robert Wood Johnson Harold Amos Medical Faculty Development Program and a National Heart, Lung, and Blood Institute’s Mentored Patient-Oriented Research Career Development Award (K23 HL079343-01A2).
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org
Abbreviations
- MRI
magnetic resonance imaging
- MESA
Multi Ethnic Study of Atherosclerosis
- CVD
cardiovascular disease
- LVM
left ventricular mass
- LVH
left ventricular hypertrophy
- M-C
mass-cavity ratio
- BMI
body mass index
- CI
confidence intervals
- OR
odds ratio
- PR
prevalence ratio
Footnotes
Disclosures: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Health Disparities Experienced By Hispanics Reported by: Office of Minority Health, Office of the Director, CDC. Morb Mortal Wkly Rep. 2004;53:935–7. [PubMed] [Google Scholar]
- 2.Davidson JA, Kannel WB, Lopez-Candales A, et al. Avoiding the looming Latino/Hispanic cardiovascular health crisis: a call to action. Ethn Dis. 2007;17:568–73. [PubMed] [Google Scholar]
- 3.Ramirez RR, dela Cruz GP. Current Population Reports. U.S. Census Bureau; Washington, D.C: 2002. The Hispanic Population in the United States: March 2002; pp. 20–545. [Google Scholar]
- 4.Hanis CL, Hewett-Emmett D, Bertin TK, Schull WJ. Origins of U.S. Hispanics. Implications for diabetes. Diabetes Care. 1991;14:618–27. doi: 10.2337/diacare.14.7.618. [DOI] [PubMed] [Google Scholar]
- 5.Racial/ethnic disparities in prevalence, treatment, and control of hypertension--United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54:7–9. [PubMed] [Google Scholar]
- 6.Sacco RL, Boden-Albala B, Abel G, et al. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke. 2001;32:1725–31. doi: 10.1161/01.str.32.8.1725. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez CJ, Sciacca RR, Diez-Roux AV, et al. Relation between socioeconomic status, race-ethnicity, and left ventricular mass: the Northern Manhattan study. Hypertension. 2004;43:775–9. doi: 10.1161/01.HYP.0000118055.90533.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–6. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez CJ, Lin F, Sacco RL, et al. Prognostic implications of left ventricular mass among Hispanics: the Northern Manhattan Study. Hypertension. 2006;48:87–92. doi: 10.1161/01.HYP.0000223330.03088.58. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz HM, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the Framingham Heart Study. J Am Coll Cardiol. 1995;25:879–84. doi: 10.1016/0735-1097(94)00473-4. [DOI] [PubMed] [Google Scholar]
- 11.Verdecchia P, Schillaci G, Borgioni C, et al. Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive patients with normal left ventricular mass. J Am Coll Cardiol. 1995;25:871–8. doi: 10.1016/0735-1097(94)00424-O. [DOI] [PubMed] [Google Scholar]
- 12.Moriuchi M, Saito S, Kasamaki Y, Komaki K, Kanmatsuse K, Hayasaka K. Three-dimensional analysis of left ventricular geometry using magnetic resonance imaging: feasibility and comparison with echocardiographic analysis. J Cardiol. 2003;42:249–60. [PubMed] [Google Scholar]
- 13.Verma A, Meris A, Skali H, et al. Prognostic implications of left ventricular mass and geometry following myocardial infarction: the VALIANT (VALsartan In Acute myocardial iNfarcTion) Echocardiographic Study. JACC Cardiovasc Imaging. 2008;1:582–91. doi: 10.1016/j.jcmg.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez Burchard E, Borrell LN, Choudhry S, et al. Latino populations: a unique opportunity for the study of race, genetics, and social environment in epidemiological research. Am J Public Health. 2005;95:2161–8. doi: 10.2105/AJPH.2005.068668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13:477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flegal KM, Ezzati TM, Harris MI, et al. Prevalence of diabetes in Mexican Americans, Cubans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care. 1991;14:628–38. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- 17.Bild DE, Detrano R, Peterson D, et al. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–20. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 19.Natori S, Lai S, Finn JP, et al. Cardiovascular function in multi-ethnic study of atherosclerosis: normal values by age, sex, and ethnicity. AJR Am J Roentgenol. 2006;186:S357–65. doi: 10.2214/AJR.04.1868. [DOI] [PubMed] [Google Scholar]
- 20.Keller AM, Peshock RM, Malloy CR, et al. In vivo measurement of myocardial mass using nuclear magnetic resonance imaging. J Am Coll Cardiol. 1986;8:113–7. doi: 10.1016/s0735-1097(86)80100-0. [DOI] [PubMed] [Google Scholar]
- 21.Dewey FE, Rosenthal D, Murphy DJ, Jr, Froelicher VF, Ashley EA. Does size matter? Clinical applications of scaling cardiac size and function for body size. Circulation. 2008;117:2279–87. doi: 10.1161/CIRCULATIONAHA.107.736785. [DOI] [PubMed] [Google Scholar]
- 22.Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–6. [PubMed] [Google Scholar]
- 24.Heckbert SR, Post W, Pearson GD, et al. Traditional cardiovascular risk factors in relation to left ventricular mass, volume, and systolic function by cardiac magnetic resonance imaging: the Multiethnic Study of Atherosclerosis. J Am Coll Cardiol. 2006;48:2285–92. doi: 10.1016/j.jacc.2006.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:962–9. doi: 10.1093/aje/kwm402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Association AH. Heart Disease and Stroke Statistics—2009 Update. Circulation. 2009;119:e21–e181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 27.Liao Y, Cooper RS, Cao G, Kaufman JS, Long AE, McGee DL. Mortality from coronary heart disease and cardiovascular disease among adult U.S. Hispanics: findings from the National Health Interview Survey (1986 to 1994) J Am Coll Cardiol. 1997;30:1200–5. doi: 10.1016/s0735-1097(97)00278-7. [DOI] [PubMed] [Google Scholar]
- 28.Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP, Hazuda HP. All-cause and cardiovascular mortality among Mexican-American and non-Hispanic White older participants in the San Antonio Heart Study- evidence against the “Hispanic paradox”. Am J Epidemiol. 2003;158:1048–57. doi: 10.1093/aje/kwg249. [DOI] [PubMed] [Google Scholar]
- 29.Roman MJ, Pickering TG, Schwartz JE, Pini R, Devereux RB. Relation of arterial structure and function to left ventricular geometric patterns in hypertensive adults. J Am Coll Cardiol. 1996;28:751–6. doi: 10.1016/0735-1097(96)00225-2. [DOI] [PubMed] [Google Scholar]
- 30.Cuspidi C, Macca G, Michev I, et al. Left ventricular concentric remodelling and extracardiac target organ damage in essential hypertension. J Hum Hypertens. 2002;16:385–90. doi: 10.1038/sj.jhh.1001420. [DOI] [PubMed] [Google Scholar]
- 31.Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114:345–52. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 32.Devereux RB, Roman MJ, de Simone G, et al. Relations of left ventricular mass to demographic and hemodynamic variables in American Indians: the Strong Heart Study. Circulation. 1997;96:1416–23. doi: 10.1161/01.cir.96.5.1416. [DOI] [PubMed] [Google Scholar]
- 33.Fang ZY, Yuda S, Anderson V, Short L, Case C, Marwick TH. Echocardiographic detection of early diabetic myocardial disease. J Am Coll Cardiol. 2003;41:611–7. doi: 10.1016/s0735-1097(02)02869-3. [DOI] [PubMed] [Google Scholar]
- 34.Julius S, Li Y, Brant D, Krause L, Buda AJ. Neurogenic pressor episodes fail to cause hypertension, but do induce cardiac hypertrophy. Hypertension. 1989;13:422–9. doi: 10.1161/01.hyp.13.5.422. [DOI] [PubMed] [Google Scholar]
- 35.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 36.Moran A, Roux AV, Jackson SA, et al. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–63. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 37.Markides KS, Lee DJ, Ray LA. Acculturation and hypertension in Mexican Americans. Ethn Dis. 1993;3:70–4. [PubMed] [Google Scholar]
- 38.Bertoni B, Budowle B, Sans M, Barton SA, Chakraborty R. Admixture in Hispanics: distribution of ancestral population contributions in the Continental United States. Hum Biol. 2003;75:1–11. doi: 10.1353/hub.2003.0016. [DOI] [PubMed] [Google Scholar]
- 39.Bonilla C, Shriver MD, Parra EJ, Jones A, Fernandez JR. Ancestral proportions and their association with skin pigmentation and bone mineral density in Puerto Rican women from New York city. Hum Genet. 2004;115:57–68. doi: 10.1007/s00439-004-1125-7. [DOI] [PubMed] [Google Scholar]
- 40.Laffer CL, Elijovich F. Essential hypertension of Caribbean Hispanics: sodium, renin, and response to therapy. J Clin Hypertens (Greenwich) 2002;4:266–73. doi: 10.1111/j.1524-6175.2002.00973.x. [DOI] [PMC free article] [PubMed] [Google Scholar]