Abstract
Objective
A better understanding of the long-term scope and impact of the comorbidity with oppositional defiant disorder (ODD) in girls with attention-deficit/hyperactivity disorder (ADHD) has important clinical and public health implications. However, most of the available information on the subject derives from predominantly male samples. This study evaluated the longitudinal course and impact of comorbid ODD in a large sample of girls with ADHD.
Methods
Subjects were pediatrically and psychiatrically referred girls with and without ADHD assessed blindly at baseline (mean age=11.6 years), and 5 years later (mean age=16.6 years) by mid to late adolescence. The subjects' diagnostic status of ADHD with and without comorbid ODD at baseline was used to define three groups (Controls [N=107], ADHD [N=77), ADHD+ODD [N=37]). Outcomes were examined using logistic regression (for binary outcomes) and linear regression (for continuous outcomes).
Results
Compared with girls who had ADHD only, those with ADHD+ODD at baseline had a significantly increased risk for ODD and major depression at follow-up. Both groups of girls with ADHD had an increased risk for CD and bipolar disorder at follow-up.
Conclusions
These longitudinal findings in girls with ADHD support and extend previously reported findings in boys indicating that ODD heralds a compromised outcome for girls with ADHD in adolescence.
Keywords: Oppositional, ADHD, children, adolescents, girls, females
INTRODUCTION
The comorbidity between attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) has been well documented in culturally and regionally diverse epidemiological1,2 and clinical samples.3,4 Although the prevalence of ODD is lower in girls than in boys with ADHD, it is clearly overrepresented in samples of girls with ADHD relative to controls without ADHD.5–7
An emergent literature documents that ODD is a morbid disorder. Greene and colleagues8 found that ODD significantly predicted compromised psychiatric, family and social functioning relative to other psychiatric comparison subjects independently of the presence of conduct disorder (CD). Similar findings were identified in our investigation of the course of ODD in a large longitudinal sample of referred boys with and without ADHD followed up into adolescent years.9 Comorbid externalizing disorders have also been shown to increase the risk for substance use in longitudinal studies of children with ADHD.10,11 However, because these studies have been almost exclusively based on samples of boys, there is a paucity of information on the course and outcome of ODD in girls with ADHD. Also, because ODD has been studied largely within the context of conduct disorder (CD), little is known about ODD proper.
A better understanding of the long-term scope and impact of the comorbidity with ODD outside the context of CD in girls with ADHD would be useful in forecasting prognosis. Such knowledge would alert clinicians to the importance of recognizing ODD in girls with ADHD for treatment planning as well as help design improved preventive and early intervention programs. The ability to predict the course of ODD in girls with ADHD could help focus limited societal resources on those at higher risk for compromised outcomes.12,13
The main aim of this study was to evaluate functional impairments associated with ODD outside the context of CD among Girls with ADHD. To this end, we used longitudinal data from a large, well-characterized sample of pediatrically and psychiatrically referred girls with and without ADHD followed prospectively for five years into adolescence. We hypothesized that comorbidity with ODD outside the context of CD in girls with ADHD will be associated with a more compromised outcome compared to Girls with ADHD without this comorbidity. To the best of our knowledge, this represents the first comprehensive evaluation of the longitudinal course of the ODD in girls with ADHD.
METHODS
Subjects
Detailed study methodology has been previously described.5,6 Briefly, subjects were derived from a longitudinal case-control family study of ADHD in girls.5,6 At baseline, we studied female subjects aged 6–18 years with (N=140) and without (N=122) ADHD ascertained from pediatric and psychiatric sources. Potential subjects were excluded if they had been adopted, if their nuclear family was not available for study, if they had major sensorimotor handicaps (paralysis, deafness, blindness), psychosis, autism, or inadequate command of the English language (i.e., unable to participate in the structured interview due to English as a second language or expressive language problems). Due to the potential for subjects with low IQ to have a differing genetic etiology for their disorder and/or cognitive dysfunction, subjects were excluded if they had full Scale IQ less than 80. All of the ADHD subjects met full diagnostic criteria for ADHD at the time of the clinical referral; at the time of recruitment they all had active symptoms of the disorder. Parents and adult offspring provided written informed consent to participate, and parents also provided consent for offspring under the age of 18. Children and adolescents provided written assent to participate. The human research committee at Massachusetts General Hospital approved this study protocol. Subjects were ascertained from pediatric and psychiatric sources.
A three-stage ascertainment procedure was used to select subjects.14 For ADHD subjects, the first stage was their referral to a psychiatric or pediatric clinic resulting in a clinical diagnosis of ADHD by a child psychiatrist or pediatrician. The second stage confirmed the diagnosis by screening all children positive at the first stage by administering a telephone questionnaire to their mothers. Eligible children meeting the first two stages of entry criteria were recruited for the study and received the third stage, a diagnostic assessment with a structured interview. Only patients who received a positive diagnosis at all three stages were included in the final analysis. We also screened potential non-ADHD controls in three stages. First, we ascertained them from consecutive referrals to medical clinics for routine physical examinations at both the psychiatric and pediatric sources. In stage two, the control mothers responded to an ADHD telephone questionnaire about their daughters. Eligible controls meeting study entry criteria were recruited for the study and received the third stage, a diagnostic assessment with a structured interview. Only subjects classified as not having ADHD at all three stages were included in the control group.
Psychiatric assessments at the 5-year follow-up relied on the Schedule for Affective Disorders and Schizophrenia for School-Aged Children – Epidemiologic Version (K-SADS-E) revised to capture DSM-IV diagnoses15 for subjects younger than 18 years of age and the Structured Clinical Interview for DSM-IV (SCID)16 (supplemented with modules from the K-SADS-E to assess childhood diagnoses) for subjects 18 years of age and older. We conducted direct interviews with subjects and indirect interviews with their mothers (i.e., interviews with the mother about the child). We considered a disorder positive if DSM-IV diagnostic criteria were unequivocally met in either interview.
Assessments were conducted by highly trained and closely supervised psychometricians. We computed kappa coefficients of agreement by having experienced, board certified child and adult psychiatrists and licensed clinical psychologists diagnose subjects from audio taped interviews. Based on 500 assessments from interviews of children and adults, the median kappa coefficient was 0.98. Kappa coefficients for individual diagnoses included: ADHD (0.88), conduct disorder (1.0), major depression (1.0), mania (0.95), separation anxiety (1.0), agoraphobia (1.0), panic (0.95), substance use disorder (1.0), and tics/Tourette's (0.89). The diagnosis of major depression was made only if the depressive episode was associated with marked impairment.17,18 Since there are many anxiety disorders measured by our structured interviews, we aggregated them into a binary measure coded positive if two or more anxiety disorders were endorsed, and negative otherwise.19 Psychoactive substance use disorder (PSUD) was defined as any alcohol abuse, alcohol dependence, substance abuse, or substance dependence. Diagnostic outcomes at the 5-year follow-up were considered positive if full criteria were met any time after baseline assessment (i.e., interval diagnosis). Socioeconomic status (SES) was measured using the 5-point Hollingshead scale.20 As a measure of overall functioning, we used the DSM-IV Global Assessment of Functioning (GAF).15
In addition to structured diagnostic methodology, assessment of psychopathology relied on the CBCL completed by the participant's mother. We used eight clinical scales from the CBCL:21 Withdrawn, Somatic Complaints, Anxious/Depressed, Social Problems, Thought Problems, Attention Problems, Delinquent Behavior, and Aggressive Behavior. Scores on the scales are reported as T scores having a mean of 50 and a standard deviation of 10. The age-appropriate norms were used for converting participants' CBCL raw scores into T scores, at both baseline and follow-up.
A committee of board-certified child and adult psychiatrists who were blind to the subject's ADHD status, referral source, and all other data resolved diagnostic uncertainties. Diagnoses presented for review were considered positive only if a consensus was achieved that criteria were met to a degree that would be considered clinically meaningful. We estimated the reliability of the diagnostic review process by computing kappa coefficients of agreement for clinician reviewers. For these diagnoses, the median reliability between individual clinicians and the review committee assigned diagnoses was 0.87. Kappa coefficients for individual diagnoses included: ADHD (1.0), conduct disorder (1.0), major depression (1.0), bipolar (0.78), separation anxiety (0.89), agoraphobia (0.80), panic (0.77), substance use disorder (1.0), and tics/Tourette's (0.68).
Statistical Procedures
The subjects' diagnostic status of ADHD, ODD, and CD at baseline defined the independent variable. Dependent variables included interval diagnoses, CBCL at baseline and follow-up, and school functioning. Outcomes were tested using logistic regression (for binary outcomes) and linear regression (for continuous outcomes) controlling for demographic confounders. To adjust for multiple comparisons, Holm's sequential Bonferroni procedure was used to set alpha levels for the omnibus tests of the 29 outcome variables. If the omnibus test was significant, an alpha level of 0.05 was used for pairwise comparisons.
RESULTS
Attrition and Demographics
As previously described6 of the 140 ADHD and 122 control subjects recruited at baseline, 123 (88%) and 112 (92%), respectively, were successfully reassessed at the 5-year follow-up. The rate of successful follow-up did not differ between the groups (p=0.30). Among ADHD and control subjects, there were no significant differences between those successfully followed up and those lost to follow-up on socioeconomic status (SES), age, GAF score, familial intactness, ascertainment source, or psychiatric comorbidity (all p values >0.05).
Subjects assessed at follow-up were grouped based on baseline diagnoses of ADHD and ODD diagnoses: Control subjects without ODD (Controls, N=107), ADHD subjects without ODD (ADHD, N=77), and ADHD subjects with non-CD ODD (ADHD+ODD, N=37). Because there were only nine ADHD subjects with a diagnosis of conduct disorder at baseline, these were removed from the analysis. There were not enough Controls with ODD to define a separate group, so the five control subjects with ODD were also excluded. As depicted in Table 1, the three groups did not differ significantly on any sociodemographic characteristics. The ADHD and ADHD+ODD groups did not have significantly different rates of lifetime pharmacotherapy for ADHD at baseline (66% versus 73%, respectively, χ2(1)=0.53, p=0.47). The ADHD+ODD group had a significantly higher rate of lifetime counseling at baseline compared to the ADHD group (67% versus 39%, χ2(1)=8.19, p=0.004).
Table 1.
Demographics represented by mean ± standard deviation or N (%).
| Controls (N=107) | ADHD (N=77) | ADHD+ODD (N=37) | Test Statistic | p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age at baseline (years) | 12.1 ± 2.9 | 11.2 ± 3.4 | 11.0 ± 3.1 | F(2,218)=2.48 | 0.09 |
| Ethnicity (Caucasian) | 94 (90) | 72 (95) | 36 (97) | χ2(2)=2.52 | 0.28 |
| Socioeconomic status | 1.7 ± 0.8 | 1.8 ± 0.9 | 1.9 ± 0.9 | χ2(2)=2.37 | 0.31 |
| Intact family | 89 (83) | 54 (70) | 27 (73) | χ2(2)=4.68 | 0.10 |
| Ascertainment source (psychiatric) | 46 (43) | 30 (39) | 21 (57) | χ2(2)=3.28 | 0.19 |
Psychiatric Outcomes at the 5-year Follow-up
Omnibus tests were significant for all psychiatric disorders at the 5-year follow-up (p<0.001) With the exception of psychoactive substance use disorders (p=0.27) and smoking (p=0.01). The large majority of the ADHD and ADHD+ODD groups maintained the ADHD diagnosis during the follow-up period (Figure 1, 81.8% and 75.0%, respectively). The majority (62.2%) of the ADHD+ODD group had ODD in the follow-up period.
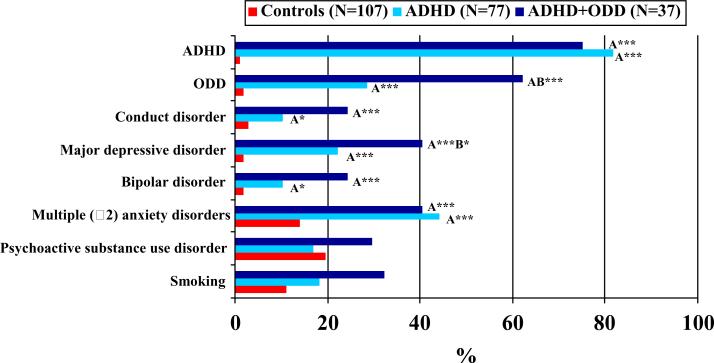
Figure 1.
Diagnoses at five-year follow-up in girls with ADHD and ODD, with ADHD without ODD, and controls.
A=vs. Controls, B=vs. ADHD; *p≤0.05, **p≤0.01, ***p≤0.001
Compared to the Controls, the ADHD group had significantly higher rates of ODD (28.6% versus 1.9%), conduct disorder (10.4% versus 2.8%), major depressive disorder with severe impairment (22.1% versus 1.9%), bipolar disorder (10.4% versus 1.9%), and multiple (≥2) anxiety disorders (44.2% versus 14.0%, Figure 1). ADHD+ODD was associated with a significantly increased risk for ODD and major depressive disorder beyond that conferred by ADHD alone. Although not reaching statistical significance (both p=0.06), the ADHD+ODD group had rates of conduct disorder and bipolar disorder twice as high as the ADHD group at follow-up.
As a post-hoc analysis, we tested whether the association between ODD and the risk for subsequent major depressive disorder varied by age. We found that girls aged 11 years or younger at baseline in the ADHD+ODD group (N=21) were at higher risk for major depressive disorder at follow-up compared to girls from the ADHD group aged 11 years or younger (N=42, 38.1% versus 11.9%, p=0.02). However, among girls aged 12 years and older at baseline, no difference was found between the ADHD (N=35) and ADHD+ODD (N=16) groups in the rate of major depressive disorder (34.3 versus 43.4%, p=0.52).
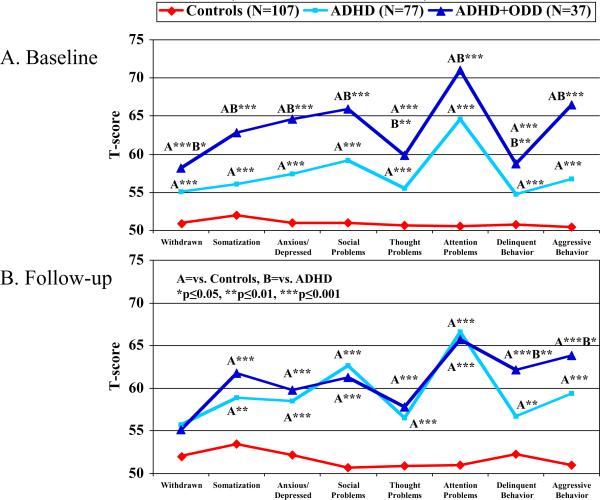
Consistent with the structured diagnostic interview findings are the Child Behavior Checklist (CBCL) results. With the exception of the Withdrawn T-score at follow-up (p=0.02), omnibus tests were significant for all CBCL T-scores (p<0.001). As shown in Figure 2A, at baseline, while the ADHD group had significantly more impaired T-scores than Controls on all the clinical subscales of the CBCL, the ADHD+ODD group had significantly more impaired T-scores than the ADHD group on all subscales of the CBCL. At follow-up (Figure 2B), while most of the subscales in the ADHD+ODD group had dropped down to the level of ADHD group, the Delinquent and Aggressive Behavior T-scores remained significantly higher than those of the ADHD group. Subjects older than 18 years of age did not have CBCL data and were not included in these analyses.
Figure 2.
Child Behavior Checklist profiles in girls with ADHD and ODD, ADHD without ODD, and controls.
School Outcomes at the 5-year Follow-up
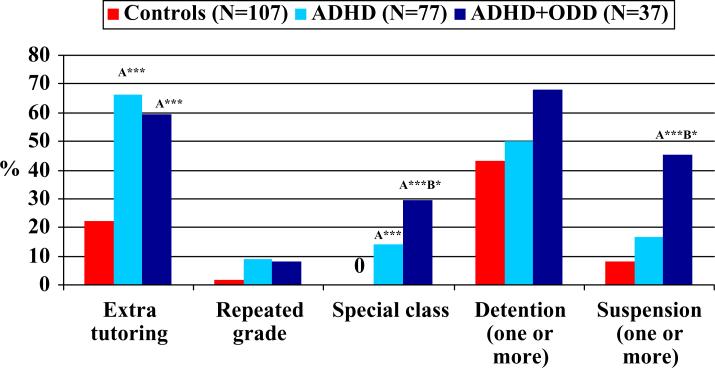
Omnibus tests were significant for need for extra tutoring, placement in a special class, and suspension from school (all p<0.001), but not repeated grade (p=0.08) or detention (p=0.09). As shown in Figure 3, while ADHD was associated with an increased risk for placement in a special class and need for extra tutoring at the 5-year follow-up, ADHD+ODD significantly added to the risk for placement in a special class (29.7%) above that conferred by ADHD alone (14.3%). Nearly half (45.4%) of the ADHD+ODD group had been suspended from school at least once, significantly higher than the ADHD group (16.7%) and Controls (8.2%). Note that while extra tutoring, special class, and repeated grade were interval outcomes, detention and suspension from school were lifetime outcomes (interval was not available).
Figure 3.
School outcomes at five-year follow-up in girls with ADHD and ODD, with ADHD without ODD, and controls.
A=vs. Controls, B=vs. ADHD; *p≤0.05, **p≤0.01, ***p≤0.001
DISCUSSION
We have investigated the longitudinal course of ODD in girls with ADHD outside the context of CD. At the 5-year follow-up assessment into adolescence, ODD at baseline predicted a significantly increased risk for ODD and major depression at follow-up beyond the risk conferred by ADHD alone. These findings expand on previous results from longitudinal studies of girls with ADHD6,22 by identifying the risks associated with comorbid ODD.
Our findings documenting that ODD (in the absence of CD) in girls with ADHD selectively increases the risks for ODD and major depression are highly consistent with our recently reported findings in a sample of boys with ADHD followed longitudinally over 10 years into young adult years.3 These findings are also consistent with results reported by Greene and colleagues8 in a cross-sectional pediatric sample that also found a strong association between ODD and MDD. These findings are also consistent with those recently reported by Brotman and colleagues23 on the longitudinal course of children with “chronic irritability and hyperarousal” (also termed severe mood dysregulation or “SMD”) largely comprising youth with ADHD and ODD. In addition, our post-hoc test by age group suggests that early onset ODD may be a more potent risk factor for MDD in adolescence.
Although not statistically significant, the finding that both ADHD and ODD in girls increased the risk for CD at the adolescent follow up is consistent with our previous longitudinal study of boys with ADHD as well as other studies in the literature. While some longitudinal prospective studies of clinic-referred children suggested that childhood ADHD predicts later antisocial behavior,24,25 others suggested that childhood ADHD only appears to be a risk factor for adolescent CD when childhood disruptive behavior problems are also present.26,27 For example, in this study of girls with ADHD, as well as in our previous study of boys with ADHD, the risk for CD was larger when comorbid with ODD (24% versus 10% in girls, p=0.06). More definitive conclusions as to the nature of the association between ADHD, ODD, CD, and antisocial personality disorder in girls with ADHD await longer follow-up studies and studies that include a sufficiently powered sample of girls with CD.
Although the finding that both ADHD and ODD increased the risk for bipolar disorder are consistent with an emerging literature linking these three disorders,28,29 they are discrepant with the findings reported in our longitudinal study of boys with ADHD grown up, showing that the risk for bipolar disorder was selectively associated with CD.30 It is noteworthy however that the risk for bipolar disorder was larger in girls with ADHD with comorbid ODD compared to those without this comorbidity (24% versus 10%, p=0.06). More work is needed with longer follow-up studies to better understand the nature of the association between ADHD, ODD, and subsequent bipolar disorder in girls with ADHD.
While we did not find a difference among the groups for PSUD and the apparent differences for smoking did not survive adjustment for multiple comparisons (p=0.01), the sample was still young at follow-up (average age=16.6 years). Additional follow-ups are needed to understand the relationship between ADHD, ODD, and substance use.
Our CBCL results showing that girls with ADHD with comorbid ODD could be distinguished from other girls with ADHD without ODD by their more severe CBCL profile are consistent with our previous findings in boys with ADHD. Equally important is the result showing that at follow-up, girls with ADHD plus ODD selectively differed from other girls with ADHD without ODD on the CBCL Aggressive Behavior and Delinquent scales, scales previously shown to correspond to structured interview derived diagnoses of ODD32 and CD.33,34 It is also noteworthy that this profile of elevations of the Aggressive and Delinquent scales of the CBCL is the same as was previously identified in a sample of boys as being predictive of boys with ODD who subsequently developed CD at the 10-year follow-up. If these results are confirmed in future follow-up studies, the ability to distinguish girls ODD at higher risk to develop subsequent CD by their CBCL profile is of high clinical and public health significance.
While ODD increased the risk for major depression at follow-up, ODD was not associated with a higher score on the CBCL Anxious/Depressed scale. The inclusion of anxiety questions in the Anxious/Depressed scale may explain why an effect was not found, because ODD was not associated with multiple anxiety disorders at follow-up. In addition, the Anxious/Depressed scale contains primarily symptoms about depressed mood (e.g., cries, worthless, sad), and it is possibility that subjects with ODD tend to have a more symptoms related to an irritable or cranky mood. Further work is needed to answer this question.
Further evidence for a compromised course associated with the comorbidity of ODD in girls with ADHD can be seen in the findings that this comorbidity predicted a higher likelihood of placement in special classes and school suspension. The compromised course associated with ODD in girls with ADHD is consistent with findings from a recent study by Harpold and colleagues35 in adults with ADHD. This study found that 30% of referred adults with ADHD and comorbid ODD in childhood continued to have ODD in adulthood regardless of comorbid CD, and adults with ODD were also at risk for more compromised outcomes.
Our findings need to be considered in light of some methodological limitations. Because our sample was referred, results may not generalize to girls with ADHD in the general population. Referred cases have been described as having potentially differing clinical characteristics (e.g., chronic course, high comorbidity) from cases in the population.36 However, our results are likely to generalize to girls with ADHD seen in pediatric and psychiatric settings. Likewise, since our sample was largely Caucasian, results may not generalize to other minority groups.
The wide age range of subjects covered a broad developmental spectrum. Samples with narrower age ranges followed over time may be more suited to studying developmental trajectories in childhood and adolescence. The rates of disorders reported here might differ from other studies that use subjects at different developmental stages. Although younger subjects were more likely to have ADHD (p=0.02) and ODD (p=0.003) at follow-up, and older subjects were more likely to have PSUD and smoking at follow-up (both p<0.001), our comparisons are valid because the groups did not significantly differ by age.
We did not conduct direct comparisons of our boys' and girls' samples because the boys' sample was several years older and therefore we would be unable to disentangle age and gender effects. The statements above comparing the boys' and girls' results should be viewed cautiously until direct statistical comparisons can determine gender differences using future follow-up assessments of these samples.
While our results show a significant association between ODD and subsequent morbidity, we cannot rule out the possibility that other correlates of ODD (e.g., poor family functioning) are the primary cause of subsequent morbidity (e.g., depression). Future studies that examine multiple risk factors in addition to disruptive behavior disorders may shed light on such hypotheses.
Despite these limitations, this systematic investigation of the longitudinal course of ODD in girls with ADHD documents that this comorbidity is associated with significant additional morbidity and disability than that associated with ADHD alone, even in the absence of CD. More definitive conclusions await subsequent research with larger samples of ADHD and ODD in the absence of CD followed for a more extended period of time.
ACKNOWLEDGEMENTS
This work was supported, in part, by a grant from USPHS (National Institute of Child Health and Human Development), 5R01 HD-36317-07 (JB).
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Anderson JC, Williams S, McGee R, et al. DSM-III disorders in preadolescent children: Prevalence in a large sample from the general population. Archives of General Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- 2.Bird HR, Canino G, Rubio-Stipec M, et al. Estimates of the prevalence of childhood maladjustment in a community survey in Puerto Rico: The use of combined measures. Archives of General Psychiatry. 1988;45:1120–1126. doi: 10.1001/archpsyc.1988.01800360068010. [DOI] [PubMed] [Google Scholar]
- 3.Biederman J, Monuteaux M, Mick E, et al. Young Adult Outcome of Attention Deficit Hyperactivity Disorder: A Controlled 10 year Prospective Follow-Up Study. Psychological Medicine. 2006;36(2):167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 4.Kadesjo C, Hagglof B, Kadesjo B, et al. Attention-deficit-hyperactivity disorder with and without oppositional defiant disorder in 3- to 7-year-old children. Dev Med Child Neurol. 2003 Oct;45(10):693–699. doi: 10.1017/s0012162203001282. [DOI] [PubMed] [Google Scholar]
- 5.Biederman J, Faraone SV, Mick E, et al. Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(8):966–975. doi: 10.1097/00004583-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Monuteaux M, Mick E, et al. Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled, five-year prospective study. Biological Psychiatry. 2006;60(10):1098–1105. doi: 10.1016/j.biopsych.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 7.Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive, and social functioning, and parenting practices. J Consult Clin Psych. 2002;70(5):1086–1098. doi: 10.1037//0022-006x.70.5.1086. [DOI] [PubMed] [Google Scholar]
- 8.Greene RW, Biederman J, Zerwas S, et al. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am J Psychiatry. 2002;159(7):1214–1224. doi: 10.1176/appi.ajp.159.7.1214. [DOI] [PubMed] [Google Scholar]
- 9.Biederman J, Faraone SV, Milberger S, et al. Is childhood oppositional defiant disorder a precursor to adolescent conduct disorder? Findings from a four-year follow-up study of children with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(9):1193–1204. doi: 10.1097/00004583-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Molina B, Pelham W. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112(3):497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- 11.August GJ, Winters KC, Realmuto GM, et al. Prospective study of adolescent drug use among community samples of ADHD and non-ADHD participants. J Am Acad Child Adolesc Psychiatry. 2006 Jul;45(7):824–832. doi: 10.1097/01.chi.0000219831.16226.f8. [DOI] [PubMed] [Google Scholar]
- 12.Farrington DP, Loeber R, Van Kammen WB. Long-term criminal outcomes of hyperactivity-impulsivity-attention deficit and conduct problems in childhood. In: Robins LN, Rutter MR, editors. Straight and devious pathways to adulthood. Cambridge University Press; New York: 1989. pp. 62–81. [Google Scholar]
- 13.Loney J, Kramer J, Milich RS. The hyperactive child grows up: predictors of symptoms, delinquency and achievement at follow-up. In: Gadow KD, Loney J, editors. Psychosocial Aspects of Drug Treatment for Hyperactivity. Westview Press; Boulder, CO: 1981. pp. 381–416. [Google Scholar]
- 14.Faraone SV, Tsuang MT. Methods in Psychiatric Genetics. In: Tohen M, Tsuang MT, Zahner GEP, editors. Textbook in Psychiatric Epidemiology. John Wiley; New York, NY: 1995. pp. 81–134. [Google Scholar]
- 15.Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. 5th Edition ed. Nova Southeastern University, Center for Psychological Studies; Ft. Lauderdale: 1994. [Google Scholar]
- 16.First M, Spitzer R, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders. American Psychiatric Press; Washington, D.C.: 1997. [Google Scholar]
- 17.Gershon ES, Hamovit J, Guroff JJ, et al. A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands. Archives of General Psychiatry. 1982;39(10):1157–1167. doi: 10.1001/archpsyc.1982.04290100031006. [DOI] [PubMed] [Google Scholar]
- 18.Weissman MM, Leckman JF, Merikangas KR, et al. Depression and anxiety disorders in parents and children: Results from the Yale Family Study. Archives of General Psychiatry. 1984;41:845–852. doi: 10.1001/archpsyc.1984.01790200027004. [DOI] [PubMed] [Google Scholar]
- 19.Mennin D, Biederman J, Mick E, et al. Towards defining a meaningful anxiety phenotpye for research in ADHD children. Journal of Attention Disorders. 2000;3(4):192–199. [Google Scholar]
- 20.Hollingshead AB. Four Factor Index of Social Status. Yale Press; New Haven: 1975. [Google Scholar]
- 21.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and the 1991 Profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- 22.Hinshaw SP, Owens EB, Sami N, et al. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006 Jun;74(3):489–499. doi: 10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- 23.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006 Nov 1;60(9):991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 24.Taylor E, Chadwick O, Heptinstall E, et al. Hyperactivity and conduct problems as risk factors for adolescent development. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(9):1213–1226. doi: 10.1097/00004583-199609000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Mannuzza S, Klein RG, Abikoff H, et al. Significance of childhood conduct problems to later development of conduct disorder among children with ADHD: a prospective follow-up study. J Abnorm Child Psychol. 2004 Oct;32(5):565–573. doi: 10.1023/b:jacp.0000037784.80885.1a. [DOI] [PubMed] [Google Scholar]
- 26.Lahey BB, Loeber R, Burke JD, et al. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. J Consult Clin Psychol. 2005 Jun;73(3):389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- 27.Loeber R, Green S, Keenan K, et al. Which boys will fare worse? Early predictors of the onset of conduct disorder in a six-year longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(4):499–509. [PubMed] [Google Scholar]
- 28.Wozniak J, Spencer T, Biederman J, et al. The clinical characteristics of unipolar versus bipolar major depression in ADHD youth. Journal of Affective Disorders. 2004;82(Suppl 1):S59–S69. doi: 10.1016/j.jad.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood onset bipolar disorder in clinically referred children. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(7):867–876. doi: 10.1097/00004583-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Biederman J, Petty CR, Dolan C, et al. The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychol Med. 2008 Jan 21;:1–10. doi: 10.1017/S0033291707002668. [DOI] [PubMed] [Google Scholar]
- 31.Biederman J, Monuteaux M, Mick E, et al. Is Cigarette Smoking a Gateway Drug to Subsequent Alcohol and Illicit Drug Use Disorders? A Controlled Study of Youths with and without ADHD. Biological Psychiatry. 2006;59(3):258–264. doi: 10.1016/j.biopsych.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 32.Biederman J, Ball SW, Monuteaux MC, et al. CBCL CLINICAL SCALES DISCRIMINATE ADHD YOUTH WITH STRUCTURED-INTERVIEW DERIVED DIAGNOSIS OF OPPOSITIONAL DEFIANT DISORDER (ODD) Journal of Attention Disorders. 2007 doi: 10.1177/1087054707299404. [DOI] [PubMed] [Google Scholar]
- 33.Biederman J, Monuteaux M, Kendrick E, et al. The CBCL as a screen for psychiatric comorbidity in paediatric patients with ADHD. Archives of Disease in Childhood. 2005;90(10):1010–1015. doi: 10.1136/adc.2004.056937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Biederman J, Faraone SV, Doyle AE, et al. Convergence of the Child Behavior Checklist with structured interview- based psychiatric diagnoses of ADHD children with and without comorbidity. Journal of Child Psychology and Psychiatry. 1993;34(7):1241–1251. doi: 10.1111/j.1469-7610.1993.tb01785.x. [DOI] [PubMed] [Google Scholar]
- 35.Harpold T, Biederman J, Gignac M, et al. Is oppositional defiant disorder a meaningful diagnosis in adults? Results from a large sample of adults with ADHD. J Nerv Ment Dis. 2007 Jul;195(7):601–605. doi: 10.1097/NMD.0b013e318093f448. [DOI] [PubMed] [Google Scholar]
- 36.Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics Bulletin. 1946;2:47–53. [PubMed] [Google Scholar]