Abstract
The acute hemodynamic efficacy of an implantable counter-pulsation device (CPD) was evaluated. The CPD is a valveless single port, 32-ml stroke volume blood chamber designed to be connected to the human axillary artery using a simple surface surgical procedure. Blood is drawn into the pump during systole and ejected during diastole. The acute hemodynamic effects of the 32-ml CPD were compared to a standard clinical 40-ml intra-aortic balloon pump (IABP) in calves (80 kg, n = 10). The calves were treated by a single oral dose of Monensin to produce a model of diminished cardiac function (DCF). The CPD and IABP produced similar increases in cardiac output (6% CPD vs. 5% IABP, p > 0.5) and reduction in left ventricular external work (14% CPD vs. 13% IABP, p > 0.5) compared to DCF (p < 0.05). However, the ratio of diastolic coronary artery flow to left ventricular external work increase from DCF baseline (p < 0.05) was greater with the CPD compared to the IABP (15% vs. 4%, p < 0.05). The CPD also produced a greater reduction in left ventricular myocardial oxygen consumption from DCF baseline (p < 0.05) compared to the IABP (13% vs. 9%, p < 0.05) despite each device providing similar improvements in cardiac output. There was no early indication of hemolysis, thrombus formation, or vascular injury. The CPD provides hemodynamic efficacy equivalent to an IABP and may become a therapeutic option for patients who may benefit from prolonged counterpulsation.
The intra-aortic balloon pump (IABP) is the most widely used short-term cardiac assist device with over 160,000 balloons implanted each year world-wide. There is also clinical evidence to suggest that counterpulsation therapy can be effective in patients with chronic congestive heart failure (CHF). The IABP has been shown to be effective in patients with poor left ventricular function undergoing coronary artery bypass surgery.1 However, the location of an IABP catheter (thoracic aorta) and biocompatibility issues limit the application of IABP therapy to short durations of hours to <14 days. When IABP support is employed for prolonged periods of more than 20 days, the frequency of vascular complications, infection, and bleeding is high.2,3 Furthermore, the IABP immobilizes the patient.
It is not surprising that a number of companies are now developing chronic heart assist devices to permit patients to be treated with long-term counterpulsation therapy that avoids catheter placement in the groin and allows patients to be mobile [left ventricular assist devices (LVAD) Technologies (CardioPlus4,5), Sunshine Heart (C-Pulse6), Cardiak (akpulsor), and SCR7,8]. These devices are being developed to offer the advantages of long-term counterpulsation with an implant procedure that is less invasive than current LVAD.
SCR Counterpulsation Device Therapy
A simple counterpulsation device (CPD) that can be implanted and explanted with a minimally invasive surface procedure is currently under development (SCR, Louisville, KY). The core component of the SCR device is a 32-ml stroke volume polyurethane-lined blood chamber, (Figure 1) designed to fit comfortably in a subcutaneous pocket, (7 cm × 7 cm × 5 cm) on the right anterior chest contralateral to an implantable cardioverter defibrillator (ICD) device implantation site. The pumping chamber is connected to the systemic circulation by a short ePTFE graft anastomosed to the right axillary artery. A percutaneous drive line runs from the chamber to an external pneumatic driver. During systole, the drive console evacuates air from the chamber thus removing blood from the arterial circulation reducing cardiac work and after-load. During diastole, the console ejects blood from the chamber into the circulation providing diastolic augmentation and improving coronary perfusion. The chamber and graft have been specifically developed for continuous washing and nominal shear stress. The shape of the CPD chamber is designed to wash continuously by creating a constant but shifting circular vortex of blood to minimize risk of blood stasis and thrombosis. The CPD graft connects seamlessly to the chamber without an inlet or outlet valve, also reducing the risk of thrombus formation. The bi-directional flow enhances washing inside the graft compared to unidirectional cannulae used in other blood pumps. The CPD graft is also supported with reinforcement rings and the distance between the chamber and axillary artery is minimized to reduce the risk of graft kinking.
Figure 1.
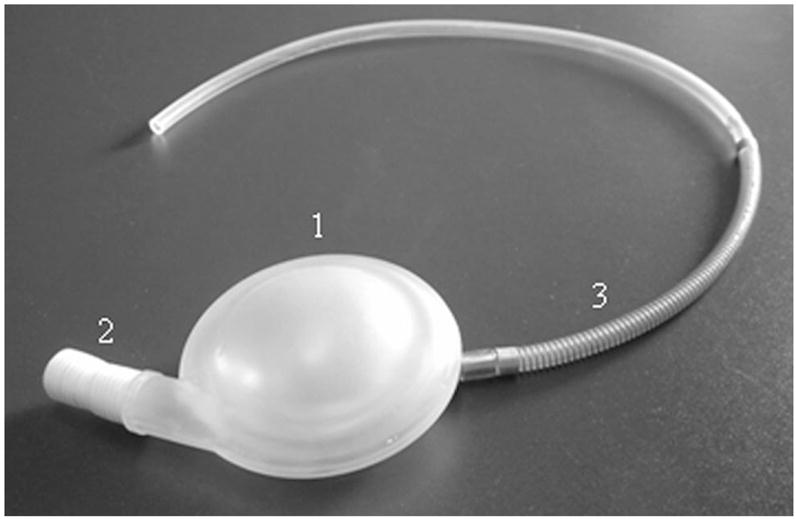
Photograph of implantable components of the SCR counterpulsation device (CPD) system: 1) chamber, 2) connector, and 3) pneumatic driveline.
Methods
All animals received humane care in accordance with the Guide for Care and Use of Laboratory Animals (NIH publication 86–23, revised 1996) and the guidelines determined by the Institutional Animal Care and Use Committee of the University of Louisville.
Experimental Design
The acute hemodynamic efficacy of a 32-ml CPD chamber (SCR, Louisville, KY) and a standard commercially-available 40-ml IABP (Datascope, Fairfield, NJ) were investigated in a large animal model (n = 10) of diminished cardiac function (DCF) created with a toxin (Monensin). The CPD device was connected to the carotid artery (6–8 mm diameter) with a 10 mm ePTFE graft and the IABP was placed in the descending thoracic aorta. The carotid artery diameter of the calf and distance from CPD to aorta are equivalent in size of human axillary artery and distance to aorta. Pressure, flow, and volume waveforms were recorded and myocardial oxygen consumption was calculated during 1) baseline (device off), 2) 1:1 support, and 3) 1:2 support for the 32-ml CPD and 40-ml IABP in the same animal. Baseline measurements were repeated between test conditions to ensure DCF baseline values were maintained at a comparable steady state. Baselines and support modes for each device were maintained for 15 minutes each to ensure a steady-state was reached while minimizing risk of deterioration of the animal preparation. Data were collected for 30 seconds at the end of each steady-state test condition. The test order of devices (IABP and CPD) and support modes (1:1 and 1:2) were randomized to eliminate experimental order bias. Cardiovascular parameters were derived and left ventricular pressure-volume (PV) loops constructed from recorded waveforms to assess the hemodynamic efficacy of each device as defined by changes in left ventricular workload, coronary perfusion, and myocardial oxygen consumption. A blood sample was drawn for all test conditions to determine plasma free hemoglobin (PFHb) as an early indication of device associated hemolysis.
Surgical Procedures (DCF Model)
Ten healthy Jersey calves (male, 80–90 kg) were used in this study. After initial physical examination and a 5–7 day quarantine period, animals were preanesthetized with Atropine (30 mg) and then anesthetized with isoflurane (3%–5%) via nose cone. After intubation, anesthesia was maintained with isoflurane (1%–3%) mixed with oxygen and room air. The left lateral chest was prepared for sterile surgery. A thoracotomy was performed over the 3rd and 4th ribs. Catheters (Millar Instruments, Houston, TX) were temporarily placed in the left atrium (5F single-tip model MPR-500) and across aortic valve (6F dual-tip conductance model SPR-562) for simultaneous measurement of aortic pressure and left ventricular pressure and volume. A flow probe (Transonics, Ithaca, NY) was temporarily placed around the pulmonary artery. Pressure and flow waveforms were recorded to assess normal baseline cardiac parameters. The catheters and flow probe were then removed. Fluid-filled arterial and venous pressure lines were implanted in the left carotid artery and jugular vein to monitor cardiac function during the recovery period. The baseline cardiac output in these animals is approximately 10 L/min. In order to reduce cardiac output for testing clinically sized devices, a cardiotoxin was administered. After a 1-week recovery period, calves were given a single oral dose of Rumensin 80 equivalent to 20 mg/kg (containing 80 mg/lb of Monensin: Elanco, Indianapolis, IN) via orogastric tube to create the DCF model. Monensin is a common cattle herd diet additive that has been shown to be a cardiotoxic producing extensive diffuse cardiomyocyte death in calves when used at these doses. Previous investigations have shown that this model can reduce cardiac output by 15%–25%, increase left atrial pressure by 67%, and increase left ventricular end-diastolic pressure by 143% in calves.9 Higher doses of Monesin produce greater reduction in cardiac output, but at the risk of an unstable model and high mortality.
Surgical Procedures (Acute Efficacy Study)
Three weeks after administering the Monensin dose, the nonsurvival acute hemodynamic study was initiated. Anesthesia, surgery (thoracotomy), and instrumentation procedures were repeated as described above with the addition of a flow probe placed around the left main coronary artery. Blood sampling catheters were placed in the aorta via the femoral artery and in the coronary sinus via the hemiazygous vein. A 10-mm ePTFE vascular graft (Atrium, Hudson, NH) was anastomosed to the right carotid artery and attached to the 32-ml CPD. A 40-ml IABP catheter (Datascope, Fairfield, NJ) was inserted into the descending thoracic aorta immediately downstream to the aortic arch vessels. The 32-ml CPD and 40-ml IABP were triggered from a surface ECG and the timing was adjusted using the aortic pressure trace. IABP timing was adjusted to inflate the balloon at the dicrotic notch and deflate the balloon immediately before ventricular systole to maximize the reduction of aortic end-diastolic pressure. CPD timing was adjusted to fill during left ventricular ejection and eject immediately after the dicrotic notch. The CPD filling occurs over a longer time period to prevent suction of the carotid artery that can occur from filling the CPD chamber too quickly. Animals were anticoagulated with heparin (3 mg/kg i.v.) and ACT was maintained above 200 seconds. Blood was sampled every 30 minutes to check ACT. Central venous pressure (CVP) was measured with a fluid-filled pressure line and monitored for observation by our anesthesia technician and surgeon throughout each experiment. The surgical team carefully monitored CVP to ensure it was maintained at approximately10–12 mm Hg for each baseline pre-, post-, and in-between IABP and CPD test conditions.
Instrumentation and Data Reduction
All transducers were pre- and postcalibrated against known physical standards to ensure measurement accuracy. Hemodynamic data were signal conditioned and A/D converted for digital analysis using a Good Laboratory Practices (GLP) compliant data acquisition system.10,11 Signal conditioning was accomplished using transducer amplifiers (Ectron, San Diego, CA), transit-time flowmeter (Transonics, Ithaca, NY), and a volume conductance unit (Leycom, Sigma V, Netherlands). These data were low-pass filtered at 60 Hz, analog-to-digitally converted (AT-MIO-16E-10 and LabVIEW, National Instruments) at a sampling rate of 400 Hz, and stored on a personal computer for postprocessing and analysis.
The measured pressure and flow waveform recordings were used to calculate heart rate, stroke volume, cardiac output, CPD stroke volume, mean aortic and mean aortic diastolic pressures, left ventricular peak systolic and end-diastolic pressures, mean left atrial pressure, mean diastolic coronary artery flow, mean coronary artery flow, and left ventricular external work. These parameters were calculated on a beat-to-beat basis, for each 30 second data set, using a Hemodynamic Evaluation and Assessment Research Tool (HEART) program12 developed in Matlab (MathWorks, Natick, MA). All analyzed beats in each data set (approximately 40–50 beats) were averaged to obtain a single representative mean value for each calculated parameter. Left ventricular PV loops were constructed by plotting left ventricular pressure against left ventricular volume with each loop representing one complete cardiac cycle. These PV loops were used to calculate left ventricular external work and evaluate changes in left ventricular end-diastolic and end-systolic pressures and volumes. Statistical analyses were conducted using t test for paired samples and assuming equal variances. Statistical analysis was performed to test for changes in the cardiac parameters between the normal and the DCF state. Statistical analysis was also performed to test for efficacy of the devices compared to the DCF state and to compare devices.
Left Ventricular Myocardial Oxygen Consumption
Paired blood samples were drawn from the aorta and coronary sinus to determine the oxygen content of the blood entering and exiting the left ventricular myocardium at the end of each 15-minute test condition while left main coronary artery blood flow (CAF, ml/min) was recorded. The blood samples were processed through a blood gas analyzer (IRMASL Blood Analysis System, Diametics Medical, Inc., St. Paul, MN) to measure the % saturation of hemoglobin with oxygen (%O2 Sat) and hemoglobin content [(Hb)gm/dl]. The oxygen content (O2) was then calculated for each blood sample by,
The left ventricular myocardial oxygen consumption (LV O2 cons.) was calculated as,
[O2]a = arterial oxygen content, [O2]cs = coronary sinus oxygen content, and LV mass [g] = weight of LV at necropsy.
Blood Hemoglobin and Necropsy
Venous blood samples were drawn to measure Total Hemoglobin (Tot Hb) and Plasma Free Hemoglobin (PFHb) for each experimental test condition and device trial. At the completion of the experiment, the CPD chamber and cannula were removed and visually inspected for gross evidence of thrombus, fractures, and other defects. Peripheral organs were removed and examined for gross evidence of thrombus related infarcts.
Results
Monensin-Induced DCF Animal Model
The oral dose of Monensin resulted in a 17% reduction in cardiac output (reduced from 10.3 to 8.5 L/min), a 9% reduction in left ventricular peak systolic pressure, an 11% reduction in mean arterial pressure, a 120% increase in left atrial pressure, and a 133% increase in left ventricular end diastolic pressure compared to normal baseline (Table 1).
Table 1.
The DCF Model Produced a Significant Reduction in Cardiac Output (CO) While Left Atrial Pressure (LAP) More Than Double
| HR (bpm) | SV (ml) | CO (L/min) | LVPpksys (mm Hg) | MAP (mm Hg) | LAP (mm Hg) | LVPed (mm Hg) | |
|---|---|---|---|---|---|---|---|
| Normal | 90 ± 5 | 118 ± 10 | 10.3 ± 0.5 | 116 ± 3 | 91 ± 4 | 5 ± 2 | 6 ± 2 |
| DCF | 77 ± 3* | 110 ± 7 | 8.5 ± 0.6* | 106 ± 3* | 81 ± 3* | 11 ± 2* | 14 ± 3* |
Values are given as mean ± SD.
Normal vs. DCF (p < 0.05).
HR, heart rate; SV, stroke volume; LVPpksys, left ventricular peak systolic pressure; MAP, mean aortic pressure; LAP, left atrial pressure; LVPed, left ventricular end diastolic pressure at normal (before oral dose of Monensin); DCF, diminished cardiac function.
Acute Efficacy Study
Example aortic pressure traces for unassisted support (baseline) and 40-ml IABP (top) and 32-ml CPD (bottom) in 1:1 assist mode are shown side-by-side in Figure 2. As indicated by the arrows, the peak systolic aortic pressures were reduced by a similar amount with both devices. Example aortic pressure traces for the CPD (dotted line) and IABP (solid line) are also shown overlaid in Figure 3. As indicated by the arrows, the IABP lowered end diastolic pressure more than the CPD.
Figure 2.
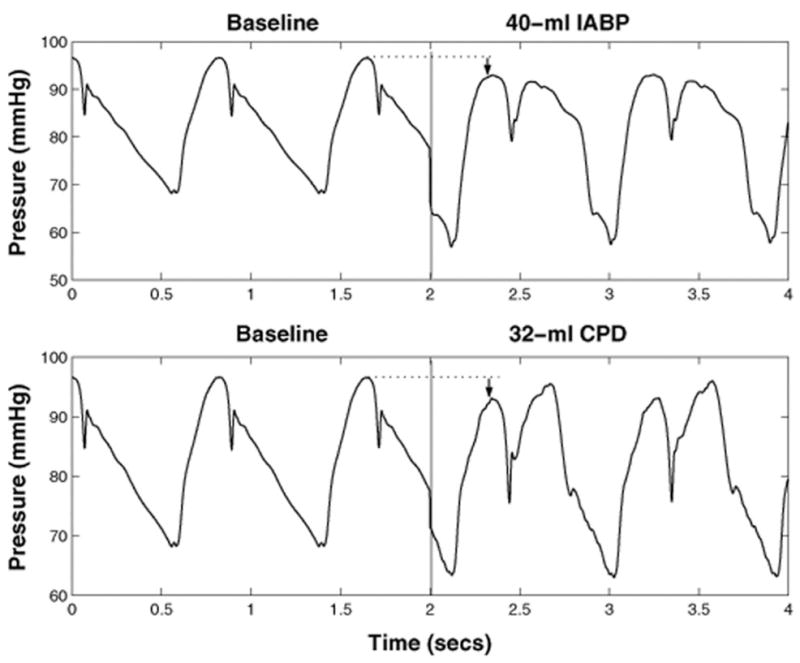
Example aortic pressure traces for unassisted support (baseline) and 40-ml IABP (top) and 32-ml CPD (bottom) in 1:1 assist mode. As indicated by the arrows, the peak systolic aortic pressures were reduced by a similar amount with both devices.
Figure 3.
Example aortic pressure traces for 40-ml IABP (solid) and 32-ml CPD (dotted) in 1:1 assist mode. As indicated by the arrows, the 40-ml IABP resulted in a lower end diastolic pressure than the CPD.
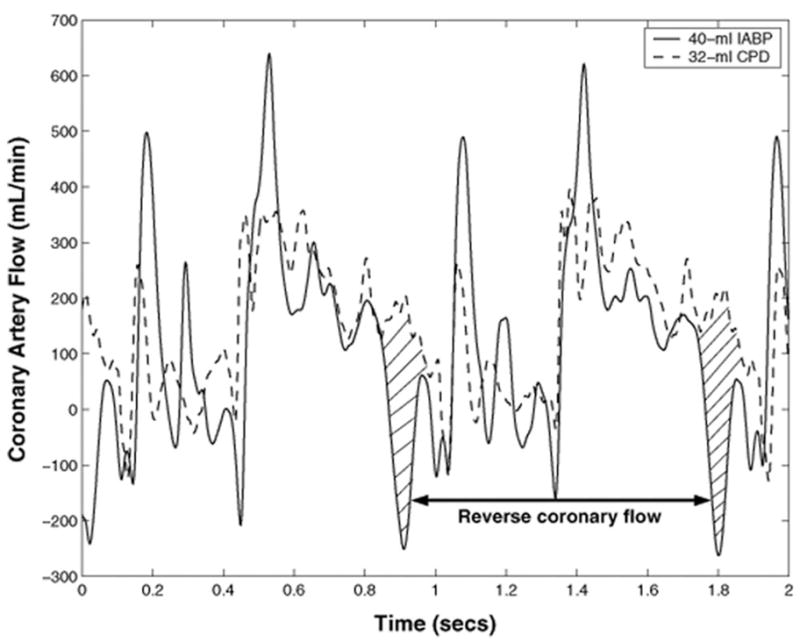
Statistically significant (p < 0.05) hemodynamic improvements were observed with both the 32-ml CPD and 40-ml IABP compared to DCF baseline values (Table 2). The CPD and IABP increased cardiac output by 6%. The mean diastolic coronary artery flow was augmented by 14% with the CPD and 7% with the IABP. Left ventricular peak systolic pressure was reduced by 7% with the CPD and 6% with the IABP. There were no statistically significant differences between the 32-ml CPD and 40-ml IABP (p > 0.5), except for the aortic end-diastolic pressure, for which the IABP produced a greater reduction (p < 0.05).
Table 2.
The 32-ml CPD and 40-ml IABP Both Produced a Significant Hemodynamic Improvement Compared to DCF Baseline
| Device | Mode | HR (bpm) | SV (ml) | CO (L/min) | LVPpksys (mm Hg) | CAFdia (ml/min) | MAP (mm Hg) | AoPed (mm Hg) |
|---|---|---|---|---|---|---|---|---|
| DCF baseline | 77 ±3 | 110 ±7 | 8.5 ±0.6 | 106 ±3 | 279 ±51 | 81 ±3 | 74 ±5 | |
| 32-ml CPD | 1:1 | 79 ±4 | 113 ±9 | 9.0 ±0.9* | 99 ±3* | 317 ±52* | 86 ±4* | 68 ±3* |
| 1:2 | 79 ±4 | 113 ±8 | 9.3 ±0.6* | 100 ±3* | 297 ±49* | 85 ±3* | 68 ±3* | |
| 40-ml IABP | 1:1 | 79 ±3 | 113 ±7 | 9.0 ±0.5* | 96 ±3* | 297 ±70* | 85 ±3* | 60 ±3*† |
| 1:2 | 80 ±4 | 111 ±4 | 8.9 ±0.6* | 95 ±2* | 294 ±64* | 81 ±3* | 60 ±3*† |
Values are given as mean [±] SD.
Vs. DCF baseline (p < 0.05).
IABP vs. CPD (p < 0.05).
HR, heart rate; SV, stroke volume; CO, cardiac output; LVPpksys, left ventricular peak systolic pressure; CAFdia, mean diastolic coronary artery flow; MAP, mean aortic pressure; AoPed, aortic end-diastolic pressure at DCF, diminished cardiac function baseline, 1:1 and 1:2 modes.
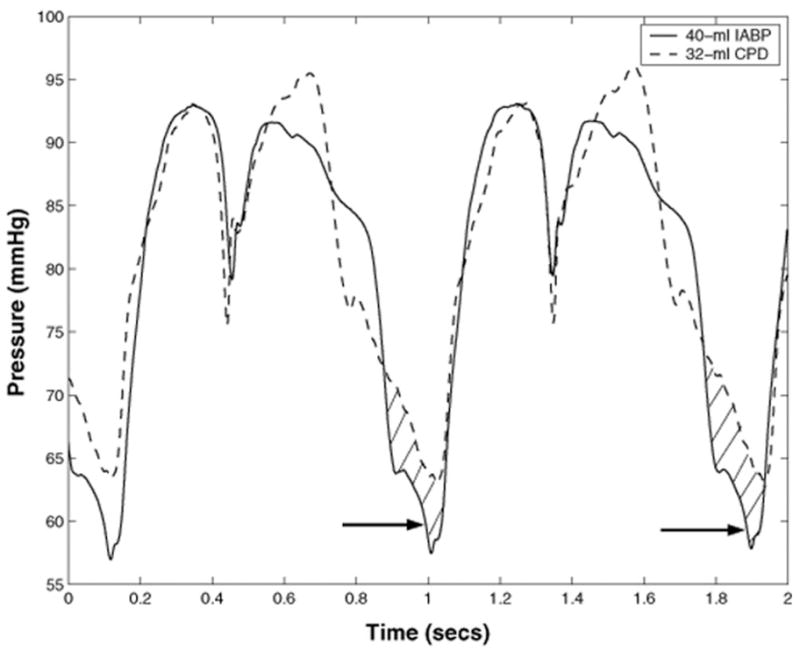
Superimposed coronary flow waveforms for the IABP (solid line) and the CPD (dotted line) are shown in Figure 4. Coronary flow was reversed prior to systole with the IABP (shaded area), but did not occur with the CPD. Thus, the CPD provided a significantly higher augmentation in coronary flow than the IABP (14% increase with CPD vs. 7% increase with IABP).
Figure 4.
Example coronary flow waveform traces for 40-ml IABP (solid) and 32-ml CPD (dotted) in 1:1 assist mode. Coronary flow was reversed prior to systole with the IABP (shaded area) but coronary flow reversal did not occur with the CPD.
A sample left ventricular pressure volume (PV) loop is shown in Figure 5. The 40-ml IABP and 32-ml CPD both reduced left ventricular volume and systolic pressures from DCF baseline as evidenced by the leftward and downward shifts in the PV loops. The left ventricular external work (equivalent to the area inside the PV loop) was reduced by both the 32-ml CPD (14%) and the 40-ml IABP (13%) compared to DCF baseline (Figure 6).
Figure 5.
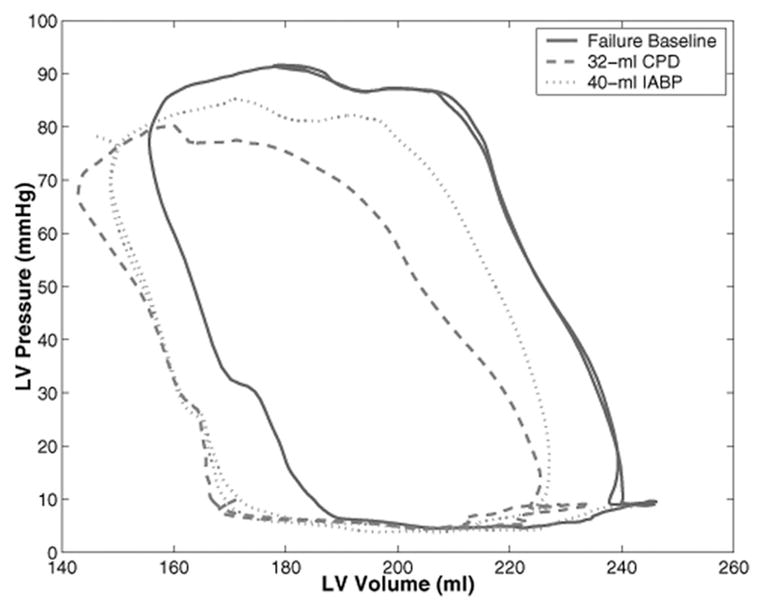
A sample left ventricular (LV) pressure volume (PV) loop. The 40-ml IABP and 32-ml CPD both reduced left ventricular volume and systolic pressures from DCF baseline as evidenced by the leftward and downward shifts in the PV loops.
Figure 6.
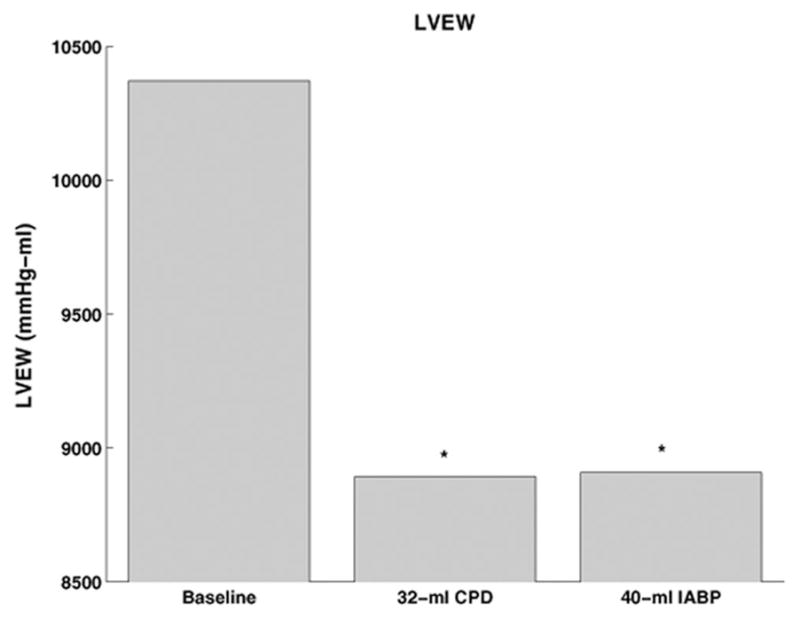
The left ventricular external work (LVEW) was reduced by both the 32-ml CPD and 40-ml IABP. [*Vs. DCF baseline (p < 0.05)].
The myocardial perfusion to work balance was also considerably better with the 32-ml CPD as evidenced by the significantly increased diastolic coronary artery flow to left ventricular external work ratio (increased 15% by CPD vs. 4% IABP), as shown in Figure 7. In addition, the 32-ml CPD resulted in a greater reduction in the left ventricular myocardial oxygen consumption (decreased 13% by CPD vs. 9% IABP) despite the fact that both devices provided similar improvements in cardiac output.
Figure 7.
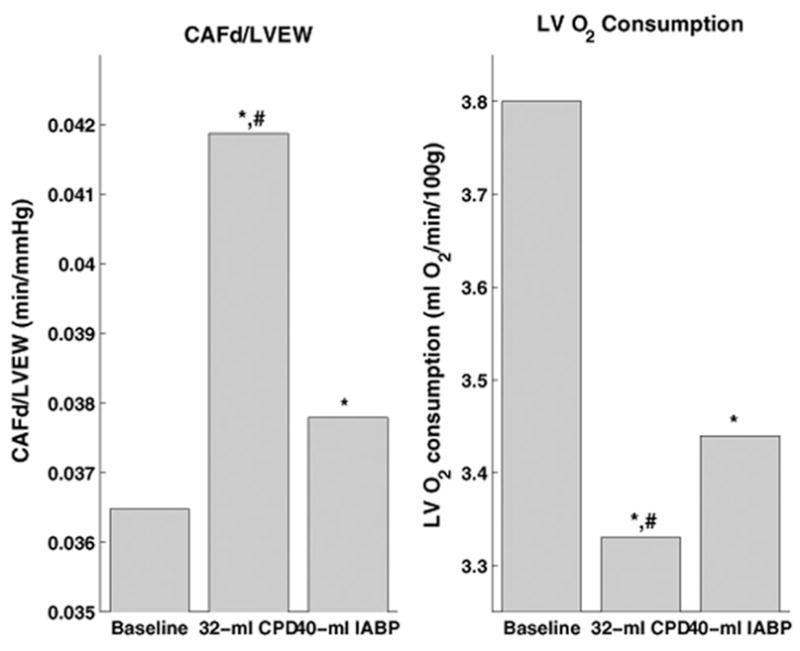
The 32-ml CPD provided a greater increase in mean diastolic coronary artery flow (CAFd) per unit left ventricular external work (LVEW) and greater reduction in left ventricular myocardial oxygen consumption (LV O2). These data demonstrate the 32-ml CPD delivers more myocardial perfusion (supply) while also reducing cardiac work (demand). [*vs. DCF baseline (p < 0.05) and #CPD Vs. IABP (p < 0.05)].
Blood Hemoglobin and Necropsy
Plasma free hemoglobin levels remained below 8 mg/dl at all measured time points. A necropsy was performed at the end of each animal study and included examination of all major abdominal and thoracic organs, and the brain. There were no signs of damage or thromboembolism in any organ. The CPD was examined carefully for signs of thrombus. The CPD chamber was entirely clear of thrombi for all experiments.
Discussion
Congestive heart failure, one of the largest unsolved problems in cardiac care today, affects more that five million patients in the United States alone. Despite pharmacological therapy, many patients deteriorate to the point where mechanical circulatory support would be clinically beneficial. Unfortunately, despite many years of research and millions of dollars of expenditure, only about 3,000 patients receive chronic mechanical circulatory support each year. Most current mechanical circulatory support requires invasive sternotomy and cannulation of the heart and aorta. Complications are frequent and include device failure, thromboembolism, stroke, infection, and bleeding. The level of invasiveness of the surgery required for implantation, the difficulty in the management of the patients, and the frequency of complications contribute to the low number of patients receiving mechanical heart assist devices.
Globally, the most common assist device for heart failure is the IABP, which is used clinically for limited time periods of several hours to several days. Each year more than 160,000 patients worldwide receive IABP therapy, often for cardiogenic shock or severe left ventricular dysfunction following acute myocardial infarction or cardiotomy.13,14 Many thousands of lives are saved each year due to IABP therapy (65% survival).15 Intra-aortic balloon pump support is simpler than current LVAD therapies and clinicians have developed a great deal of confidence in the therapeutic effectiveness of intra-aortic balloon counterpulsation. The IABP requires no direct cannulation of the heart leading to easier implantation and explantation. Furthermore, control algorithms to fill and empty the balloon are considerably less complex than to control an LVAD and simplify patient management. Short-term counterpulsation therapy, although unquestionably less powerful than LVAD therapy, does offer considerable practical clinical advantages. With over 30 years of use, clinicians trust counterpulsation therapy in their sickest patients.
Counterpulsation therapy is achieved by rapidly inflating the IABP immediately after aortic valve closure (dicrotic notch) and rapidly deflating the balloon just before the onset of systole. The rapid inflation of the balloon increases the aortic diastolic pressure by 30%–70% improving end-organ perfusion and coronary perfusion.13,14 The rapid deflation of the IABP reduces the ejection pressure of the native ventricle, reducing after load and left ventricular external work.13,16,17 The peak systolic pressure is reduced by up to 15%,13,17 whereas the end diastolic pressure is decreased by up to 30%.1,17 Cardiac output and stroke volume have been found to increase by up to 20%,16,18 while no changes have been observed.14,16,18 Intra-aortic balloon pump therapy also decreases the heart rate by 10%14 and may reduce the left ventricular end diastolic volume by 10%–15%.19 Intra-aortic balloon pump improves the cardiac energy balance by increasing the oxygen supply to the myocardium through increased coronary perfusion of 0%–100%20,21 and by reducing myocardial oxygen consumption through a decrease in after-load and left ventricular external work.14 Intra-aortic balloon pump also has been reported to augment cerebral, renal, mesenteric, and pulmonary blood flows.22–24 Further, increases in urine output and lactate use, decrease in lactic acidosis and enhancement of venous oxygen saturation have also been observed in patients supported with IABP.14
Counterpulsation can also be performed with a blood chamber connected directly to the aorta. Nanas et al. showed that a 30-ml blood chamber was more effective in reducing aortic systolic and end-diastolic pressures and myocardial oxygen consumption while increasing coronary flow when directly compared to a 40-ml IABP.5 In our laboratory, computer simulation and feasibility experiments have suggested that a 32-ml blood chamber connected to the axillary artery can be as effective as a 40-ml IABP in the descending aorta.7,8 The results of this study demonstrate that the 32-ml CPD anastamosed to a peripheral vessel (carotid artery) produced hemodynamic efficacy equivalent to a standard clinical 40-ml IABP. Importantly, in this study, the 32-ml CPD provided greater diastolic myocardial perfusion per unit work (supply) with lower myocardial oxygen consumption (demand) compared to the IABP. This study also demonstrated that there were no early indicators of hemolysis, thrombus formation, or vascular injury associated with the 32-ml CPD.
Counterpulsation therapy is most effective when the balloon or blood chamber volumes are comparable to the ventricular stroke volume and when the vasculature is stiffer.25–29 Calves weighing 80 –90 kg were selected for this study because the size of their carotid arteries (6 mm) and the distance from the anastomotic site to the aortic valve (14 cm) approximated the clinical situation that will be encountered with a 32-ml CPD anastomosed to the axillary artery (8 mm diameter and 12 cm to the aortic valve). In these acute experiments, a reproducible patent end-to-side anastomosis was achieved with a 10 mm graft. Calves have higher cardiac outputs and stroke volumes (even with cardiac dysfunction produced by the DCF model) and higher arterial compliance than humans. Therefore, the improvement in cardiac performance was less pronounced in this study than would be expected in the clinical application of counterpulsation. Importantly, despite the limitations of the calf model, the improvements in cardiac function produced by the 32-ml CPD were equivalent to those produced by the 40-ml IABP.
There are important distinctions in the method of delivery and timing of counterpulsation therapy between the IABP and the CPD. The IABP displaces blood volume within the aorta while the CPD chamber shuttles blood in and out of the aorta. The ejection and filling phases of the CPD are longer than the balloon inflation and deflation time periods of the IABP. The faster balloon deflation is necessary to prevent the obstruction of the aorta during ventricular systole. However, this rapid deflation, leads to reverse coronary flow (Figure 3). The IABP rapidly inflates and deflates during diastole within the same assisted beat. In contrast, the CPD fills during systole and ejects during diastole. In this study, these differences in timing resulted in a lower aortic end diastolic pressure and diastolic coronary flow with the 40-ml IABP compared with the CPD (Figures 3 and 4). Ultimately, the IABP and CPD both produced comparable after load reduction compared to unassisted condition when operating in 1:1 or 1:2 mode. The myocardial perfusion and perfusion to work balance was superior with the CPD compared to the IABP.
Counterpulsation with IABP has not gained widespread acceptance as a long-term therapy to treat heart failure, because of the high risk of complication and lack of patient mobility. There are reports that counterpulsation can have a sustained effect when used for prolonged periods of support.25 Recently, Jeevanandam reported that patients who received an aortic CPD (CardioPlus, LVAD Technologies) demonstrated considerable improvements in exercise capacity.4,5 Unfortunately, implantation of this device required a thoracotomy and resulted in a high level of morbidity and mortality for these patients.
SCR (Louisville, KY) is developing a chronic implantable CPD to treat HF patients who may be responsive to a partial form of cardiac assist. It is intended to be a low cost device that can be implanted and explanted without major surgical trauma or extensive postoperative care. The device is implanted by a surface procedure in a pacemaker pocket on the right side and connected to the axillary artery. The size and shape of the SCR device are designed to provide a good anatomical fit in humans while closely matching the expected levels of support needed for effective counterpulsation therapy support in HF patients. Chronic testing of the CPD is on-going. The CPD has successfully supported two calves chronically for 30 days without adverse events or device failures.
Conclusion
This acute study demonstrated that the 32-ml CPD and the 40-ml IABP produced an equivalent and statistically significant improvement in cardiac performance compared to the DCF state. The 32-ml CPD did not cause any acute hemolysis, thrombus formation, or vascular injury.
Acknowledgments
Supported by grants from the National Institutes of Health (NIH) Heart Lung and Blood Institute (HLBI) Small Business Innovative Research (SBIR) program (grant number 1R43HL083586-01) and the Kentucky Science and Engineering Foundation (KSEF) program (grant number KSTC-184-512–07-011).
References
- 1.Cochran RP, Starkey TD, Panos AL, Kunzelman KS. Ambulatory intraaortic balloon pump use as bridge to heart transplant. Ann Thorac Surg. 2002;74:746–751. doi: 10.1016/s0003-4975(02)03808-0. discussion 751–752. [DOI] [PubMed] [Google Scholar]
- 2.Freed PS, Wasfie T, Zado B, et al. Intraaortic balloon pumping for prolonged circulatory support. Am J Cardiol. 1988;61:554–557. doi: 10.1016/0002-9149(88)90763-1. [DOI] [PubMed] [Google Scholar]
- 3.Manord JD, Garrard CL, Mehra MR, et al. Implications for the vascular surgeon with prolonged (3 to 89 days) intraaortic balloon pump counterpulsation. J Vasc Surg. 1997;26:511–516. doi: 10.1016/s0741-5214(97)70044-2. [DOI] [PubMed] [Google Scholar]
- 4.Jeevanandam V, Jayakar D, Anderson AS, et al. Circulatory assistance with a permanent implantable IABP: Initial human experience. Circulation. 2002;24:I183–I188. [PubMed] [Google Scholar]
- 5.Terrovitis JV, Charitos CE, Tsolakis EJ, et al. Superior performance of a paraaortic counterpulsation device compared to the intraaortic balloon pump. World J Surg. 2003;27:1311–1316. doi: 10.1007/s00268-003-6928-5. [DOI] [PubMed] [Google Scholar]
- 6.Legget ME, Peters WS, Milsom FP, et al. Extra-aortic balloon counterpulsation: An intraoperative feasibility study. Circulation. 2005;112:I26–I31. doi: 10.1161/CIRCULATIONAHA.104.521831. [DOI] [PubMed] [Google Scholar]
- 7.Giridharan GA, Koenig SC, Pantalos GM, et al. Predicted hemodynamic benefits of counterpulsation therapy using a superficial surgical approach. ASAIO J. 2006;52:39–46. doi: 10.1097/01.mat.0000196522.29376.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koenig SC, Litwak KN, Pantalos GM, et al. Development and early testing of a simple subcutaneous circulatory support device. ASAIO J. 2006;52:362–367. doi: 10.1097/01.mat.0000227729.70008.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Litwak KN, McMahan A, Lott KA, et al. Monensin toxicosis in the bovine calf: A large animal model of cardiac dysfunction. Comp Med. 2005;44:45–49. [PubMed] [Google Scholar]
- 10.Drew GA, Koenig SC. Biomedical Patient Monitoring, Data Acquisition, and Playback with LabVIEW®. In: Olansen JB, Rosow E, editors. Virtual Bio-Instrumentation: Biomedical, Clinical, and Healthcare Applications in LabVIEW®. Prentice Hall; 2002. pp. 180–186. [Google Scholar]
- 11.Koenig SC, Woolard C, Drew GD, et al. Integrated data acquisition system for medical device testing and physiology research in compliance with good laboratory practices. Biomed Instrum Technol. 2004;38:229–240. doi: 10.2345/0899-8205(2004)38[229:IDASFM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Schroeder MJ, Perrrault B, Ewert DL, Koenig SC. HEART: An automated beat-to-beat cardiovascular analysis package using Matlab™. Comput Biol Med. 2004;34:371–388. doi: 10.1016/S0010-4825(03)00087-8. [DOI] [PubMed] [Google Scholar]
- 13.Nanas JN, Moulopoulos SD. Counterpulsation: Historical background, technical improvements, hemodynamic and metabolic effects. Cardiology. 1994;84:156–167. doi: 10.1159/000176394. [DOI] [PubMed] [Google Scholar]
- 14.Papaioannou GT, Stefanadis C. Basic principles of the intraaortic balloon pump and mechanisms affecting its performance. ASAIO J. 2005;51:296–300. doi: 10.1097/01.mat.0000159381.97773.9b. [DOI] [PubMed] [Google Scholar]
- 15.Torchiana DF, Hirsch G, Buckley MJ, et al. Intraaortic balloon pumping for cardiac support: trends in practice and outcome, 1968 to 1995. J Thor Cardiovasc Surg. 1997;13:758–764. doi: 10.1016/S0022-5223(97)70235-6. [DOI] [PubMed] [Google Scholar]
- 16.Scheidt S, Wilner G, Mueller H, et al. Intra-aortic balloon counterpulsation in cardiogenic shock. Report of a cooperative clinical trial. N Engl J Med. 1973;288:979–984. doi: 10.1056/NEJM197305102881901. [DOI] [PubMed] [Google Scholar]
- 17.Bolooki H, editor. Clinical Application of the Intra-aortic Balloon Pump. 3. New York: Futura; 1998. [Google Scholar]
- 18.Dunkman WB, Leinbach RC, Buckley MJ, et al. Clinical and hemodynamic results of intra-aortic balloon pumping and surgery for cardiogenic shock. Circulation. 1972;46:465–477. doi: 10.1161/01.cir.46.3.465. [DOI] [PubMed] [Google Scholar]
- 19.Weiss AT, Engel S, Gotsman CJ, et al. Regional and global left ventricular function during intra-aortic balloon counterpulsation in patients with acute myocardial infarction shock. Am Heart J. 1984;108:249–254. doi: 10.1016/0002-8703(84)90607-0. [DOI] [PubMed] [Google Scholar]
- 20.Kern MJ, Aguirre FV, Tatineni S, et al. Enhanced coronary blood flow velocity during intra-aortic balloon counterpulsation in critically ill patients. J Am Coll Cardiol. 1993;21:359–368. doi: 10.1016/0735-1097(93)90676-r. [DOI] [PubMed] [Google Scholar]
- 21.Ishihara M, Sato H, Tateishi H, et al. Effects of intraaortic balloon pumping on coronary hemodynamics after coronary angioplasty in patients after an acute myocardial infarction. Am Heart J. 1992;124:1133–1138. doi: 10.1016/0002-8703(92)90391-8. [DOI] [PubMed] [Google Scholar]
- 22.Bhayana JN, Scott SM, Sethi GK, Takaro T. Effects of intra-aortic balloon pumping on organ perfusions in cardiogenic shock. J Surg Res. 1979;26:108–113. doi: 10.1016/0022-4804(79)90086-6. [DOI] [PubMed] [Google Scholar]
- 23.Sugita Y, Emoto H, Morita K, et al. The effect of intraaortic balloon pumping (IABP) on pulmonary circulation. ASAIO Trans. 1985;31:389–394. [PubMed] [Google Scholar]
- 24.Hilberman M, Derby GC, Spencer RJ, Stinson EB. Effect of the intra-aortic balloon pump upon postoperative renal function in man. Crit Care Med. 1981;9:85–89. doi: 10.1097/00003246-198102000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Sun Y. Modeling the dynamic interaction between left ventricle and intra-aortic balloon pump. Am J Physiol. 1991;261:H1300–H311. doi: 10.1152/ajpheart.1991.261.4.H1300. [DOI] [PubMed] [Google Scholar]
- 26.Papaioannou TG, Mathioulakis D, Nanas J, et al. Arterial compliance is a main variable determining the effectiveness of intra-aortic balloon counterpulsation: Quantitative data from an in-vitro study. Med Eng Physics. 2002;24:279–284. doi: 10.1016/s1350-4533(02)00013-9. [DOI] [PubMed] [Google Scholar]
- 27.Lin C-Y, Galysh FT, Ho KJ, Patel AS. Response to single-segment intraaortic balloon pumping as related to aortic compliance. Ann Thorac Surg. 1972;13:468–476. doi: 10.1016/s0003-4975(10)65160-0. [DOI] [PubMed] [Google Scholar]
- 28.Papaioannou TG, Lekakis J, Dagre A, et al. Arterial compliance is an independent factor that predicts acute hemodynamic performance of intra-aortic balloon counterpulsation. Int J Artif Organs. 2001;24:478–483. [PubMed] [Google Scholar]
- 29.Feola M, Haiderer O, Kennedy JG. Intra-aortic balloon pumping (IABP) at different levels of experimental acute left ventricular failure. Chest. 1971;59:68–76. doi: 10.1378/chest.59.1.68. [DOI] [PubMed] [Google Scholar]


