Abstract
Purpose
To identify the frequency of and factors associated with changes in employment among cancer survivors.
Methods
This prospective cohort study took place in the context of the population-based Cancer Care Outcomes Research and Surveillance Consortium. Patients with nonmetastatic lung or colorectal cancer who survived approximately 15 months after diagnosis without cancer recurrence provided their self-reported employment status, employment experiences, and changes in insurance coverage at 4 and 15 months after diagnosis. Multiple logistic regression was used to relate sociodemographic and disease factors to the probability of labor force departure.
Results
Among 2,422 eligible patients, employment declined from 3% to 31% over the 15 months after cancer was diagnosed. Labor force departures attributable to cancer occurred in 17% of those employed at baseline. Factors associated with significantly higher rates of labor force departure were lung versus colon cancer, stage III versus I or II disease, lower educational and income levels, and, among colorectal patients, older age. Married women were significantly more likely than unmarried women to leave the workforce. Only 2% of patients lacked health insurance during the study period.
Conclusion
Most employed patients with nonmetastatic lung or colorectal cancer return to work, but approximately one sixth of patients leave the workforce, particularly those with worse prognoses or lower socioeconomic status. Potential economic effects must be considered in management decisions about cancer.
INTRODUCTION
There is estimated to be more than 11 million people in the United States with a personal history of cancer.1 Cancer disrupts patients' lives in many ways. One potential sphere is employment. Some patients may have to reduce their time at work, become temporarily disabled, or quit or lose their employment to receive treatment or deal with residual physical or psychological effects of their cancer.2 Moreover, in the United States, such changes in employment status may also lead to changes in health insurance coverage. A study in 2000 found that 18% of cancer survivors were unable to work because of health problems compared with only 10% of matched controls.3 A further 27% were limited in the amount or kind of work they could do. Instances of demotion, denial of promotion, and undesirable transfers have been reported.4,5
Almost all prior studies of the effect of cancer on employment have focused on patients with breast cancer.6–16 This study sought to describe the frequency of altered employment status after a diagnosis of colorectal or lung cancer; to relate changes in employment status to changes in insurance; and to assess the patient sociodemographic, disease, and treatment characteristics that may predict such changes.
METHODS
Study Design
This analysis was carried out using data collected by the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium. This study has been described in detail elsewhere.17 CanCORS is a collaboration of seven research sites from around the United States funded by the National Cancer Institute and the Department of Veterans Affairs to evaluate the quality of cancer care. The CanCORS study was approved by the institutional review boards at each site.
Between May 2003 and December 2005, each site identified, through either a rapid case registry or from administrative data, a population-based sample of patients with newly diagnosed lung or colorectal cancer. The primary data sources in CanCORS were patient surveys and medical record review. Data were collected about the care that the patients received during different stages of illness (including diagnosis, treatment, surveillance for recurrent disease, and palliation), comorbidity, outcomes, and information about patient and provider preferences and behaviors. Patients were interviewed by telephone an average of 4 months after diagnosis (baseline survey) and again at an average of 15 months after diagnosis (follow-up survey). Patients who became too ill to participate or who would rather have a close relative or other caregiver respond could elect a surrogate respondent. There were long and short versions of the survey; the latter was used for patients who were not willing to answer the full survey. Spanish- and Chinese-language versions of the surveys were administered by bilingual interviewers.
Cohort Selection
For this analysis, we identified patients alive at the time of the baseline survey with stage I to III (nonmetastatic) lung or colorectal cancer at presentation, who were alive and completed the follow-up survey, who had completed primary therapy at the time of the follow-up survey, and who had not experienced a recurrence of their cancer within 15 months of diagnosis.
Analytic Variables
The dependent variables for the analysis were based on questions from the CanCORS follow-up survey in which surviving patients were asked, “When you were diagnosed with your (cancer) were you working in a job for which you got paid?” Self-employed respondents were instructed to answer “yes.” Patients were then asked, “Are you now working in a job for which you get paid?” If they had been working at any of these time points, they were then asked specifically about whether they had taken a leave of absence, changed jobs, declined job advancement, quit, or been fired. Respondents were also asked detailed questions about their health insurance and whether their insurance status changed at any time after the diagnosis of cancer.
Disease and treatment factors were obtained from the baseline and follow-up surveys and medical records. Race and ethnicity were self-reported on the baseline survey. On the basis of prior knowledge of factors likely to influence employment status, age, sex, race/ethnicity, marital status, level of schooling, baseline household income level, insurance coverage, cancer type, presenting stage, and receipt of chemotherapy at any point were chosen for evaluation in regression modeling; the final model was obtained using forward selection on all variables and two-way interactions with a significance threshold of P = .05. Each of these variables was measured with an item response rate of greater than 99%, except for income, which had an item response rate of 89.6%. Because of item nonresponse, all analyses reported here were performed on a multiply-imputed data set using standard statistical methods for multiply-imputed data. Imputations were performed using sequential regression multiple imputation, an iterative imputation procedure in which each partially observed variable is regressed on all observed and imputed variables.
Statistical Analysis
We calculated frequencies of labor force departure separately within various categories defined by our independent variables. An overall estimate of excess labor force departure as a result of cancer was calculated by comparing the observed number of employed patients with that expected at follow-up in each age bracket; expected total employment was obtained by multiplying the number of patients in the age bracket at follow-up by the employment rate in that bracket just before diagnosis, which represents the expected number in this cohort at follow-up in the absence of any cancer or treatment effects on employment rate. Job loss as a result of retirement was accounted for by calculating the proportion of patients who would have moved from one age bracket into the next (eg, crossing the usual retirement threshold of age 65) over the course of the 15-month observation period, after which they would be analyzed against the expected employment levels in their new bracket.
We also conducted descriptive analyses of reported experiences in the workplace and alterations in insurance among the patients employed at baseline and alive at follow-up. Subsequently, the analytic cohort was restricted to patients who were younger than 75 years old and employed at diagnosis because most changes in employment status seemed to be concentrated within this group. We conducted exploratory analyses to identify and describe associations between each of the independent variables and a negative alteration in employment or insurance status. Significantly associated predictor variables were then analyzed in a multivariable logistic regression model to identify the sociodemographic and disease factors independently associated with labor force departure. A similar model was created for insurance loss, but that end point was uncommon, so estimates of effect size are not presented.
RESULTS
Cohort Characteristics
The participation rate in the larger CanCORS study was 66.1%, and the absolute response rate to both the baseline and follow-up surveys was 49.3%. CanCORS included 10,180 patients who completed a baseline survey. Of 7,242 patients alive and eligible on follow-up, a follow-up survey was completed by 5,844 (81% follow-up rate). Of those, 2,422 patients were nonmetastatic at baseline and, at the time of follow-up, had completed all treatment and were alive and without recurrence. These patients were included in our analysis. The demographics and clinical characteristics of the cohort are listed in Table 1. Appendix Table A1 (online only) lists the characteristics of the samples from which the cohort was drawn. Both nonrespondents and patients who died before follow-up tended to be older, unmarried, and have lower income and later stage of lung cancer. White and Asian patients seemed to have similar experiences in our data set, as did African American and Hispanic/Latino patients; thus, these groups were combined for analysis.
Table 1.
Patient Demographics and Clinical Characteristics
| Demographic or Clinical Characteristic | All Patients |
% of Patients Working Before Diagnosis | % of Patients Working at 15 Months | |
|---|---|---|---|---|
| No. | % | |||
| Total | 2,422 | 100 | 39 | 31 |
| Age at diagnosis, years | ||||
| 21-49 | 236 | 10 | 76 | 65 |
| 50-54 | 224 | 9 | 78 | 66 |
| 55-59 | 291 | 12 | 63 | 52 |
| 60-64 | 332 | 14 | 49 | 35 |
| 65-69 | 395 | 16 | 30 | 21 |
| 70-74 | 354 | 15 | 19 | 15 |
| 75-79 | 318 | 13 | 11 | 9 |
| 80+ | 272 | 11 | 5 | 4 |
| Sex | ||||
| Male | 1,282 | 53 | 42 | 33 |
| Female | 1,134 | 47 | 35 | 28 |
| Race/ethnicity | ||||
| Non-Hispanic white | 1,788 | 74 | 36 | 30 |
| African American | 292 | 12 | 45 | 29 |
| Hispanic/Latino | 145 | 6 | 48 | 31 |
| Asian | 71 | 3 | 54 | 48 |
| > 1 race | 72 | 3 | 36 | 29 |
| Marital status | ||||
| Married | 1487 | 63 | 41 | 33 |
| Unmarried | 935 | 37 | 33 | 26 |
| Income at baseline, $ | ||||
| < 10,000 | 165 | 7 | 25 | 10 |
| 10,000-15,000 | 245 | 10 | 22 | 11 |
| 15,000-20,000 | 212 | 9 | 26 | 16 |
| 20,000-40,000 | 697 | 29 | 32 | 25 |
| 40,000-60,000 | 483 | 20 | 41 | 36 |
| 60,000-80,000 | 205 | 8 | 54 | 42 |
| 80,000-100,000 | 173 | 7 | 58 | 49 |
| 100,000-120,000 | 100 | 4 | 60 | 51 |
| 120,000+ | 141 | 6 | 70 | 65 |
| Highest educational level attended | ||||
| Elementary | 140 | 6 | 25 | 14 |
| High school | 946 | 39 | 35 | 24 |
| College/vocational | 892 | 37 | 42 | 35 |
| Graduate school | 444 | 18 | 46 | 40 |
| Insurance at baseline | ||||
| Private | 1,767 | 73 | 43 | 35 |
| Public* | 1,464 | 60 | 19 | 14 |
| None | 47 | 2 | 53 | 30 |
| Primary cancer site | ||||
| Lung | 812 | 34 | 32 | 21 |
| Colorectal | 1,610 | 66 | 42 | 35 |
| Stage | ||||
| I | 1,031 | 43 | 38 | 30 |
| II | 732 | 30 | 39 | 31 |
| III | 639 | 27 | 39 | 32 |
| Chemotherapy† | ||||
| Yes | 972 | 40 | 50 | 37 |
| No | 1,449 | 60 | 31 | 26 |
| Comorbidity | ||||
| Total lung cancer | 812 | |||
| Total CRC | 1,610 | |||
| Heart attack | ||||
| Lung cancer | 114 | 14 | 18 | 6 |
| CRC | 147 | 9 | 19 | 14 |
| Heart failure | ||||
| Lung cancer | 59 | 7 | 10 | 9 |
| CRC | 78 | 4 | 22 | 18 |
| Stroke | ||||
| Lung cancer | 73 | 9 | 23 | 14 |
| CRC | 121 | 7 | 20 | 14 |
| Lung disease | ||||
| Lung cancer | 301 | 37 | 30 | 17 |
| CRC | 198 | 12 | 30 | 27 |
| Diabetes | ||||
| Lung cancer | 109 | 13 | 22 | 16 |
| CRC | 325 | 20 | 28 | 24 |
| Other | ||||
| Lung cancer | 361 | 44 | 38 | 28 |
| CRC | 983 | 61 | 51 | 42 |
Abbreviation: CRC, colorectal cancer.
Public insurance includes Medicare, Medicaid, or Veterans Affairs/military insurance.
Chemotherapy indicates receipt of chemotherapy before baseline survey as part of treatment for cancer.
Overall Employment Trends
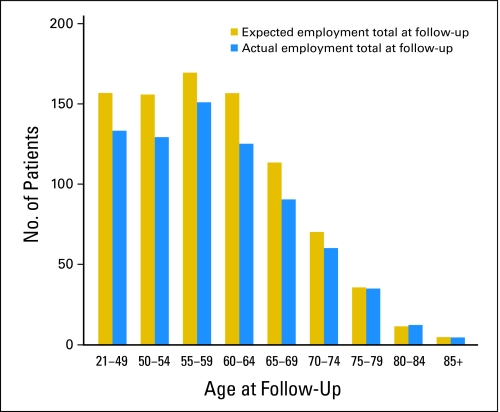
Among the 2,422 survivors, 936 (39%) were employed at diagnosis. At follow-up, only 693 of these patients (29%) were employed. Of note, 48 individuals not employed at the time of their diagnosis were employed at follow-up, resulting in an overall employment rate at follow-up of 31%. Because 70% of the cohort consisted of patients age 60 and older, some workforce departure would be expected over a 15-month follow-up even in the absence of cancer (Fig 1). Figure 2 and Table 2 show the observed versus expected workforce departure rates, accounting for the cohort's aging. Clearly, most labor force departure attributable to cancer occurred in patients younger than age 75. Among all patients younger than 75 who were employed at diagnosis and survived to follow-up, excess labor force departures occurred in 17%.
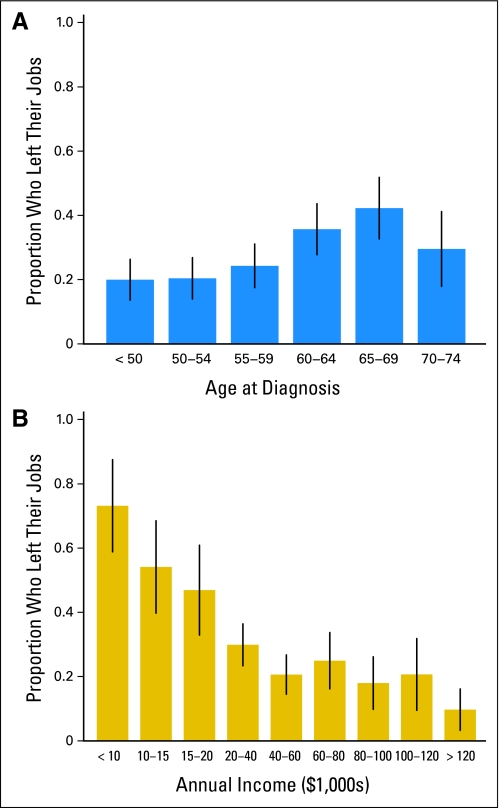
Fig 1.
Workforce departure by (A) age and (B) income stratum. Vertical bars denote 95% CIs for the rate within each stratum.
Fig 2.
Expected versus actual employment status at approximately 15 months after diagnosis.
Table 2.
Expected Versus Actual Employment Status at Approximately 15 Months After Diagnosis
| Employment | Age Group (years) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 21-49 | 50-54 | 55-59 | 60-64 | 65-69 | 70-74 | 75-79 | 80-84 | 85+ | |
| Expected employment rate, % | 76 | 78 | 63 | 49 | 30 | 19 | 11 | 5 | 4 |
| Actual employment rate, % | 64 | 65 | 55 | 39 | 24 | 17 | 11 | 5 | 4 |
NOTE. An overall estimate of excess labor force departure as a result of cancer was calculated by comparing the observed number of employed patients with that expected at follow-up in each age bracket; expected total employment was obtained by multiplying the number of patients in the age bracket at follow-up by the employment rate in that bracket just before diagnosis, which represents the expected number in this cohort at follow-up in the absence of any cancer or treatment effects on employment rate.
Multivariable Analyses
On logistic regression predicting job loss, there were significant interactions for patients with different groupings of selected characteristics that were related to hypotheses. Main effects are listed in Table 3, whereas the effects of various interactions are listed in Appendix Tables A2 to A4 (online only). Lung cancer was associated with higher risk of departing the workforce than colon cancer, as was later stage disease. For example, the adjusted odds ratio for patients with stage I to II lung cancer versus colorectal cancer younger than age 60 was 2.8 (95% CI, 1.5 to 5.2; P = .001), and for stage III disease, it was 6.1 (95% CI, 2.8 to 13.2; P < .001). Differences between African American or Hispanic patients and white or Asian patients varied with age and income level but did not reach statistical significance. Better educated survivors were less likely to leave the workforce. Examination of the relationship of marital status with workforce departure suggested that at lower income levels, married women were more likely than unmarried women to leave the workforce (adjusted odds ratio for unmarried v married women = 0.36; 95% CI, 0.15 to 0.90; P = .03), whereas there was no significant difference among men regardless of income. Across all income levels, older patients were either equally likely or more likely to leave the workforce than younger patients. After adjusting for other variables, however, the difference in workforce departure between older and younger patients was only statistically significant (P < .05) among higher income patients with colon cancer.
Table 3.
Logistic Regression Model of Main Effects Predicting Workforce Departure
| Variable | Estimated Odds Ratio Coefficient* | Estimated 95% CI |
|---|---|---|
| Intercept | 1.17 | 0.28 to 4.91 |
| Age > 60 years | 0.33 | 0.07 to 1.54 |
| Female sex | 1.75 | 0.74 to 4.14 |
| Race (1 = African American/Hispanic, 0 = white/Asian) | 2.41 | 0.54 to 10.69 |
| Unmarried | 1.52 | 0.77 to 3.02 |
| Female sex × unmarried | 0.24 | 0.08 to 0.72 |
| Lung cancer v colorectal cancer | 2.83 | 1.54 to 5.19 |
| Chemotherapy receipt | 1.36 | 0.92 to 2.02 |
| Education (1 = elementary, 2 = high school, 3 = college, 4 = graduate) | 0.76 | 0.62 to 0.95 |
| Public health insurance | 1.42 | 0.76 to 2.66 |
| Stage III v I or II | 1.65 | 1.01 to 2.69 |
| Lung cancer × stage III | 2.16 | 0.97 to 4.82 |
| Lung cancer × age > 60 years | 0.49 | 0.23 to 1.04 |
| Race × age > 60 years | 1.28 | 0.55 to 2.98 |
| Income.low† | 0.41 | 0.23 to 0.70 |
| Income > $40,000 | 2.12 | 0.62 to 7.28 |
| Female sex × income > $40,000 | 0.62 | 0.22 to 1.75 |
| Unmarried × income > $40,000 | 0.26 | 0.07 to 1.00 |
| Female sex × unmarried × income > $40,000 | 6.55 | 0.98 to 43.87 |
| Public insurance × income > $40,000 | 0.82 | 0.33 to 2.06 |
| Age > 60 years × income.low | 2.08 | 1.15 to 3.74 |
| Age > 60 years × income > $40,000 | 0.48 | 0.13 to 1.81 |
| Race × income.low | 0.79 | 0.43 to 1.46 |
| Race × income > $40,000 | 1.84 | 0.44 to 7.70 |
Odds ratio coefficient represents the exponentiated value of the regression coefficient in the logistic regression model. Thus, for instance, if a patient with stage III lung cancer and a patient with stage III colorectal cancer have identical values of all other covariates, then the model predicts that the odds of workforce departure of the patient with lung cancer are 2.83 × 2.16 = 6.11 times the odds for the patient with colorectal cancer.
Income.low is defined as follows: (1/10,000) × (X–max[0, (X–40,000)]), where X = midpoint of patient's income bracket. Thus, a patient whose income falls into the $15,000 to $20,000 bracket has an income.low value of 1.75. A patient whose income is greater than $40,000, by contrast, has an income.low value of 4.
Experiences in the Workplace
On the follow-up survey, some patients who had been employed at baseline reported adverse experiences at work, such as being passed over for promotion or being treated differently by coworkers, but these experiences were not common and were not related to labor force departure. Not unexpectedly, 39% of patients missed some time at work, and 31% felt that their work suffered. Ten percent of employed patients quit work, although it is not known whether some of these patients did so voluntarily. Five percent of patients reported being fired.
Insurance
Overall, only 2% of patients reported being without insurance at diagnosis, baseline, or follow-up. On the follow-up survey, only 12% of survivors had experienced a change in their insurance coverage since the time of the baseline survey. Among those who reported a change in insurance, 26% reported that it was better, 48% said that it was about the same, and 26% said that their insurance coverage was worse than it was before diagnosis. Higher income, older age, and having public insurance were all significantly associated with a lower probability of insurance loss. As could be expected, loss of employment was associated with loss of insurance, although the association did not reach statistical significance after adjusting for other variables. Overall, only 29 patients reported losing health insurance coverage completely between diagnosis and follow-up.
DISCUSSION
Many cancer survivors face challenges that extend beyond strictly medical issues, including their ability to continue working and maintain insurance coverage. Prior research on this topic is dominated by cross-sectional or retrospective studies.18 Prospective studies like ours have focused mainly on patients with breast cancer and have shown that most employed patients return to work19 and that some are able to work through cancer treatment.4 This study adds to the literature by exploring these issues in patients with lung or colorectal cancer and presenting estimates of workforce departures that can be attributed to patients' cancer.
In our study, 74% of patients employed at diagnosis were also employed at follow-up. This compares favorably to the rate of 62% found by Spelten et al19 in their review of the employment literature related to cancer. When adjusted for age-related workforce departure, the excess rate of workforce departure was 17%. Moreover, we found little evidence that cancer survivors experience overt discrimination at work. In our study, younger, less educated, and lower income patients were particularly prone to depart from the workforce. If a young cancer survivor departs the workforce permanently because of cancer, the cumulative loss of potential earnings is enormous.3 Bradley et al20 found the effect of breast cancer on labor force departure to be twice as great in African American women than in white women. Our study did not find conclusive evidence of racial differences after adjusting for factors such as age, education level, and income, although we had only limited statistical power to investigate this effect in all subgroups, particularly among older patients. The finding that wage loss is associated with lower sociodemographic status has been reported in other contexts.21 For example, Lauzier et al6 found that lower education, shorter tenure in a job, part-time work, and self-employment were all associated with wage loss in a prospective cohort of women with breast cancer in Quebec, Canada. Rothstein et al22 found manual laborers to be most likely and professionals least likely to have their job duties reassigned on return to work. Drolet et al13 reported that being unionized was protective for these workers.
We did not find an association between receipt of chemotherapy and workforce departure. However, more advanced disease is understandably a barrier to work that has also been observed in other studies.2 Cancer and its treatment often leave patients with disabilities that may be subtle or pronounced, such as difficulty with memory and concentration (so-called chemo-brain) or fatigue that can interfere with the ability to perform work-related tasks. In one survey of working-age cancer survivors, 17% reported that they were unable to work because of physical, mental, or emotional problems.23 Although data on cancers other than breast cancer are limited, survivors of brain tumors, leukemia, and head and neck cancers may be particularly vulnerable.2 In addition to the direct effects of cancer, logistical burdens related to care may also lead to workforce departure.
Insurance loss did not seem to be a significant problem for CanCORS participants. This may have been partly related to selection into the cohort for some patients, such as those in the Veterans Affairs sites. Married women of lower incomes were significantly more likely than unmarried women to stop working,24 possibly because they may have a spouse who is the primary source of health insurance or income in their households, resulting in more flexibility to leave the workforce. Similarly, patients near age 65 years may be more likely to leave work as they become eligible for Medicare insurance. Patients who exited the workforce seem to have either obtained public insurance (ie, those age > 65 years) or insurance through a family member (ie, married women). Patients younger than age 65, unmarried patients, and patients who are the primary breadwinners may not be able to do so as easily.
A recent study found that workers with health coverage at cancer diagnosis were no more likely to alter employment after treatment than similar insured workers without cancer but that cancer survivors with no employer-related health insurance were more likely to stop working, switch jobs, or cut back from full-time to part-time work than other workers with health insurance.25 There are some protections in place for patients who depart the workforce. Examples include the Consolidated Omnibus Budget Reconciliation Act, which allows workers to maintain their health insurance for 18 months after losing or leaving a job, and the Health Insurance Portability and Accountability Act (HIPAA), which prohibits insurers from denying or limiting coverage because of pre-existing conditions. However, Consolidated Omnibus Budget Reconciliation Act premium surcharges are not controlled and can be insurmountable for patients who are unemployed, and the HIPAA provisions do not apply to employers with less than 20 workers.
Our study has some limitations. Although the goal of CanCORS was to create a population-based cohort of patients, nonparticipants may have differed from participants. Nonetheless, participants in CanCORS have been shown to be demographically similar to population-based samples with these cancers in Surveillance, Epidemiology, and End Results registries.26 However, the older age distribution of the cohort resulted in less than half of the patients being employed at diagnosis and somewhat limits the power to study employment trends. Among participants, there was further attrition between the baseline and follow-up surveys for a variety of reasons, including death, and these patients may have experienced even greater rates of workforce departure than patients able to complete the follow-up survey. We did not have information on the specific types of jobs patients had. We also did not know whether patients had other sources of support, such as disability benefits, which may have affected their decision making regarding returning to work. Finally, insurance loss was an uncommon problem in our study cohort, so we were unable to explore this issue in great depth.
We found that approximately 80% of patients with colorectal and lung cancer who survive their cancer are able to return to work. However, patients who are most vulnerable to the negative economic consequences of cancer are those with the most need of support—those with the fewest resources and the most advanced disease. These findings are worthy of consideration in several types of policy decisions. For example, employers have an interest in choosing health plans with adequate resources to assist survivors to return to work. Moreover, because primary cancer treatment often takes longer than 12 weeks to complete, federal and state governments should consider lengthening the duration of guaranteed medical leaves in the workplace. Finally, patients may benefit from discussions with clinicians about the possibility that their cancer could impact their ability to work. Ultimately, new strategies to limit cancer-related disability will be important to minimize disruptions in employment.
Appendix
Table A1.
Demographic and Clinical Characteristics of the CanCORS Cohort
| Characteristic | % of Patients With Any Type of Baseline Survey (N = 10,180) | % of Eligible Patients With a Follow-Up Survey (n = 5,844) |
|---|---|---|
| Sex | ||
| Male | 57 | 56 |
| Female | 43 | 44 |
| Age at diagnosis, years | ||
| < 50 | 8 | 10 |
| 50-54 | 8 | 9 |
| 55-59 | 11 | 12 |
| 60-64 | 12 | 13 |
| 65-69 | 15 | 15 |
| 70-74 | 15 | 15 |
| 75-79 | 14 | 14 |
| 80-84 | 10 | 9 |
| 85+ | 6 | 4 |
| Marital status | ||
| Married | 58 | 60 |
| Not married | 42 | 40 |
| Race/ethnicity | ||
| Non-Hispanic white | 68 | 70 |
| African American | 14 | 14 |
| Hispanic/Latino | 7 | 7 |
| Asian | 5 | 4 |
| Primary cancer site | ||
| Lung | 51 | 45 |
| Colorectal | 49 | 55 |
| Stage | ||
| I | 21 | 24 |
| II | 14 | 16 |
| III | 23 | 23 |
| IV | 23 | 15 |
| Descriptive staging (local/regional/distant) | 20 | 21 |
Abbreviation: CanCORS, Cancer Care Outcomes Research and Surveillance.
Table A2.
Association Between Selected Variables and Workforce Departure: Observed Rates and aORs for Each Group
| Variable | < Age 60 Years |
≥ Age 60 Years |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Departed Workforce |
aOR | 95% CI | P | Departed Workforce |
aOR | 95% CI | P | |||
| No. of Patients | % | No. of Patients | % | |||||||
| Disease stage | ||||||||||
| I/II | 2.8 | 1.5 to 5.2 | .001 | 1.4 | 0.81 to 2.4 | .23 | ||||
| Lung cancer | 82 | 27 | 101 | 36 | ||||||
| Colorectal cancer | 285 | 22 | 155 | 25 | ||||||
| III | 6.1 | 2.8 to 13.2 | < .001 | 3.0 | 1.4 to 6.5 | .005 | ||||
| Lung cancer | 27 | 67 | 31 | 58 | ||||||
| Colorectal cancer | 143 | 18 | 64 | 47 | ||||||
| Income, $ | ||||||||||
| 10,000-20,000 | 1.7 | 0.75 to 3.8 | .20 | 2.2 | 0.97 to 5.0 | .06 | ||||
| African American/Hispanic | 21 | 55 | 12 | 48 | ||||||
| White/Asian | 26 | 43 | 41 | 47 | ||||||
| 40,000-80,000 | 1.8 | 0.86 to 3.6 | .12 | 2.3 | 1.0 to 5.1 | .05 | ||||
| African American/Hispanic | 33 | 19 | 15 | 55 | ||||||
| White/Asian | 149 | 12 | 100 | 29 | ||||||
Abbreviation: aOR, adjusted odds ratio.
Table A3.
Association Between Selected Variables and Workforce Departure: Observed Rates and aORs for Each Group
| Income ($) | Men |
Women |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Departed Workforce |
aOR | 95% CI | P | Departed Workforce |
aOR | 95% CI | P | |||
| No. of Patients | % | No. of Patients | % | |||||||
| 10,000-20,000 | 1.5 | 0.76 to 3.0 | .23 | 0.36 | 0.15 to 0.90 | .03 | ||||
| Unmarried | 25 | 58 | 41 | 42 | ||||||
| Married | 40 | 40 | 6 | 77 | ||||||
| 40,000-80,000 | 0.4 | 0.13 to 1.2 | .11 | 0.63 | 0.25 to 1.6 | .33 | ||||
| Unmarried | 30 | 11 | 42 | 15 | ||||||
| Married | 142 | 22 | 82 | 24 | ||||||
Abbreviation: aOR, adjusted odds ratio.
Table A4.
Association Between Selected Variables and Workforce Departure: Observed Rates and aORs for Each Group
| Cancer | White/Asian |
African American/Hispanic |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Departed Workforce |
aOR | 95% CI | P | Departed Workforce |
aOR | 95% CI | P | |||
| No. of Patients | % | No. of Patients | % | |||||||
| Lung | ||||||||||
| Income: $10,000-$20,000 | 0.5 | 0.20 to 1.2 | .12 | 0.6 | 0.22 to 1.8 | .38 | ||||
| Age, years | ||||||||||
| ≥ 60 | 20 | 51 | 3 | 35 | ||||||
| < 60 | 10 | 80 | 6 | 34 | ||||||
| Income: ≥ $40,000 | 1.4 | 0.71 to 3.0 | .31 | 1.9 | 0.64 to 5.4 | .26 | ||||
| Age, years | ||||||||||
| ≥ 60 | 56 | 27 | 5 | 100 | ||||||
| < 60 | 60 | 24 | 8 | 28 | ||||||
| Colorectal | ||||||||||
| Income, $10,000-$20,000 | 1.0 | 0.42 to 2.38 | .99 | 1.3 | 0.50 to 3.3 | .61 | ||||
| Age, years | ||||||||||
| ≥ 60 | 21 | 43 | 8 | 52 | ||||||
| < 60 | 16 | 19 | 15 | 64 | ||||||
| Income: ≥ $40,000 | 2.9 | 1.6 to 5.5 | .001 | 3.8 | 1.5 to 9.5 | .005 | ||||
| Age, years | ||||||||||
| ≥ 60 | 106 | 24 | 18 | 36 | ||||||
| < 60 | 243 | 9 | 52 | 13 | ||||||
Abbreviation: aOR, adjusted odds ratio.
Footnotes
Supported by Grant No. U01 CA093344 from the National Cancer Institute (NCI) to the Statistical Coordinating Center; by NCI-supported Primary Data Collection and Research Centers Grants No. U01 CA093332 to Dana-Farber Cancer Institute/Cancer Research Network, U01 CA093324 to Harvard Medical School/Northern California Cancer Center, U01 CA093348 to RAND/University of California, Los Angeles, U01 CA093329 to University of Alabama at Birmingham, U01 CA01013 to University of Iowa, U01 CA093326 to University of North Carolina; and by a Department of Veteran's Affairs grant to the Durham VA Medical Center CRS 02-164.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Craig C. Earle, Yves Chretien, John Z. Ayanian, Robert Wallace, Patricia A. Ganz, Jane C. Weeks
Collection and assembly of data: Craig C. Earle, John Z. Ayanian, Nancy L. Keating, Robert Wallace, Patricia A. Ganz, Jane C. Weeks
Data analysis and interpretation: Craig C. Earle, Yves Chretien, Carl Morris, Linnea A. Polgreen, Robert Wallace, Patricia A. Ganz, Jane C. Weeks
Manuscript writing: Craig C. Earle, Yves Chretien
Final approval of manuscript: Craig C. Earle, Yves Chretien, Carl Morris, John Z. Ayanian, Nancy L. Keating, Linnea A. Polgreen, Robert Wallace, Patricia A. Ganz, Jane C. Weeks
REFERENCES
- 1.Ries LAG, Melbert D, Krapcho M, et al. Bethesda, MD: National Cancer Institute; 2008. SEER Cancer Statistics Review, 1975-2005. [Google Scholar]
- 2.Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer. 2005;103:1292–1301. doi: 10.1002/cncr.20912. [DOI] [PubMed] [Google Scholar]
- 3.Yabroff KR, Lawrence WF, Clauser S, et al. Burden of illness in cancer survivors: Findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–1330. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 4.Messner C, Patterson D. The challenge of cancer in the workplace. Cancer Pract. 2001;9:50–51. doi: 10.1046/j.1523-5394.2001.91009.x. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Washington, DC: National Academies Press; 2005. From Cancer Patient to Cancer Survivor: Lost in Transition. [Google Scholar]
- 6.Lauzier S, Maunsell E, Drolet M, et al. Wage losses in the year after breast cancer: Extent and determinants among Canadian women. J Natl Cancer Inst. 2008;100:321–332. doi: 10.1093/jnci/djn028. [DOI] [PubMed] [Google Scholar]
- 7.Gordon L, Scuffham P, Hayes S, et al. Exploring the economic impact of breast cancers during the 18 months following diagnosis. Psychooncology. 2007;16:1130–1139. doi: 10.1002/pon.1182. [DOI] [PubMed] [Google Scholar]
- 8.Lidgren M, Wilking N, Jonsson B, et al. Resource use and costs associated with different states of breast cancer. Int J Technol Assess Health Care. 2007;23:223–231. doi: 10.1017/S0266462307070328. [DOI] [PubMed] [Google Scholar]
- 9.Arozullah AM, Calhoun EA, Wolf M, et al. The financial burden of cancer: Estimates from a study of insured women with breast cancer. J Support Oncol. 2004;2:271–278. [PubMed] [Google Scholar]
- 10.Lauzier S, Maunsell E, De KM, Drolet M, et al. Conceptualization and sources of costs from breast cancer: Findings from patient and caregiver focus groups. Psychooncology. 2005;14:351–360. doi: 10.1002/pon.851. [DOI] [PubMed] [Google Scholar]
- 11.Maunsell E, Brisson C, Dubois L, et al. Work problems after breast cancer: An exploratory qualitative study. Psychooncology. 1999;8:467–473. doi: 10.1002/(sici)1099-1611(199911/12)8:6<467::aid-pon400>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 12.Chirikos TN, Russell-Jacobs A, Cantor AB. Indirect economic effects of long-term breast cancer survival. Cancer Pract. 2002;10:248–255. doi: 10.1046/j.1523-5394.2002.105004.x. [DOI] [PubMed] [Google Scholar]
- 13.Drolet M, Maunsell E, Mondor M, et al. Work absence after breast cancer diagnosis: A population-based study. CMAJ. 2005;173:765–771. doi: 10.1503/cmaj.050178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maunsell E, Drolet M, Brisson J, et al. Work situation after breast cancer: Results from a population-based study. J Natl Cancer Inst. 2004;96:1813–1822. doi: 10.1093/jnci/djh335. [DOI] [PubMed] [Google Scholar]
- 15.Chirikos TN, Russell-Jacobs A, Jacobsen PB. Functional impairment and the economic consequences of female breast cancer. Women Health. 2002;36:1–20. doi: 10.1300/J013v36n01_01. [DOI] [PubMed] [Google Scholar]
- 16.Bradley CJ, Bednarek HL, Neumark D. Breast cancer survival, work, and earnings. J Health Econ. 2002;21:757–779. doi: 10.1016/s0167-6296(02)00059-0. [DOI] [PubMed] [Google Scholar]
- 17.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: The Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22:2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 18.de Boer AG, Taskila T, Ojajarvi A, van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: A meta-analysis and meta-regression. JAMA. 2009;301:753–762. doi: 10.1001/jama.2009.187. [DOI] [PubMed] [Google Scholar]
- 19.Spelten ER, Sprangers MA, Verbeek JH. Factors reported to influence the return to work of cancer survivors: A literature review. Psychooncology. 2002;11:124–131. doi: 10.1002/pon.585. [DOI] [PubMed] [Google Scholar]
- 20.Bradley CJ, Neumark D, Bednarek HL, et al. Short-term effects of breast cancer on labor market attachment: Results from a longitudinal study. J Health Econ. 2005;24:137–160. doi: 10.1016/j.jhealeco.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Park JH, Park EC, Park JH, et al. Job loss and re-employment of cancer patients in Korean employees: A nationwide retrospective cohort study. J Clin Oncol. 2008;26:1302–1309. doi: 10.1200/JCO.2007.14.2984. [DOI] [PubMed] [Google Scholar]
- 22.Rothstein MA, Kennedy K, Ritchie KJ, et al. Are cancer patients subject to employment discrimination? Oncology (Williston Park) 1995;9:1303–1306. [PubMed] [Google Scholar]
- 23.Hewitt M, Breen N, Devesa S. Cancer prevalence and survivorship issues: Analyses of the 1992 National Health Interview Survey. J Natl Cancer Inst. 1999;91:1480–1486. doi: 10.1093/jnci/91.17.1480. [DOI] [PubMed] [Google Scholar]
- 24.Bradley CJ, Bednarek HL. Employment patterns of long-term cancer survivors. Psychooncology. 2002;11:188–198. doi: 10.1002/pon.544. [DOI] [PubMed] [Google Scholar]
- 25.Tunceli K, Short PF, Moran JR, et al. Cancer survivorship, health insurance, and employment transitions among older workers. Inquiry. 2009;46:17–32. doi: 10.5034/inquiryjrnl_46.01.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Catalano P. Representativeness of CanCORS participants relative to Surveillance, Epidemiology, & End Results (SEER) Cancer Registries. Presented at the 2008 AcademyHealth Annual Research Meeting; June 8-10, 2008; Washington, DC. [Google Scholar]