Abstract
Objectives
Determine the impact of an 8-week mindfulness meditation program on disability, psychological function, and pain severity in community-dwelling older adults with chronic low back pain, and to test the education control program for feasibility.
Design
Randomized controlled trial.
Participants
Forty community-dwelling older adults with moderate low back pain or greater for at least the previous 3 months.
Intervention
Participants were randomized to an 8-week meditation program or an 8-week education control program.
Outcome Measures
Disability, psychological function, and pain severity were assessed. The same measures were obtained for both groups at baseline, at the end of the program, and 4 months after program completion.
Results
Sixteen participants (80%) completed the meditation program and 19 (95%) completed the education program. Both the meditation and control group improved on measures of disability, pain, and psychological function, both at program completion and 4-month follow-up. The differences between the two groups did not reach statistical significance. The meditation group practiced mindfulness meditation a mean of 5 days/week (range 1–7) and mean of 31 minutes/session (range 22–48). At 4 months follow-up 14/16 (88%) participants continued to meditate.
Conclusion
Both the intervention group and the education control group improved on outcome measures suggesting both programs had a beneficial effect. Participants continued to meditate on 4-month follow-up. The control program was feasible but not inert. Piloting the control program in mind–body research can inform the design of larger clinical trials.
Keywords: Low Back Pain, Mindfulness, Meditation, Mind-Body, Aged
Introduction
Among the 37 million seniors (≥65 years) alive today [1], it is estimated that up to 50% of them live with chronic pain [2]. Greater than 17 million elders have experienced at least one episode of low back pain (LBP) during the past year [3] and it is the most frequently reported musculoskeletal problem [4]. Medicare data from 1991–2002 indicate that visits for LBP increased 132% and LBP charges increased 388% [5]. Pain is associated with a significant amount of morbidity in the older adult and includes decreased physical function, disability, quality of life, poor sleep, and depression [6]. Despite its prevalence and associated morbidities, many older adults suffer from inadequately treated pain. Why should this be the case? Because conventional treatment options are not always feasible for the older adult. Nonsteroidal anti-inflammatory agents (NSAIDs) and opioids are commonly toxic in the older population. NSAIDs are limited by their well-described gastrointestinal and nephrotoxic side effects [7]. Opioids are associated with an increased susceptibility to falls and hip fractures [8].
Because mind–body therapies such as mindfulness meditation do not use medications, they offer a relatively safe treatment option for older adults who may have exhausted all other forms of pain therapy or for whom the risk of conventional therapy is unacceptably high. As pain is experienced through sensory, cognitive, and affective domains, mindfulness meditation is particularly well-suited to chronic pain patients as it teaches them to work with these domains in a positive way to cope with pain.
There are many forms of meditation that are used for medical purposes around the world. The two forms used commonly in the United States are mantra meditation and mindfulness meditation. Meditation has been difficult to define because there are many types of meditation that people practice worldwide. Nevertheless, the Agency for Healthcare Research and Quality published a 2007 report on Meditation Practices for Health and offered the following definition:
A form of mental training that requires either stilling or emptying the mind, and that has as its goal a state of “detached observation” in which practitioners are aware of their environment, but do not become involved in thinking about it [9].
Kabat-Zinn, who first introduced mindfulness meditation to the medical community, described mindfulness simply as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” [10]. This is congruent with the consensus definition of meditation above. To elaborate on Kabat-Zinn’s simple definition, Shapiro [11] has proposed three aspects of mindfulness that include 1) the intention or purpose of practicing mindfulness that is set by the individual, 2) how attention is placed during the meditation. This involves focusing attention on an object like the breath, and continually bringing back the focus of attention to breathing when it is distracted, and 3) attitude, which describes the attitudes that support mindfulness and include being nonjudgmental toward thought or emotions or sensations as they arise, patience, nonstriving, compassion, acceptance, and curiosity. Other supporting attitudes described have been letting go and trust. This theory of mindfulness is highly relevant to treating chronic pain. This is because it teaches chronic pain patients to uncouple the sensory from the cognitive and emotional responses to pain, which in turn may result in both increased function and pain reduction.
We previously piloted an 8-week mindfulness meditation program among older adults with chronic LBP (CLBP) and have shown it to be feasible. One of the limitations of this initial study was the use of a wait-list control group. We were interested in repeating our initial randomized controlled trial (RCT) [13] with a more rigorous comparison group. A health education program would accomplish this by controlling for group, time, and instructor effects. As there were no examples in the mindfulness literature on the optimum educational program we developed our own. Additionally, we again wanted to test pain and disability outcomes, as well as psychological outcomes we had not previously piloted. We hypothesized that immediately following an 8-week mindfulness meditation program, participants who received the program would demonstrate significantly greater decrease in pain related disability and decrease in pain as compared with control participants who received an 8-week health education program.
Methods
Participants
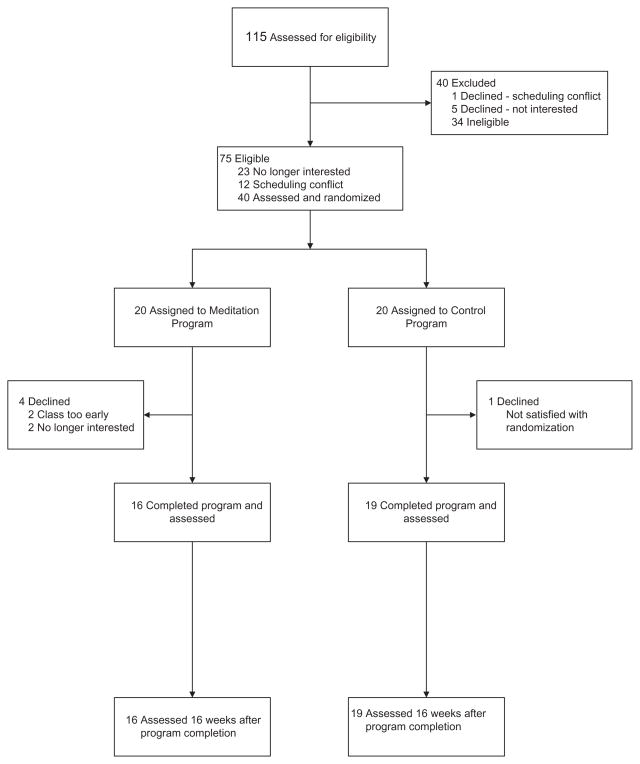
Participants were recruited from the greater Pittsburgh area by local newspaper advertisements, posted flyers, and brochures located in the University of Pittsburgh Medical Center. We screened older adults over the telephone. See Figure 1 for study flow. Inclusion criteria included CLBP of at least 3 months duration and of at least moderate intensity according to a vertical verbal descriptor scale (pain thermometer) [14], age ≥65 years, and intact cognition (Mini-Mental Status Exam ≥24). Exclusion criteria were non-English speaking, previous participation in a mindfulness meditation program, serious hearing or vision impairment that would preclude responding to questionnaires or participating in the meditation program, medical instability from heart or lung disease, multiple recent falls or inability to stand independently, pain caused by an acute injury in the previous 3 months, and underlying red flags of serious underlying illness such as recent unexplained weight loss, fever, or sudden worsening of back pain.
Figure 1.
Participant flow diagram.
Procedures
Informed Consent, Baseline Measures, Randomization
If participants met the inclusion criteria by telephone screening they were invited to the University of Pittsburgh Center for Research on Health Care where informed consent was obtained before baseline measures were administered. The study was approved by the University of Pittsburgh Institutional Review Board.
After informed consent was obtained measures were administered to all participants by a trained research assistant. After completion of measures participants were randomized to the 8-week mindfulness meditation program (intervention) or to the 8-week health education program (control).
The randomization process was performed by a systems analyst using statistical software with a random-number generator to create a list of group assignments before study recruitment began. Randomization occurred in blocks of 10. The assignments were created based on the specific number of expected eligible participants (40) and divided equally between the intervention (20) and control groups (20). Once an eligible participant had completed the baseline measures, the Principal Investigator (PI; N.E.M.) submitted a request to randomize the eligible participant. The program located the first unassigned record in the randomization list and assigned the participant to the group designated in that record. Only the systems analyst had access to the randomization table.
The program was taught by two instructors one of them the PI (N.E.M.). Both have a personal mindfulness meditation practice of 25 years and have undergone at least 50 hours of teacher training in the mindfulness-based stress reduction (MBSR) program [12].
Intervention and Control Program
Intervention Program
Program Principles
The intervention was modeled on the work of Jon Kabat-Zinn at the University of Massachusetts Medical School. He has adapted Eastern methods of mindfulness meditation to a Western audience. Classes met weekly for 8 weeks, and sessions lasted 90 minutes. Three methods of mindfulness meditation were taught. These techniques take regular activities like sitting, walking, and lying down and transform them into a meditation through directed breathing and mindful awareness of thoughts and sensations.
The methods used were 1) the body scan, where in a lying position, the participant is guided to place their attention nonjudgmentally on each area of the body from the toes to the top of the head; 2) sitting practice, where the participant is guided to focus their attention on breathing while sitting on a chair; and 3) walking meditation, where the participant is guided in mindful slow walking with focused attention on body sensation and/or breathing [12].
Program Protocol
During the first week participants were introduced to the principles and practice of mindfulness meditation. The homework requirement of daily meditation (6 of 7 days/week) lasting 50 minutes (45 minutes of meditation, 5 minutes to complete a log) was reviewed. Support materials of CD recording, daily log and reading materials were handed out. The CD recording was a 45 minute guided body scan meditation and a 30 minute guided sitting meditation. Participants were provided with a CD player if they did not own one, which was 1/3 of participants. The reading materials were reviewed during the sessions and were not part of the homework. The body scan technique was taught at the first session. The group meditated together using the body scan technique for 45 minutes at the first, second, and eighth session. If physical discomfort arose during any meditation participants were encouraged to change to a more comfortable position. The first class introduced mindful eating, which was done through a guided exercise of eating a raisin. This exercise began to introduce the concept of informal meditation, in that mindfulness can be brought to everyday activities like eating.
During the second and following weeks the sessions included a general discussion of the participants’ experience with the meditation method, including problem-solving regarding obstacles to the meditation practice. Theoretical material related to meditation, relaxation, pain, and the mind–body connection were presented at this time. About 30 minutes were spent at each session in these discussions. Also during the second week, quiet sitting meditation was introduced. The group practiced together using the sitting meditation technique for 15 minutes during this and at the beginning of subsequent sessions.
The third session introduced pain theory and the multidimensional response to pain. Participants learned about the cognitive, emotional, and sensory components of nociceptive processing. The triangle of awareness was also introduced, which describes the thoughts, emotions, and sensations that make up the activity that arises at any given moment in the mind. The relationship between the multidimensional model of pain and the triangle of awareness was discussed.
The fourth session introduced the flight or fight response and the relaxation response. This was an interactive session with participants describing their response to stress as well as their response to mindfulness meditation. Stress and the relaxation response were discussed in relation to worsening or decreasing pain.
At the fifth week’s session, walking meditation was introduced. How to use mindfulness meditation methods to work with pain were discussed. This occurred at this and all remaining sessions. An interactive approach was taken, so that participants discussed how they had used mindfulness meditation methods to work with pain. Participants were also taught how to work with pain during formal meditation. They learned this by guided meditation during this and subsequent sessions, as well as a recording on CD of the body scan that was specific for working with pain.
At the sixth week’s session applying mindfulness to everyday situations (informal meditation) was discussed.
At the seventh week’s session breaking through habitual tendencies that prevented effective coping with pain were discussed.
The eighth session integrated what had been learned over the course of the program.
Therefore, the structure of each session was 1 hour (total) of meditation and 30 minutes of discussion.
Control Program
A convincing comparison group is essential for subject recruitment and retention as well as essential for controlling for key components of the MBSR program. Therefore, we developed a comparison group that controlled for time, group size, and facilitator time. We based the 8-week health education program on a successful aging curriculum that has been used in other trials [15,16]. The health education curriculum involved lectures, group discussion, and homework assignments based on the health topics discussed. Additionally, a general theme of “brain health” was emphasized for the 8 weeks. Session topics were 1) pain medications, 2) complementary treatments for back pain (focusing on chiropractic), 3) types of back pain, 4) role of physical therapist in treating back pain, 5) eating and health, and 6) Alzheimer’s. Additionally, subjects were given materials to promote participation and retention in the program. They were given the use of a Nintendo DS “Brain Age” game and encouraged to do this as daily homework, as well as homework assignments from the book “Keep Your Brain Alive” [17]. For each class 45–60 minutes were devoted to a lecture given by a heath professional on the topic for the session and 30–45 minutes (total 90 minutes) spent doing a class “brain” exercise and discussion. The consistent presence of a class coordinator (N.E.M.) controlled for the facilitator contact of the MBSR program.
Outcome Measures
The following measures were administered to all participants by a blinded research assistant at baseline, at completion of the 8-week program, and 4 months after completion of the program.
Disability was assessed with the Roland and Morris Disability Questionnaire (RMDQ) that asks yes/no questions about physical function and back pain. Cronbach’s alpha is 0.93 and test–retest correlation is 0.73–0.91 [14,18]. Higher scores indicate more disability.
Pain intensity was assessed with two measures: the Short-Form McGill Pain Questionnaire (SF-MPQ) [19], that is reliable and valid in an older population [20]. Lower scores indicate less pain and the SF-36 Pain scale (see below).
Self-efficacy was assessed with the Chronic Pain Self-Efficacy Scale [21]. It measures chronic pain patients’ perceived ability to cope with chronic pain. It has three subscales: pain self-efficacy (PSE), function self-efficacy, and coping self-efficacy. Cronbach’s alpha among older adults with CLBP is 0.87 for the entire scale [22]. Higher score indicates greater self-efficacy.
Quality of life was measured with the SF-36 Health Status Inventory [23]. It includes two summary scores (physical and mental health) and 8-scale scores. We report the Pain scale and Role Limitations Due to Emotional Problems scale. Normative data are available for older adults. Cronbach’s alpha among older adults is 0.80–0.92 [24]. Higher scores indicate better quality of life.
Mindfulness was assessed with the Mindful Attention Awareness Scale (MAAS) [25] which measures attention and awareness of present moment experience in daily life. Cronbach’s alpha is 0.87 among a general adult population in the United States. Higher scores reflect higher levels of mindfulness. We also administered the Five Facet Mindfulness Questionnaire (FFMQ) [26] that separates mindfulness into five domains: observing, describing, acting with awareness, nonjudging of inner experience, and nonreactivity to inner experience. Cronbach’s alpha for the domains range from 0.67–0.92. Higher scores reflect greater mindfulness.
Additionally, participants were asked about the credibility of the treatment program at baseline and program completion. They were also asked about their global impression of change as a result of the 8-week program at the 4-month follow-up session.
Statistical Methods
Descriptive statistics were used to summarize demographic characteristics of study participants. The t-test was used for the continuous variable age and Fisher’s exact test was used for categorical variables to detect differences in demographic characteristics between those in the intervention and control groups.
To determine whether the meditation program was associated with improvements in disability, pain, self-efficacy, and mindfulness scales, further models were fit using generalized estimating equations. For these analyses, time, treatment groups, the interaction term of time and treatment groups, and baseline age were included as covariates. All generalized estimating equation models were fit using an exchangeable variance structure. All analyses used SAS 9.1.3 (SAS Institute Inc., Cary, NC). We considered a P value of <0.05 to be significant. The small sample size did not lend itself to an imputation technique for missing values and, therefore, a completer’s analysis was performed.
Results
Participants were recruited from the greater Pittsburgh area between July 26, 2007–October 26, 2007. There were 115 people who responded and were screened for eligibility over the telephone. See Figure 1 for a diagram of study flow. Out of 75 eligible callers, 12 had scheduling conflicts and 23 were no longer interested, resulting in 40 adults eligible and available for the study. Twenty were randomized to the meditation program and 20 to the control program. Four participants dropped out of the meditation program. Two did not attend any classes because the class was too early, one dropped out after one class, and one dropped out after three classes. The overall completion rate for the meditation group was 80% (16/20). One person dropped out of the control program before classes started for an overall completion rate of 95% (19/20). Dropouts (from both groups) did not differ significantly from program completers on measures of race, ethnicity, education, marital status, income, religion, comorbid conditions, and cognition. However, dropouts were significantly older (84 vs 76 years, P = 0.03). The meditation group meditated an average of 5 days a week (range 1–7) and meditated an average of 31 minutes/session (range 22–48).
The two groups did not differ significantly on demographic factors (see Table 1), except for age, as the meditation group was significantly older than the control group (78 years vs 73 years respectively, P = 0.03), and because of this all analyses controlled for age. The most common cause of CLBP was osteoarthritis (N = 19). The majority of patients used nonopioid analgesics to treat their back pain. Of the eight classes offered the mean number attended by the intervention group was 7.5 (range 6–8) and by the control group was 7.1 (range 3–8).
Table 1.
Demographic characteristics of study participants
| Treatment Condition |
||
|---|---|---|
| Variable | Meditation n = 16 | Control n = 19 |
| Age*, mean ± SD | 78 ± 7.1 | 73 ± 6.2 |
| Gender, n | ||
| Male | 5 | 8 |
| Female | 11 | 11 |
| Ethnicity, n | ||
| White | 15 | 15 |
| African American | 1 | 3 |
| Asian | 0 | 1 |
| Education†, n | ||
| Low | 4 | 4 |
| Medium | 4 | 4 |
| High | 8 | 11 |
| Religious faith, n | ||
| Yes | 16 | 18 |
| No | 0 | 1 |
| Income, n | ||
| Less than $10,000 | 0 | 2 |
| $10,000–$29,999 | 4 | 5 |
| $30,000–$49,999 | 2 | 4 |
| $50,000 or greater | 4 | 4 |
| Marital status, n | ||
| Single | 0 | 3 |
| Married | 9 | 8 |
| Separated/divorced | 1 | 4 |
| Widowed | 6 | 4 |
| Low back pain cause, n | ||
| Osteoarthritis | 10 | 9 |
| Disc herniation | 1 | 1 |
| Unknown | 4 | 6 |
| Failed back surgery | 1 | 1 |
| Scoliosis | 0 | 3 |
| Spinal stenosis | 5 | 2 |
| Spondylolisthesis | 2 | 1 |
| Osteoporosis | 0 | 1 |
| Medications‡, n | ||
| Opioids | 3 | 5 |
| Other analgesics | 19 | 24 |
| None | 2 | 2 |
| Pain duration§, mean ± SD, (n) | 9.4 ± 18.1 (12) | 11.1 ± 13.7 (14) |
| Folstein Mini-Mental State Examination, mean ± SD | 29.3 ± 0.8 | 29.1 ± 1.2 |
Because P = 0.03 all subsequent analyses adjusted for age.
Low: includes ≤9th, 10th–12th and high school graduate; Medium: includes technical school and some college; High: includes college degree and master’s or above.
Total number of medications >40 because participants could be on more than one type of pain medication.
Data inadvertently not collected on nine participants.
SD = standard deviation.
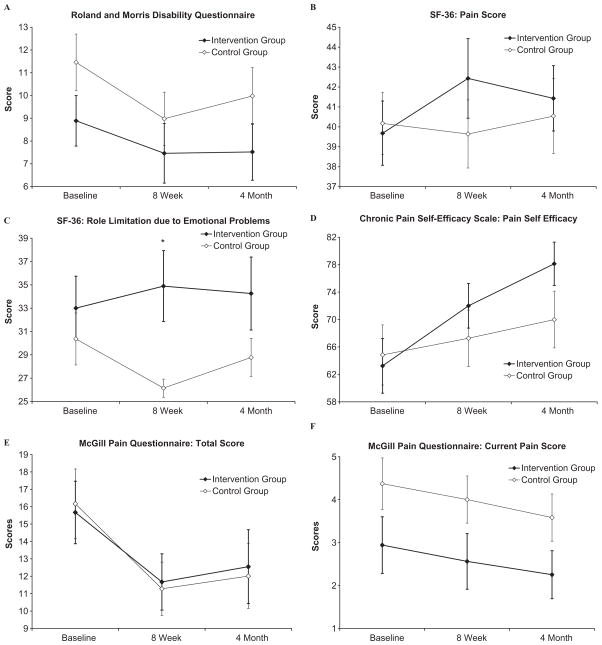
Figure 2 presents the main outcomes for the study. Disability, as measured by the RMDQ and pain, as measured by the SF-MPQ and SF-36 Pain scale improved in the expected direction for the meditation group. The control group also improved, except for pain as measured by the SF-36 Pain scale, which slightly worsened at the completion of the program and then slightly improved at 4-month follow-up. The improvement in disability was maintained at 4 months for the meditation group, but less so for the control group. The differences for disability and pain between the meditation and control groups did not reach statistical significance.
Figure 2.
Effects of meditation (n = 16) vs control (n = 19) in outcomes at completion of the trial (8 weeks) and 4-month follow-up. All graphs present age-adjusted mean scores. (A) Roland and Morris Disability Questionnaire: Answer range 0–24, higher scores indicate more disability. (B) SF-36 Health Status Inventory Pain scale: Answer range 10–62, higher scores indicate improvement. (C) SF-36 Health Status Inventory Role Limitations Due to Emotional Problems scale: Answer range 14–58, higher scores indicate improvement. (D) Chronic Pain Self-Efficacy Scale: Answer range 0–100, higher scores indicate greater self-efficacy. (E) McGill Pain Questionnaire Total Score: Answer range 0–45, lower scores indicate less pain. (F) McGill Pain Questionnaire Current Pain Scale: Answer range 0–10, lower scores indicate less pain. *P < 0.05.
Both groups also improved in self-efficacy at program completion. The meditation group continued to improve in self-efficacy at 4-month follow-up as compared with the control group. While the meditation group improved at program completion and at 4-month follow-up on the SF-36 Role Limitation Due to Emotional Problems scale, the control group did worse. Again, while there are consistent trends toward improvement, these numbers did not reach statistical significance at 4-month follow-up, although there was a statistically significant difference at completion of the 8-week program.
Table 2 presents the results of the two mindfulness scales used in the study. Mindfulness levels were high for the entire sample at baseline and remained stable for the duration of the study. We present the data in detail because this is the first study that presents results of these two mindfulness scales in an exclusively older adult population with chronic pain.
Table 2.
Mindfulness measures results for meditation and control group
| Baseline |
Post Program |
4 month |
||||
|---|---|---|---|---|---|---|
| Measure | Meditation Group n = 16 | Control Group n = 19 | Meditation Group n = 16 | Control Group n = 19 | Meditation Group n = 16 | Control Group n = 19 |
| Five facet mindfulness questionnaire,* (Mean ± SD) | ||||||
| Observe | 27.8 ± 4.6 | 30.4 ± 5.1 | 27.8 ± 5.2 | 29.7 ± 5.7 | 28.1 ± 4.6 | 31.0 ± 5.3 |
| Describe | 30.6 ± 6.0 | 30.2 ± 5.0 | 29.8 ± 5.6 | 30.1 ± 5.3 | 30.4 ± 5.6 | 29.8 ± 6.0 |
| Act with awareness | 30.0 ± 6.0 | 31.3 ± 4.3 | 29.0 ± 5.1 | 31.6 ± 4.5 | 28.9 ± 6.6 | 32.9 ± 4.9 |
| Nonjudge | 29.2 ± 7.2 | 29.3 ± 6.1 | 27.8 ± 6.4 | 29.4 ± 5.8 | 27.2 ± 6.8 | 29.8 ± 5.7 |
| Nonreact | 22.7 ± 3.3 | 21.5 ± 4.4 | 23.2 ± 3.1 | 23.8 ± 4.3 | 23.3 ± 4.4 | 23.1 ± 4.4 |
| Mindful attention awareness scale,† (Mean ± SD) | 4.4 ± 0.8 | 4.7 ± 0.6 | 4.4 ± 0.6 | 4.7 ± 0.5 | 4.3 ± 0.9 | 4.9 ± 0.6 |
Range 8–40 for each subscale, except nonreact 7–35, higher is better.
Range 1–6, higher is better.
Participants were asked at the completion of the study how much their back pain symptoms had changed as a result of the treatment provided in the study. Both groups noted an improvement in symptoms as a result of the program (see Table 3). Of the 16 people in the meditation group 13 (81%) were at least minimally improved. No one was worse, while in the control group (N = 18), 12 (67%) described themselves as a least minimally improved.
Table 3.
Participant global impression of change
| Intervention (%) n = 16 | Control (%) n = 18 | |
|---|---|---|
| Much improved | 5 (31%) | 2 (11%) |
| Minimally improved | 8 (50%) | 10 (56%) |
| No change | 3 (19%) | 5 (28%) |
| Minimally worse | 1 (5%) |
Treatment expectancy was high in both groups. At baseline, when asked “how successful do you think this program will be in helping you with your back pain problem?” the meditation group’s mean response to this question was 4.63 (range of 0 = not successful to 6 = very successful) and the control group’s was 4.84. At the completion of the 8-week program responses remained high: meditation group 4.65 and control group 4.16.
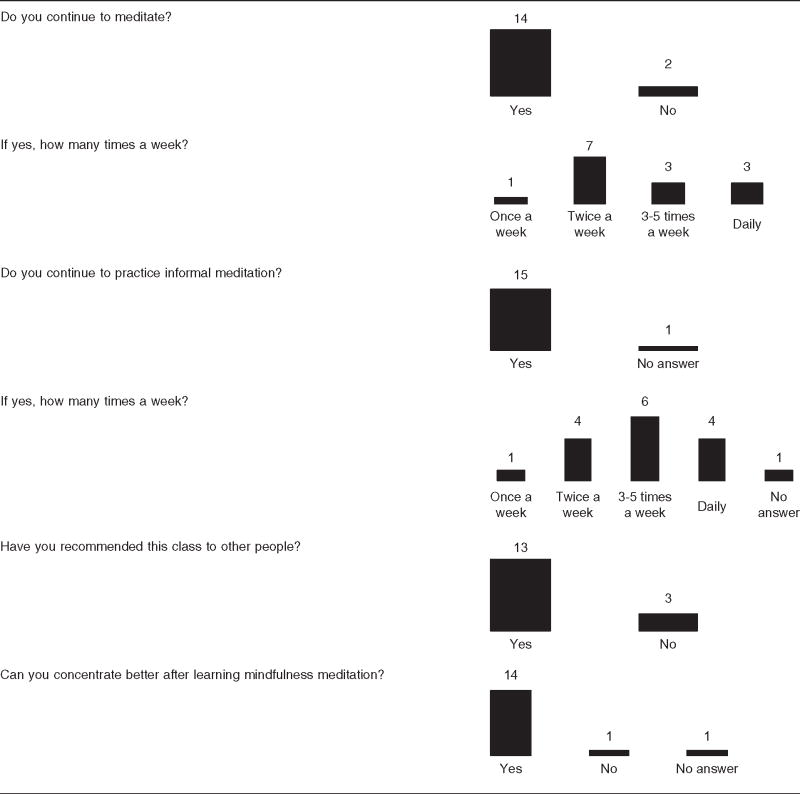
The majority of the older adults in the meditation group continued to meditate four months after program completion (Table 4). The number who practiced formal meditation was 14/16 (88%) and informal meditation was 15/16 (94%).
Table 4.
Practice of meditation four months after program completion, N = 16
 |
There were no adverse events reported.
Discussion
This is the first pilot RCT of mindfulness meditation in older adults with chronic pain to use a health education program as the control group. Both the meditation and control group improved on measures of disability, pain, and self-efficacy suggesting both programs had a beneficial effect. Many of the participants continued to meditate at 4-month follow-up indicating that some participants successfully incorporated meditation into their daily lives.
The control program we implemented was feasible and resulted in high participation (only one drop-out). However, the program was not “inert” and appears to have had an affect on the main outcome measures. Other pain researchers that have used an education control in their RCT have also shown improvement in the control group. In a study of 128 people with fibromyalgia randomized to a mindfulness meditation plus Qigong program vs an education control program, both groups showed improvement in all outcome measures [27]. The education program included topics related to pain, exercise and stress. In another study of 137 patients with rheumatoid arthritis with or without depression randomized into cognitive behavioral therapy (CBT), mindfulness meditation, or an education control program, all groups improved significantly on daily pain scores. Additionally, the CBT and education groups both significantly improved on pain control scores at the end of the 8-week program as compared with the mindfulness group [28]. The education program included topics on treatment, medications, neurophysiology of pain, natural remedies, exercise, and sleep.
Part of the improvement in the control group seen in our and the above studies may have been the result of the positive effects of group support, attention of the instructor, and participant expectations for improvement. In our study, both groups expected to improve as a result of the program (intervention or control) and at the completion of the study 67% of participants in the control group said they had at least minimally improved as a result of the program.
However, there is evidence that simply educating patients about pain independently helps their symptoms. This would mean that we were not implementing an education program that was “inert” but that actually had an effect. A 2004 Cochrane review of back schools for low back pain found that there was moderate evidence for short and intermediate-term improvement on pain and functional status for patients with CLBP [29]. This was especially true for back schools within an occupational setting. Back schools are varied in their intensity, but typically involve education on the anatomy of the back, optimal posture, treatment options, and back exercises. The review was limited by the availability of high quality studies. Given this evidence, it is likely that the educational program we developed had a positive effect on the outcome measures as it included many of the topics taught in back schools. As a result of this finding, RCTs of CLBP should consider implementing a control group that does not involve any education related to pain and the lower back but with enough topics of general interest that would allow recruitment and retention into the study. As mind–body research is still in its infancy careful planning and design of clinical trials is critical to obtain accurate results.
Another explanation for our findings is that an educational intervention is as good as the mindfulness meditation intervention for older adults with chronic pain. While it would be easy to dismiss the value of the mindfulness meditation program in this way we believe it deserves further study because program participants continued to meditate after program completion, suggesting they were receiving benefit from the meditation methods learned. Additionally, qualitative statements made by participants in this study and our previous pilot work provide clues of how mindfulness meditation helps reduce pain, improve physical function, and increase quality of life. Mindfulness methods participants used for pain reduction included distraction away from pain, increased body awareness leading to change in behavior which reduced pain, better pain coping skills, imagery, and direct pain reduction through meditation [30]. One participant in the current study wrote “After the meditation, I felt a sense of well-being, even if I still had pain. The meditation always makes me feel better. Most of the time it helps reduce my pain.” Training participants to uncouple the sensory, emotional, and cognitive responses to pain theoretically explains some but not all of the methods use to reduce pain. Other factors involved such as increased positive affect and physical well-being involved in pain reduction require further study.
Another likely factor explaining our negative findings is the heterogeneity of participant responses. Thus, some participants may have improved in psychological function, others in physical function, and yet others in sleep, resulting in insufficient power to detect small effects. To address these issues the mindfulness meditation program requires further study with large, well-designed clinical trials.
Since both the meditation and control group improved in pain-related disability as measured by the Roland and Morris Disability Questionnaire, the difference between the groups did not reach statistical significance. However, a closer look at the scores from this measure suggest that the minimal improvement seen in the meditation group may have been due to a ceiling effect-meaning that there was not much room for improvement in the RMDQ as the participants in the meditation group were already functioning as well as possible given their chronic pain. This is supported by normative data that have been published for older adults with chronic pain to aid in the interpretation of the RMDQ scores. Mean scores for older adults were around 12 [31]. As the mean score for the meditation group was 8.9, they had significantly less pain interference with function than Nicholas’ normalized group of older adults. The baseline RMDQ score was 12 for both the intervention and wait-list control in our original pilot work and we were able to show a small effect size of 0.35 after trial completion [13], further supporting the likelihood of a ceiling effect for the current study. Given this, future studies of mind–body interventions for chronic pain in older adults should consider a cut-off for eligibility of important outcome measures such as the RMDQ, or the study results risk inconclusive findings.
The trend toward improvement in chronic PSE in the meditation group is notable because self-efficacy has been found to be an important component of treatment response in younger CLBP patients. Self-efficacy has been found to correlate significantly with post-treatment pain ratings, tolerance for physical activities, and use of pain medication [32–34]. This preliminary finding deserves further exploration in future studies as it may be a mediator of treatment response.
Among meditation researchers there is an interest in identifying the minimal amount of meditation that can have a beneficial health effect. Yet in working with a chronic pain population the traditional 8-week mindfulness meditation program may be too short to see a lasting effect. The idea that it may take time to successfully implement meditation for health benefits is not new. Included in instructions for meditation (regardless of tradition), is the emphasis on regular meditation practice [35]. This is because it takes time to develop familiarity with meditation, and proficiency and beneficial effects are presumed to take time to occur. Yet mindfulness meditation studies typically focus on results from a brief 8-week MBSR program, which in and of itself is only an introduction to meditation. Acknowledging this, most MBSR programs offer regularly scheduled (e.g., monthly) “booster” classes. Empirical studies that have followed participants with chronic disorders over time show support for this idea. Teasdale and Ma have shown that mindfulness-based cognitive therapy in nondepressed patients with a history of three or more episodes of depression reduced relapse by 39% and 42%, respectively at 12 months after program completion as compared with a treatment-as-usual group [36]. Pradhan in her study of MBSR for patients with rheumatoid arthritis found no statistically significant changes at program completion, but did find statistical significance for measures of psychological distress and well-being at 6 months, compared with a wait-list control group [37]. Expecting chronic pain patients to show significant improvement after just 8 weeks may not be realistic. While anecdotally there were participants who had clinically significant improvement in their pain and function in our study, to see beneficial effects in a larger population of chronic back pain patients may take more time.
Brief mention of the results of the mindfulness scales used in this study is worthwhile because the baseline scores of mindfulness in this cohort of older adults (age ≥65 years) were high. Whether looking at normative data for the MAAS or FFMQ, our participants scored at the level of experienced meditators at baseline [25,26]. There are a variety of reasons that this may be the case, such as demographic characteristics of our sample which were well-educated and white. However, validation studies for these mindfulness measures have not been done in older adults, and our results may indicate that generally, older adults are more mindful than a younger population. As this may be the case, mindfulness measures need to be validated in an older population.
Many of the limitations of the study have already been touched upon in the above discussion, including the small sample size and the modest scores on the RMDQ indicating the meditation group was fairly high functioning. The sample was also predominantly white and well-educated limiting generalizability.
In conclusion, an 8-week mindfulness meditation program for older adults with chronic pain and an education control group both showed improvement at program completion on measures of pain, and physical and psychological function. Our results have important implications for the design of clinical trials in mind–body research including the importance of piloting the control group before running a large clinical trial, and inclusion or exclusion criteria that considers cutoffs of important outcome measures for participant inclusion into the trial. Careful attention to these details will help move meditation research on pain forward to more definitively answer the question of its effectiveness as an adjunct treatment for CLBP in older adults.
Acknowledgments
During the time of this work Dr. Morone was funded by the NIH Roadmap Multidisciplinary Clinical Research Career Development Award Grant (1KL2RR024154-04) from the National Institutes of Health (NIH). This publication was also made possible by Grant Number UL1RR024153 from the National Center for Research Resources (NCRR), a component of the NIH and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Special thanks to Daniel Schenck, DC for co-teaching the mindfulness meditation program and to Vinny Losasso for assistance in data collection and preparation of the manuscript.
Footnotes
There are no financial or other conflicts of interests to declare by Drs. Morone, Rollman, Moore, Qin or Weiner.
References
- 1. [accessed September 2008];Number of older Americans. Available at: http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2008_Documents/Population.aspx.
- 2.Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;7:417–31. doi: 10.1016/s0749-0690(05)70078-1. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–99. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 4.Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24:1813–19. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 5.Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: Are we utilizing healthcare resources wisely? Pain Med. 2006;7:143–50. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 6.Scudds RJ, Mc DRJ. Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain. 1998;75:229–35. doi: 10.1016/s0304-3959(97)00224-8. [DOI] [PubMed] [Google Scholar]
- 7.Walt R, Katschinski B, Logan R, Ashley J, Langman M. Rising frequency of ulcer perforation in elderly people in the United Kingdom. Lancet. 1986;1:489–92. doi: 10.1016/s0140-6736(86)92940-5. [DOI] [PubMed] [Google Scholar]
- 8.Shorr RI, Griffin MR, Daugherty JR, Ray WA. Opioid analgesics and the risk of hip fracture in the elderly: Codeine and propoxyphene. J Gerontol. 1992;47:M111–15. doi: 10.1093/geronj/47.4.m111. [DOI] [PubMed] [Google Scholar]
- 9.Ospina M, Bond T, Karkhaneh M, et al. Evidence Report/Technology Assessment No. 155. (Prepared by the University of Alberta Evidence-based Practice Center under Contract No. 290-02-0023.) AHRQ Publication No. 07-E010. Rockville, MD: Agency for Healthcare Research and Quality; 2007. Meditation Practices for Health: State of the Research; p. 10. [Google Scholar]
- 10.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clin Psychology Sci Pract. 2003;10:144–56. [Google Scholar]
- 11.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychology. 2006;62:373–86. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Delacorte; 1990. [Google Scholar]
- 13.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: A randomized controlled pilot study. Pain. 2008;134:310–19. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roland M, Morris R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–4. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Rejeski WJ, Fielding RA, Blair SN, et al. The lifestyle interventions and independence for elders (LIFE) pilot study: Design and methods. Contemp Clin Trials. 2005;26:141–54. doi: 10.1016/j.cct.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 16.LIFE Study Investigators. Pahor M, Blair SN, et al. Effects of a physical activity intervention on measures of physical performance: Results of the Lifestyle Interventions and Independence for Elders pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1157–65. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 17.Katz LC, Rubin M. Keep Your Brain Alive. New York: Workman Publishing Company; 1999. [Google Scholar]
- 18.Dunn KM, Cherkin DC. The Roland-Morris Disability Questionnaire. Spine. 2007;32:287. doi: 10.1097/01.brs.0000249551.00481.3d. [DOI] [PubMed] [Google Scholar]
- 19.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 20.Weiner D, Pieper C, McConnell E, Martinez S, Keefe F. Pain measurement in elders with chronic low back pain: Traditional and alternative approaches. Pain. 1996;67:461–7. doi: 10.1016/0304-3959(96)03150-8. [DOI] [PubMed] [Google Scholar]
- 21.Anderson KO, Dowds BN, Pelletz RE, Edwards WT, Peeters-Asdourian C. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain. 1995;63:77–84. doi: 10.1016/0304-3959(95)00021-J. [DOI] [PubMed] [Google Scholar]
- 22.Rudy TE, Weiner DK, Lieber SJ, Slaboda J, Boston JR. The impact of chronic low back pain on older adults: A comparative study of patients and controls. Pain. 2007;131:293–301. doi: 10.1016/j.pain.2007.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hays RD, Prince-Embury S, Chen H. RAND-36 Health Status Inventory. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- 24.Andresen EM, Bowley N, Rothenberg BM, Panzer R, Katz P. Test-retest performance of a mailed version of the Medical Outcomes Study 36-Item Short-Form Health Survey among older adults. Med Care. 1996;34:1165–70. doi: 10.1097/00005650-199612000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 26.Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–42. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 27.Astin JA, Berman BM, Bausell B, et al. The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: A randomized controlled trial. [see comment] J Rheumatol. 2003;30:2257–62. [PubMed] [Google Scholar]
- 28.Zautra AJ, Davis MC, Reich JW, et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J Consult Clin Psychol. 2008;76:408–21. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]
- 29.Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev. 2004:CD000261. doi: 10.1002/14651858.CD000261.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. “I felt like a new person” the effects of mindfulness meditation on older adults with chronic pain: Qualitative narrative analysis of diary entries. J Pain. 2008;9:841–8. doi: 10.1016/j.jpain.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicholas MK, Asghari A, Blyth FM. What do the numbers mean? Normative data in chronic pain measures. Pain. 2008;134:158–73. doi: 10.1016/j.pain.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 32.Dolce JJ, Crocker MF, Moletteire C, Doleys DM. Exercise quotas, anticipatory concern and self-efficacy expectancies in chronic pain: A preliminary report. Pain. 1986;24:365–72. doi: 10.1016/0304-3959(86)90122-3. [DOI] [PubMed] [Google Scholar]
- 33.Kores RC, Murphy WD, Rosenthal TL, Elias DB, North WC. Predicting outcome of chronic pain treatment via a modified self-efficacy scale. Behav Res Ther. 1990;28:165–9. doi: 10.1016/0005-7967(90)90029-i. [DOI] [PubMed] [Google Scholar]
- 34.Dolce JJ. Self-efficacy and disability beliefs in behavioral treatment of pain. Behav Res Ther. 1987;25:289–99. doi: 10.1016/0005-7967(87)90007-6. [DOI] [PubMed] [Google Scholar]
- 35.Ospina MB, Bond K, Karkhaneh M, et al. Meditation practices for health: State of the research. Evid Rep/Technol Assess. 2007:1–263. [PMC free article] [PubMed] [Google Scholar]
- 36.Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004;72:31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- 37.Pradhan EK, Baumgarten M, Langenberg P, et al. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis Rheum. 2007;57:1134–42. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]