Abstract
Objective: To evaluate the effect of heparin on duration of catheter patency and on prevention of complications associated with use of peripheral venous and arterial catheters.
Design: Critical appraisal and meta-analysis of 26 randomised controlled trials that evaluated infusion of heparin intermittently or continuously. Thirteen trials of peripheral venous catheters and two of peripheral arterial catheters met criteria for inclusion.
Main outcome measures: Data on the populations, interventions, outcomes, and methodological quality.
Results: For peripheral venous catheters locked between use flushing with 10 U/ml of heparin instead of normal saline did not reduce the incidence of catheter clotting and phlebitis or improve catheter patency. When heparin was given as a continuous infusion at 1 U/ml the risk of phlebitis decreased (relative risk 0.55; 95% confidence interval 0.39 to 0.77), the duration of patency increased, and infusion failure was reduced (0.88; 0.72 to 1.07). Heparin significantly prolonged duration of patency of radial artery catheters and decreased the risk of clot formation (0.51; 0.42 to 0.61).
Conclusions: Use of intermittent heparin flushes at doses of 10 U/ml in peripheral venous catheters locked between use had no benefit over normal saline flush. Infusion of low dose heparin through a peripheral arterial catheter prolonged the duration of patency but further study is needed to establish its benefit for peripheral venous catheters.
Key messages
Despite almost universal use, agreement has not been reached on the need to administer heparin through peripheral intravascular catheters
The results of 13 trials on peripheral venous catheters and two trials on peripheral arterial catheters were critically appraised to clarify what evidence supports the use of heparin
Flushing peripheral venous catheters locked between use with heparinised saline at 10 U/ml is no more beneficial than flushing with normal saline
Heparin significantly prolongs the duration of peripheral arterial catheter patency and decreases the risk of clot formation
In peripheral venous catheters heparin added to the infusion at 1 U/ml decreases phlebitis and may prolong duration of catheter patency and decrease infusion failure
Introduction
Almost all patients admitted to hospital require a peripheral intravenous catheter to provide access for administration of drugs and fluids and parenteral nutrition. In addition, many critically ill patients require arterial catheterisation for haemodynamic monitoring and blood sampling. Maintenance of the patency of these indwelling catheters is important for minimising patients’ discomfort and the expense associated with replacement. Vascular thrombosis,1 visible scarring, and infection related to the catheter2 are complications associated with use of these indwelling vascular devices.
The anticoagulant properties of heparin led clinicians to use heparin flushes or heparinised infusion in an attempt to prevent thrombus formation and to prolong the duration of catheter patency. The effective dose of heparin, however, has not been clearly established for venous and arterial catheters. Two meta-analyses evaluating use of heparin flush solutions for peripheral intermittent infusion devices concluded that the effect of heparin flushes was equivalent to that of 0.9% sodium chloride flushes. Both meta-analyses combined the results of controlled and uncontrolled trials.3,4 Goode et al included 17 studies (seven randomised controlled trials)3 and Peterson et al included 20 studies (three randomised controlled trials).4 Peterson et al combined trials that evaluated continuous infusion of heparinised solution with trials that assessed intermittent flushing in catheters locked between use.4 None the less, these results led some organisations to state that sodium chloride injection should be the standard of care for maintaining intravenous catheters used for peripheral intermittent infusion.5
Despite its beneficial antithrombotic effects, decreasing unnecessary exposure to heparin is important to minimise the complications resulting from sensitisation. Autoimmune mediated thrombocytopenia induced by heparin occurs in about 3% of patients exposed to unfractionated heparin, which greatly increases the risk of thrombotic events.6,7 Heparin induced thrombocytopenia is a risk even in newborns.8 Other risks of heparin use include allergic reactions and the potential for bleeding complications after multiple, unmonitored heparin flushes.5
A large percentage of heparin exposure in patients in hospital is through heparin use in peripheral venous catheters. If the risks associated with heparin use are considered what is the benefit of using heparin in peripheral venous or arterial access devices? Individual trials of heparin in peripheral venous catheters are contradictory, and there are no systematic reviews assessing various heparin dosing strategies for arterial catheters. We therefore conducted this systematic review to resolve and synthesise the conflicting literature. We have critically appraised the clinical trials evaluating use of heparin in continuous and intermittent infusion solutions on the duration of patency of peripheral venous and arterial catheters and on phlebitic complications.
Methods
Study identification
Trials included in this review were identified by cross referencing the following MeSH terms from Medline from 1966 to April 1997: “catheterisation” and “catheters, indwelling” and “heparin” with “randomisation,” “random allocation,” “randomised controlled trial(s), randomised response technique,” and “(controlled) clinical trials, randomised.” Embase was searched from 1974 through 1996 by using the search terms “catheter” and “catheterisation, intravascular, random,” and “heparin.” After examining the full manuscripts of all abstracts deemed potentially relevant we reviewed the reference lists of each retrieved article and obtained the manuscript of any reference considered to be a randomised controlled trial. The trials included in two meta-analyses3,4 were retrieved. Package inserts from catheter kits were searched for references regarding published and unpublished data. We also contacted companies manufacturing heparin bonded catheters regarding other unpublished and published randomised controlled trials. In addition, we hand searched the National Intravenous Therapy Association Journal from 1985 to 1992.
Study selection
The following selection criteria were used to identify studies for inclusion in this analysis: study design—randomised controlled clinical trial; population—adult or paediatric patients; intervention—heparin infused through the catheter via intermittent or continuous flush versus a control group with no heparin; outcomes—catheter patency, catheter related phlebitis, catheter thrombus, infusion failure.
We excluded studies in which over 40% of patients were excluded from analysis after randomisation.
Data abstraction
Data abstraction was conducted by two investigators; disagreement was resolved by consensus. To evaluate agreement we calculated a quadratic weighted κ for each item. Data on the number of catheters or the numbers of patients, or both, were abstracted in the form in which they were reported. Catheters were the unit of analysis when data were pooled because this was the way that most results were reported. We tried to contact authors to provide further information when the data necessary for critical appraisal or analysis, or both, were missing or unclear.
Definitions
The following definitions of terms were used. Duration of catheter patency was the number of hours the catheters were in place. Loss of patency was removal of the catheter because of inability to flush it. Catheter thrombus referred to a clot adherent to or occluding the catheter. Catheter related phlebitis indicated the presence of any one or more of the following: pain, erythema, induration, or a palpable venous cord at the catheter site. Infusion failure was loss of patency, phlebitis, or infiltration resulting in premature removal of the catheter.
Data analysis
We combined data to estimate the relative risks and associated 95% confidence intervals across studies by using the DerSimonian and Laird random effects model.9 We tested for heterogeneity (major differences in the apparent effect of the interventions across studies) by using the method proposed by Fleiss.9 We have reported tests of heterogeneity of variance in the results only when they were significant (P<0.05).
A priori we decided to analyse the data in clinically relevant categories on the basis of similar heparin dosing strategies when sufficient data were available. This was possible for heparin flush of peripheral intravenous catheters at the most common dose of 10 U/ml and at 100 U/ml used intermittently at a minimum of 6 to 12 hour intervals. We separately examined the effect of adding 1 U/ml of heparin to continuous infusions. Because heparin bonding is only on the outside of some catheters and lasts from 30 minutes to 48 hours depending on the type of bonding used (personal communications, technical support staff, Cook, Arrow, Medcomp, Abbott, and Baxter catheter manufacturing companies) we excluded trials of heparin bonding.
Results
Study identification and selection
Twenty six trials of heparin use in peripheral venous catheters were identified in which random assignment was used, and 13 were included—12 published trials10–21 and one unpublished (FD Craig and SR Anderson, Harrison Methodist Fort Worth Hospital, personal communication). Two trials of heparin use in peripheral arterial catheters were identified in which random assignment was used and both were included.22,23 Three trials claiming random allocation that actually used alternate assignment or assignment by odd-even hospital number were excluded.24–26 Five trials were excluded that randomised by hospital unit or wards instead of individual patient because only two units were randomised and a before-after design was applied within each unit.27–31 One randomised study was excluded because all patients received 5000 U heparin subcutaneously for prophylaxis of deep venous thrombosis.32 Three randomised studies were excluded because more than 40% of observations were not reported after randomisation.33–35 One randomised study was excluded because only half the patients were randomised and the rest were allocated to treatment arms at the discretion of the physician.36 The authors of one unpublished trial were unable to provide the necessary primary data (N Bell, D Brown, L Poon, Eden Hospital Medical Centre, California, personal communication). One randomised trial of peripheral venous catheters was performed in patients treated with cephalothin37 and another was done in patients receiving a lignocaine infusion,38 both of which are associated with higher rates of phlebitis leading us to exclude these trials from our analysis. We were unable to include the results of one unpublished randomised study because they reported the number of events per patient, many of whom had more than one catheter, and the primary author could not re-extract the data (A Kasparek, J Wenger, R Feldt, Mercy Medical Centre, Iowa, personal communication).
Trial characteristics and assessment of quality
The populations, interventions, number of patients, number of catheters, catheter gauges used, and methodological characteristics of the studies included in the final analysis are described in table 1. For peripheral venous catheters, intermittent heparin flushes varied from 10 U/ml to 100 U/ml and continuous heparin infusion was 1 U/ml. In the trial by Moclair et al all patients received a glyceryl trinitrate transdermal patch and twice daily application of hydrocortisone cream to the infusion site in an attempt to prolong vein survival and decrease phlebitis.10 The doses of heparin used in trials evaluating continuous flush in arterial catheters varied, and the actual dose was not reported in the largest trial as it was an effectiveness study of any amount of heparin versus no heparin.23
Table 1.
Study design of randomised trials of heparin infusion and bonding
| Author | Population | Heparin |
Catheters
|
Methods
|
|||
|---|---|---|---|---|---|---|---|
| No | Gauge | Blinding | Exclusion (%) * | ||||
| Peripheral venous catheters | |||||||
| Kleiber et al, 199311 | 124 Infants and children | 10 U every 6 hours† | 124 | 22,24 | Double | 2% | |
| Craig et al, 1991‡ | 173 Adults, medical | 10 U every 8 hours† | 274 | 18-22 | Double | 0 | |
| Shoaf et al, 199212 | 260 Adults, cardiac surgery | 10 U every 8 hours† | 260 | NA | Double | 15% | |
| Ashton et al, 199014 | 32 Adults, intensive care unit | 10 U every 12 hours | 321 | 8-22 | Double | 0 | |
| Hamilton et al, 198815 | 241 Adults, medical-surgical | 100 U every 8 hours† | 307 | 18-22 | Double | 34% | |
| Meyer et al, 199516 | 65 Adults, obstetric | 100 U every 6 hours† | 65 | 18 | Double | 2% | |
| Daniell et al, 197317 | 166 Adults, coronary care | 1 U/ml infused | 221 | 18 | Double | 9% | |
| Alpan et al, 198418 | 826 Neonates, intensive care unit | 1 U/ml infused | 227 | 22 | Double | 0 | |
| Wright et al, 199520 | 80 Children, medical | 1 U/ml infused | 80 | 22, 24 | Double | 0 | |
| Moclair et al, 199110 | 16 Adults, surgical | 1 U/ml infused | 16 | 18 | Double | 0 | |
| Sketch et al, 197221 | Adults, coronary care | 1 U/ml infused | 239 | NA | Double | NA | |
| Messing et al, 198519 | 65 Adults, medical-surgical | 1 U/ml infused | 65 | NA | Double | 0 | |
| Tanner et al, 198013 | 72 Adults, surgical | 1 U/ml infused | 72 | NA | None | 0 | |
| Peripheral arterial catheters | |||||||
| Clifton et al, 199122 | 30 Adults, intensive care unit | 4 U/ml normal saline | 30 | 20 | Double | 0 | |
| AACC Nurses, 199323 | 5139 Adults, medical-surgical | Variable | 5139 | 18-22 | None | 2% | |
Patients excluded after randomisation; catheters included in analysis after randomisation.
Flush solution (control or heparin) used after medications in addition to or in place of scheduled flush.
Craig FD, Anderson SR. Comparison of normal saline versus heparinised saline in the maintenance of intermittent infusion devices. Harrison Methodist Fort Worth Hospital. Unpublished.
NA=data not available.
Four trials evaluated multiple catheter insertions in a single patient. Two of these trials evaluated intermittent heparin flushes at 10 U every 8 hours (FD Craig and SR Anderson, Harrison Methodist Fort Worth Hospital, personal communication) and 100 U every 8 hours15 with 274 catheters in 173 patients and 307 catheters in 241 patients, respectively. The other two trials evaluated use of 1 U of heparin per ml of infusion with 226 catheters in 26 neonates18 and 221 catheters in 166 adult patients.17 Three trials were in infants and children11,18,20 and 12 were in adult patients.
Design features and methodological characteristics of the 15 published studies included in this review are described in table 1. Agreement regarding data abstraction was good (quadratic weighted κ of 0.72 to 1.00).
Duration of catheter patency
Table 2 shows the effect of heparin on duration of catheter patency in six trials. We were unable to pool the results because of differences in reporting. The two trials of intermittent heparin flushes at concentrations of 10 U/ml11 and 100 U/ml15 showed no effect on duration of catheter patency. Two trials showed that heparin added to the infusion to make a concentration of 1 U/ml effectively prolonged peripheral venous catheter patency18,20 and two trials showed non-significant trends in the direction of benefit.10,17 The results could not be pooled because not all investigators reported the standard deviation around the mean and some reported the median. In peripheral arterial catheters, heparin significantly prolonged the duration of catheter patency in two trials,22,23 although investigators reported the percentage of catheters patent at 72 hours (4 U/ml normal saline; 90% of heparin catheters v 79% of control catheters; difference 11%; P<0.0523) and 96 hours (variable dose; 86% v 52%; difference 34%; P<0.0122) and not the average number of hours catheters were patent.
Table 2.
Effect of heparin on duration of peripheral venous catheter patency. Figures are means with or without SD unless stated otherwise
| Author | Heparin | Patency duration (hours)
|
Difference (hours) for heparin − control | |
|---|---|---|---|---|
| Heparin | Control | |||
| Kleiber et al, 199311 | 10 U every 6 hours* | 38.2 (40) | 35.4 (30) | 2.8 |
| Hamilton et al, 198815 | 100 U every 8 hours* | 44.3 (19) | 45.4 (18) | −0.9 |
| Daniell et al, 197317 | 1 U/ml infused | 88.5 | 57.6 | 30.9 |
| Alpan et al, 198418 | 1 U/ml infused | 58.7 (45) | 26.1 (20) | 32.6† |
| Wright et al, 199520 | 1 U/ml infused | 97‡ | 43‡ | 54.0† |
| Moclair et al, 199110 | 1 U/ml infused | 69‡ | 31‡ | 38.0 |
Flush solution (control or heparin) used after medications in addition to or in place of scheduled flush.
Authors report P<0.05.
Medians.
Catheter clotting and loss of patency
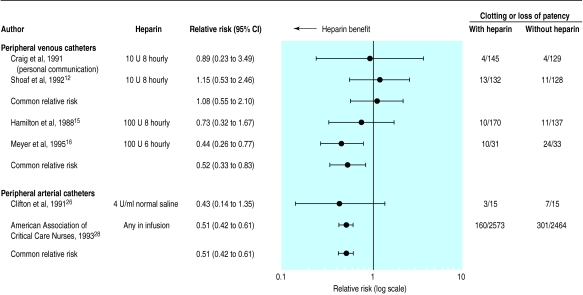
Figure 1 shows that use of 10 U intermittent heparin flushes had no effect on catheter clotting compared with normal saline when the results of two trials were pooled (FD Craig and SR Anderson, Harrison Methodist Fort Worth Hospital, personal communication, and Shoaf and Oliver12). At doses of 100 U/ml flushed every 6 or 8 hours heparin was associated with a significantly lower loss of catheter patency when the results of two trials were pooled.15,16 Heparinised infusion significantly decreased loss of patency in arterial catheters when the results of two trials were pooled.22,23
Figure 1.
Relative risks (95% confidence intervals) for catheter clot formation in and loss of patency of peripheral venous and arterial catheters according to treatment with or without heparin. Last two columns are numbers of catheters with clots/total number of catheters
Infusion failure
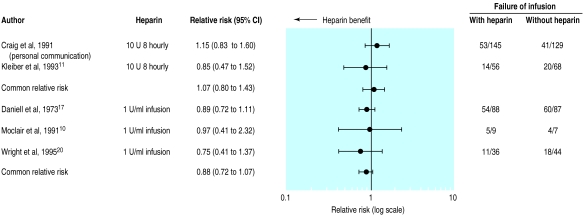
Figure 2 shows that use of intermittent 10 U heparin flushes had no effect on infusion failure rates for peripheral intravenous catheters when the results of two trials were pooled (FD Craig and SR Anderson, Harrison Methodist Fort Worth Hospital, personal communication, and Shoaf and Oliver12). Addition of heparin at a concentration of 1 U/ml to the infusion was associated with a reduced risk of infusion failure when the results of three trials were pooled.10,17,20
Figure 2.
Relative risks (95% confidence intervals) for failure of infusion in peripheral venous catheters according to treatment with or without heparin. Last two columns are numbers of catheters with failure of infusion/total number of catheters
Catheter related phlebitis
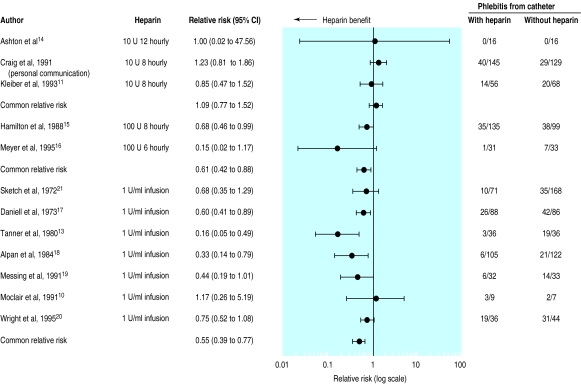
Figure 3 shows that there was a significant difference in the risk of phlebitis when the results of three trials of 10 U/ml intermittent heparin flushes versus normal saline were pooled (FD Craig and SR Anderson, Harrison Methodist Fort Worth Hospital, personal communication).11,14 When the results of two trials of 100 U/ml of intermittent heparin flush were pooled phlebitis was significantly decreased.15,16 The test of homogeneity, however, was significant (P=0.0006) for the decreased risk of phlebitis, with one trial that used 100 U/ml every 6 hours16 showing a much larger but non-significant trend in the direction of heparin being beneficial than the trial that used 100 U/ml every 8 hours.15 When the data from seven trials of heparin at concentrations of 1 U/ml infusion flushed continuously through the catheter were pooled (see figure 2) there was a significant decrease in phlebitis with use of heparin.
Figure 3.
Relative risks (95% confidence intervals) of phlebitis from peripheral venous catheters according to treatment with or without heparin. Last two columns are numbers of catheters associated with phlebitis/total number of catheters
Discussion
Use of heparin as an antithrombotic agent in catheters has been widespread for over 20 years. Despite almost universal use, the benefit of heparin has not been firmly established. Half of the available trials claiming to be randomised had to be excluded because of quality considerations or the presence of potentially confounding cointerventions. The evidence supporting use of heparin in peripheral arterial catheters comes mainly from one large (5139 patients) randomised trial including 198 sites in which various heparin dosing strategies were used.23 The limited evidence available suggests that use of heparin as an intermittent flush solution at a concentration of 10 U/ml in catheters locked between episodes of use is not beneficial. Use of heparin in peripheral arterial catheters will prolong their life and utility. Current evidence does not allow us to make firm conclusions regarding the benefit of adding heparin to the solutions infused continuously through peripheral venous catheters, but this intervention warrants further study.
Use of heparin in peripheral venous catheters
Our meta-analyses included three randomised controlled trials of intermittent heparin flushes and seven randomised controlled trials of continuous infusion of heparinised solution that were not included in the two previously published meta-analyses.3,4 Our finding that heparin at doses if 10 U/ml for intermittent flushing is no more beneficial than flushing with normal saline alone is in agreement with the results of these meta-analyses, which combined controlled and uncontrolled studies.3,4 This intervention has been evaluated in only four truly randomised controlled, double blind trials including a total of 652 catheters. These trials involved different populations and evaluated different outcomes. Added to the larger number of uncontrolled studies, however, the weight of the evidence supports discontinuation of use of 10 U/ml heparin flush in intermittent intravenous infusion devices.
Heparin at 100 U/ml used as an intermittent flush solution in locked catheters may increase catheter patency and may decrease catheter related phlebitis. The usual heparin dose of 10 U/ml was established from a study in dogs,39 and, although later studies confirmed the safety of this dose, the efficacy in maintaining catheter patency was not established. The safety and efficacy of heparin concentrations of 100 U/ml used as an intermittent flush needs further study on a wider variety of patients; the study showing a significant benefit for increasing patency and decreasing phlebitis was in obstetric patients with 18 gauge catheters for serial phlebotomy16 and the other trial in a more variable population of adult medical patients lost 34% during follow up.15
Phlebitis is associated with duration of catheter patency because red inflamed catheter sites lead to early discontinuation. Continuously infused heparinised solutions may prolong patency because they significantly decrease the risk of phlebitis. The type of solution being infused is related to the risk of phlebitis. In newborn infants with 24 gauge catheters the duration of catheter patency is prolonged, and infiltration rates are decreased with use of 10 U/ml heparin in normal saline in catheters locked between use versus 10% dextrose by continuous infusion (no added heparin).40 Regular changing of the catheter has been advocated as an intervention to prevent phlebitis and clot formation, but in adult patients changing the heparin lock every 72 hours was shown to be of no benefit compared with leaving the catheter in place for up to 168 hours.41
Use of heparin in peripheral arterial catheters
Mostly on the basis of the results of one multicentre study heparin has been shown effectively to prolong the life of peripherally placed arterial pressure monitoring devices. The minimal effective dose of heparin, however, has not been established. Bolgiano et al reported no significant difference in duration of arterial catheter patency when heparin was used at 0.25 U/ml versus 1 U/ml in adults.42 Butt et al reported that increasing the heparin concentration from 1 U/ml to 5 U/ml in 22 gauge catheters in children significantly prolonged arterial catheter patency.43 The type of solution, however, may be important as Rais-Bahrami et al reported that neonatal peripheral arterial lines infused continuously with heparinised normal saline functioned significantly longer (107 (SD 71) hours) than those with heparinised 5% dextrose (39 (32) hours).44 Other agents besides heparin have also been shown to be effective in prolonging the duration of patency of radial arterial catheters. Arterial catheter solutions containing papaverine45 and 1.4% sodium citrate46 effectively prolong the duration of catheter patency and their risk profile should be compared with that of heparin.
Conclusions
In this systematic review we have clarified that low dose heparin is beneficial for maintaining peripherally placed arterial catheters when added to the continuously infused solutions. Heparin at a concentration of 1 U/ml infused continuously through peripheral venous catheters is a promising intervention to prolong catheter life but requires further study. While the use of 100 U/ml of intermittent heparin flushes for peripheral intravenous catheters needs further evaluation, evidence currently available suggests that the current use of 10 U/ml as an intermittent flush is no more effective than normal saline flush.
Acknowledgments
We thank Derek King for statistical assistance. DJC is a career scientist of the Ontario Ministry of Health.
Footnotes
Funding: National Research Service Award F32 HS00106-01 from the Agency for Health Care Policy and Research (AGR).
Conflict of interest: None.
References
- 1.Gauer PK, Downs JB. Complications of arterial catheterization. Respir Care. 1982;27:435–444. [Google Scholar]
- 2.Shinozaki T, Deane RS, Mazuzan JE, Hamel AJ, Hazelton D. Bacterial contamination of arterial lines. A prospective study. JAMA. 1983;249:223–225. [PubMed] [Google Scholar]
- 3.Goode CJ, Titler M, Rakel B, Ones DS, Kleiber C, Small S et al. A meta-analysis of effects of heparin flush and saline flush: quality and cost implications. Nurs Res 1991;40:324-30. [PubMed]
- 4.Peterson FY, Kirchhoff KT. Analysis of the research about heparinized versus nonheparinized intravascular lines. Heart Lung. 1991;20:631–640. [PubMed] [Google Scholar]
- 5.American Society of Hospital Pharmacists. ASHP therapeutic position statement on the institutional use of 0.9% sodium chloride injection to maintain the patency of peripheral indwelling intermittent infusion devices. Am J Hosp Pharm. 1994;51:1572–1574. [PubMed] [Google Scholar]
- 6.Brismar B, Hardstedt C, Jacobson S, Kager L, Malmborg A-S. Reduction of catheter-associated thrombosis in parenteral nutrition by intravenous heparin therapy. Arch Surg. 1982;117:1196–1199. doi: 10.1001/archsurg.1982.01380330054013. [DOI] [PubMed] [Google Scholar]
- 7.Warkentin TE, Levine MN, Hirsh J, Horsewood P, Roberts RS, Gent M, et al. Heparin-induced thrombocytopenia in patients treated with low-molecular weight heparin or unfractionated heparin. N Engl J Med. 1995;332:1330–1335. doi: 10.1056/NEJM199505183322003. [DOI] [PubMed] [Google Scholar]
- 8.Spadone D, Clark F, James E, Laster J, Hoch J, Silver D. Heparin-induced thrombocytopenia in the newborn. J Vasc Surg. 1992;15:306–312. doi: 10.1067/mva.1992.33807. [DOI] [PubMed] [Google Scholar]
- 9.Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2:121–145. doi: 10.1177/096228029300200202. [DOI] [PubMed] [Google Scholar]
- 10.Moclair AE, Moselhi M, Benjamin IS, Hecker JF. Total parenteral nutrition via a peripheral vein: a comparison of heparinized and non-heparinized regimens. Int J Pharm Pract. 1991;1:38–40. [Google Scholar]
- 11.Kleiber C, Hanrahan K, Fagan CL, Zittergruen MA. Heparin vs saline peripheral IV locks in children. Pediatr Nurs. 1993;19:405–409. [PubMed] [Google Scholar]
- 12.Shoaf J, Oliver S. Efficacy of normal saline injection with and without heparin for maintaining intermittent intravenous site. Appl Nurs Res. 1992;5:9–12. doi: 10.1016/s0897-1897(05)80077-1. [DOI] [PubMed] [Google Scholar]
- 13.Tanner WA, Delaney PV, Hennessy TP. The influence of heparin on intravenous infusions: a prospective study. Br J Surg. 1980;67:311–312. doi: 10.1002/bjs.1800670503. [DOI] [PubMed] [Google Scholar]
- 14.Ashton J, Gibson V, Summers S. Effects of heparin versus saline solution on intermittent infusion device irrigation. Heart Lung. 1990;19:608–612. [PubMed] [Google Scholar]
- 15.Hamilton RA, Plis JM, Clay C, Sylvan L. Heparin sodium versus 0.9% sodium chloride injection for maintaining patency of indwelling intermittent infusion devices. Clin Pharm. 1988;7:439–443. [PubMed] [Google Scholar]
- 16.Meyer BA, Little CJ, Thorp JA, Cohen GR, Yeast JD. Heparin versus normal saline as a peripheral line flush in maintenance of intermittent intravenous lines in obstetric patients. Obstet Gynecol. 1995;85:433–436. doi: 10.1016/0029-7844(94)00409-7. [DOI] [PubMed] [Google Scholar]
- 17.Daniell HW. Heparin in the prevention of infusion phlebitis. A double blind controlled study. JAMA. 1973;226:1317–1321. [PubMed] [Google Scholar]
- 18.Alpan G, Eyal F, Springer G, Glick B, Groder K, Armon L. Heparinization of alimentation solutions: a controlled study. Pediatrics. 1984;74:375–378. [PubMed] [Google Scholar]
- 19.Messing B. Infusion related phlebitis [letter] N Engl J Med. 1985;312:1432. doi: 10.1056/NEJM198505303122211. [DOI] [PubMed] [Google Scholar]
- 20.Wright A, Hecker J, McDonald G. Effects of low-dose heparin on failure of intravenous infusions in children. Heart Lung. 1995;24:79–82. doi: 10.1016/s0147-9563(05)80099-8. [DOI] [PubMed] [Google Scholar]
- 21.Sketch MH, Cale M, Mohiuddin SM, Booth RW. Use of percutaneously inserted venous catheters in coronary care units. Chest. 1972;62:684–689. doi: 10.1378/chest.62.6.684. [DOI] [PubMed] [Google Scholar]
- 22.Clifton GD, Branson P, Kelly HJ, Dotson LR, Record KE, Phillips BA, et al. Comparison of normal saline and heparin solutions for maintenance of arterial catheter patency. Heart Lung. 1991;20:115–118. [PubMed] [Google Scholar]
- 23.American Association of Critical Care Nurses. Evaluation of the effects of heparinized and nonheparinized flush solutions on the patency of arterial pressure monitoring lines: the AACN thunder project. Am J Crit Care. 1993;2:3–15. [PubMed] [Google Scholar]
- 24.Treas LS, Latinis-Bridges B. Efficacy of heparin in peripheral venous infusion in neonates. J Obstet Gynecol Neonatal Nurs. 1991;21:214–219. doi: 10.1111/j.1552-6909.1992.tb02258.x. [DOI] [PubMed] [Google Scholar]
- 25.Stradling JR. Heparin and infusion phlebitis. BMJ. 1978;ii:1195–1196. doi: 10.1136/bmj.2.6146.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kulkarni H, Elsner C, Ouellet D, Zeldin R. Heparinized saline versus normal saline in maintaining patency of the radial arterial catheter. Can J Surg. 1994;37:37–42. [PubMed] [Google Scholar]
- 27.Danek GD, Noris EM. Pediatric IV catheters: efficacy of saline flush. Pediatr Nurs. 1992;18:111–113. [PubMed] [Google Scholar]
- 28.Epperson EL. Efficacy of 0.9% sodium chloride injection with and without heparin for maintaining indwelling intermittent injection sites. Clin Pharm. 1984;3:626–629. [PubMed] [Google Scholar]
- 29.Barrett PJ, Lester RL. Heparin versus saline flushing solutions in a small community hospital. Hosp Pharm. 1990;25:115–118. [PubMed] [Google Scholar]
- 30.Geritz MA. Saline versus heparin in intermittent infuser patency maintenance. West J Nurs Res. 1992;14:131–137. doi: 10.1177/019394599201400202. [DOI] [PubMed] [Google Scholar]
- 31.Garrelts JC, LaRocca J, Ast D, Smith DF, Sweet DE. Comparison of heparin and 0.9% sodium chloride injection in the maintenance of indwelling intermittent iv devices. Clin Pharm. 1989;8:34–39. [PubMed] [Google Scholar]
- 32.Jowett NI, Stephens JM, Thompson DR, Sutton TW. Do indwelling cannulae on coronary care units need a heparin flush? Intens Care Nurs. 1986;2:16–19. doi: 10.1016/0266-612x(86)90070-2. [DOI] [PubMed] [Google Scholar]
- 33.Donham J, Denning V. Heparin vs saline in maintaining patency of intermittent infusion devices: pilot study. Kansas Nurse. 1987;62:6–7. [PubMed] [Google Scholar]
- 34.McMullen A, Fioravanti ID, Pollack V, Rideout K, Sciera M. Heparinized saline or normal saline as a flush solution in intermittent intravenous lines in infants and children. Am J Matern Child Nurs. 1993;18:78–85. [PubMed] [Google Scholar]
- 35.Kotter RW. Heparin vs saline for intermittent intravenous device maintenance in neonates. Neonatal Network. 1996;15:43–47. [PubMed] [Google Scholar]
- 36.Robertson J. Intermittent intravenous therapy: a comparison of two flushing solutions. Contemp Nurse. 1994;3:174–179. doi: 10.5172/conu.3.4.174. [DOI] [PubMed] [Google Scholar]
- 37.Maddox RR, Rush DR, Rapp RP, Foster TS, Mazella V, McKean HE. Double-blind study to investigate methods to prevent cephalothin-induced phlebitis. Am J Hosp Pharm. 1977;34:29–34. [PubMed] [Google Scholar]
- 38.Bassan MM, Sheikh-Hamad D. Prevention of lidocaine-infusion phlebitis by heparin and hydrocortisone. Chest. 1983;84:439–441. doi: 10.1378/chest.84.4.439. [DOI] [PubMed] [Google Scholar]
- 39.Hanson RL, Grant AM, Majors KR. Heparin-lock maintenance with ten units of sodium heparin in one milliliter of normal saline solution. Surg Gynecol Obstet. 1976;142:373–376. [PubMed] [Google Scholar]
- 40.Taylor J, Shannon R, Kilbride HW. Heparin lock intravenous line. Use in newborn infants. A controlled trial. Clin Pediatr (Phila) 1989;28:237–240. doi: 10.1177/000992288902800509. [DOI] [PubMed] [Google Scholar]
- 41.Smith I, Hathaway M, Goldman C, Ng T, Brunton J, Simor AE, et al. A randomized study to determine complications associated with the duration of heparin locks. Res Nursing Health. 1990;13:367–373. doi: 10.1002/nur.4770130604. [DOI] [PubMed] [Google Scholar]
- 42.Bolgiano CS, Subramaniam PT, Montanari JM, Minick L. The effect of two concentrations of heparin on arterial catheter patency. Crit Care Nurse. 1990;10:47–57. [PubMed] [Google Scholar]
- 43.Butt W, Shann F, McDonnell G, Hudson I. Effect of heparin concentration and infusion rate on the patency of arterial catheters. Crit Care Med. 1987;15:230–232. doi: 10.1097/00003246-198703000-00010. [DOI] [PubMed] [Google Scholar]
- 44.Rais-Bahrami K, Karna P, Dolanski EA. Effect of fluids on the life span of peripheral arterial lines. Am J Perinatol. 1990;7:122–124. doi: 10.1055/s-2007-999461. [DOI] [PubMed] [Google Scholar]
- 45.Heulitt MJ, Farrington EA, O’Shea TM, Stoltzman SM, Srubar NB, Levin DL. Double-blind, randomized, controlled trial of papaverine-containing infusions to prevent failure of arterial catheters in pediatric patients. Crit Care Med. 1993;21:825–829. doi: 10.1097/00003246-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 46.Branson PK, McCoy RA, Phillips BA, Clifton GD. Efficacy of 1.4 percent sodium citrate in maintaining arterial catheter patency in patients in a medical ICU. Chest. 1993;103:882–885. doi: 10.1378/chest.103.3.882. [DOI] [PubMed] [Google Scholar]