Elsewhere in this issue Julian Walters and his colleagues report a major advance in our understanding of the pathogenesis of chronic diarrhea associated with idiopathic bile acid malabsorption.1 The story is a fascinating one and unites long standing and very recent discoveries in physiology, biochemistry, and molecular biology.
Conjugated bile acids are absorbed from the terminal ileum by the combined action of an apical sodium-dependent transporter that takes bile acids into the cell, and a basolateral transporter that takes bile acids out of the cell and into portal venous blood. The ileum was recognized as the preferential site of bile acid absorption by Tappeiner in 18782, and his observations were confirmed repeatedly. In 1960, Lack and Weiner used the everted gut sac technique to show that conjugated bile acids moved uphill, against a concentration gradient, in segments prepared from the distal ileum.3 Expression cloning was used by Paul Dawson and his colleagues to clone the apical sodium dependent bile acid transporter in 1994.4 Seven years later, the heterodimeric basolateral transporter OSTα/OSTβ of the skate hepatocyte was cloned by Ballatori et al5,6 and its essential role in the transport of bile acids across the basolateral membrane of the ileal enterocyte established by Dawson et al.7
Bile acid biosynthesis from cholesterol is under negative feedback control. Interruption of the enterohepatic circulation by a biliary fistula8 or ileal dysfunction9–13 leads to a marked increase in bile acid biosynthesis. Pandak et al made the observation that such upregulated bile acid synthesis could be down regulated by bile acid infusion into the small intestine but not by intravenous infusion.14 This observation was confirmed and extended by a Japanese surgical group who showed that duodenal infusion downregulated bile acid biosynthesis whereas portal venous infusion did not.15 These experiments raised the intriguing possibility that an unknown intestinal factor was released by bile acids and was necessary for feedback inhibition of bile acid synthesis. Ten years later, this intestinal factor was discovered by Inagaki et al to be a protein, fibroblast growth factor-19, an atypical FGF family member that functions as a hormone.16 FGF19 is synthesized in the ileal enterocytes in response to bile acids and released into the portal venous circulation. Upon reaching the liver, FGF19 signals through a cell surface receptor on hepatocytes to repress bile acid synthesis.
Increased bile acid biosynthesis in patients with bile acid malabsorption because of ileal dysfunction meant that more bile acids passed into the colon. A group of studies in animals and humans led by Sidney Phillips at the Mayo showed that colonic perfusion with dihydroxy bile salts induced colonic secretion17,18, and elevated concentrations of fecal bile acids were shown to be present in patients with ileal resection.9–11 The elevated concentrations were the result of greatly increased bile acid synthesis.9–13
It was quite straightforward to combine these findings and predict the sequence of events in patients undergoing ileal resection.19 Defective bile acid absorption led to increased hepatic synthesis. In this new steady state, increased bile acids passed into the colon and induced secretion, manifest clinically as diarrhea. If diarrhea were caused by bile acid induced secretion in the colon, it should respond to a bile acid sequestrant. Indeed, cholestyramine was shown to be effective for the treatment of diarrhea in a small clinical study20 Colesevelam, a more potent bile acid sequestrant, was developed a few years ago and its off label utility in diarrhea associated with bile acid malabsorption has been claimed in anecdotal reports.21 Colesevelam is available in tablet form and appears to be better tolerated than cholestyramine which is marketed as a granular powder.
The diagnosis of bile acid malabsorption has never been simple to establish. One can collect stools for a day or more and measure fecal bile acids by gas chromatography22 or by an enzymatic method23, but fecal bile acid measurement by either method is complex, and patients do not like to collect stool samples. Boyd, a biochemist working in Edinburgh, had the idea of making a taurocholate analogue tagged with a gamma emitting isotope. He worked with colleagues at the Amersham company to introduce a 75selenium atom (a gamma particle emitter) into the side chain of the bile acid (between the 22nd and 23rd carbon atom), and this compound 75Selenohomocholyltaurine, SeHCAT) was shown to behave physiologically like taurocholate.25 In patients with bile acid malabsorption, the compound is lost from the body much more rapidly than in patients without bile acid malabsorption as quantified by whole body scanning with a gamma camera.25–28 However, this valuable diagnostic radionuclide has never been available for clinical purposes in the United States.
A blood test for the detection of bile acid malabsorption would be more convenient. Rudling and Gälman and their Swedish colleagues showed that an intermediate in bile acid synthesis named C4 (actually cholest-4-ene-3-one) spills over from the hepatocyte into plasma in direct proportion to the rate of bile acid synthesis29 When bile acid synthesis was increased, plasma levels of C4 were markedly elevated.30,31
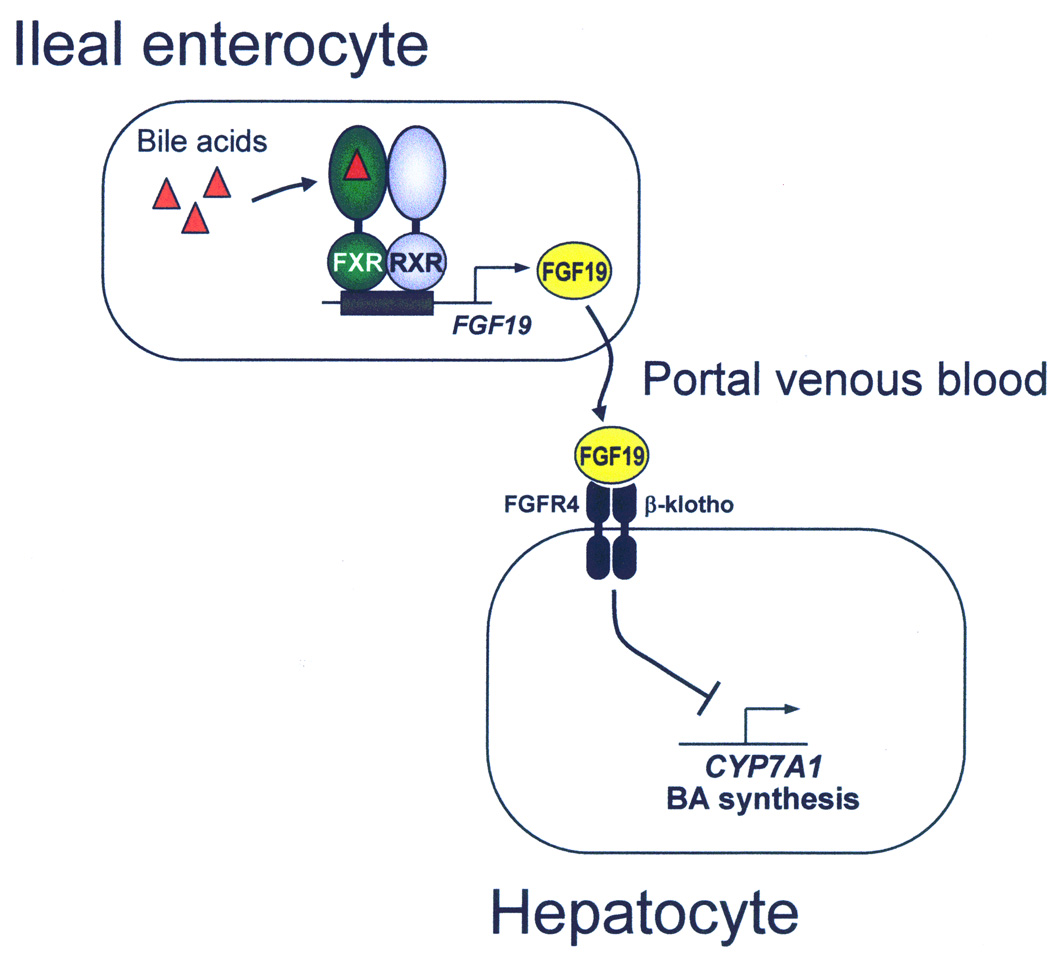
In the meantime, the mechanistic details of the negative feedback regulation of bile acid biosynthesis in the hepatocyte were being clarified.32 An orphan member of the steroid hormone receptor family, named FXR, was discovered to be activated by bile acids and to play a central role in the regulation of bile acid homeostasis.33–36 In the ileum, bile acid-mediated activation of FXR was shown to induce the synthesis and secretion of the hormone FGF19, which subsequently represses bile acid synthesis in hepatocytes by binding to a cell surface receptor comprised of the FGF receptor 4, a tyrosine kinase, and β-klotho, a single pass transmembrane protein.37–39 Activation of the FGF receptor 4/β-klotho complex activates phosphorylation cascades that culminate in the transcriptional repression of the gene encoding cholesterol 7α-hydroxylase, the rate-limiting enzyme in bile acid synthesis16,40,41 In mice, elimination of either FXR, FGF15 (the mouse ortholog of FGF19), FGF receptor 4 or β-klotho increases cholesterol 7α-hydroxylase expression and bile acid synthesis,16,42–45 highlighting the importance of each of these proteins in the feedback regulatory pathway. This pathway of feedback inhibition of bile acid synthesis is illustrated in Figure 1.
Figure 1.
Pathway by which the enterohepatic circulation of bile acids down regulates bile acid biosynthesis. Bile acids traversing the ileal enterocyte activate FXR, the nuclear receptor for bile acids (shown as a heterodimer with RXR, the retinoid X receptor). FXR activation promotes the synthesis of a protein, fibroblast growth factor – 19 (FGF19), which exits the ileal enterocyte by an unknown mechanism, and travels to the liver in portal venous blood. FGF19 interacts with a FGFR4/βklotho receptor complex present on the sinsudoidal membrane of the hepatocyte. The activated receptor initiates a phosphorylation cascade that culminates in the transcriptional repression of the gene encoding cholesterol 7α-hydroxylase, the rate limiting enzyme in bile acid biosynthesis.32
The late Hess Thaysen, working in Denmark, identified a group of patients who had bile acid malabsorption and diarrhea responsive to cholestyramine, yet had no detectable ileal pathology.46 The defect has been termed primary bile acid malabsorption or idiopathic bile acid malabsorption. Merrick et al showed that bile acid malabsorption was common in patients diagnosed as irritable bowel syndrome, diarrhea predominant.47,48 This observation was confirmed by Bardhan and his colleagues working in Rotherham, UK49 as well as in Italy50 and Sweden51. It was logical to assume that such patients would have a defect in the gene encoding the ileal apical bile acid transporter. However, in a careful study by Montagnani et al, no defects in the gene encoding the apical sodium dependent bile acid transporter (SLC10a2) were identified.52 Moreover, independent studies by Tilburg et al53, and Bajor et al54 showed that conjugated bile acid transport by human ileal biopsy samples was not defective, but either normal or increased.
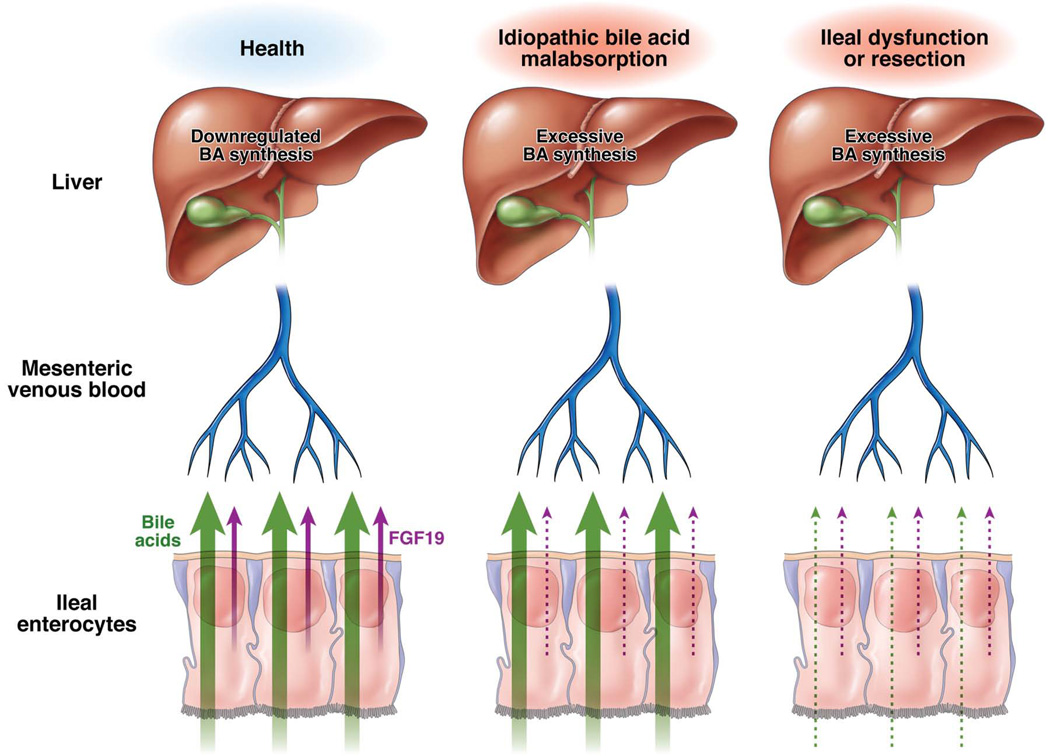
In this issue of CGH, Julian Walters and his colleagues present evidence for a new and fascinating explanation for the altered bile acid metabolism that is present in such patients.1 They describe a group of patients with chronic diarrhea responsive to cholestyramine who have bile acid malabsorption based on SeHCAT non-retention and increased plasma levels of C4. Their exciting discovery was that these patients had low plasma levels of FGF19. A low plasma level of FGF19 should in turn lead to defective negative feedback of bile acid biosynthesis and increased bile acid biosynthesis. In this new steady state, ileal transport is saturated, and increased bile acids pass into the colon, inducing secretion that in turn is manifest clinically as diarrhea. This pathophysiological defect can explain why Bajor et al53 and Tilburg et al54 and Bajor et al found unimpaired bile acid transport in their ileal biopsy samples. It is not known why plasma levels of FGF19 are abnormally low, and this will surely be investigated. Figure 2 compares the pathophysiological defect in patients with idiopathic bile acid malabsorption (as elucidated by the study of Walters et al1) with that present in patients with ileal dysfunction or resection.
Figure 2.
Presumed pathophysiological defect in release of FGF19 from the ileal enterocyte in idiopathic bile acid malabsorption (middle panel) is contrasted with normal release in health (left panel) or defective release in ileal dysfunction or resection (right panel). Bile acid transport is unimpaired in idiopathic bile acid malabsorption. As yet, defective synthesis and/or release from the ileal enterocyte is an inference based on the abnormally low plasma levels of FGF19 found in patients with idiopathic bile acid malabsorption as reported in this issue by Walters et al.1 Not shown is the colonic flux of bile acids. It is increased in idiopathic bile acid malabsorption and ileal dysfunction causing colonic secretion manifest as diarrhea.
At last, we have a satisfying explanation for at least some cases of idiopathic bile acid malabsorption. Such patients should have increased bile acid biosynthesis and increased bile acid secretion. Presumably ileal transport is at its maximum, although some animal and human studies suggest that the ileal bile acid transport system should downregulate when exposed to an increased flux of bile acids55
The observation by the Walters group is the culmination of fifty years of research on the enterohepatic circulation of bile acids. For the physician, an explanation is available for a subset of patients with chronic diarrhea. The diagnosis of bile acid malabsorption can be made by finding an increased plasma level of C4. However, a simple therapeutic trial of a bile acid sequestrant such as colesevelam or cholestyramine should generally be sufficient to establish the diagnosis and, if the patient responds, indicate successful therapy, providing symptomatic relief. In the future, it may be possible to synthesize nonprotein FGF19 agonists that would act to downregulate bile acid synthesis to normal rates and thereby correct the pathophysiological defect..
Acknowledgments
This work was supported by National Institutes of Health grant DK067158 and the Welch Foundation (D.J.M. and S.A.K.) and the Howard Hughes Medical Institute (D.J.M.). All of the authors have served as ad hoc consultants to Daiichi Sankyo Inc. who market colesevelam for the treatment of type 2 diabetes in the United States.
References
- 1.Walters JRF, Tasleem AM, Omer OS, et al. A new mechanism for bile acid diarrhea: excessive bile acid biosynthesis caused by defective fibroblast growth factor 19 release from the ileum. Clin Gastro Hepatol. 2009;8 00-00. [Google Scholar]
- 2.Tappeiner AJFH. Uber die Aufsaugung der Gallsäuren alkalien in Dünndarme. Wien Akad Sitzb. 1878;77:281–304. [Google Scholar]
- 3.Lack L, Weiner IM. Intestinal absorption of bile salts by small intestine of rats and guinea pigs. Am J Physiol. 1961;200:313–317. doi: 10.1152/ajplegacy.1961.200.2.313. [DOI] [PubMed] [Google Scholar]
- 4.Wong MH, Oelkers P, Craddock AL, et al. Expression cloning and characterization of the hamster ileal sodium-dependent bile acid transporter. J Biol Chem. 1994;269:1340–1347. [PubMed] [Google Scholar]
- 5.Wang W, Seward DJ, Li L, et al. Expression cloning of two genes that together mediate organic solute and steroid transport in the liver of a marine vertebrate. Proc Natl Acad Sci USA. 2001;98:9431–9436. doi: 10.1073/pnas.161099898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballatori N, Christian WV, Lee JY, et al. OSTalpha/OSTbeta: a major basolateral bile acid and steroid transporter in human, intestinal, renal, and biliary epithelia. Hepatology. 2005;42:1270–1279. doi: 10.1002/hep.20961. [DOI] [PubMed] [Google Scholar]
- 7.Dawson PA, Hubbert M, Haywood J, et al. The heteromeric organic solute transporter alpha-beta, Ostalpha-Ostbeta, is an ileal basolateral bile acid transporter. J Biol Chem. 2006;280:6960–6968. doi: 10.1074/jbc.M412752200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shefer S, Hauser S, Bekersky I, et al. Feedback regulation of bile acid biosynthesis in the rat. J Lipid Res. 1969;10:646–655. [PubMed] [Google Scholar]
- 9.Hofmann AF, Poley JR. Role of bile acid malabsorption in pathogenesis of diarrhea and steatorrhea in patients with ileal resection. I. Response to cholestyramine or replacement of dietary long chain triglyceride by medium chain triglyceride. Gastroenterology. 1972;62:918–934. [PubMed] [Google Scholar]
- 10.Aldini R, Roda A, Festi D, et al. Bile acid malabsorption and bile acid diarrhea in intestinal resection. Dig Dis Sci. 1982;27:495–502. doi: 10.1007/BF01296727. [DOI] [PubMed] [Google Scholar]
- 11.McJunkin B, Fromm H, Sarva RP, et al. Factors in the mechanism of diarrhea in bile acid malabsorption: fecal pH--a key determinant. Gastroenterology. 1981;80:1454–1464. [PubMed] [Google Scholar]
- 12.Grundy SM, Ahrens EH, Jr, Salen G. Interruption of the enterohepatic circulation of bile acids in man: comparative effects of cholestyramine and ileal exclusion on cholesterol metabolism. J Lab Clin Med. 1971;78:94–121. [PubMed] [Google Scholar]
- 13.Miettinen TA. Relationship between faecal bile acids, absorption of fat and vitamin B 12 and serum lipids in patients with ileal resections. Eur J Clin Invest. 1971;1:452–460. doi: 10.1111/j.1365-2362.1971.tb00557.x. [DOI] [PubMed] [Google Scholar]
- 14.Pandak WM, Heuman DM, Hylemon PB, et al. Failure of intravenous infusion of taurocholate to down-regulate cholesterol 7 alpha-hydroxylase in rats with biliary fistulas. Gastroenterology. 1995;108:533–544. doi: 10.1016/0016-5085(95)90083-7. [DOI] [PubMed] [Google Scholar]
- 15.Nagano M, Kuroki S, Mizuta A, et al. Regulation of bile acid synthesis under reconstructed enterohepatic circulation in rats. Steroids. 2004;69:701–709. doi: 10.1016/j.steroids.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 16.Inagaki T, Choi M, Moschetta A, et al. Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab. 2005;2:217–225. doi: 10.1016/j.cmet.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Mekhjian HS, Phillips SF, Hofmann AF. Colonic secretion of water and electrolytes induced by bile acids: perfusion studies in man. J Clin Invest. 1971;50:1569–1577. doi: 10.1172/JCI106644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chadwick VS, Gaginella TS, Carlson GL, et al. Effect of molecular structure on bile acid-induced alterations in absorptive function, permeability and morphology in the perfused rabbit colon. J Lab Clin Med. 1979;94:661–674. [PubMed] [Google Scholar]
- 19.Hofmann AF. The syndrome of ileal disease and the broken enterohepatic circulation: cholerheic enteropathy. Gastroenterology. 1967;52:752–757. [PubMed] [Google Scholar]
- 20.Hofmann AF, Poley JR. Cholestyramine treatment of diarrhea associated with ileal resection. N Engl J Med. 1969;281:397–402. doi: 10.1056/NEJM196908212810801. [DOI] [PubMed] [Google Scholar]
- 21.Puleston J, Morgan H, Andreyev J. New treatment for bile salt malabsorption. Gut. 2005;54:441–442. doi: 10.1136/gut.2004.054486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grundy SM, Ahrens EH, Jr, Miettinen TA. Quantitative isolation and gas-liquid chromatographic analysis of total fecal bile acids. J Lipid Res. 1965;6:397–410. [PubMed] [Google Scholar]
- 23.Porter JL, Fordtran JS, Santa Ana CA, et al. A simple and accurate enzymatic method for measurement of total fecal bile acids in patients with severe fat Malabsorption. J Lab Clin Med. 2003;141:411–418. doi: 10.1016/S0022-2143(03)00040-4. [DOI] [PubMed] [Google Scholar]
- 24.Hofmann AF, Bolder U. Detection of bile acid malabsorption by the SeHCAT test: principles, problems and clinical utility. Gastroenterol Clin Biol. 1994;18:847–851. [PubMed] [Google Scholar]
- 25.Thaysen EH, Orholm NM, Arnefred T, et al. Assessment of ileal function by abdominal counting of the retention of a gamma emitting bile acid analogue. Gut. 1982;23:862–865. doi: 10.1136/gut.23.10.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brydon WG, Nyhlin H, Eastwood MA, et al. Serum 7 alpha-hydroxy-4-cholesten-3-one and selenohomocholyltaurine (SeHCAT) whole body retention in the assessment of bile acid induced diarrhoea. Eur J Gastroenterol Hepatol. 1996;8:117–123. doi: 10.1097/00042737-199602000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Sciarretta G, Fagioli G, Furno A, et al. 75SeHCAT test in the detection of bile acid malabsorption in functional diarrhoea and its correlation with small bowel transit. Gut. 1987;28:970–975. doi: 10.1136/gut.28.8.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fellous K, Jian R, Haniche M, et al. Mesure de l’absorption ileale des sels biliaires par le test a l’homotaurocholate marquee au selenium 75. Validation et signification clinique. Gastroenterol Clin Biol. 1994;18:865–872. [PubMed] [Google Scholar]
- 29.Gälman C, Arvidsson T, Angelin B, et al. Monitoring hepatic cholesterol 7 alpha-hydroxylase activity by assay of the stable bile acid intermediate 7 alpha-hydroxy-4-cholesten-3-one in peripheral blood. J Lipid Res. 2003;44:859–866. doi: 10.1194/jlr.D200043-JLR200. [DOI] [PubMed] [Google Scholar]
- 30.Eusufzai S, Axelson M, Angelin B, et al. Serum 7alpha-hydroxy-4-cholesten-3-one concentrations in the evaluation of bile acid malabsorption in patients with diarrhoea: correlation to SeHCAT test. Gut. 1993;34:698–701. doi: 10.1136/gut.34.5.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sauter GH, Munzing W, von Ritter C, et al. Bile acid malabsorption a cause of chronic diarrhea: diagnostic value of 7alpha-hydroxy-4-cholest-3-one in serum. Dig Dis Sci. 1999;44:14–19. doi: 10.1023/a:1026681512303. [DOI] [PubMed] [Google Scholar]
- 32.Chiang JYL. Bile acids: regulation of synthesis. J Lipid Res. 2009 doi: 10.1194/jlr.R900010-JLR200. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parks DJ, Blanchard SG, Bledsoe RK, et al. Bile Acids: Natural ligands for an orphan nuclear receptor. Science. 1999;284:1365–1368. doi: 10.1126/science.284.5418.1365. [DOI] [PubMed] [Google Scholar]
- 34.Makashima M, Okamoto AY, Repa JJ, et al. Identification of a nuclear receptor for bile acids. Science. 1999;284:1362–1365. doi: 10.1126/science.284.5418.1362. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Chen J, Holister K, et al. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol Cell. 1999;3:543–553. doi: 10.1016/s1097-2765(00)80348-2. [DOI] [PubMed] [Google Scholar]
- 36.Lu TT, Makashima M, Repa JJ, et al. Molecular basis for feedback regulation of bile acid synthesis by nuclear receptors. Mol Cell. 2000;6:507–515. doi: 10.1016/s1097-2765(00)00050-2. [DOI] [PubMed] [Google Scholar]
- 37.Goetz R, Beenken A, Ibrahimi OA, et al. Molecular insights into the klotho-dependent, endocrine mode of action of fibroblast growth factor 19 subfamily members. Mol Cell Biol. 2007;27:3417–3428. doi: 10.1128/MCB.02249-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin BC, Wang M, Blackmore C, et al. Liver-specific activities of FGF19 require Klotho beta. J Biol Chem. 2007;282:27277–27284. doi: 10.1074/jbc.M704244200. [DOI] [PubMed] [Google Scholar]
- 39.Wu X, Ge H, Gupte J, et al. Co-receptor requirements for fibroblast growth factor-19 signaling. J Biol Chem. 2007;282:29069–29072. doi: 10.1074/jbc.C700130200. [DOI] [PubMed] [Google Scholar]
- 40.Holt JA, Luo G, Billin AN, et al. Description of a novel growth factor-dependent signal cascade for the suppression of bile acid biosynthesis. Genes Dev. 2003;17:1581–1591. doi: 10.1101/gad.1083503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Song KH, Li T, Owsley E, et al. Bile acids activate fibroblast growth factor 19 signaling in human hepatocytes to inhibit cholesterol 7alpha-hydroxylase gene expression. Hepatology. 2009;49:297-3. doi: 10.1002/hep.22627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kok T, Hulzebos CV, Wolters H, et al. Enterohepatic circulation of bile salts in farnesoid X receptor-deficient mice: efficient intestinal bile salt absorption in the absence of ileal bile acid-binding protein. J Biol Chem. 2003;278:41930–41937. doi: 10.1074/jbc.M306309200. [DOI] [PubMed] [Google Scholar]
- 43.Sinal CJ, Tohkin M, Miyata M, et al. Targeted disruption of the nuclear receptor FXR/BAR impairs bile acid and lipid homeostasis. Cell. 2000;102:731–744. doi: 10.1016/s0092-8674(00)00062-3. [DOI] [PubMed] [Google Scholar]
- 44.Yu C, Wang F, Kan M, et al. Elevated cholesterol metabolism and bile acid synthesis in mice lacking membrane tyrosine kinase receptor FGFR4. J Biol Chem. 2000;275:15482–15489. doi: 10.1074/jbc.275.20.15482. [DOI] [PubMed] [Google Scholar]
- 45.Ito S, Fujimori T, Furuya A, et al. Impaired negative feedback suppression of bile acid synthesis in mice lacking betaKlotho. J Clin Invest. 2005;115:2202–2208. doi: 10.1172/JCI23076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thaysen EH. Idiopathic bile acid diarrhoea reconsidered. Scand J Gastroenterol. 1985;20:452–456. doi: 10.3109/00365528509089679. [DOI] [PubMed] [Google Scholar]
- 47.Merrick MV, Eastwood MA, Ford MJ. Is bile acid malabsorption underdiagnosed? An evaluation of diagnosis by measurement of SeHCAT retention. Br Med J (Clin Res Ed) 1985;290:665–668. doi: 10.1136/bmj.290.6469.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams AJ, Merrick MV, Eastwood MA. Idiopathic bile acid malabsorption – a review of clinical presentation, diagnosis, and response to treatment. Gut. 1991;32:1004–1006. doi: 10.1136/gut.32.9.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith MJ, Cherian P, Raju GS, et al. Bile salt malabsorption in persistent diarrhoea. J R. Coll Physicians Lond. 2000;34:448–451. [PMC free article] [PubMed] [Google Scholar]
- 50.Galatola G. The prevalence of bile acid malabsorption in irritable bowel syndrome and the effect of cholestyramine: an uncontrolled open multicentre study. Eur J Gastroenterol Hepatol. 1992;4:533–537. [Google Scholar]
- 51.Wildt S, Norby Rasmussen S, Lysgard Madsen J, et al. Bile acid malabsorption in patients with chronic diarrhoea: clinical value of SeHCAT test. Scand J Gastroenterol. 2003;38:826–830. doi: 10.1080/00365520310004461. [DOI] [PubMed] [Google Scholar]
- 52.Montagnani M, Love MW, Rossel P, et al. Absence of dysfunctional ileal sodium-bile acid cotransporter gene mutations in patients with adult-onset idiopathic bile acid malabsorption. Scand J Gastroenterol. 2001;36:1077–1080. doi: 10.1080/003655201750422693. [DOI] [PubMed] [Google Scholar]
- 53.Bajor A, Kilander A, Fae A, et al. Normal or increased bile acid uptake in isolated mucosa from patients with bile acid malabsorption. Eur J Gastroenterol Hepatol. 2006;18:397–403. doi: 10.1097/00042737-200604000-00013. [DOI] [PubMed] [Google Scholar]
- 54.Tilburg AJ, de Rooij FW, van den Berg JW, et al. Primary bile acid diarrhoea without an ileal carrier defect: quantification of active bile acid transport across the ileal brush border membrane. Gut. 1991;32:500–503. doi: 10.1136/gut.32.5.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lillienau J, Munoz J, Longmire-Cook SJ, et al. Negative feedback regulation of the ileal bile acid transport system in rodents. Gastroenterology. 1993;104:38–46. doi: 10.1016/0016-5085(93)90833-x. [DOI] [PubMed] [Google Scholar]