Abstract
Objective
This is an observational prospective cohort study to explore the treatment effect of mechanical vs. manual manipulation for acute low back pain.
Methods
Ninety two patients with a history of acute low back pain were recruited from 3 private chiropractic offices, 2 of which utilized manual lumbar manipulation and 1 used mechanical instrument manipulation (Activator) as their primary modes of treatment. The chiropractors used their “treatment as usual” protocols for a maximum of 8 visits or 4 weeks, which ever occurred first. Primary outcome measures were changes in Numeric Pain Rating Scale (NPRS) and Oswestry Disability Index (ODI) scores from baseline to 4 weeks. The linear regression models were adjusted for baseline NPRS and ODI scores, age, and treatment expectancy.
Results
Comparison of baseline characteristics did not show any significant differences between the groups except for age (38.4 vs. 49.7 years; p < .001) and treatment expectancy (5.7 vs. 6.3; p = .003). Linear regression revealed significantly lower NPRS scores in the manual manipulation group at four weeks [β = −1.2; 95% CI (−2.1, −.28)] but no significant difference in ODI scores between the two groups at four weeks [β = 1.5; 95% CI (−8.3, 2.4)]. Treatment expectancy, but not age, was found to have a significant main effect on both NPRS and ODI scores at 4 weeks. Exploratory analysis of the clinical patterns of care between the clinicians revealed significant differences in treatment frequency, duration, modality and radiograph usage between the 2 cohorts.
Conclusions
This study highlights the challenges inherent with conducting research that allows for “treatment-as-usual”. The data and experience derived from this investigational study will be used to design a future randomized clinical trial in which tighter controls will be imposed on the treatment protocol.
Keywords: Manipulation, Spinal, Low Back Pain, Chiropractic
INTRODUCTION
Low back pain (LBP) is a serious public health issue in the United States and many other Western societies for three basic reasons, the first of which is the large prevalence of low back pain in American society. The general yearly prevalence in the U.S. population is estimated at 15–20% and among working-age adults at 50%. (1) Back pain is the most common cause of disability for persons under the age of 45 and the second most common reason for office visits to primary care physicians. (2) The second reason is the high rate of disability and activity intolerance due to low back pain. A population based survey of adults showed a low back pain point prevalence of about 25%, with about 50% of those low back pain patients showing moderate disability and about 10% reporting severe or total disability. (3) The third reason is increasing evidence that low back pain is not necessarily a self-limiting disorder. One recent study showed that of patients who experienced LBP for greater than thirty days, 40% continued to have symptoms for another one to five years. (4)
In 1994, the Agency for Health Care Policy and Research (AHCPR) published clinical practice guidelines for the management of acute low back problems in adults based upon a quantitative review of the literature that included a meta-analysis investigating the relative effectiveness of various treatments for low back pain. (5) The AHCPR guidelines were the first time that an official government health agency recommended manipulation as an effective treatment for patients with acute low back pain. During the past fifteen years since the publication of these AHCPR guidelines, many additional clinical trials have been published that continue to show significant benefits of spinal manipulation for certain types of low back and neck pain. These trials have been the subject of several systematic reviews and meta-analyses of the manipulation literature, (6–13) the majority of which conclude that spinal manipulation is an established and effective treatment for acute low back pain.
This intervention called “spinal manipulation” that appears to be beneficial for acute low back pain is not a single treatment procedure. Spinal manipulation is an umbrella term that includes a multitude of different procedures that introduce a variety of manual and mechanical forces into the musculoskeletal structures. The type of manipulation used in the majority of manipulation trials included in systematic reviews of the literature was side posture thrust manipulation (Fig 1). An analysis by the editor of the Journal of Chiropractic Technique stated that there were over 100 chiropractic technique systems using a variety of manipulative methods. (14) The National Board of Chiropractic Examiners (NBCE) conducted questionnaire research to survey the chiropractic profession about the most frequently used manipulative techniques in clinical practice. (15, 16) The data indicated that the two most commonly-used methods were reported as Diversified Technique, which is essentially a side posture manual thrust technique; and Activator which utilizes a hand-held device to deliver a mechanical impulse in lieu of a manual thrust.
Figure 1.
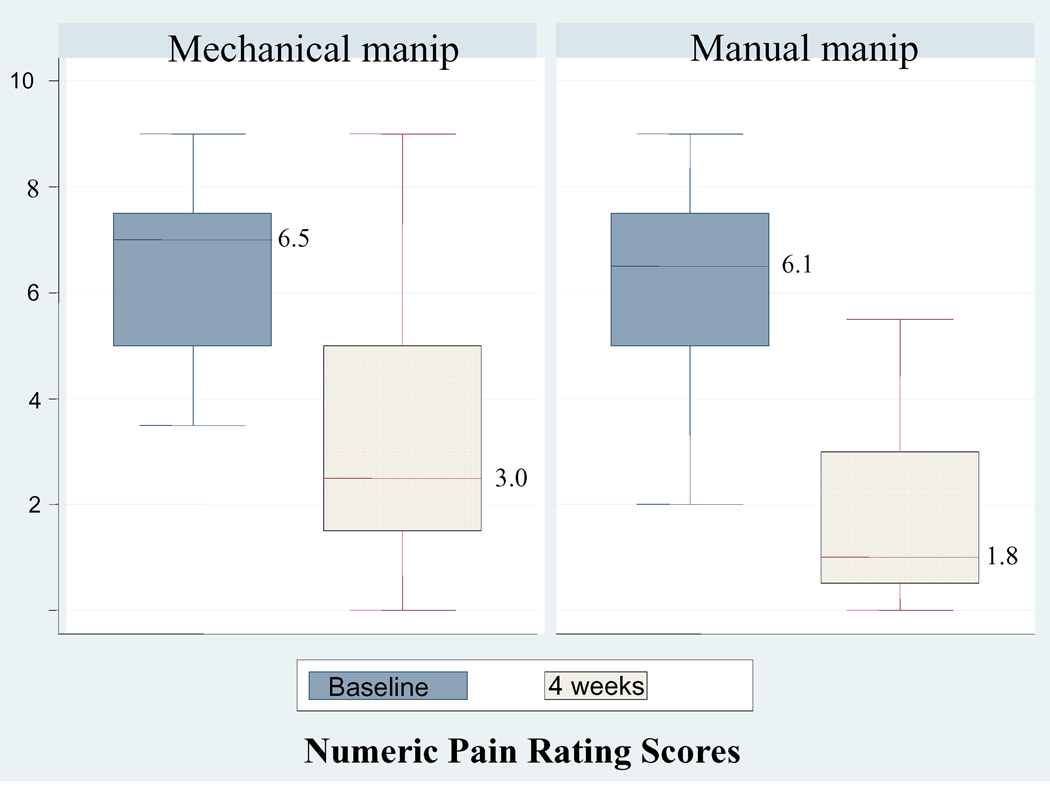
Baseline and 4-week unadjusted mean Numeric Pain Rating Scores (NPRS) by cohort. Regression analysis revealed that a significant difference in the mean adjusted 4-week pain scores remained after controlling for baseline pain, cohort, and expectation.
There is strong evidence for the clinical effectiveness of side posture thrust manipulation for the treatment of acute low back pain (8), with equivocal evidence for mechanical manipulation methods such as the Activator Instrument. (17, 18) Yet Activator is reported as the second most commonly used manipulative method within the chiropractic profession, and is reportedly used by over 32,000 chiropractors around the globe (http://www.activator.com/). The Activator Instrument and other mechanical impulse devices are often used as a substitute method for manual thrust manipulation with the assumption that they are gentle, safe, and clinically effective. (19) However, this assumption has not yet been validated with evidence from clinical trials; it is not known if an impulse delivered by a mechanical device such as the Activator Instrument is as clinically effective as a manual thrust manipulation. This study was designed to explore the question of whether there is a difference in clinical outcome using the Activator and manual thrust manipulation for treatment of LBP.
METHODS
Participants
Ninety two patients with a history of LBP were recruited from 3 private chiropractic clinics during the period January 1, 2006 through April 30, 2008. Informed consent was obtained from all research participants prior to initiation of any treatment, and the research design was approved by the University of Pittsburgh Institutional Review Board (IRB Approval # 0501148).
Inclusion criteria consisted of the following: age greater than 18 years with acute onset of LBP within the previous 12 weeks, Numeric Pain Rating Scale (NPRS) score between 4 to 8 points, and Oswestry LBP Disability Index (ODI) score between 20 to 70 percentage points. These ranges were designed to exclude patients with extremely high or low NPRS and ODI scores, in order to avoid ceiling or floor effects (regression to the mean). Exclusion criteria included red flags of serious pathology, including past history of cancer, pregnancy, previous lumbar surgery, stenosis, instability, or other serious pathology. Patients were also excluded if they had any absolute contraindications to manipulation (severe osteoporosis, prolonged use of steroids, etc.) or had any positive nerve root tension signs, sensory or motor deficit in the lower extremities. Lastly, patients were excluded from participation if they had received any physical therapy or chiropractic treatment for LBP within the past 3 months.
Interventions
The research patients were all treated in one of three private chiropractic clinics. One clinic employed two Activator Methods proficiency-certified chiropractors who exclusively used the Activator Instrument as the sole manipulative treatment for LBP. The other two offices exclusively utilized side posture thrust manipulation for treatment of LBP, with a single chiropractor rendering all treatments at each respective office. Therefore, patients attending the Activator clinic received only mechanical manipulations and those attending the other chiropractic clinics received only manual thrust manipulations.
The medical device used in this study was the Activator IV Instrument, FDA Approval # K003185 (Activator Methods International Ltd., 2950 N 7th Street, Phoenix, AZ 85014). This instrument is a hand-held device containing a spring-loaded mechanism that delivers a mechanical impulse. Some chiropractors use the Activator Instrument according to a defined protocol as taught by Activator Methods International, and others use the instrument in a more informal manner as a substitute for manual thrust manipulation. In this study, both clinicians were certified and trained in the Activator Methods protocol.
For purposes of this study, the research treatment period was considered to start at the initial baseline visit and to end at the eighth office visit or 4 weeks, whichever occurred first. The clinicians were not obligated to treat patients for a total of 8 visits or four weeks; the research design permitted treatment for as many visits as the clinician deemed clinically warranted. This design allowed for data collection about treatment frequency/duration to be used for a secondary analysis. The chiropractors were asked to treat the research patients like any other patients in their offices, but to refrain from providing any mechanical traction or supervised exercises during the course of the study. The use of physical agents and other modalities was permitted, and these were recorded for data analysis.
Objectives
The primary aim of this study was to gather data and calculate treatment effect sizes on NPRS and ODI, when comparing manual thrust manipulation and Activator for treatment of low back pain. Secondary aims were: (1) to explore the differences in clinical practice style and patient characteristics between chiropractic offices that were permitted to use a “treatment-as-usual” approach and (2) to explore the effect of treatment expectancy on clinical outcomes and see if there was an interaction effect with treatment method.
The primary outcome measure was the Numeric Pain Rating Scale (NPRS) and the secondary outcome measure was the Oswestry LBP Disability Index (ODI). These scores were taken at baseline and four weeks. Both of these outcome measures have been widely used in previously published LBP clinical trials, and have been previously shown to have good reliability and validity. (20, 21)
The NPRS asks patients to respond to three questions about their pain intensity on an 11 point scale ranging from 0 (no pain) to 10 (worst pain); (1) pain level right now, (2) worst pain level in past 24 hours, and (3) best level of pain in past 24 hours. For the purpose of analysis in this study, we created a composite pain variable by taking the average of the “pain right now” and “worst pain in past 24 hours” scores recorded at baseline and four weeks.
The ODI form consists of a series of ten questions that each have six possible responses that are graded from 0 (good) to 5 (bad) points, based upon the severity of self-perceived disability regarding each question. Therefore the total possible number of points is 50 points, which would indicate crippling disability. It is customary to report ODI scores as a percentage, which is derived by dividing the number of total points by 50.
In addition to the NPRS and ODI, research subjects were asked at baseline to complete a treatment expectancy questionnaire (TEQ). The TEQ asked a series of questions about the research participant’s expectations about each type of manipulation, as well as their belief about how well they would respond to treatment in general. The variable used for analysis was the score from the general question “How well do you expect to feel in 4 weeks?”, which was self-rated on a seven-point Likert scale ranging from 1 = ”I expect to be much worse” to 7 = ”I expect to be completely better”. The TEQ was developed by the author (MJS) and has not been validated. Since the observational design permitted treatment-as-usual, clinical data was also collected about the number of treatment sessions, adjunctive modalities and physical agents used in each clinic, clinical history, and the frequency/duration of treatment.
Sample Size and Randomization
Previous low back pain literature has indicated that the minimal clinically important difference (MCID) in ODI scores is 8 points with a standard deviation of 14 points. (20, 22) Power analysis was therefore performed using a mean difference of 8 ODI points and a standard deviation of 14 points, which revealed that 50 patients per group would be needed to achieve 80% power at an alpha level of .05 (STATA, Ver. 10.1, College Station, TX).
No randomization process was utilized in this study; patients self-selected their choice of chiropractic method and clinic. This study involved a treatment-as-usual observational design; therefore no experimental treatment methods were used. The chiropractors at each clinic were instructed to treat the research participants in the same manner as they would normally treat any other LBP patient in their offices. The research participants and treating clinicians were obviously not blinded, due to the self-selection of treatment method.
Statistical Analysis
Baseline characteristics were compared between the two cohorts using Chi Square tests for all categorical variables. Student’s t-tests were used to compare the continuous variables (age and expectation) between the patients in the 2 cohorts. The main analysis of primary and secondary outcome measures started with a basic regression model that was built with final NPRS and ODI scores at 4-weeks as the dependent variables, and cohort (type of manipulation) as the key independent variable. This basic model was used to compare the unadjusted mean 4-week NPRS and ODI scores between the two cohorts.
The basic regression model was then expanded with a forced entry step-wise approach adding the following four independent variables and their associated cohort interaction terms:
Centered baseline NPRS and ODI scores: These were included as covariates because of the assumption that the baseline NPRS and ODI scores would account for a significant amount of the variability in their respective 4-week scores. Baseline scores were centered by subtracting each individual score from the mean of all baseline scores (within-group mean) in each cohort.
Age: Age is a well recognized risk factor for low back pain and might have an independent influence on treatment outcome.
Medication Usage: Use of various anti-inflammatory/pain medications could have a potential independent therapeutic effect and confound the analysis.
Treatment Expectancy: A secondary aim of this study was to explore the hypothesis that treatment expectancy might influence clinical outcomes.
The forward step-wise regression model was built by adding each of the above independent variables and their respective interaction terms individually, and retaining any variables whose partial t-tests showed a p-value of least .05 or less. Separate regression models were constructed for the primary (NPRS) and secondary (ODI) outcome measures.
RESULTS
Comparisons of the baseline characteristics of both cohorts were performed and the results are summarized in Table 1. The 2 cohorts did not differ significantly on any of these variables other than age and treatment expectancy. The mean age and treatment expectancy scores were significantly higher in the manual manipulation cohort. Although medication usage appeared different between the two cohorts (41% vs 22%) this difference did not achieve statistical significance, most likely due to the small sample size.
Table 1.
Baseline characteristics by cohort. Chi Square tests of all categorical variables did not reveal any significant differences between the two groups except for age and treatment expectancy. T-tests were used to analyze the mean age and treatment expectancy scores.
| Baseline Characteristics | Mechanical manip | Manual manip | p-value | |
|---|---|---|---|---|
| n = 53 | n = 39 | |||
| Gender (males) | 56% | 54% | .81 | |
| Age (mean in years) | 38.4 | 49.7 | .001 (t-test) |
|
|
Treatment expectancy (mean score; 1–7 Likert scale) |
5.7 | 6.3 | .003 (t-test) |
|
| Race (Caucasian) | 100% | 100% | - | |
| Marital Status | .21 | |||
| Single | 35% | 18% | ||
| Married | 56% | 68% | ||
| Other | 9% | 14% | ||
| Education | .25 | |||
| ≤ High School | 49% | 36% | ||
| College | 51% | 64% | ||
| Income | .25 | |||
| ≤ $35,000/ yr | 56% | 47% | ||
| $35,001 to $70,000 | 30% | 23% | ||
| > $70,000/ yr | 15% | 30% | ||
| Employment Status | .99 | |||
| Working Full-time | 65% | 63% | ||
| Working Part-time | 13% | 13% | ||
| Other (not working) | 22% | 24% | ||
| Smoker | 30% | 26% | .73 | |
| Medications | .14 | |||
| None | 59% | 78% | ||
| NSAIDs | 32% | 19% | ||
| Prescription pain meds | 9% | 3% | ||
The primary outcome measure in this study was NPRS at 4-weeks compared to baseline NPRS score. There was a significant difference between the unadjusted mean 4-week NPRS scores of the 2 cohorts (mean difference=1.2; p=.011). Figure 1 displays the unadjusted mean pain scores of each cohort at baseline and 4-weeks. After adjusting for centered baseline NPRS scores, there remained a significant difference in the adjusted means between groups. The 2 significant predictor variables (cohort and baseline pain) predicted about 11% of the variation in NPRS score at 4-weeks (R2 = .11). There were no significant main effects for medication, age, or their interaction terms when these variables were added to the regression model.
Subgroup analysis explored the effect of adding treatment expectancy score and its interaction effect with treatment method (cohort) to the regression model described above, which had curious effects on the results. There was no significant interaction effect for the variable ‘expectancy score*cohort’, indicating that treatment expectancy scores did not exert differential influence on the 4-week NPS scores in the 2 cohorts. The new model did reveal a significant main effect for expectancy and explained 16% of the variation in 4-week NPRS scores (R2 = .16). However, the addition of treatment expectancy to the model eliminated the previously significant main effects of cohort and baseline NPRS score. When the expectation variable was removed from the model, cohort and baseline pain again showed significant main effects. This paradoxical effect of the expectancy variable strongly suggests that expectation is a confounder of the relationship between cohort (treatment method) and outcome.
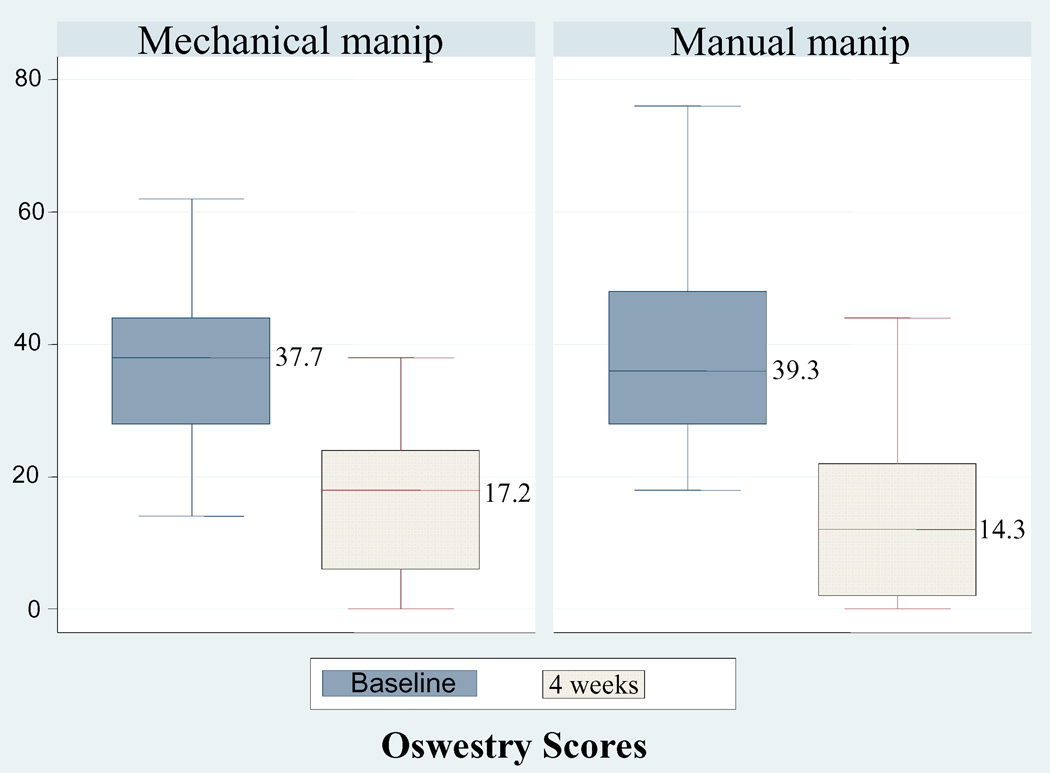
The secondary outcome analysis created similar regression models, but this time using 4-week ODI score compared to baseline ODI score. There was no significant difference between the unadjusted mean 4-week ODI scores of the two cohorts (mean difference=2.9; p=.29). Figure 2 displays the unadjusted mean Oswestry scores of each cohort at baseline and 4-weeks. The addition of centered baseline ODI score to the model did not change these results; the difference in 4-week ODI scores between groups was not statistically significant and the confidence interval was very wide (adjusted mean difference = 1.5 points, 95% CI; −8.3, 2.4). These two predictor variables (centered baseline ODI and cohort) as a whole only predicted about 7% of the variation in the 4-week ODI scores (R2 = .069).
Figure 2.
Baseline and four-week unadjusted mean Oswestry Disability Index (ODI) scores by cohort. Regression analysis did not reveal any significant difference in mean four-week ODI scores after controlling for baseline ODI.
Subgroup analysis with the addition of treatment expectancy to the model showed no main effect for expectancy or its interaction term, but eliminated the previously significant main effects of cohort and baseline ODI scores as predictor variables. Yet the new model which included the expectancy variable was able to explain 11% of the predicted variation in 4-week ODI scores (R2 =.11). Again, the most reasonable explanation for these paradoxical effects is that expectancy score is a confounder of the relationship between treatment method (cohort) and 4-week outcome.
The observational design of this study permitted us to capture additional descriptive data about the clinical patterns of care provided to the patients in both cohorts, which allowed for further exploratory subgroup analyses. A comparison was made between the proportions of modalities and adjunctive procedures used in the two treatment groups, which revealed many significant differences (Table 2). The Activator patients had significantly more application of electrical muscle stimulation, laser therapy, inter-segmental traction (roller) table, and posture education. The manual manipulation patients had significantly more applications of heat/ice packs.
Table 2.
Comparison of modalities and adjunctive procedures.
| Type of Modality | Mechanical manip n = 53 |
Manual manip n = 39 |
p-value (Chi-square) |
|---|---|---|---|
| Electrical stimulation | 96% | 74% | .002 |
| Ultrasound | 2% | 5% | .38 |
| Laser | 9% | 0% | .05 |
|
Roller table (intersegmental mobs) |
74% | 0% | .001 |
| Myofascial therapy | 0% | 3% | .24 |
| Posture education | 54% | 31% | .03 |
| Home exercises | 60% | 56% | .70 |
| Heat/Ice | 0% | 8% | .04 |
Another exploratory subgroup analysis compared the various clinical patterns of the two treatment groups, including frequency/duration of treatment, diagnostic imaging usage, and physical examination findings. The results of this analysis are displayed in Table 3. There was a significant difference between the two cohorts with respect to the number of patients in each group that required the maximum number of treatment sessions (8 visits); 70% in the Activator group compared to only 15% in the manual manipulation group. 78% of the Activator patients continued with additional chiropractic care after study termination whereas only 18% in the manual manipulation groups received additional chiropractic treatment. The mean number of visits at 4 weeks also was significantly different between the two cohorts, with the Activator group having a mean of 9.2 visits as compared with the manual manipulation group mean of 4.5 visits.
Table 3.
Comparison of treatment frequency/duration and other clinical patterns.
| Clinical Variable | Mechanical manip n=53 |
Manual manip n=39 | p-value (Chi-square) | |
|---|---|---|---|---|
| Study terminated at: | <.001 | |||
| 8 visits | 70% | 15% | ||
| 4 weeks | 17% | 23% | ||
| < 4 weeks | 13% | 62% | ||
|
Continued with care after study? (yes) |
78% | 18% | <.001 | |
|
Diagnostic studies ordered during study |
<.001 | |||
| None | 41% | 100% | ||
| Lumbar radiographs | 54% | 0% | ||
| Lumbar MRI | 5% | 0% | ||
| Number of visits at 4 weeks | ||||
| (Mean / standard deviation) | 9.2 (2.7) | 4.5 (2.3) | <.001 (t-test) | |
| Location of Symptoms | .07 | |||
| LBP only | 50% | 74% | ||
| LBP and buttock | 28% | 16% | ||
| LBP, buttock, and thigh | 22% | 10% | ||
| Onset of LBP | .016 | |||
| ≤ 14 days | 52% | 81% | ||
| 15 days to 12 weeks | 48% | 19% | ||
| Antalgic Lean Present? | .01 | |||
| None | 94% | 74% | ||
| Flexion | 0% | 18% | ||
| Lateral list | 6% | 8% | ||
| Limitation of Lumbar Flexion | <.001 | |||
| None | 2% | 31% | ||
| Mild (> 41º) | 48% | 45% | ||
| Moderate (20º – 40º) | 41% | 21% | ||
| Severe (< 20º) | 9% | 3% | ||
The manual manipulation cohort had a significantly higher number of acute patients (onset < 14 days) with lumbar pain only, and more patients displaying flexion antalgia. The Activator patients were more likely to receive lumbar radiographs (54%) or MRI (5%); none (0%) of the manual manipulation patients received any of these diagnostic tests during the course of this study. The Activator cohort had a significantly greater number of patients with buttock and thigh pain, as well as more patients with moderate to severe limitation of lumbar flexion.
DISCUSSION
The primary analysis between the differences in baseline and 4-week NPRS scores showed a significantly larger reduction in pain scores in the manual manipulation cohort, even after controlling for baseline pain. It is interesting to note that the 95% confidence interval for the change in pain score ranged from 2.05 to .28 points lower in the manual manipulation cohort, indicating a relatively robust treatment effect. The minimal clinically detectable change in NPRS score (within-subject) is considered to be about 2 points (20) and the mean difference in NPRS scores between these two groups (between-subjects) at 4-weeks was 1.2 points.
Conversely, the secondary analysis of ODI scores showed that the manipulation group had lower ODI scores at 4 weeks compared to the Activator group but this difference was not statistically significant. The 95% confidence interval for ODI scores is very wide, ranging from −8.3 to 2.4 points between the two cohorts. This wide confidence interval makes interpretation of these data very tenuous, considering that the minimal clinically important difference (MCID) for ODI scores is 8 points and the mean difference in ODI scores between these 2 groups at 4-weeks was only 2.9 points. It is appears that NPRS score was a more responsive outcome measure in this group of patients than ODI score.
This study confirmed the observation that chiropractors do not limit their treatment approach to spinal manipulation; they routinely include a number of other active and passive care procedures into their routine clinical care of LBP patients. It was also surprising to find that the majority of patients in both treatment arms received electrical muscle stimulation; when the literature has shown this modality to have little or no independent treatment effect (23, 24). On the other hand, posture education and home exercises were prescribed (hand-out literature only) for a majority of the patients in both treatment arms; an approach which is consistent with the best current evidence for non-surgical management of LBP (25).
Treatment expectancy in our study was positively correlated with clinical outcome, which is congruent with the findings from another recent study of expectancy and various treatments for LBP (26). Treatment expectancy has a well known effect pain relieving effect within the context of clinical research trials, as exemplified by the strong power of the placebo effect (27, 28). Most of our research population was composed of patients who had previous experience with chiropractic care, with patients in both groups recording overall high expectancy scores at baseline. Therefore it was not surprising to see treatment expectancy show up as a significant predictor variable in the regression analysis of NPRS scores, independent of the grouping variable. By allowing patients to self-select their treatment method and chiropractic clinic, we were able to confirm our suspicion that treatment expectancy is indeed a confounder of outcome and that chiropractic patients tend to have high expectancy that their self-selected treatment method will be helpful for their condition.
The data derived from this observational study serves as an important source of background information on the issues of treatment expectancy, treatment frequency/duration, attention bias, use of modalities and exercise/posture instruction. All of this background information may be useful in the design and implementation of a future randomized trial on this same research question.
Limitations
There were several limitations to this study, many of which are directly related to the observational design. No external constraints were placed upon the clinicians as to their treatment protocols and this lead to big variations in treatment frequency, application of adjunctive therapies, and other clinical activities. We did not record the amount of time spent during the doctor-patient interaction or total time spent during each office visit, and therefore attention bias is a possible confounder to the results. Without having a good estimate of treatment effect size in advance, it was hard to power this study appropriately. Although previous literature gave an estimate of within-person MCIDs for NPRS and ODI scores, there was no good literature estimating the between-person MCIDs for these outcome measures in LBP patients treated with 2 different types of manipulation. By allowing patients to self-select their clinicians, the independent effect of treatment expectancy could not be explored properly. Lastly, there was the limitation of no control group for comparison; natural history and regression to the mean may therefore account for some of the change in outcomes.
However, the intrinsic limitations of an observational design also gave this study some important strengths; including the ability to capture data from treatment-as-usual without an external locus of control over the treatment parameters. It was expected that some difference in clinical patterns of care would be found between the groups. However, it was surprising to find that the Activator group had twice the number of office visits at 4 weeks with higher utilization of modalities and radiographs compared to the manual manipulation group. These utilization findings may reflect differences in practice management styles between doctors/clinics, rather than an intrinsic difference between the clinical effectiveness of mechanical and manual manipulation methods.
CONCLUSION
In conclusion, this study provided some very important data and information about the clinical effects of mechanical versus manual methods of manipulation. It provided a good estimate of treatment effect sizes for changes in NPRS and ODI, which can now be used for power analysis in a future randomized trial. The wide variation in clinical practice patterns and management styles between the clinicians was a very interesting finding that could only have been uncovered within the context of a “treatment-as-usual” research design. Treatment expectancy was found to be a surprisingly strong predictor variable that was independent of treatment method. These data will play an important role in the design and implementation of a future randomized clinical trial that will impose a structured treatment frequency and use of physical agents, while controlling for treatment expectancy and attention bias.
PRACTICAL APPLCATIONS.
Primary outcome measures were Numeric Pain and Oswestry scores compared from baseline to 4 weeks.
Manual manipulation group showed greater reduction in Numeric Pain scores at 4 weeks, but no difference between groups in Oswestry scores at 4 weeks.
Treatment expectancy was found to be a strong predictor variable and confounder.
Wide variations in treatment frequency/duration and modalities were found between the cohorts.
This study highlights the inherent difficulties of observational research studies.
ACKNOWLEDGEMENTS
I thank Mitch Haas, Darcy Vavrek, and Sunday Clark for refinements in the statistical analysis and regression models, especially the data involving the expectancy scores. I would also like to thank the following doctors of chiropractic who volunteered their time to help with refinement of research ideas and who provided treatment to the patients recruited to this study: Drs. Anthony Barber, Robert Homonai, Frank Imbarlina, Brian Moreland, and William Tellin.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
FUNDING SOURCES AND CONFLICTS OF INTEREST
Dr. Schneider completed this study while receiving salary support under a grant from the National Institutes of Health (NIH) National Center for Complementary and Alternative Medicine (NCCAM) NIH/NCCAM Grant #: K99 A T004196-01. No conflicts of interest were reported for this study.
Contributor Information
Michael J Schneider, Visiting Assistant Professor, School of Health and Rehabilitation Sciences, University of Pittsburgh, Pittsburgh, PA.
Jennifer Brach, Assistant Professor, Department of Physical Therapy, School of Health and Rehabilitation Sciences, University of Pittsburgh, Pittsburgh, PA, jbrach@shrs.pitt.edu.
James J. Irrgang, Associate Professor and Director of Clinical Research, Department of Orthopaedic Surgery, School of Medicine, University of Pittsburgh, Pittsburgh, PA, irrgangjj@msx.upmc.edu.
Katherine Verdolini Abbott, Professor, Department of Communication Science and Disorders; Professor, Department of Otolaryngology, University of Pittsburgh, Pittsburgh, PA, kittie@csd.pitt.edu.
Stephen R. Wisniewski, Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA, wisniew@edc.pitt.edu.
Anthony Delitto, Professor and Chair, Department of Physical Therapy, School of Health and Rehabilitation Sciences, University of Pittsburgh, Pittsburgh, PA, delitto@pitt.edu.
REFERENCES
- 1.Bigos S, Bowyer O, Braen G. Agency for Health Care Polilcy and Research PHS, U.S. Dept. of Health and Human Services, editor. Rockville, MD: 1994. Acute Low Back Problems in Adults. Clinical Practice Guideline No. 14. [Google Scholar]
- 2.Cunningham LS, Kelsey JL. Epidemiology of musculoskeletal impairments and associated disability. Am J Public Health. 1984;74:574–579. doi: 10.2105/ajph.74.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker BF, Muller R, Grant WD. Low back pain in Australian adults: prevalence and associated disability. J Manipulative Physiol Ther. 2004;27(4):238–244. doi: 10.1016/j.jmpt.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Hestbaek L, Leboeuf-Yde C, Engberg M, Lauritzen T, Bruun NH, Manniche C. The course of low back pain in a general population. Results from a 5-year prospective study. J Manipulative Physiol Ther. 2003;26(4):213–219. doi: 10.1016/s0161-4754(03)00006-x. [DOI] [PubMed] [Google Scholar]
- 5.Bigos S, Bowyer O, Braen G. Clinical Practice Guideline No. 14. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, U.S. Dept. of Health and Human Services; 1994. Acute Low Back Problems in Adults. [Google Scholar]
- 6.Anderson R, Meeker WC, Wirick BE, Mootz RD, Kirk DH, Adams A. A meta-analysis of clinical trials of spinal manipulation. J Manipulative Physiol Ther. 1992;15(3):181–194. [PubMed] [Google Scholar]
- 7.Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann Intern Med. 2003;138(11):871–881. doi: 10.7326/0003-4819-138-11-200306030-00008. [DOI] [PubMed] [Google Scholar]
- 8.Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4(3):335–356. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Koes BW, Assendelft WJ, van der Heijden GJ, Bouter LM. Spinal manipulation for low back pain. An updated systematic review of randomized clinical trials. Spine. 1996;21(24):2860–2871. doi: 10.1097/00007632-199612150-00013. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence V. Spinal Manipulation for Low-Back Pain: A Meta-analysis. ACP JClub. 1993 Mar–April;118:49. [Google Scholar]
- 11.Mohseni-Bandpei MA, Stephenson R, Richardson B. Spinal manipulation in the treatment of low back pain: a review of the literature with particular emphasis on randomized controlled clinical trials. Phys Ther Rev. 1998;3(4):185–194. [Google Scholar]
- 12.Shekelle PG, Adams A. 1991; Santa Monica: RAND (R-4025/2-CCR/FCER) 1991. The Appropriateness of Spinal Manipulation for Low-Back Pain: Indications and Ratings by a Multidisciplinary Expert Panel. [Google Scholar]
- 13.Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH. Spinal manipulation for low-back pain. Ann Intern Med. 1992;117(7):590–598. doi: 10.7326/0003-4819-117-7-590. [DOI] [PubMed] [Google Scholar]
- 14.Bergmann TF. Various forms of chiropractic technique. J Chiro Tech. 1993;5(2):53–55. [Google Scholar]
- 15.Christensen MG, Kerkhoff D, Kollash MW. Job Analysis of Chiropractic. Greeley, CO: National Board of Chiropractic Examiners; 2000. [Google Scholar]
- 16.Christensen MG, Morgan DR. Job Analysis of Chiropractic. Greeley, CO: National Board of Chiropractic Examiners; 1993. [Google Scholar]
- 17.Taylor SH, Arnold ND, Biggs L, et al. A review of the literature pertaining to the efficacy, safety, educational requirements, uses, and usage of mechanical adjusting devices. Part 2 of 2. J Can Chiropr Assoc. 2004;48(2):152–179. [PMC free article] [PubMed] [Google Scholar]
- 18.Taylor SH, Arnold ND, Biggs L, et al. A review of the literature pertaining to the efficacy, safety, educational requirements, uses, and usage of mechanical adjusting devices. Part 1 of 2. J Can Chiropr Assoc. 2004;48(1):74–88. [PMC free article] [PubMed] [Google Scholar]
- 19.Fuhr AW, Colloca CJ, Green JR, Keller TS. Activator Methods Chiropractic Technique. St. Louis: Mosby; 1997. [Google Scholar]
- 20.Childs J, Piva SR, Fritz J. Responsiveness of the Numeric Pain Rating Scale in Patients with Low Back Pain. Spine. 2005;30(11):1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- 21.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–2953. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 22.Fritz J, Irrgang J. A Comparison of a Modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81(2):776–788. doi: 10.1093/ptj/81.2.776. 81. [DOI] [PubMed] [Google Scholar]
- 23.Hurwitz EL, Morgenstern H, Kominski GF, Yu F, Chiang LM. A randomized trial of chiropractic and medical care for patients with low back pain: eighteen-month follow-up outcomes from the UCLA low back pain study. Spine. 2006;31(6):611–621. doi: 10.1097/01.brs.0000202559.41193.b2. discussion 622. [DOI] [PubMed] [Google Scholar]
- 24.Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain. Phys Ther. 2001;81(10):1641–1674. [PubMed] [Google Scholar]
- 25.Bronfort G, Haas M, Evans R, Kawchuck G, Dagenais S. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine J. 2008;8(1):213–225. doi: 10.1016/j.spinee.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 26.Smeets RJ, Beelen S, Goossens ME, Schouten EG, Knottnerus A, Vlaeyen JW. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive behavioral treatment in chronic low back pain. Clin J Pain. 2008;24(4):305–315. doi: 10.1097/AJP.0b013e318164aa75. [DOI] [PubMed] [Google Scholar]
- 27.Miller FG, Kaptchuk TJ. The power of context: reconceptualizing the placebo effect. J RSoc Med. 2008;101(5):222–225. doi: 10.1258/jrsm.2008.070466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol. 2008;59:565–590. doi: 10.1146/annurev.psych.59.113006.095941. [DOI] [PubMed] [Google Scholar]