Abstract
This article examines social stratification in individual health trajectories for multiple cohorts in the context of China’s dramatically changing macro-social environment. Using data from the China Health and Nutrition Survey, we find significant socioeconomic status (SES) differences in the mean level of health and that these SES differentials generally diverge over the life course. We also find strong cohort variations in SES disparities in the mean levels of health and health trajectories. The effect of education on health slightly decreases across successive cohorts. By contrast, the income gap in health trajectories diverges for earlier cohorts but converges for most recent cohorts. Both effects are more pronounced in rural areas. Given that these cohort effects are opposite those reported in recent U.S. studies, we discuss China’s unique social, economic, and political settings. We highlight the association between SES and health behaviors, China’s stage of epidemiologic transition, and the changing power of the state government and its implications for health care.
Keywords: socioeconomic status, health disparity, social change, cohort, life course
Throughout the twentieth century, massive social changes swept through many countries around the world. Along with the two World Wars, the United States saw the Great Depression, the Cold War, and the Civil Rights movement. Across the globe, Chinese society went through a series of dramatic political, economic, and cultural upheavals, including the Communist Revolution (late 1940s), the Great Leap Forward and Famine (late 1950s), the Cultural Revolution (mid-1960s to 1970s), and the introduction of the post-Mao economic reforms (late 1970s to present). For sociologists interested in the linkage between social change and social stratification, the volatility of China’s social surroundings, as well as the dominance of a powerful state socialist government, makes the country a unique and valuable resource for study.
In this article, we focus on the social stratification of individual health trajectories in the context of China’s ever-changing macro-social environment. We address the longstanding issue of social inequality and health, which extends back to the early Chicago school researchers Faris and Dunham (1939) and their work on socioeconomic status (SES) and mental disorders. The vast amount of literature since then documents a consistently positive relationship between SES and health. People with higher SES are more likely to report better health, greater levels of physical functioning and mobility, better mental health outcomes, and lower rates of disability and mortality (Kitagawa and Hauser 1973; Marmot 1999; Rogers, Rogers, and Belanger 1992; Turner, Wheaton, and Lloyd 1995). The seemingly universal relation between SES and health is clouded, however, when put in the context of aging and the life course; some prior studies report a convergence of health inequality by SES, while others demonstrate a persistent or diverging gap in health between the socioeconomically advantaged and disadvantaged in later life. Scholars have attributed this inconsistency in U.S. studies to confounding an age effect (the effect of SES on health over the individual life course) with a cohort effect (a changing SES effect on health across birth cohorts who came of age at different historical times) in cross-sectional designs (Lynch 2003; Yang 2007). The crux of the problem, however, is not merely methodological or data related, but rather conceptual. Birth cohorts serve as a proxy for the historical times in which individuals were exposed. Failure to account for cohort structure in studying the relationship between SES and health over the life course amounts to ignoring the influence of social change on human lives.
The need to disentangle life course and cohort processes in the study of social inequality in health is particularly evident in China, where large-scale societal transitions dominated the past 60 years and had long-lasting effects on the country’s social order. For example, in Maoist China, the state government actively promoted the social ideal of a “classless society,” resulting in decreased differentials in income and social services since 1949 and low socioeconomic stratification by international standards. In terms of policies, a massive public health campaign since the 1950s helped reduce health differentials and led to an exceptionally accelerated model of mortality and health transitions. This trend later reversed, as market reform after the 1980s generated astounding growth in income inequality. At the same time, the government’s health insurance and health care systems, which were established in the prereform era and provided a comprehensive level of basic health care in both urban and rural areas, became increasingly dysfunctional given pressure from privatization and sharply reduced government support. While these state policies affected the social stratification of health outcomes at different points in time, the extent of their influence may vary considerably for different birth cohorts who came of age at different historical times. Cohort membership thus potentially offers crucial evidence of varying macro-social influences on individuals at different life stages.
Using a five-wave dataset spanning 13 years (China Health and Nutrition Survey [CHNS] 1991, 1993, 1997, 2000, 2004), we carry out the first longitudinal study of changes in socioeconomic differentials in health for multiple cohorts of individuals in China. We investigate how health trajectories are shaped by recent socioeconomic and health transitions, and how historical events may leave different imprints on successive cohorts’ life experiences and, consequently, lead to diverging health outcomes. Our goal is to advance our understanding of the mechanisms that generate inequality in health in a society undergoing rapid change in its social structure and health parameters. In particular, we underscore the prominent role of the state government. A large body of sociological research examines the impact of the transformation of China’s state socialist economy on social stratification and mobility, with an emphasis on economic well-being, such as earnings, income, occupation, and wealth (e.g., Bian 2002; Bian and Logan 1996; Lin and Bian 1991; Nee 1989; Wu and Xie 2003; Zhou 2000). Relatively little is known, however, about how such transitions affect health stratification, a type of social inequality that deserves academic as well as public attention.
THEORETICAL PERSPECTIVES
Does social inequality in health change with age? And how is this process shaped by an ever-changing social-historical context? This study is guided by the life course perspective, which provides an excellent framework for studying the relationship between human lives and a rapidly changing society such as China. By studying both age and cohort effects on individuals’ health, we capture the imprint of time on human lifespans at personal and social-historical levels.
We begin by first addressing the process of aging from the perspective of cumulative disadvantage theory. Originating from the status attainment literature and studies of scientific careers (Merton 1968), cumulative disadvantage theory has found fruitful applications in aging and life course research to characterize the processes by which the effects of initial disadvantages in educational attainment and income accrue over the life span to produce high levels of late-life inequality (O’Rand 2006). Described by O’Rand (2006) as “forms of life course capitals,” economic, health, and personal resources accumulate over the life course. By selection and interaction with various societal institutions through complex processes, even small initial differences in life course capital can result in wide disparities in outcomes. The cumulative disadvantage process emphasizes the depreciation of life course capital over time, through cumulative hardship and adversity, for those with early disadvantages and lower achievements.1 Health trajectories are shaped through a chain of life course “insults” (Hayward and Gorman 2004) and strong path dependence, whereby a disadvantage increases the risk of early hardships, such as poor health and lower educational attainment and economic status, that constrain subsequent socioeconomic attainment and health maintenance (O’Rand 2002, 2006).
Studies on health disparities over the life course find evidence of cumulative disadvantage in which the effects of early and sustained hardship lead to self-reinforcing patterns of physical decline, as manifested by higher rates of disability and mortality in later life (Lynch, Kaplan, and Shema 1997; Smith and Kington 1997) and health problems such as obesity (Ferraro and Kelley-Moore 2003), hypertension, heart disease, and cognitive decline (Dupre 2007, 2008; Rodgers, Ofstedal, and Herzog 2003). Empirical tests, however, also show inconsistent findings with respect to whether the SES effects on health outcomes strengthen or diminish over the life course. Education and income gaps in health have been found to either diverge (Power, Matthews, and Manor 1998; Ross and Wu 1996; West 1991; Willson, Shuey, and Elder 2007), converge (Feldman et al. 1989; House, Kessler, and Herzog 1990; House et al. 1994), remain stable (Clark and Maddox 1992), or diverge from early to middle age and then converge in old age (House, Lantz, and Herd 2005).
Although this body of research explicitly employs a cumulative disadvantage/advantage framework for addressing health differentials in the life course, it hinges largely on cross-sectional studies with no intracohort cross-time linkages. It thus cannot adequately test the cumulative disadvantage theory of intracohort differentiation. Several recent U.S. studies have begun to tease out the process of aging from cohort differences by using longitudinal designs; they report substantial intercohort differences in health (Yang 2007) and patterns of increasing intracohort disparity in health with age (Lynch 2003; Willson et al. 2007). One study also finds constant intracohort disparity in health trajectories, showing African Americans’ persistent disadvantage (Yang and Lee 2009). Together, these studies lend support to the cumulative dis/advantage theory.
Although systematic examination of trajectories of inequality within and between cohorts has begun, knowledge of the cumulative disadvantage process in other national settings is limited. Examining the SES-health gradient over the life course is crucial in nations such as China, where social, economic, and political transitions dominated the second half of the twentieth century. This leads to a second research question: How does social change influence health disparities as individuals age? The interplay of human lives and historical times is central to the life course framework (see Elder, Johnson, and Crosnoe 2003). Historical times may affect a person’s life course in terms of a cohort effect, with social change differentiating the life course patterns of successive cohorts. Cohort effects on health may be due to differentials in early life conditions, a commonly cited explanation for susceptibility to diseases and mortality in the epidemiological research on chronic diseases (Barker 1998). Similarly, cohort changes may reflect shifts in individual health capital since birth. More recent cohorts in the United States tend to have better health capital at birth and lower depreciation rates in the stock of health capital (Fogel and Costa 1997). Furthermore, successive U.S. birth cohorts experience later onset of chronic diseases and disabilities (Freedman and Martin 1998).
Different cohorts could also have diverse life experiences due to “the timing of lives,” (Elder et al. 2003:12) another closely related life stage principle. In Elder’s seminal work on the children of the great depression, he demonstrates convincingly that economic loss and deprivation early in life for the Oakland cohort (born in 1920 to 1921) did not have the same magnitude of effect on physical and emotional health across different social classes; the most socioeconomically disadvantaged experienced the most adverse effects on adult health (Elder [1974] 1999). Interestingly, when compared with a slightly younger cohort (born in 1928 to 1929) who were more adversely influenced by family hardship, the Oakland males were more resilient in later life, owing possibly to military service and its benefits (Elder 1986, 1987). Clearly, individuals feel the impact of social change differently, depending on where they are in their lives.
RESEARCH ON SES AND HEALTH IN CHINA AND OTHER ASIAN COUNTRIES
Although there are only a few studies that document the relationship between SES and health in contemporary China, their findings are inconsistent and vary by type of health outcome and measures of SES. Some studies report that people in higher education and income groups have better self-reported health and experience lower rates of chronic disease (Li and Zhu 2006; Wu et al. 2004). Other studies find wide socioeconomic disparities in functional health and old-age disability among older adults, with educational attainment exerting a beneficial influence on both functional decline and recovery from disability (Beydoun and Popkin 2005; Liang, Liu, and Gu 2001). However, one study on the oldest old in China documents that education is not strongly associated with the dynamics of disability (Gu and Zeng 2004). Moreover, studies on China’s adult population report paradoxical findings, in that higher SES standing is positively associated with increased health risks, such as smoking, heavy alcohol consumption, and a poor diet (Du et al. 2002; Kim, Symons, and Popkin 2004). Similarly, Zimmer and Kwong (2003) found a positive association between SES and the prevalence of chronic conditions. The positive link between SES and health also appears in several other Eastern and Southeastern Asian societies, including Taiwan (Chiu et al. 2005; Zimmer, Hermalin, and Lin 2002), Japan (Fukuda, Nakamura, and Takano 2004; Liang et al. 2002), Thailand (Zimmer and Amornsirisomboon 2001), and Malaysia (Wu and Rudkin 2000). Studies reveal that higher SES is associated with a higher risk for heart disease, myocardial infarction, and obesity in Korea (Song et al. 2006; Yoon, Oh, and Park 2006) and Hong Kong (Wong and Donnan 1992).
Our study contributes significantly to the existing body of literature on SES and health in China. Although most previous research focuses on the older population to understand aging as a lifelong process and to explain the SES gradient in health that occurs early in adult life, the present study investigates the complete age span of the adult population. In addition, with ongoing socioeconomic transitions sweeping through China, we address not only the question of how rising inequality may affect health outcomes and behaviors, but how the SES effect may vary for individuals who come of age in different social-historical contexts. Given the major episodes of social unrest and transitions from the 1940s to the present, we argue it is vital to understand health disparities in a cohort-specific context. Therefore, we examine interactions among age, cohort, and SES using a longitudinal data design to offer greater insight into the social stratification of health among Chinese adults.
RESEARCH HYPOTHESES
We test cumulative disadvantage theory by modeling SES differentials in growth trajectories of health within cohorts (i.e., the age by SES interaction effects net of cohort effects). By following multiple birth cohorts over multiple time points, we intend to capture the varying effect of SES on health by age and simultaneously assess the effects of intracohort and intercohort differentiations. This leads to our first hypothesis:
Hypothesis 1 (Intracohort variation): Socioeconomic disparities in health will increase over the life course within cohorts, net of cohort effects.
We also investigate the hypothesis of intercohort changes in intracohort inequalities by modeling variations in SES disparities in health trajectories across birth cohorts (i.e., three-way interactions between cohort, age, and SES). We are especially interested in how recent socioeconomic transformations and health transitions in China have affected cohorts’ changes in health over time. During the past two decades of economic reforms, China has experienced phenomenal economic growth, which has not only improved average living standards but has also generated pronounced economic disparities. Rising income inequality, together with the collapse or dysfunction of government health insurance schemes and reduced funding of public health programs, generated widely unequal access to health care. Growing inequality in health care access may have strong implications for the health trajectories of earlier cohorts born in the 1930s and 1940s, who entered old age in the 1990s (the beginning of our observation window). On the other hand, although more recent cohorts (born in the 1950s and 1960s) benefited from the mass public health campaigns during their childhoods, experiences in their adult lives may have negative effects. Typical for a developing society experiencing health transitions, the socioeconomically advantaged tend to adopt unhealthier lifestyle choices, resulting in a diet high in fat and sugar intake, less physical exercise, and an increasing prevalence of smoking, drinking, and obesity.
Given these social trends unique to the China context, we expect to find cohort-specific health trajectories by socioeconomic status. We also expect that the pattern is different from that in a developed country. This leads to our second hypothesis:
Hypothesis 2 (Intercohort change): Substantial intercohort variations in intracohort heterogeneity in health trajectories will exist over the life course, with socioeconomic differentials in the age trajectories of health possibly decreasing in successive cohorts.
We hypothesize that the interaction effect between SES and cohort on health trajectories will differ by rural and urban residence. The divide between rural and urban China is one of its most salient features. The Hukou (household registration system) divides the population into agricultural and nonagricultural sectors, which in turn have different social and economic systems. By the early twenty-first century, the difference in living standards and access to health care between urban and rural areas yielded an average advantage of five years in life expectancy for urban residents (Wang and Mason 2007). We thus expect urban residents to have better health than their rural counterparts and that the pattern of intercohort variations in socioeconomic differentials in health trajectories will be different in urban and rural China. In the pre-reform era, the urban population enjoyed guaranteed employment, housing, access to health care, and retirement benefits. The market transition that began in the 1980s brought major challenges to the health care system in urban China, as stateowned enterprises became responsible for their own benefits and losses. The government initiated new health care system reform policies, limiting the public funds available for health care and allowing private ownership of health facilities and clinical practices (Rosner 2004). Escalating medical costs worsened rural residents’ living and health conditions considerably, particularly for older adults who are more likely to use health care facilities. However, in contrast to the near collapse of the rural cooperative medical scheme (CMS), which facilitated remarkable health improvements from the 1950s through the 1970s for rural populations, reforms were modest. Therefore, given the dramatic increase in inequality in health care access in rural areas, we expect that the effect of SES on health will be stronger for earlier cohorts in the rural population. Because of these differences, we conduct separate analyses for urban and rural subsamples. This leads to our third hypothesis:
Hypothesis 3: The patterns of cohort variations in the SES differentials of health trajectories will differ in urban and rural areas, with the SES gap more pronounced in the rural sample for earlier cohorts.
DATA
We use data from the China Health and Nutrition Survey (CHNS), an ongoing collaborative project of the Carolina Population Center at the University of North Carolina, the Institute of Nutrition and Food Hygiene, and the Chinese Academy of Preventive Medicine in Beijing. The survey was designed to study how social and economic transformations in Chinese society affect the nutritional, demographic, and health status of the population. It has collected panel data on individuals, households, and their communities. The survey covers nine provinces and autonomous regions in China: Liaoning, Heilongjian, Shandong, Jiangsu, Henan, Hubei, Hunan, Guangxi, and Guizhou.2 One third of China’s population (approximately 450 million people in 1989) live in these provinces, which vary substantially in geography and economic development. The sample has a stratified multistage cluster design whereby in each province, low-, middle-, and high-income counties were selected, and subsequently within them, the county seat and three randomly chosen villages were selected. Also, in each province, the provincial capital, a low-income city, and suburban villages located near these cities were included. (A detailed description of the design of the China Health and Nutrition Survey can be found at http://www.cpc.unc.edu/projects/china.) Although the CHNS data are not a representative sample of China’s population, previous studies show that the characteristics of the CHNS households and individuals are comparable to those from national samples (see Du et al. 2002; Entwisle and Chen 2002; Short, Ma, and Yu 2000).
Although few longitudinal studies involve multiple follow-up surveys of adults in the United States, the CHNS has collected five waves of data so far (1991, 1993, 1997, 2000, and 2004).3> This creates a unique opportunity for cohort analysis of age change. We selected a sample of adults age 21 and older in 1991 as the baseline and constructed 10-year birth cohorts. The only exceptions are the 1951 to 1955 and 1956 to 1960 cohorts, which were separated because of the historical significance of the Great Leap Forward and the Three-Year Famine, both of which occurred in the late 1950s. We then followed the six birth cohorts to later survey years (1993, 1997, 2000, and 2004). Respondents’ age in 1991 ranges from 21 to 101 years. At each follow-up, surviving respondents in each cohort aged together, yielding cohort-specific age trajectories.
The CHNS collects extensive information, including health outcomes, measures of health behavior, and access to health care. The survey asked the following question of each household member regarding their health: “How would you describe your health compared to that of other people your age?” The responses range from 1 to 4, indicating excellent to poor health.4 Respondents who answered “refuse to answer” and “do not know” were coded as missing and dropped from our analysis, and we reverse coded self-rated health so that higher values indicate better health. We use self-reported health as our main dependent variable. In U.S. studies, it has been consistently documented as a valid measure of health (Farmer and Ferraro 1997; Hays, Schoenfeld, and Blazer 1996; Johnson and Wolinsky 1993) and as a potent predictor of survival and mortality, even when objective measures of health based on physicians’ examinations, medical records, or extensive health histories are controlled (Idler and Angel 1990; Idler and Benyamini 1997). In addition, self-rated health is a broader and more inclusive assessment of health, capturing an individual’s health status beyond that of objective measures of health (Idler and Benyamini 1997). Having said that, we acknowledge that the construct of self-reported health reflects subjective perceptions and thus is affected by individual characteristics and cultural contexts (Desesquelles, Egidi, and Salvatore 2009; Jylhä et al. 1998). Because of this, we cross-validated the findings presented below by using alternative health measures such as physical functioning. These results are available from the first author upon request.
Our working sample consists of 7,432 individuals in 1991, 6,717 in 1993, 6,991 in 1997, 6,494 in 2000, and 6,648 in 2004.5> Among them, 617 individuals died by the end of 2004. From one wave of the survey to the next, loss due to follow-up ranges from 2 to 8 percent. Altogether, these respondents yield 34,282 person-year records. Because individuals remaining in the sample are likely to be healthier, and the disadvantaged are more likely to die earlier, the effect of SES on health may be overestimated. Below, we explain our approach to handling the potential bias in the analysis due to attrition and death.
The CHNS not only includes basic questions on education but also elicits detailed information on income from different sources. Based on preliminary analyses, we use two different measures of SES: education and per capita family income. In preliminary analyses, we also tested for different specifications of these two variables and conducted sensitivity tests. To simplify the interpretation, we use two dichotomous variables in the final analyses. We operationalize education as those with primary school or less (= 0) and those with more than primary school (= 1). We divide respondents into the lowest quintile of the income distribution (= 0) and those who have higher incomes (= 1).
While urban and rural residency may affect the mean level of health and growth rate of health problems, we also control for regional differences in economic development with regional dummy variables: coastal (Shandong and Jiangsu, the two most economically developed provinces); Northeast (Liaoning and Heilongjian); inland (Henan, Hubei, and Hunan); and the mountainous south region (Guangxi and Guizhou), also the most economically underdeveloped region, as the reference category. The CHNS provides information on health behaviors, including smoking, drinking, and Body Mass Index (BMI as a proxy for diet) derived from height and weight. Our analytic models control for these health behaviors, gender, and marital status. Table 1 presents summary statistics of all variables used in the analyses for all waves combined. The urban and rural samples are similar in their average level of self-reported health and some other characteristics. As expected, urban residents enjoy higher education and income levels than do their rural counterparts.
Table 1.
Descriptive Statistics of All Variables in the Analyses (N = 34,282)
| Whole Sample (N = 34,282) |
Urban (N = 10,120) |
Rural (N = 24,162) |
||||
|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | Mean | SD |
| Self-Rated Health | 2.73 | .74 | 2.75 | .75 | 2.73 | .73 |
| Age | 46.32 | 13.60 | 47.18 | 14.15 | 45.91 | 13.20 |
| Birth Cohort (0 to 5) | 2.92 | 1.67 | 2.80 | 1.76 | 2.97 | 1.63 |
| Education (more than primary school = 1, primary school or less = 0) |
.49 | .50 | .66 | .47 | .42 | .49 |
| Family Income (lowest quintile = 0, else = 1) |
.80 | .40 | .91 | .28 | .75 | .43 |
| Urban (urban = 1, rural = 0) | .30 | .46 | ||||
| Region | ||||||
| Northeast (Northeast = 1, else = 0) | .14 | .35 | .14 | .34 | .14 | .35 |
| Coastal (coastal = 1, else = 0) | .23 | .42 | .22 | .42 | .24 | .43 |
| Inland (inland = 1, else = 0) | .36 | .48 | .38 | .48 | .35 | .48 |
| (Reference category: mountainous south) |
.26 | .44 | .26 | .44 | .26 | .44 |
| Sex (male = 1, female = 0) | .49 | .50 | .50 | .50 | .49 | .49 |
| Died (died = 1, not died = 0) | .04 | .20 | .04 | .19 | .04 | .21 |
| Marital Status (married = 1, not married = 0) |
.88 | .33 | .86 | .35 | .88 | .32 |
| Smoking (smoking = 1, not smoking = 0) |
.33 | .47 | .31 | .46 | .34 | .47 |
| Drinking (drinking = 1, not drinking = 0) |
.38 | .49 | .39 | .49 | .37 | .48 |
| Body Mass Index | 22.52 | 3.31 | 23.18 | 3.48 | 22.24 | 3.19 |
ANALYTIC STRATEGY
Because the design of the CHNS follows multiple age cohorts for multiple waves (Tonry, Ohlin, and Farrington 1991), it allows for more rapid accumulation of information on age for multiple cohorts than does a single longitudinal cohort design. The data have restricted coverage of the individual life course for each cohort because complete life histories of all cohorts from birth to death are rarely available, if they exist at all. If the observable age trajectories of different cohorts start and end at different ages, comparison of different cohorts must be based on different segments of the cohort members’ life course. As waves of data accumulate, however, age and cohort will become less and less confounded, making it increasingly possible to estimate cohort-specific age trajectories. Miyazaki and Raudenbush (2000) and Raudenbush and Bryk (2002) illustrate that hierarchical linear models (HLM) or growth curve models can be used to test for cohort differences in age trajectories. Using U.S. datasets, this modeling reveals significant cohort variations in the age trajectories of health (Lynch 2003; Willson et al. 2007; Yang 2007; Yang and Lee 2009). We apply this modeling strategy to the CHNS, because with more waves of data than most U.S. studies, it offers more power to test aging and cohort related hypotheses.
We specify two-level hierarchical linear models to estimate age trajectories of health and heterogeneity in these trajectories by cohort and SES.
Level-1 Model:
| (1) |
Level-2 Model:
Model for the intercept:
| (2) |
Model for the linear rate of change (age):
| (3) |
The level-1 model characterizes within-individual change over time, or individual growth trajectories with age. In this model of repeated measurement within individuals, the response variable yti for person i at time t is modeled as a function of linear and quadratic terms of age for person i at time t. The coefficients β0i, β1i, and β2i represent the intercept or mean level, the linear rate of change, and the quadratic rate of change with age, respectively. Following the HLM methodological literature, we center the age variable around , the median age of the cohort to which person i belongs (Miyazaki and Raudenbush 2000; Raudenbush and Bryk 2002). This operationalization has several advantages. First, it allows us to interpret intercept and growth rate as the average level of health and rate of growth at the median age of the cohort during the data collection period. Second, it minimizes the correlation between age and age squared and stabilizes the estimation procedure. Third, centering around cohort-specific median ages prevents bias in the estimate that arises from systematic variation in mean age across the cohorts. Hence, it eliminates confounding of age and cohort variables.
The goal of the level-2 analysis is to detect heterogeneity in change across individuals and to determine the association between predictors (SES, cohort, and urban/rural residency) and the shape of each person’s growth trajectory. The level-2 model assesses inter-individual differences in change with age, or whether individuals with different SES from various cohorts manifest different patterns of within-individual change. Each of the parameters of age trajectories, β0i, β1i, and β2i, is further modeled as functions of person-level attributes. The associated coefficients of these covariates are denoted as γ, where γ00– γ04 are coefficients for the intercept model that includes the main effects of SES indicated by education and income, cohort (coded as 0 – 5),6 SES by cohort interaction effect, and urban residence. Note that γ10 – γ14 are the corresponding coefficients for the linear rate of change model, and they are equivalent to interaction effects of age with the above covariates. We tested a similar model for the quadratic rate of change but omitted it. We entered control variables at level-1 for time-varying covariates (marital status, smoking, drinking, and BMI centered around mean) and at level-2 for time-constant covariates (sex, attrition type, and region). The random within-person error term, eti, is assumed to be normally distributed, and the level-2 residual random errors, u0i and u1i, have a multivariate normal distribution.7
The CHNS data span 13 years and might exhibit period effects on health. We do not explicitly incorporate period effects in our analysis for both methodological and substantive reasons. In a longitudinal design, repeated observations over time for each individual are recorded in the form of a person-year dataset. A fundamental feature of a person-year dataset is that it contains one time indicator—age or wave (period)—that identifies the specific time of measurement. In growth curve models, the level-1 analysis reflects within-individual change by modeling the outcome as a function of the chosen time indicator (Singer and Willett 2003). This means that one can choose to include age or wave depending on substantive focus, but not both because within individuals age and period are perfectly collinear.8 We do not estimate period effects per se, but focus instead on the age by cohort interaction effects (γ12 and γ13). Because cohorts vary in age at any historical moment, effects associated with historical time, if any, tend to produce cohort differences in the age-outcome relationship.
Nonrandom selection may occur if mortality and nonresponse are significantly correlated with worse health, producing biased sample estimates of health trajectories. We considered various methods to deal with the potential selection bias. Because the Heckman two-step selection correction and some other techniques do not appear to offer universal or predictable rescue for this problem (Stolzenberg and Relles 1997; Winship and Mare 1992), we use a more intuitive approach suitable for our particular empirical analysis. The nonrandom selection occurs in our data through attrition. HLM allows data to be unbalanced across time because it includes all persons when estimating trajectories, irrespective of attrition status or number of waves in a person-year dataset (Raudenbush and Bryk 2002). This largely reduces the number of cases lost to followup and alleviates the sample selection problem common in other regression models that exclude cases lost to follow-up. In addition, instead of requiring a sample of respondents who have complete data for all waves, our model allows for the inclusion, and hence identification, of individuals who died or became nonrespondents at any follow-ups. The problem is to distinguish the health trajectories of those who had missing data in later waves from those who did not. A simple but effective solution is to control for attrition type directly in the level-2 model. Therefore, by entering dummy variables indicating the deceased and nonrespondent identities, we account for the possibility that respondents lost due to mortality or nonresponse had poorer health than the survivors with complete data. We performed all statistical analyses using SAS 9.1 (Littell et al. 2006).9
RESULTS
Table 2 presents findings from the estimation of growth curve models. We conducted analyses for each of the two SES indicators—education and family income—separately, first in consideration of their high correlations with each other and then simultaneously for both. Because the results are largely consistent, Table 2 presents only results from the analysis using both indicators; we report any differences from the separate analyses in the text below.
Table 2.
Growth Curve Models of Aging, SES, and Cohort Effects on Health in China (N = 34,282)
| Whole Sample |
Urban |
Rural |
p Value for Z Test |
|||||
|---|---|---|---|---|---|---|---|---|
| Fixed Effects | Model 1 Coef. | Model 2 Coef. | Model 3 Coef. | Model 4 Coef. | Model 5 Coef. | Model 6 Coef. | Model 7 Coef. | Models 6 and 7 |
| For Intercept | ||||||||
| Intercept | 2.57*** (226.21) |
2.29*** (167.86) |
2.27*** (118.07) |
2.27*** (116.84) |
2.20*** (97.46) |
2.28*** (49.57) |
2.28*** (106.61) |
94 |
| Education (≤primary = 0) |
.27*** (21.61) |
.05*** (4.63) |
.09*** (3.96) |
.08*** (3.80) |
.05* (2.30) |
.07* (1.98) |
.11*** (3.60) |
.46 |
| Income (lowest 20 percent = 0) |
.05*** (5.54) |
.07*** (6.86) |
.07*** (3.41) |
.06*** (3.29) |
.05** (2.61) |
.05 (1.09) |
.08*** (3.63) |
.56 |
| Cohort | .11*** (34.38) |
.12*** (19.50) |
.12*** (19.55) |
.11*** (18.76) |
.11*** (6.61) |
.12*** (18.34) |
.43 | |
| Education × Cohort | −.01* (−1.97) |
−.01* (−2.02) |
−.00 (−.72) |
.01 (.67) |
−.02** (−2.88) |
.04 | ||
| Income × Cohort | .00 (.13) |
.00 (.14) |
−.00 (−.00) |
.01 (.58) |
−.00 (−.67) |
.42 | ||
| Urban | .02 (1.46) |
.01 (1.12) |
||||||
| Northeast | .14*** (9.43) |
|||||||
| Coastal | .21*** (15.88) |
|||||||
| Inland (Reference category: mountainous south) |
.05*** (4.52) |
|||||||
| For Linear Growth Rate | ||||||||
| Intercept | −.27*** (−14.89) |
−.30*** (−14.00) |
−.35*** (−11.20) |
−.36*** (−11.20) |
−.37*** (−11.12) |
−.30*** (−4.03) |
−.37*** (−10.49) |
.47 |
| Education (≤primary = 0) |
.09*** (6.03) |
.05** (3.05) |
.09* (2.46) |
.09* (2.42) |
.08* (2.24) |
.08 (1.37) |
.09+ (1.83) |
.90 |
| Income (lowest 20 percent = 0) |
.03 (1.40) |
.01 (.60) |
.07* (2.02) |
.07* (1.97) |
.06+ (1.67) |
.02 (.30) |
.08* (2.07) |
.52 |
| Cohort | .02*** (3.66) |
.04*** (3.97) |
.04*** (4.00) |
.03** (2.76) |
−.01 (−.37) |
.05*** (4.40) |
.04 | |
| Education × Cohort | −.01 (−1.05) |
−.01 (−1.08) |
−.01 (−.97) |
−.01 (−.26) |
−.01 (−.86) |
.81 | ||
| Income × Cohort | −.02* (−2.05) |
−.02* (−2.05) |
−.02* (−1.97) |
.03 (1.16) |
−.03** (−2.64) |
.03 | ||
| Urban | .01 (.58) |
.02 (1.11) |
||||||
| Northeast (mountainous south) |
.07** (2.79) |
|||||||
| Coastal (mountainous south) |
.07*** (3.33) |
|||||||
| Inland (mountainous south) |
.07*** (3.48) |
|||||||
| For Quadratic Growth Rate | ||||||||
| Intercept | −.08*** (−6.02) |
−.07*** (−5.44) |
−.07*** (−5.29) |
−.07*** (−5.28) |
−.06*** (−4.64) |
−.05* (−2.25) |
−.07*** (−4.84) |
.46 |
| Control Variables | ||||||||
| Died | −.34*** (−15.40) |
−.18*** (−8.46) |
−.18*** (−8.25) |
−.18*** (−8.23) |
−.16*** (−7.22) |
−.14** (−3.22) |
−.20*** (−7.74) |
.25 |
| Sex (female = 0) | .06*** (6.39) |
.10*** (10.46) |
.10*** (10.37) |
.10*** (10.41) |
.04** (3.22) |
.08*** (4.64) |
.10*** (9.49) |
.20 |
| Married | .02 (1.37) |
|||||||
| Smoking | .04*** (3.41) |
|||||||
| Drinking | .07*** (7.48) |
|||||||
| BMI | .01*** (8.99) |
|||||||
| Random-Effects Variance Components | ||||||||
| Level-1: within-person | .11*** | .09*** | .09*** | .09*** | .07*** | .09*** | .09*** | |
| Level-2: in intercept in linear growth rate |
.04*** .07*** |
.03*** .07*** |
.03*** .07*** |
.03*** .07*** |
.03*** .07*** |
.03*** .07*** |
.04*** .07*** |
|
| Goodness-of-fit | ||||||||
| BIC (smaller is better) | 73,147.70 | 72,014.30 | 72,036.80 | 72,048.30 | 71,593.70 | 21,500.50 | 50,614.90 | |
Note: t ratios are in parentheses.
p<.10
p<.05
p<.01
p<.001 (two-tailed tests).
We begin with Models 1 through 5, which refer to the whole sample, and successively add the variables for cohort, the interaction of cohort-by-education, the interaction of cohort-by-income, urban residence, and various control variables for the intercept and linear growth rate models. Models 6 and 7 essentially replicate Model 4,10 but separately for the urban and rural subsamples. We conduct Z tests of the difference between coefficients in the urban and rural samples (Cohen 1983) and highlight any p value less than .05, which suggests a statistically different effect in the subsamples (see the last column in Table 2).
SES Differentials within Cohorts
Models 1 and 2 strongly support Hypothesis 1: there exist significant SES differentials in health trajectories within cohorts, net of cohort differences. Model 1 shows the overall age trajectory of health, which has a mean of 2.57 and decreases at a rate of .27 units per 10 years of age, slowing at a rate of .08 with age, thereby exhibiting a quadratic pattern.11 There are strongly significant SES gradients in the intercept or mean level of health. Relative to the most disadvantaged (individuals with primary education or less and in the lowest income quintile), respondents with more than primary education and higher income levels have better self-rated health by units of .27 and .05, respectively. In addition, the educational differential in health increases with age (.09) because more educated individuals experience a less rapid decrement in health with age (−.18 = −.27 + .09).
Model 2 tests the intracohort variation and examines how controlling for cohort effects modifies the SES disparities in average health levels and growth rates (age change) shown in Model 1. More recent cohorts show both higher mean levels of health and less rapid declines in health with age. This supports our expectation that, similar to their U.S. counterparts, Chinese citizens do not experience a universal age pattern of health decline, but cohort-specific age patterns of health change. Controlling for cohort effects reduces the magnitude of the education effect on the intercept, suggesting that some of the educational differential in health found in Model 1 is actually due to birth cohort differences. Consistent with the prediction of the cumulative disadvantage theory, the education effect strengthens with age within cohorts, as indicated by the significant coefficient for education in the linear growth model in Model 2 and subsequent Models 3 through 5 with added controls. The income effect does not appear to change significantly with age in Model 2. In the analysis of income-only models and Models 3 through 5, however, we find similar and significant age-by-income interaction effects. Because the models control for selection effects due to deaths and nonresponses in the follow-up surveys, the increasing SES gaps in health with age are not downwardly biased by selective survival but reflect actual divergences in intracohort SES gaps in health with age.
SES Differentials across Cohorts
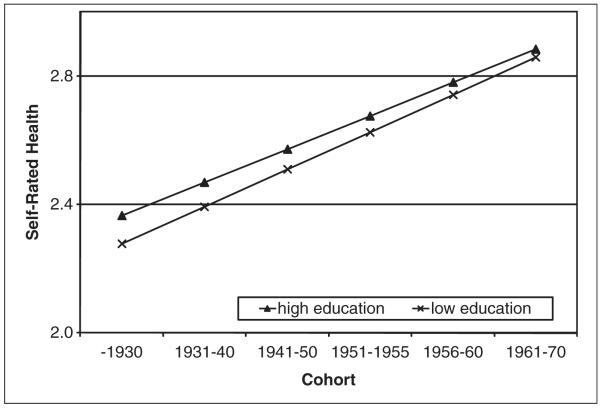
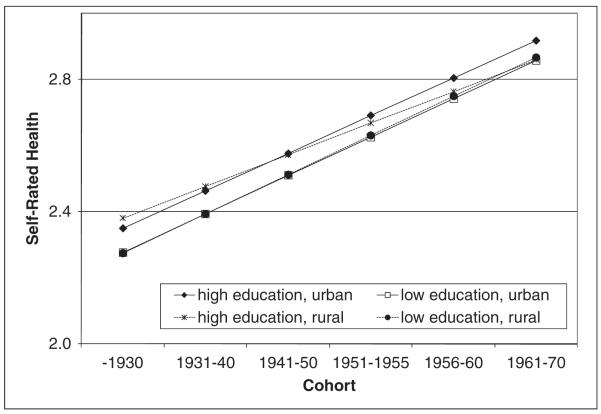
We also find support for Hypothesis 2: there are intercohort variations in intracohort SES disparities in health trajectories. Model 3 reports a significant cohort-by-education effect for the intercept model. To see the implication of this effect more clearly, we compare the predicted mean levels of selfrated health across cohorts by education based on estimates of Model 3 in Figure 1.12 This shows that the educational gap in mean levels of health slightly decreases across successive cohorts, consistent with Hypothesis 2. When separating the analyses by urban and rural subsamples, we find a significant difference in the cohort-by-education effect for the intercept model. As Figure 2 shows (based on estimates from Models 6 and 7 in Table 2), there is little difference in the predicted mean level of health for the low education group in the urban and rural samples. For respondents with higher education in the more recent cohorts, however, those in the rural sample have poorer health than their urban counterparts. While the educational gap in the predicted mean levels of health barely changes across cohorts in the urban sample, it almost disappears between the low and high education groups across cohorts in the rural sample. This supports Hypothesis 3, that is, the cohort varying effects of SES on mean levels ofhealth differ by rural and urban residence, with the SES gap decreasing in successive cohorts in rural but not urban areas.
Figure 1.
Educational Gap in Predicted Mean Levels of Self-Rated Health by Birth Cohort
Figure 2.
Educational Gap in Predicted Mean Levels of Self-Rated Health by Birth Cohort and Urban versus Rural Residence
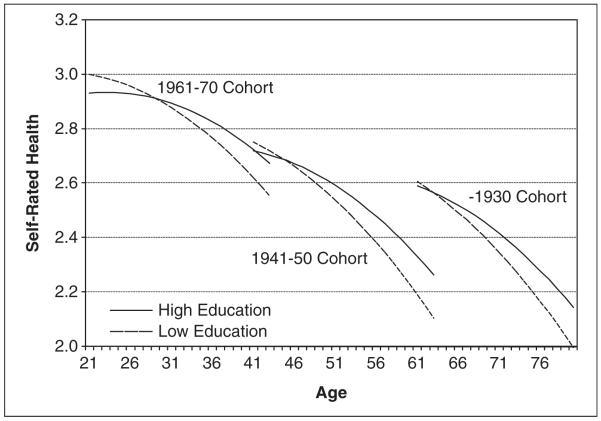
The results for the linear growth rate model suggest no significant three-way interaction among age, cohort, and education when all combinations of two-way interactions (cohort-by-education, age-bycohort, and age-by-education) are controlled. Because each two-way interaction effect is significant, however, there is some evidence for cohort differences in the way the educational gap changes with age, as suggested by Hypothesis 2. Figure 3 presents the predicted age trajectories of health-by-education levels for three selected cohorts in the whole sample.13 The pattern of divergence in the age trajectories of health is similar (with small differences in the degree of divergence) for each cohort, illustrating a cumulative disadvantage process over the life course.
Figure 3.
Educational Gap in Predicted Age Trajectories of Self-Rated Health by Birth Cohort
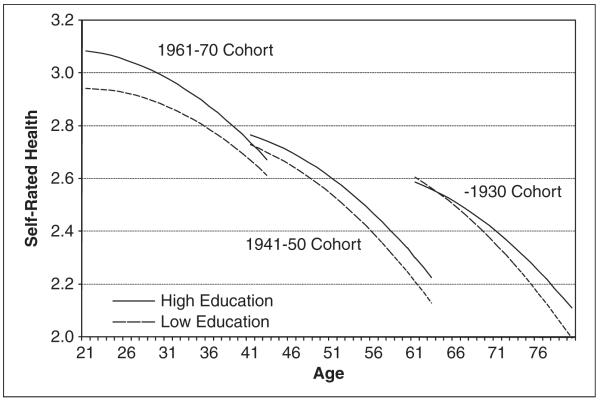
The results for cohort differences in the income gap in health trajectories are slightly different, however. Model 3 shows that cohort differences in the income gap do not exist in mean levels of health (and hence there is no significant cohort-by-income interaction effect in the intercept model), but they do exist in the rate of change of health. The significant income and cohortby-income interaction effects for the linear growth rate model (i.e., a three-way interaction among age, cohort, and income) indicate that the income gap diverges with age, but this trend of divergence lessens in successive cohorts. Figure 4 depicts how various cohorts differ in the way income differentials in health change with age. In support of Hypothesis 2, the within-cohort income gap does not uniformly increase across the life course but varies by cohort membership. While the income gap first diverges in the earliest cohort born before 1930, it becomes more constant in the 1941 to 1950 cohort, and then converges in the 1961 to 1970 cohort. Taken together, this shows a cumulative disadvantage process that gradually weakens in more recent cohorts.
Figure 4.
Income Gap in Predicted Age Trajectories of Self-Rated Health by Birth Cohort
In addition, we observe significant urbanrural differences in the effects of cohort and cohort-by-income interaction for the linear growth rate model. This supports Hypothesis 3; that is, the cohort varying SES effects on the age trajectories of health problems differ in urban and rural samples. The cohort-specific health trajectories in the rural sample appear very similar to those of the whole sample: the within-cohort income gap over the life course lessens for the more recent cohorts. For the urban sample, the cohort-by-income interaction is not significant in the linear growth rate model.
With urban residence added to the analyses in Model 4, all key effects mentioned above remain the same. As expected, urban residence is associated with better health across ages in analyses that separately estimate the education and income effects (results not shown), but not in Model 4, which simultaneously estimates education and income effects. This result suggests that part of the urban residence effect on health trajectories is mediated through education or income. As discussed above, when separating the urban and rural samples, we find some significant differences in the intercohort variations relating to the effect of SES on individual health trajectories, a finding that supports Hypothesis 3.
Finally, Model 5 shows that adjusting for all other factors that have been shown to correlate with health reduces the magnitudes of the education and income effects on the intercept and diminishes the statistical significance of the education-by-cohort interaction on the intercept.14 The net cohort effects on mean health levels and income differentials in health change with age remain. Using Bayesian Information Criteria (BIC) to assess goodness-of-fit across models, this final model has the smallest BIC statistics and thus is the best model fit.
As expected, the economically most developed region (Shandong and Jiangsuprovinces) has the highest mean health level, while the most underdeveloped region (Guizhou and Guangxi) has the lowest. Paradoxically, the effects of smoking, drinking, and BMI are positive in direction, reflecting the positive association between SES and these health behaviors in the overall sample. Although the model includes education and income as SES indicators, it may not fully capture all dimensions of SES. Furthermore, we do not include other proximate determinants of health that are positively associated with SES and have beneficial effects on health, such as nutrition, access to health care, exposure to stressors, and social support. Therefore, the positive effects of the included health behaviors may simply reflect the residual effects of SES on health, rather than true beneficial effects on health.
DISCUSSION AND CONCLUSIONS
Health differentials closely reflect one of many patterns of social inequality. The link between social inequality and health disparities provides a particularly useful line of inquiry into how individual lives evolve with social change. In this longitudinal study of stratification in health in China, we examine socioeconomic disparities in health over the adult life course. Amid political and economic instabilities in the early years of communist rule, remarkable socioeconomic restructuring since the late 1970s, and dramatic demographic and health transitions in the past several decades, it is critically important to understand the role of cohort change in shaping individuals’ life course trajectories. Taking birth cohort differences into account helps contextualize the process by which life course inequalities are generated and thus illuminates the dynamics between social change and individual lives. Our study offers evidence for the existence of large intercohort differences in health trajectories. Ignoring this source of variation would bias the relationship between SES, age, and health. Overall, our findings reveal strong SES gradients in health trajectories within cohorts and different patterns of SES disparities in health trajectories between cohorts.
Specifically, we find compelling empirical evidence of significant intracohort SES differences in the mean level of health and that SES differentials in health increase over the life course. Controlling for cohort effects, the models largely support cumulative disadvantage theory: the SES gap in health is wider at older ages than at younger ages. These findings are consistent with those in U.S. studies that depict a pattern of health decline as people age, and this cumulative process is affected by education and income. By influencing resources such as access to health care, health behavior, and social support, the cumulative effect of SES results in greater inequalities in health over the life course.
At the same time, we also find that the aging process of health change is not universal across cohorts. Instead, cohort variations in SES disparities exist in health trajectories. While this finding has been reported in empirical studies for individuals in the United States, the direction of the cohort effect in our China-based study is distinctively different. For example, our study documents that the effect of education on mean level of health decreases slightly across successive cohorts. In addition, we find that the income gap in health trajectories tends to diverge for earlier cohorts, but then converges for the most recent cohort. Both patterns are more saliently observed in the rural sample. By contrast, recent studies in the United States provide evidence for just the opposite (Lynch 2003; Willson et al. 2007).
What can possibly explain such reversed patterns in China and the United States? We believe that the answer lies in Chinese society’s unique social, economic, and political configurations. First, the differences may be due to how lifestyle choices mediate theeffect of SES on health. In developed countries such as the United States, higher SES groups tend to have healthier lifestyles, indicated by a healthier diet, more frequent exercise, and a lower prevalence of excessive smoking and drinking. In developing countries experiencing rapid economic development, however, the higher SES groups are often more likely to have unhealthy diets (characterized by higher fat levels and more added sugar), to be obese, to smoke and drink more, and to be sedentary (Du et al. 2002; Kim et al. 2004; Popkin 1998). With their rising purchasing power, the socioeconomically advantaged adopt these unhealthy behaviors because they view these choices as privileges. The most recent cohort (1961 to 1970) in the study is the first to benefit from China’s economic boom that started in the late 1970s. It is the first cohort exposed to a Western lifestyle, and they may have adopted some unhealthy behaviors associated with that lifestyle. For earlier cohorts, this is likely not the case. As a result, this may explain why the effect of SES on health is stronger for earlier cohorts and weaker for successive cohorts. That the pattern is more pronounced in the rural versus urban sample may also be explained by a stronger positive association between SES, smoking, and drinking in the rural sample (results not shown).
Second, difference in the cohort effect between China and the United States may reflect differences in their stages of epidemiologic transition. The United States, along with many other industrialized societies, is in the advanced stage of the transition (Olshansky and Ault 1986). Despite the recent re-emergence of infectious diseases such as AIDS, chronic and degenerative diseases have long replaced infectious diseases as the leading causes of death (Olshansky et al. 1998). By contrast, just three decades ago, China’s epidemiologic environment had high rates of infectious diseases and early mortality. With strong government intervention, China has made impressive improvements in public health since the 1950s. Rates of infectious diseases have declined decisively, accompanied by a rise in chronic diseases, which accounted for an estimated 80 percent of all deaths in 2005 (L. Wang et al. 2005). This accelerated model of a health transition clearly has different effects for the different cohorts included in this study (from pre-1930 to 1961 through 1970). In an earlier stage of the epidemiologic transition, where the prevalence of chronic diseases is on the rise, socioeconomic differentials in China are decreasing. In the United States, the SES gap in mortality rates initially widened when communicable diseases were dominant, with the higher SES group initially benefiting more from public health improvements. The SES gap then narrowed as the leading causes of death transitioned from communicable to degenerative disease, but since the 1960s, the gap has widened again as degenerative diseases declined, reflecting the diffusion of medical technology and knowledge to the high SES group first (Feldman et al. 1989; Pappas et al. 1993).
Third, we acknowledge the power of the state in shaping the health trajectories of different cohorts in China. State government played a pivotal role in accelerating an extraordinarily rapid decline of mortality within a short period of time (Caldwell 1986). Life expectancy at birth rose from 41 years in 1950 to 66 years in 1980 (from five years below to five years above the world average) (United Nations 2005). Such a dramatic increase in life expectancy is largely attributed to state intervention. Mass public health campaigns since the 1950s included environmental cleanups, expansion of immunization programs, the establishment of Hygiene and Anti-Epidemic Stations, and the introduction of barefoot doctors, that is, medical personnel in rural China with basic training to practice medicine and deal with hygiene matters (Cook and Dummer 2004). In this study, more recent cohorts born in the 1950s and 1960s, especially those from rural areas, are unquestionably the beneficiaries of state public-health campaigns. In other words,state efforts may have leveled the playing field, thereby reducing the SES effect on health. This may also be why the income gap in health remains constant over the life course or shows a tendency toward convergence for these cohorts, being most pronounced for the rural sample.
By the same token, diminished state power may be why we witness a clear divergence in health trajectories among the earlier cohorts by income. For cohorts who entered old age in the 1990s and 2000s, access to health care becomes vitally important. While China has experienced unprecedented growth in its economy and a much improved standard of living, access to health care has become widely unequal. This is due to the collapse and dysfunction of government health care and health insurance schemes in both urban and rural areas during market reforms, when income inequality grew dramatically (Grogan 1995; Hsiao 1995; Zhao 2006). The weakened role of the state may be another reason for the rural-urban difference seen in a wider divergence pattern for the pre-1930 cohort.
Compared with urban China’s extensive problems with the health care system after the economic reforms, rural areas have seen even greater inequality in health care access. Prior to economic reforms, China achieved remarkable improvement in health for its rural population through rural cooperative medical schemes (CMS), which covered over 90 percent of rural communes in the mid-1970s (Feng et al. 1995; H. Wang et al. 2005). However, since the 1970s, decollectivization in agricultural production made it impossible for townships and villages to finance CMS. By the 1990s, CMS covered less than 10 percent of rural residents (Liu et al. 1995). Results from the 2003 National Health Services Survey suggest that over 80 percent of the rural population had no health care coverage, compared with 40 percent of individuals in urban areas (Zhao 2006). For rural residents of the cohort that entered old age in the 1990s, this dramatic growth in unequal access to health care could lead to a more pronounced widening of the income gap in the age trajectories of health.
The results from our China-based study suggest relatively weaker support for the cumulative disadvantage theory than is found in U.S. studies. China’s unique position, including rapid social change and a powerful state government, suggests the importance of societal context in understanding the theory’s explanatory power. The China–U.S. difference in support for cumulative disadvantage theory may be due to the fact that more recent cohorts’ life histories are not yet available in the CHNS data, such that the effects of cumulative disadvantage on health trajectories become more visible as respondents’ lives unfold andastheyage in thetwenty-first century. As socioeconomic inequality continues to grow, health disparities in more recent cohorts will likely closely correspond to China’s increasing social stratification. At the same time, the Chinese government is currently undertaking major reforms of its health care and health insurance systems and is under tremendous pressure to meet the demands of an aging society (Chen and Liu 2009). Does this mean that the state will once again act as a leveler for health inequality? Although the answer is not easy to predict, it is certain that any influence exerted by policy changes will have unique effects on an individual’s life course—a life course shaped by cohort membership and social context.
Acknowledgments
We would like to thank Glen H. Elder Jr., Kate Strully, Steve McDonald, Troy Case, Matthew E. Dupre, the ASR editors, and four anonymous reviewers for their helpful comments and advice.
Funding Funding for the research comes from NICHD (K01 HD047369) for the first author and P30 AG-12857 NIA/Center on Aging at NORC Pilot Award for the second author.
Biography
Feinian Chen is Associate Professor of Sociology at North Carolina State University. She will join the Department of Sociology at The University of Maryland in fall 2010. Her primary research interests are intergenerational relationships, family structures and dynamics, and their implications for health and aging processes in transitional societies. Her current research project investigates the phenomenon of grandparents caring for grandchildren in China.
Yang Yang is Assistant Professor of Sociology and research associate of the Population Research Center and the Center on Aging at NORC at the University of Chicago. Her research interests include social heterogeneity in aging and life course trajectories of health and comorbidity, mortality and fertility declines in the twenty-first century, new models and methods for cohort analysis, and integrative sociodemographic and biological approaches to explaining social differentials in health and longevity.
Guangya Liu is a graduate student in the Department of Sociology and Anthropology at North Carolina State University. Her research focuses on health, family, aging, and intergenerational relations. Her articles have recently appeared in the American Journal of Public Health, International Handbook of the Demography of Aging, Social Science and Medicine, and International Aging and Human Development.
Footnotes
The processes of cumulative disadvantage and cumulative advantage are different (O’Rand 2002, 2006). The latter emphasizes the positive compounding and accumulation of economic and health capitals over time for those with early advantages and achievements.
Liaoning dropped out of the survey in 1997 and was replaced by Heilongjiang; Liaoning has returned to the survey since 2000.
The survey began in 1989, but we are unable to include that year because it did not include a measure of self-reported health.
The wording of the self-reported health (SRH) question in the CHNS is similar to an age comparative SRH, but the response items are close to that of a global SRH. A descriptive analysis of the relationship between age and SRH controlling for cohort shows a pattern of health decline over the life course, thus demonstrating that it is a valid health measure to capture the aging effect (results available from the first author upon request).
The original sample size at 1991 was 8,146. Among the missing cases (7.7 percent), less than 1 percent are missing on the dependent variable and the rest are missing on various independent variables. The overall working sample excludes missing values on any variable included in the analysis (averaged around 1,208 individuals across waves, excluding death and loss to follow-up). We conducted sensitivity tests using the method of mean imputation and dummy variable adjustment (including a dummy variable suggesting missingness in the model). The results are robust, so we treat them as missing at random.
We experimented with dummy variables of cohort in preliminary analyses and found no evidence for nonlinearity in the cohort effects, nor a better model fit that supports this alternative specification. We thus use the continuous variable for the final analysis.
We considered an alternative distributional assumption of self-rated health, an ordinal response and estimated Generalized Linear Mixed Models (GLMM) with ordinal logit link using SAS PROC GLIMMIX, but do not present these results for three reasons. First, the fixedand random-effect coefficients and variance estimates are qualitatively similar to these two sets of analyses, yet the current normal specification has the advantages of aiding straightforward interpretation of the results and no requirement of a proportional-odds assumption. In fact, the ordered logit analysis shows that the proportional-odds assumption does not hold for the data. Second, the hierarchical ordinal logit models using PROC GLIMMIX are based on residual pseudo-likelihood estimation. There is no overall goodness-of-fit statistic available in the literature, nor any extant computational software, that can be used to compare models estimated using pseudolikelihood (Littell et al. 2006). Third, normal models of self-rated health are widely used in medical sociology, demography, and gerontology research (e.g., George 1996; Idler 1993; Lynch 2003) and suggest their adequacy and utility in substantive studies of health and well-being. This study uses the same variable for more direct comparisons across populations.
To illustrate this point, consider the age variable, Ageti, in Equation 1. The nature of this variable is that age for individual i covaries with time t exactly; that is, individual i of age A at time T will be age A + 1 at time T + 1.
Given that the sample includes multiple respondents from the same household, we use the GLLAMM procedure from STATA 9.0 to adjust for clustering at the household level. The results are very similar to those produced by PROC MIXED in SAS. We therefore present the results from SAS in this article.
We omitted models with the control variables to avoid redundancy, as the results are consistent with those without them.
We divided the centered age variable by 10 to make the effect coefficients more visible.
We entered all the control variables in both the intercept and the growth rate models. The effects of sex, marital status, smoking, drinking, and BMI are not significant in the growth rate model and thus were dropped from the final model.
This article was first presented at the 2008 Annual Meetings of the Population Association of America in New Orleans.
References
- Barker DJP. Mothers, Babies, and Health in Later Life. Churchill Livingstone; Edinburgh, UK: 1998. [Google Scholar]
- Beydoun May A., Popkin Barry M. The Impact of Socio-Economic Factors on Functional Status Decline among Community-Dwelling Older Adults in China. Social Science & Medicine. 2005;60:2045–57. doi: 10.1016/j.socscimed.2004.08.063. [DOI] [PubMed] [Google Scholar]
- Bian Yanjie. Chinese Social Stratification and Social Mobility. Annual Review of Sociology. 2002;28:91–116. [Google Scholar]
- Bian Yanjie, Logan John R. Market Transition and the Persistence of Power: The Changing Stratification System in Urban China. American Sociological Review. 1996;61:739–58. [Google Scholar]
- Caldwell John C. Routes to Low Mortality in Poor Countries. Population and Development Review. 1986;12:171–220. doi: 10.1111/j.1728-4457.2010.00353.x. [DOI] [PubMed] [Google Scholar]
- Chen Feinian, Liu Guangya. Population Aging in China. In: Uhlenberg P, editor. The International Handbook of Population Aging. Springer Publishers; New York: 2009. pp. 157–72. [Google Scholar]
- Chiu Herng-Chia, Ying-Hui Hsieh, Lih-Wen Mau, Lee Mei-Lin. Associations between Socioeconomic Status Measures and Functional Change among Older People in Taiwan. Ageing & Society. 2005;25:377–95. [Google Scholar]
- Clark Daniel O., Maddox George L. Racial and Social Correlates of Age-Related Changes in Functioning. Journals of Gerontology: Social Sciences. 1992;47:S222–S232. doi: 10.1093/geronj/47.5.s222. [DOI] [PubMed] [Google Scholar]
- Cohen Ayala. Comparing Regression Coefficients across Subsamples: A Study of the Statistical Test. Sociological Methods and Research. 1983;12:77–94. [Google Scholar]
- Cook Ian G., Dummer Trevor J. B. Changing Health in China: Re-evaluating the Epidemiological Transition Model. Health Policy. 2004;67:329–43. doi: 10.1016/j.healthpol.2003.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desesquelles Aline, Viviana Egidi, Salvatore Michele A. Why Do Italian People Rate their Health Worse than French People Do? An Exploration of Cross-Country Differentials of Self-Rated Health. Social Science & Medicine. 2009;68:1124–28. doi: 10.1016/j.socscimed.2008.12.037. [DOI] [PubMed] [Google Scholar]
- Du Shufa, Bing Lu, Fengying Zhai, Popkin Barry M. A New Stage of the Nutrition Transition in China. Public Health Nutrition. 2002;5:169–74. doi: 10.1079/PHN2001290. [DOI] [PubMed] [Google Scholar]
- Dupre Matthew E. Educational Differences in Age-Related Patterns of Disease: Reconsidering the Cumulative Disadvantage and Age-as-Leveler Hypotheses. Journal of Health and Social Behavior. 2007;48:1–15. doi: 10.1177/002214650704800101. [DOI] [PubMed] [Google Scholar]
- — — — Educational Differences in Health Risks and Illness over the Life Course: A Test of Cumulative Disadvantage Theory. Social Science Research. 2008;37:1253–66. doi: 10.1016/j.ssresearch.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Elder Glen H., Jr. Military Times and Turning Points in Men’s Lives. Developmental Psychology. 1986;22:233–45. [Google Scholar]
- — — — War Mobilization and the Life Course: A Cohort of World War II Veterans. Sociological Forum. 1987;2:449–72. [Google Scholar]
- — — — . Children of the Great Depression: Social Change in Life Experience. 25th anniversary ed. Westview Press; Boulder, CO: 1999. [1974] [Google Scholar]
- Elder Glen H., Jr., Johnson Monica K., Crosnoe Robert. The Emergence and Development of Life Course Theory. In: Mortimer J, Shanahan M, editors. Handbook of the Life Course. Plenum; New York: 2003. pp. 3–19. [Google Scholar]
- Entwisle Barbara, Chen Feinian. Work Patterns Following a Birth in Urban and Rural China: A Longitudinal Study. European Journal of Population. 2002;18:99–119. [Google Scholar]
- Faris Robert E. L., Dunham H. Warren. Mental Disorders in Urban Areas: An Ecological Study of Schizophrenia and other Psychoses. The University of Chicago Press; Chicago, IL: 1939. [Google Scholar]
- Farmer Melissa M., Ferraro Kenneth F. Distress and Perceived Health: Mechanisms of Health Decline. Journal of Health and Social Behavior. 1997;38:298–311. [PubMed] [Google Scholar]
- Feldman Jacob J., Makuc Diane M., Kleinman Joel C., Cornoni-Huntley Joan. National Trends in Educational Differentials in Mortality. American Journal of Epidemiology. 1989;129:919–33. doi: 10.1093/oxfordjournals.aje.a115225. [DOI] [PubMed] [Google Scholar]
- Feng Xueshan, Tang Shenglan, Bloom Gerald, Segall Malcolm, Gu Xingyuan. Cooperative Medical Schemes in Contemporary Rural China. Social Science & Medicine. 1995;41:1111–18. doi: 10.1016/0277-9536(94)00417-r. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F., Kelley-Moore Jessica A. Cumulative Disadvantage and Health: Long-Term Consequences of Obesity? American Sociological Review. 2003;68:707–29. [PMC free article] [PubMed] [Google Scholar]
- Fogel Robert W., Costa Dora L. A Theory of Technophysio Evolution, with Some Implications for Forecasting Population, Health Care Costs, and Pension Costs. Demography. 1997;34:49–66. [PubMed] [Google Scholar]
- Freedman Vicki A., Martin Linda G. Understanding Trends in Functional Limitations among Older Americans. American Journal of Public Health. 1998;88:1457–62. doi: 10.2105/ajph.88.10.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda Yoshiharu, Nakamura Keiko, Takano Takehito. Municipal Socioeconomic Statusand Mortality in Japan: Sex and Age Differences, and Trends in 1973–1998. Social Science & Medicine. 2004;59:2435–45. doi: 10.1016/j.socscimed.2004.04.012. [DOI] [PubMed] [Google Scholar]
- George Linda K. Missing Links: The Case for a Social Psychology of the Life Course. Gerontologist. 1996;36:248–55. doi: 10.1093/geront/36.2.248. [DOI] [PubMed] [Google Scholar]
- Grogan Colleen M. Urban Economic Reform and Access to Health Care Coverage in the People’s Republic of China. Social Science & Medicine. 1995;41:1073–84. doi: 10.1016/0277-9536(94)00419-t. [DOI] [PubMed] [Google Scholar]
- Gu Danan, Zeng Yi. Sociodemographic Effects on the Onset and Recovery of ADL Disability among Chinese Oldest-Old. Demographic Research. 2004;11:1–42. [Google Scholar]
- Hays Judith C., Schoenfeld David E., Blazer Dan G. Determinants of Poor Self-Rated Health in Late Life. American Journal of Geriatric Psychiatry. 1996;4:188–96. doi: 10.1097/00019442-199622430-00002. [DOI] [PubMed] [Google Scholar]
- Hayward Mark D., Gorman Bridget K. The Long Arm of Childhood: The Influence of Early-Life Social Conditions on Men’s Mortality. Demography. 2004;41:87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- House James S., Kessler Ronald C., Herzog A. Regula. Age, Socioeconomic Status, and Health. The Milbank Memorial Quarterly. 1990;68:383–411. [PubMed] [Google Scholar]
- House James S., Lantz Paula M., Herd Pamela. Continuity and Change in the Social Stratification of Aging and Health over the Life Course: Evidence from a Nationally Representative Study from 1986 to 2001/2002 (Americans’ Changing Lives Study) Journal of Gerontology: Social Sciences. 2005;60:S15–S26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- House James S., Lepkowski James M., Kinney Ann M., Mero Richard P., Kessler Ronald C., Herzog A. Regula. The Social Stratification of Aging and Health. Journal of Health and Social Behavior. 1994;35:213–34. [PubMed] [Google Scholar]
- Hsiao William C. L. The Chinese Health Care System: Lessons for Other Nations. Social Science & Medicine. 1995;41:1047–55. doi: 10.1016/0277-9536(94)00421-o. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L. Age Differences in Self-Assessments of Health: Age Changes, Cohort Differences or Survivorship? Journal of Gerontology: Social Sciences. 1993;48:S289–S300. doi: 10.1093/geronj/48.6.s289. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L., Angel Ronald J. Age, Chronic Pain, and Subjective Assessments of Health. Advances in Medical Sociology. 1990;1:131–52. [Google Scholar]
- Idler Ellen L., Benyamini Yael. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Johnson Robert J., Wolinsky Fredric D. The Structure of Health Status among Older Adults: Disease, Disability, Functional Limitation and Perceived Health. Journal of Health and Social Behavior. 1993;34:105–21. [PubMed] [Google Scholar]
- Jylhä Marja, Guralnik Jack M., Ferrucci Luigi, Jokela Jukka, Heikkinen Eino. Is Self-Rated Health Comparable across Cultures and Genders? Journal of Gerontology: Social Sciences. 1998;53:S144–S152. doi: 10.1093/geronb/53b.3.s144. [DOI] [PubMed] [Google Scholar]
- Kim Soowon, Symons Michael, Popkin Barry M. Contrasting Socioeconomic Profiles Related to Healthier Lifestyles in China and the United States. American Journal of Epidemiology. 2004;159:184–91. doi: 10.1093/aje/kwh006. [DOI] [PubMed] [Google Scholar]
- Kitagawa Evelyn M., Hauser Philip M. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. Harvard University Press; Cambridge, MA: 1973. [Google Scholar]
- Li Hongbin, Zhu Yi. Income, Income Inequality, and Health: Evidence from China. Journal of Comparative Economics. 2006;34:668–93. [Google Scholar]
- Liang Jersey, Bennett Joan, Krause Neal, Kobayashi Erika, Kim Hyekyung, Brown J. Winchester, Akiyama Hiroko, Sugisawa Hidehiro, Jain Arvind. Old Age Mortality in Japan: Does the Socioeconomic Gradient Interact with Gender and Age? Journal of Gerontology: Social Sciences. 2002;57:S294–S307. doi: 10.1093/geronb/57.5.s294. [DOI] [PubMed] [Google Scholar]
- Liang Jersey, Liu Xian, Gu Shengzu. Transitions in Functional Status among Older People in Wuhan, China: Socioeconomic Differentials. Journal of Clinical Epidemiology. 2001;54:1126–38. doi: 10.1016/s0895-4356(01)00390-0. [DOI] [PubMed] [Google Scholar]
- Lin Nan, Bian Yanjie. Getting Ahead in Urban China. American Journal of Sociology. 1991;97:657–88. [Google Scholar]
- Littell Ramon C., Milliken George A., Stroup Walter W., Wolfinger Russell D., Schabenberger Oliver. SAS for Mixed Models. 2nd ed SAS Institutes, Inc.; Cary, NC: 2006. [Google Scholar]
- Liu Yuanli, Hsiao William C. L., Li Qing, Liu Xingzhu, Ren Minghui. Transformation of China’s Rural Health Care Financing. Social Science Medicine. 1995;41:1085–93. doi: 10.1016/0277-9536(95)00428-a. [DOI] [PubMed] [Google Scholar]
- Lynch John W., Kaplan George A., Shema Sarah J. Cumulative Impact of Sustained Economic Hardship on Physical, Cognitive, Psychological, and Social Functioning. New England Journal of Medicine. 1997;337:1889–95. doi: 10.1056/NEJM199712253372606. [DOI] [PubMed] [Google Scholar]
- Lynch Scott M. Cohort and Life Course Patterns in the Relationship between Education and Health: A Hierarchical Approach. Demography. 2003;40:309–31. doi: 10.1353/dem.2003.0016. [DOI] [PubMed] [Google Scholar]
- Marmot Michael G. Epidemiology of Socioeconomic Status and Health: Are Determinants within Countries the Same as between Countries? Annals of the New York Academy of Sciences. 1999;896:16–29. doi: 10.1111/j.1749-6632.1999.tb08102.x. [DOI] [PubMed] [Google Scholar]
- Merton Robert K. The Matthew Effect in Science. Science. 1968;159:56–63. [PubMed] [Google Scholar]
- Miyazaki Yasuo, Raudenbush Stephen W. Tests for Linkage of Multiple Cohorts in an Accelerated Longitudinal Design. Psychological Methods. 2000;5:44–63. doi: 10.1037/1082-989x.5.1.44. [DOI] [PubMed] [Google Scholar]
- Nee Victor. A Theory of Market Transition: From Redistribution to Markets in State Socialism. American Sociological Review. 1989;54:663–81. [Google Scholar]
- Olshansky S. Jay, Ault A. Brian. The Fourth Stage of the Epidemiologic Transition: The Age of Delayed Degenerative Disease. The Milbank Quarterly. 1986;64:355–91. [PubMed] [Google Scholar]
- Olshansky S. Jay, Carnes Bruce A., Rogers Richard G., Smith Len. Emerging Infectious Diseases: The Fifth Stage of the Epidemiologic Transition? World Health Statistics Quarterly. 1998;51:207–17. [Google Scholar]
- O’Rand Angela M. Cumulative Advantage Theory in Life Course Research. In: Crystal S, Shea D, editors. Economic Outcomes in Later Life: Public Policy, Health, and Cumulative Advantage. Annual Review of Gerontology and Geriatrics. Special Issue. Vol. 22. 2002. pp. 14–30. [Google Scholar]
- — — — . Stratification and the Life Course: Life Course Capital, Life Course Risks, and Social Inequality. In: Binstock RH, George LK, editors. Handbook of Aging and the Social Sciences. 6th ed Elsevier; Boston, MA: 2006. pp. 146–65. [Google Scholar]
- Pappas Gregory, Queen Susan, Hadden Wilbur, Fisher Gail. The Increasing Disparity in Mortality between Socioeconomic Groups in the US, 1960 and 1986. The New England Journal of Medicine. 1993;329:103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- Popkin Barry M. The Nutrition Transition and Its Health Implications in Lower Income Countries. Public Health Nutrition. 1998;1:5–21. doi: 10.1079/phn19980004. [DOI] [PubMed] [Google Scholar]
- Power Chris, Matthews Sharon, Manor Orly. Inequalities in Self-Rated Health: Explanations from Different Stages of Life. The Lancet. 1998;351:1009–13. doi: 10.1016/S0140-6736(97)11082-0. [DOI] [PubMed] [Google Scholar]
- Raudenbush Stephen W., Bryk Anthony S. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Rogers Richard G., Rogers Andrei, Belanger Alain. Disability-Free Life among the Elderly in the United States: Sociodemographic Correlates of Functional Health. Journal of Aging and Health. 1992;4:19–42. [Google Scholar]
- Rodgers Willard L., Ofstedal Mary B., Herzog A. Regula. Trends in Scores on Tests of Cognitive Ability in the Elderly U.S. Population, 1993–2000. Journal of Gerontology: Social Sciences. 2003;58:S338–S346. doi: 10.1093/geronb/58.6.s338. [DOI] [PubMed] [Google Scholar]
- Rosner Hans J. China’s Health Insurance System in Transformation: Preliminary Assessment, and Policy Suggestions. International Social Security Review. 2004;57:65–90. [Google Scholar]
- Ross Catherine E., Wu Chia-Ling. Education, Age, and the Cumulative Advantage in Health. Journal of Health and Social Behavior. 1996;37:104–20. [PubMed] [Google Scholar]
- Short Susan E., Ma Linmao, Yu Wentao. Birth Planning and Sterilization in China. Population Studies. 2000;54:279–91. doi: 10.1080/713779090. [DOI] [PubMed] [Google Scholar]
- Singer Judith D., Willett John B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; New York: 2003. [Google Scholar]
- Smith James P., Kington Raynard S. Demographic and Economic Correlates of Health in Old Age. Demography. 1997;34:159–70. [PubMed] [Google Scholar]
- Song Yun-Mi, Ferrer Robert L., Cho Sung-il, Sung Joohon, Ebrahim Shah, Smith George Davey. Socioeconomic Status and Cardiovascular Disease among Men: The Korean National Health Service Prospective Cohort Study. American Journal of Public Health. 2006;96:152–59. doi: 10.2105/AJPH.2005.061853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolzenberg Ross M., Relles Daniel A. Tools for Intuition about Sample Selection Bias and Its Correction. American Sociological Review. 1997;62:494–507. [Google Scholar]
- Tonry Michael H., Ohlin Lloyd E., Farrington David P. Human Development and Criminal Behavior: New Ways of Advancing Knowledge. Springer-Verlag; New York: 1991. [Google Scholar]
- Turner R. Jay, Wheaton Blair, Lloyd Donald A. The Epidemiology of Social Stress. American Sociological Review. 1995;60:104–25. [Google Scholar]
- United Nations (Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat) World Population Prospects: The 2004 Revision Population Database. 2005 ( http://esa.un.org/unpp/)
- Wang Feng, Mason Andrew. Population Ageing: Challenges, Opportunities, and Institutions. In: Zhao Z, Guo F, editors. Transition and Challenge: China’s Population at the Beginning of the 21st Century. Oxford University Press; Oxford, UK: 2007. pp. 177–96. [Google Scholar]
- Wang Hong, Yip Winnie, Zhang Licheng, Wang Lusheng, Hsiao William. Community-Based Health Insurance in Poor Rural China: The Distribution of Net Benefits. Health Policy & Planning. 2005;20:366–74. doi: 10.1093/heapol/czi045. [DOI] [PubMed] [Google Scholar]
- Wang Longde, Lingzhi Kong, Wu Fan, Bai Yamin, Burton Robert. Preventing Chronic Diseases in China. The Lancet. 2005;366:1821–24. doi: 10.1016/S0140-6736(05)67344-8. [DOI] [PubMed] [Google Scholar]
- West Patrick. Rethinking the Health Selection Explanation for Health Inequalities. Social Science & Medicine. 1991;32:373–84. doi: 10.1016/0277-9536(91)90338-d. [DOI] [PubMed] [Google Scholar]
- Willson Andrea E., Shuey Kim M., Elder Glen H., Jr. Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health. American Journal of Sociology. 2007;112:1886–1924. [Google Scholar]
- Winship Christopher, Mare Robert. Models for Selection Bias. Annual Review of Sociology. 1992;18:327–50. [Google Scholar]
- Wong SL, Donnan SP. Influence of Socioeconomic Status on Cardiovascular Diseases in Hong Kong. Journal of Epidemiology and Community Health. 1992;46:148–50. doi: 10.1136/jech.46.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Jing, Liu Yuanli, Rao Keqin, Sun Qi, Qian Juncheng, Li Zhu. Education-Related Gender Differences in Health in Rural China. American Journal of Public Health. 2004;94:1713–16. doi: 10.2105/ajph.94.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Xiaogang, Xie Yu. Does the Market Pay Off? Earnings Returns to Education in Urban China. American Sociological Review. 2003;68:425–42. [Google Scholar]
- Wu Z. Helen, Rudkin Laura. Social Contact, Socioeconomic Status, and the Health Status of Older Malaysians. Gerontologist. 2000;40:228–34. doi: 10.1093/geront/40.2.228. [DOI] [PubMed] [Google Scholar]
- Yang Yang. Is Old Age Depressing? Growth Trajectories and Cohort Variations in Late Life Depression. Journal of Health and Social Behavior. 2007;48:16–32. doi: 10.1177/002214650704800102. [DOI] [PubMed] [Google Scholar]
- Yang Yang, Lee Linda C. Sex and Race Disparities in Health: Cohort Variations in Life Course Patterns. Social Forces. 2009;87:2093–2124. [Google Scholar]
- Yoon Yeong Sook, Oh Sang Woo, Park Hye Soon. Socioeconomic Status in Relation to Obesity and Abdominal Obesity in Korean Adults: A Focus on Sex Differences. Obesity. 2006;14:909–19. doi: 10.1038/oby.2006.105. [DOI] [PubMed] [Google Scholar]
- Zhao Zhongwei. Income Inequality, Unequal Health Care Access, and Mortality in China. Population and Development Review. 2006;32:461–83. [Google Scholar]
- Zhou Xueguang. Economic Transformation and Income Inequality in Urban China: Evidence from Panel Data. American Journal of Sociology. 2000;105:1135–74. [Google Scholar]
- Zimmer Zachary, Amornsirisomboon Pattama. Socioeconomic Status and Health among Older Adults in Thailand: An Examination Using Multiple Indicators. Social Science & Medicine. 2001;52:1297–1311. doi: 10.1016/s0277-9536(00)00232-x. [DOI] [PubMed] [Google Scholar]
- Zimmer Zachary, Hermalin Albert I., Lin Huisheng. Whose Education Counts? The Added Impact of Adult-Child Education on Physical Functioning of Older Taiwanese. Journal of Gerontology: Social Sciences. 2002;57:S23–S32. doi: 10.1093/geronb/57.1.s23. [DOI] [PubMed] [Google Scholar]
- Zimmer Zachary, Kwong Julia. Family Size and Support of Older Adults in Urban and Rural China: Current Effects and Future Implications. Demography. 2003;40:23–44. doi: 10.1353/dem.2003.0010. [DOI] [PubMed] [Google Scholar]