Abstract
Background
There is no specific serum-based biomarker for the diagnosis or prognosis of relapsing-remitting multiple sclerosis (RRMS).
Objective
We investigated whether levels of IgM antibodies to Glc(α1,4)Glc(α) (GAGA4) or to a panel of four glucose-based glycans could differentiate MS from other neurological diseases (OND) or predict risk of early relapse following first presentation (FP) of RRMS.
Methods
Retrospective analysis of 440 sera samples of three cohorts: A) FP-RRMS (n = 44), OND (n = 44); B) FP-RRMS (n = 167), OND (n = 85); and C) FP (n = 100). Anti-GAGA4 IgM levels were measured by enzyme immunoassay in cohort-A and cohort-B. Cohort-C IgM antibodies to glucosebased glycan panel were measured by immunofluorescence.
Results
FP-RRMS had higher levels of anti-GAGA4 IgM than OND patients (cohort-A, P = 0.01; cohort-B, P = 0.0001). Sensitivity and specificity were 27% and 97% for cohort-A; and 26% and 90% for cohort-B, respectively. In cohort-C, 58 patients experienced early relapse (<24 months), 31 had late relapse (≥24 months), and 11 did not experience second attack during follow-up. Kaplan– Meier curves demonstrated decrease in time to next relapse for patients positive for the antibody panel (P = 0.02, log rank).
Conclusions
Serum anti-GAGA4 IgM discerns FP-RRMS patients from OND patients. Higher levels of serum anti-α-glucose IgM in FP patients predict imminent early relapse.
Keywords: antibodies, anti-glucose antibodies, anti-glycan antibodies, biomarker, diagnosis, enzyme immunoassay, IgM, multiple sclerosis, prognosis
Introduction
Multiple sclerosis (MS) is an inflammatory demyelinating disease of the central nervous system (CNS), although the exact etiology and pathogenesis have not yet been deciphered. The finding of IgG antibody formation specifically in the cerebrospinal fluid (CSF), but not in a corresponding serum (i.e. oligoclonal banding), has long been a useful test for diagnosis and differential diagnosis of MS [1], though no known antigenic specificity has ever been universally defined. The search has been ongoing for useful serum-derived biomarkers, including antibodies. Serum IgM antibodies to an N-glucosylated peptide were specifically increased in relapsing-remitting multiple sclerosis (RRMS) patients [2,3]. High antibody titers to two myelin peptides, myelin oligodendrocyte glycoprotein and myelin basic protein were reported by some [4], but not others [5], to predict early relapse in patients after their first presentation (FP) of MS.
We previously demonstrated elevated levels of IgM antibodies to Glc(α1,4)Glc(α) (GAGA4) in RRMS patients in comparison to patients with other neurological diseases (OND) [6]. We were, therefore, interested in knowing when in the course of disease higher antibody titers to GAGA4 or a panel of glucose-based glycans first occurs or whether there was any correlation to disease activity by focusing on patients studied after their FP.
Materials and methods
Serum Samples
A retrospective study of frozen (-70°C) and rethawed serum samples collected from patients at the time of diagnostic work-up for their FP were later diagnosed as RRMS. The control group included sera samples taken from patients with OND that were stored around the same time from routine samples sent to the respective CSF diagnostic laboratories. Demographic and clinical data were obtained from hospital records. Inclusion criteria for MS samples were as follows: patient age (18-60 years) at time of sampling, follow-up for at least 4 years from blood sampling, and diagnosis of RRMS according to Poser criteria [7], or as OND. Samples which meet the above criteria were identified from one of two serum repositories located at the Ottawa Hospital-General Campus, Ottawa, Canada (Mark S. Freedman) between the years 1993 and 2001 or the Cliniques Universitaires Saint-Luc in Brussels, Belgium (Christian Sindic) between the years 1998 and 2002. Samples were collected under a broad consent for scientific research allowing for multiple studies and approved by local ethics boards. Relapse was defined as any new neurological event accompanied by symptoms or signs, or significant worsening of previous symptoms or signs in the absence of fever that lasted at least 48 hours. All samples were encoded at respective institutions before being sent to Glycominds Ltd. laboratories for antibody analysis—decoding occurred only after all the analyses were completed. Three distinct cohorts were analyzed: cohort-A included 88 samples (44 FP n = 44, OND n = 44), OND patients were matched to the MS patients according to age and gender; cohort-B included 252 samples (FP n = 167, OND n = 85); and cohort-C included 100 FP patients. All samples were assayed in a ‘blinded’ fashion.
Total IgM measurement
Total IgM level was measured as previously described [6] and reported in relative fluorescence units (RFU) (cohort-A). For cohort-B and cohort-C, total IgM levels were measured using a commercial enzyme-linked immunosorbent assay (ELISA) kit (Bethyl laboratories, Montgomery, TX) according to manufacturer instructions and reported in milligram per milliliter.
Enzyme-linked immunoassay of anti-GAGA4 IgM
In cohort-A and cohort-B, levels of anti-GAGA4 IgM were determined in IgG depleted samples by enzyme-linked immunoassay (EIA) and normalized according to the levels of total IgM as previously reported [6]. IgG depletion was performed using a commercial mini Rapi-Sep® units (PanBio, Baltimore, MD) according to manufacturer's instructions. p-nitrophenyl derivative of GAGA4 were covalently attached to the surface of a 96-well microtiter plate via a linker as previously described [8]. Serum samples were diluted 1:1200 in a sample diluent (Cat. No. G300023, Glycominds, Lod, Israel), dispensed into the wells in duplicates, and incubated for 120 min in 5°C, then washed with wash buffer (Cat. No. G300022, Glycominds Ltd). Bound antibodies were labeled with horseradish peroxidase-conjugated goat anti-human IgM type-specific antibody (1:2000), washed, and 3, 3′, 5, 5′-tetramethylbenzidine was added for detection. After 30 min, the enzymatic reaction was stopped with 1% sulfuric acid solution and optical density (OD) of the wells was read at 450 nm with a Victor 1420 plate reader (Wallac, Turku, Finland). In cohort-A, anti-GAGA4 OD levels were normalized by dividing them by the square root of total IgM levels (RFU) multiplied by 106. Cutoff value was set as mean [OD/(total IgM × 106)0.5] level of OND group + 2 standard deviations (SD).
In cohort-B, in addition to the tested samples, each plate included positive- and negative-control sera samples from MS patients and a calibrator sample considered as 50 units. Anti-GAGA4 EIA units (EU) values were calculated for each sample by dividing the sample ODs by the calibrator OD multiplied by 50. Anti-GAGA4 EU were normalized for total IgM in serum samples, by dividing by the square root of total IgM (mg/mL)0.5 corrected to gender by adding 0.17 (mg/mL)0.5 for male samples. Cutoff value for determination of anti-GAGA4 positivity was 42 EU/(mg/mL)0.5. This cutoff was based on receiver operator characteristic curve analysis for achieving 90% specificity for RRMS. The coefficient of variation (CV) of anti-GAGA4 ELISA level was 11% between wells in the same plate (intra-plate), and 15% for different assays (inter-plate). Inter-plate constant variance for calibrator sample was 15%.
Immunofluorescence assay for anti-GAGA2, -GAGA3, -GAGA4, and -GAGA6 IgM using glycan array
Glycan array
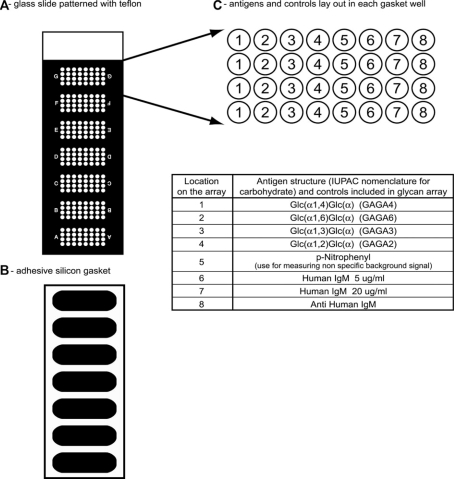
Levels of anti-GAGA2, -GAGA3, -GAGA4, and -GAGA6 IgM antibodies in cohort-C samples were measured by immunofluorescence assay, using glass slides patterned with teflon mask, creating 7 clusters of microwells with 32 wells in each cluster (Figure 1A). An adhesive silicon superstructure (Figure 1B) was attached to the slide. This silicon gasket defined wells for manual application of multiple serum samples per slide. Each well was arrayed with glycan antigens and internal controls (Figure 1C). p-nitrophenyl derivatives of GAGA2, GAGA3, GAGA4, and GAGA6 (Toronto Research Chemicals, Toronto, Canada) were covalently bound by a linker to the glass slide as previously described [6].
Figure 1.
Glycan array format: A – Glass slide patterned with Teflon mask creating 7 clusters of microwells, 32 wells in each cluster. B – An adhesive silicon superstructure attached to the slide defines wells for manual application of multiple serum samples per slide. C – Antigens and controls lay out in each gasket well.
Assay procedures
The slide wells were incubated for 60 min at room temperature with blocking solution (400 μL/well). After removal of blocking solution, 300 μL/well of patients’ sera, diluted 1:40 in aqueous solution of 1% bovine serum albumin in 20 mM Tris–HCl pH 7.2, 0.9% NaCl, 0.05% Tween-20 was added to each well. Each slide included five sera samples and a reference sample for one arbitrary unit. Each sample was tested five times on different slides. Samples were incubated for 45 min. Following sera were removed and slides further washed and processed in an HS4800 system. Briefly, slides were washed in TNTT buffer (20 mM Tris–HCl pH 7.2, 2 M NaCl, 0.05% Tween-20, 0.05% Triton X-100) by the hybridization system. Biotinylated goat antihuman IgM (1:500) and Alexa-633-labeled streptavidin (1:150; Molecular Probes Inc. Eugene, OR, USA) were incubated sequentially with washings in between for 1 h at 32°C in the light-protected and temperature-controlled environment of the hybridization system.
Following the washing and drying, slides were scanned using laser scanner (GenePix 4000B, Molecular Device, Baltimore, MD); slide image was analyzed using Optiquant™ software and RFU representing relative binding of anti-glycan IgM to each antigen and control micro-well were calculated. The data quality from each well was verified by ensuring signal levels from human IgM and anti-human IgM spots above cutoff. If the data quality from the wells did not meet criteria, samples were tested again. Levels of anti-GAGA2, -GAGA3, -GAGA4, and -GAGA6 IgM were calculated for each sample by dividing the sample RFU by the reference sample RFU. The CV of anti-α-glucose levels was 8–12% for intra-slides wells and 15–22% for different hybridization station running cycles (inter-slide).
Samples were considered as positive if results were above cutoff levels for at least one of the four antibodies. Cutoff values for each antigen were calculated as mean value of the FP population plus 1, 1.5, or 2 SD, and best fit cutoffs (4.0, 4.5, 4.5, and 4.3 for anti-GAGA2, -GAGA3, -GAGA4, and -GAGA6 IgM, respectively).
Statistical methods
Numerical variables were compared across groups by Student's t-test or by the Mann–Whitney U-test, depending on whether or not they followed a normal distribution, and the χ2 test for rates comparison between groups or the Fisher exact if any cells had an expected count of less than 5. Pearson correlations were calculated between numerical variables. P-values of less than 0.05 were considered to be statistically significant. Uncertainty of results was expressed by 95% confidence intervals. For comparison between FP patients and OND patients, levels of anti-GAGA4 IgM EU were corrected for total IgM level by dividing them by the square root of total human IgM in the sample. Diagnostic accuracy was calculated by sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Predictive values were calculated based on the prevalence of MS in the present cohort (0.68). The cumulative risk of the development of clinically definite MS (CDMS) was calculated for each group according to the Kaplan–Meier method, and the differences between the groups were evaluated in a univariate analysis by the log-rank test.
We implemented a two-stage analysis for testing the ability of GAGA4 to differentiate OND from FP subjects. In the first stage, a preliminary analysis on OND and FP groups that were age- and gender-matched (cohort-A) were performed. Our aim was to explore the ability of an anti-GAGA4 assay to differentiate between OND and FP subjects under conditions that maximize the power of detection of disease-specific effects. In the second stage, we tested if the results from the preliminary analysis could be repeated by a more optimal EIA method in a different and relatively larger population in which the FP and OND groups were not matched for age and gender (cohort-B).
For testing the ability of the marker antibodies to differentiate FP patients with a high risk vs. a low risk for early conversion to CDMS (cohort-C), several cutoff values were investigated. Although this analysis involved the application of multiple statistical tests that would normally require the application of a correction factor, our study was in fact exploratory, which beckons multiple analyses in order to obtain testable hypotheses that would require confirmation in subsequent studies [9]. We nevertheless applied a Bonferroni correction factor to our analysis.
Results
Cohort-A: Anti-GAGA4 IgM in FP-RRMS vs. OND group
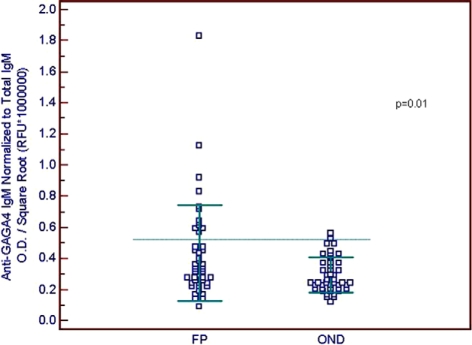
Clinical and demographic characteristics as well as anti-GAGA4 levels for cohort-A are described in Table 1. The OND and FP groups were matched for age and gender. In cohort-A, there were significant differences between the Brussels and Ottawa groups regarding gender composition, and a higher number of samples from Ottawa in the FP group versus the OND group. However, no significant difference regarding the levels of total IgM and anti-GAGA4 IgM normalized to total IgM was found between the 22 samples from Brussels in comparison to the 66 samples from Ottawa. Levels of anti-GAGA4 IgM normalized to total IgM were significantly higher (P = 0.01) in samples from FP patients compared to OND controls. Distribution of normalized anti-GAGA4 IgM in the FP and OND groups is shown in Figure 2.
Table 1.
Demographic, clinical characteristics, and anti-GAGA4 IgM levels of cohort-A
| FP (n = 44) | OND (total n = 44, OIND 21, ONIND 23) | Ottawa (n = 66) | Brussels (n = 22) | |
| Mean age, years (SD) | 37.6 (9.0) | 38.5 (9.5) | 39.1 (8.8) | 35.1 (9.8) |
| Female, n (%) | 38 (86) | 33 (75) | 55 (83)a | 16 (73) |
| Center Ottawa, n (%) | 37 (84)b | 26 (59) | NA | NA |
| Total Ig M, Mean RFU × 106 (SD) | 2.10 (0.80) | 1.94 (0.68) | 2.08 (0.79) | 1.83 (0.53) |
| 2nd relapse within 24 months, n (% of FP population only) | 26 (60)c | NA | 21 (57) | 5 (71) |
| Anti-GAGA4 IgM, Mean signal intensity, OD/(Total IgM RFU × 106)0.5 (SD) | 0.44 (0.30)d | 0.30 (0.11) | 0.37 (0.26) | 0.35 (0.16) |
All FP patients had CDMS at the end of the follow-up.
Other inflammatory neurological disease (OIND) group included the following: 2 bacterial meningitis, 4 viral meningitis, 1 IV Ig-induced meningitis, 2 optic neuritis, 2 cerebral vasculitis, 1 Churg–Strauss vasculitis, 2 myelitis, 1 sarcoidosis, 1 SLE, 1 HIV, 1 sinusitis, 1 brachial plexitis, 1 epidural abscess; Other noninflammatory neurological disease (ONIND) group included the following: 2 fibromyalgia, 2 migraine, 5 idiophathic headache, 1 progressive dementia, 1 motor neuron disease, 1 valproate-induced encephalopathy, 1 migraine + stroke, 1 dementia NYD (not yet determined), 1 neurosis, 1 brainstem stroke, 1 anisocoria, 1 chronic insomnia, 1 diabetic amyotropy, 1 numbness, 1 motor neuropathy, 1 occipital neuralgia and ataxia, 1 breast cancer; NA, not applicable.
Note: All the data in this Table derive from samples collected at or near the time of FP.
FP, first presentation; OND, other neurological diseases; SD, Standard deviation; RFU, relative fluorescence units; OD, optical density.
aχ2 test P = 0.025 versus Brussels.
bχ2 test P = 0.01 versus OND.
cVerified data regarding occurrence of second relapse within 24 months and EDSS score at 4 years were available only for 41 of the 44 FP patients.
dMann–Whitney U-test, P = 0.01 versus OND.
Figure 2.
Distribution of anti-GAGA4 IgM levels in cohort-A [FP (n = 44) and OND (n = 44) patients]. Lines indicate SD ± mean. Crossing line indicates cutoff for defining antibody status. P-value (Mann–Whitney U) is FP group versus OND.
Using the results from the OND patients, we set a cutoff value for anti-GAGA4 IgM antibodies of mean OD + 2 SD as 0.53[OD/(Total IgM RFU × 106)0.5]. Using this cutoff value it was possible to identify patients who had high levels of anti-GAGA4, who were later diagnosed as RRMS with a sensitivity of 27.3% (95% -CI [15–43]) and specificity of 97.7% (95% CI [88–99]), PPV 92.3%, and NPV 52.3%.
Cohort-A: Identifying FP patients who will have a second attack within 24 months
Data regarding the time period between blood extraction and first relapse was available for 41/44 FP patients. Twenty-six out of forty-one FP patients (63%) had their first relapse within 2 years of blood sampling. Mean age of these patients was significantly lower than those suffering from a second attack later (mean age 34 versus 42 years, P = 0.001); however, no association was found between age and anti-GAGA4 IgM levels among the study population. To examine for a relationship between anti-GAGA4 IgM levels and the risk of an earlier (i.e. 2 vs. 4 years) second attack, we looked at patients whose anti-GAGA4 IgM levels were above the median antibody levels for the FP group as a whole. Sixteen out of twenty patients (80%) with antibody titers above median had a second clinical attack within 2 years compared to only 10/21 (47%) patients with titers equal or below the median (odds ratio 4.4 CI 95% 1.1–17.7, Fisher exact test, P = 0.05).
Cohort-B: Anti-GAGA4 IgM in FP-RRMS versus OND group
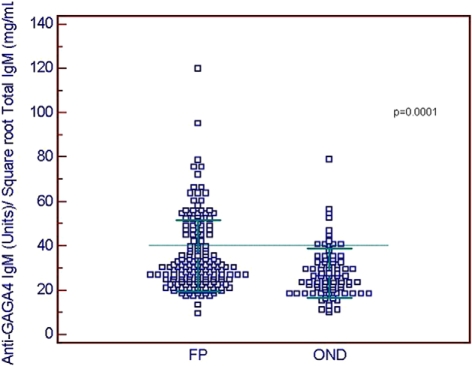
Clinical and demographic characteristics as well as anti-GAGA4 levels for cohort-B are described in Table 2. Total IgM levels were significantly higher in the FP group, and associated with gender and anti-GAGA4 IgM levels, therefore, we corrected the total IgM for gender by adding 0.17 (mg/mL)0.5 to all male samples. Anti-GAGA4 EU were normalized for total IgM in serum samples by dividing by the square root of total IgM (mg/mL)0.5 corrected to gender. There were significant differences between the OND group versus the FP group in mean age, gender composition, total IgM corrected for gender, and anti-GAGA4 IgM. However, more importantly, the levels of anti-GAGA4 corrected for total IgM was observed to be significantly higher (P = 0.0001, Mann–Whitney U-test) in FP patients as opposed to OND patients. Distribution of normalized anti-GAGA4 IgM in the FP and OND groups is shown in Figure 3.
Table 2.
Demographic, clinical characteristics and anti-GAGA4 IgM levels of cohort-B
| FP (n = 167) | OND (n = 85) OIND, n = 33, ONIND, n = 52 | Ottawa (n = 177) | Brussels (n = 75) | |
| Mean age, years (SD) | 37(10)a | 44 (10) | 39(11) | 39(10) |
| Female, n (%) | 126 (75)a | 44 (52) | 128 (72)b | 42 (56) |
| Center Ottawa, n (%) | 121 (72) | 56(66) | NA | NA |
| Total IgM(mg/mL)0.5, corrected for gender, mean (SD) | 1.32 (0.27)c | 1.21 (0.28) | 1.29 (0.28) | 1.25 (0.26) |
| Anti-GAGA4 IgM, Units, mean (SD) | 47.7 (27.1)c | 36.7 (33.5) | 46.3 (32.3)b | 38.6 (22.2) |
| Anti-GAGA4 IgM, Units/Total IgM (mg/mL)0.5, corrected for gender, mean (SD) | 36.4 (23.1)c | 29.9 (23.2) | 35.5 (25.8) | 31.2 (15.4) |
Other inflammatory neurological disease (OIND) group included the following: 1 bacterial meningitis, 1 Aspergillus meningitis, 5 viral meningitis, 4 optic neuritis, 1 cerebral vasculitis, 1 vasculitic neuropathy, 1 cerebral malaria, 2 myelitis, 1 neurosarcoidosis, 1 chronic meningitis, 1 neurosyphilis, 3 HIV encephalopathy, 1 Sjögren encephalopathy, 1 Grave's disease, 4 Guilain-Barre syndrome, 1 chronic inflammatory demyelinating polyneuropathy, 1 acute disseminated encephalomyelitis, 1 Brachial plexopathy, 1 carcinomatous meningitis, 1 infectious meningitis of unknown origin; Other non-inflammatory neurological disease (ONIND) group included the following: 1 adrenomyelopathy, 1 amyotrophic lateral sclerosis, 2 anxiety, 3 idiopathic intracranial hypertension, 2 cerebrovascular disease, 1 cervical cancer, 2 neurodegenerative dementia, 2 degenerative disc disease, 2 diabetic retinopathy, 1 dizziness, 1 facial myokimia, 2 fibromyalgia, 1 glioblastoma multiforme, 8 idiopathic headache, 1 nerve palsy, 1 intermittent diplopia, 2 labyrinthitis, 1 left sixth nerve palsy, 1 lymphoma of cavum, 1 meningismus, 1 motor neuron disease, 1 motor neuropathy, 1 myelopathy, 1 neuralgia, 1 neurogenic bladder, 1 nystagmus, 1 optic neuropathy left eye, 2 papilledema, 1 pituitary tumor, 1 psychiatric disorder, 1 quadriplegia, 1 tingling NYD, 1 vertical diplopia/mild ptosis, 2 vertigo; NA, not applicable.
aP < 0.05 versus OND.
bP < 0.05 versus Brussels.
cMann–Whitney U-test Total IgM FP vs. OND P = 0.004; Anti-GAGA4 IgM FP vs. OND P < 0.0001; Anti-GAGA4 IgM corrected for gender FP vs.OND P = 0.0001.
Figure 3.
Distribution of anti-GAGA4 IgM levels in cohort-B [FP patients (n = 167), and OND (n = 85)]. Lines indicate SD ± mean. Crossing line indicates cutoff value for antibody status. P-value (Mann-Whitney U) is FP group versus OND.
Using a cutoff of 42 anti-GAGA4 IgM (EU)/square root total IgM (mg/mL serum), we found that 44/167 (26.3%) FP patients were positive, whereas 77/85 (90.6%) OND patients were negative, corresponding to a sensitivity of 26.3% (95% CI [19.8–33.7]), a specificity of 90.6% (95% CI [82.3–95.4]), PPV of 84.6%, and NPV of 38.5%. Inter-plate CV for calibrator sample was 15%.
Cohort-C: Levels of anti-α glucose IgM in FP patients that will have a second early relapse (up to 24 months), versus late or no relapse
Demographics, clinical characteristics, and anti-glycan antibodies levels of FP (n = 100) patients who had early relapse (≤24 months, n = 58) versus late or no relapse (>24 months, n = 42) are described in Table 3.
Table 3.
Demographic characteristics, clinical characteristics, and anti-glycan antibodies levels of FP (n = 100) patients who had early relapse (≤24 months) versus late or no relapse (≥24 months) in cohort-C
| Early relapse, ≤24 m (n = 58) | Late or no relapse, ≥24 m (n = 42)a | |
| Mean age, years (SD) | 34.9 (10.9) | 36.2 (8.2) |
| Female, n (%) | 43 (74) | 29 (69) |
| Center Ottawa, n (%) | 22 (38) | 23 (54) |
| Square root total IgM, Mean mg/mL (SD) | 1.18 (0.26) | 1.13 (0.20) |
| Time to relapse, Mean months (SD)b | 11.4 (7.0) | 44.8 (18.8)c |
| Anti-GAGA2 IgM levels, Mean (SD) | 2.4 (1.3) | 2.2 (0.9) |
| Anti-GAGA3 IgM levels, Mean (SD) | 2.5 (1.3) | 2.2 (0.9) |
| Anti-GAGA4 IgM levels, Mean (SD) | 2.4 (1.3) | 2.0 (1.1) |
| Anti-GAGA6 IgM levels, Mean (SD)d | 3.1 (1.9) | 2.4 (1.1) |
SD, Standard deviation.
a11 patients remain still FP without drug treatment, 2 patients for 72 months and 9 patients for 48 months.
bCalculated only for patients who had relapse during the follow-up time.
cP < 0.0001, T-test.
dFisher exact test of anti-GAGA6 status (positive or negative) vs. early/late relapse, P = 0.015, Odds Ratio 6.4 (95%CI 1.4–29.8).
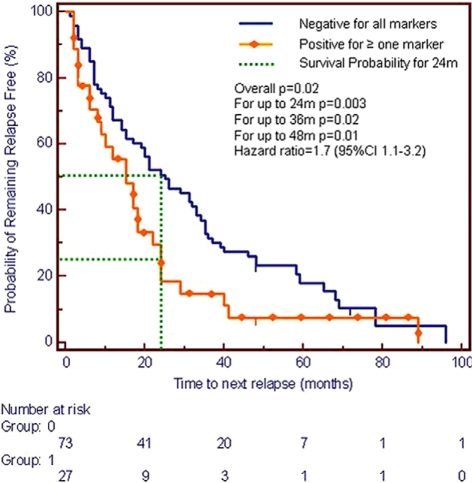
Except for time to first relapse, no significant differences were found among demographics, clinical characteristics, and square root total IgM of the early versus late relapsing group. Therefore, in this cohort, there was no need to correct for total IgM. Levels of all anti-glycan antibodies were higher in the early versus later relapsers, however, this did not reach statistical significance. To evaluate the possible relationship between levels of anti-α-glucose-based glycans IgM levels and the risk of imminent (i.e. within 24 months) first relapse, we looked at positive patients whose antibodies levels were above cutoff levels for at least one of the four antibodies versus patients negative for all four antibodies. Twenty-two (22/58 (38%) early relapsing patients were positive for at least one antibody compared to only 5/42 (12%) positive patients that had a late or no relapse at all, (P = 0.003 χ2 test, odds ratio = 4.5 (95% CI [1.5–13.2]), 0.0125 (Bonferroni correction) should be considered the significant threshold for this analysis since four different methods for determining the cutoff values of the antibodies was applied. In the group of patients who did not experience a second attack within the study period, only one was antibody-positive. Kaplan– Meier survival plot comparison (Figure 4) between cumulative risk of FP patients who were positive for at least one marker (anti-GAGA4, -GAGA2, -GAGA3, or -GAGA6 IgM) versus negative patients revealed significant differences between the groups (P = 0.0025 for up to 24 months, respectively) indicating that antibody positive patients consistently had their first relapse earlier. A high level in at least one of the anti-α-glucose IgM antibodies, identified 37.9% of FP patients who had an early attack (<24 months) versus those who had a late or no attack within the follow-up period with 88.1% specificity, 81.5% PPV, and 50.7% NPV (Table 4).
Figure 4.
Time to CDMS, Kaplan–Meier, survival plot for cohort-C. FP patients positive for ≥1 (anti-GAGA4, -GAGA2, -GAGA3, or -GAGA6 IgM) versus patients negative for all markers. Cutoff values were 4.0, 4.5, 4.5, and 4.3 for anti-GAGA2, -GAGA3, -GAGA4, and -GAGA6 IgM, respectively. P-values determined by log rank test. With Bonferroni correction only P-values below 0.0125 are considered significant.
Table 4.
Diagnostic characteristics for identification of FP patients who had an early relapse (≤24 months, n = 58) vs. late or no relapse (≥24 months, n = 42) using a panel of anti-α-glucose disaccharide and different cutoffs (Cohort C)
| Cutoff useda | Mean + SD | Mean + 1.5 SD | Mean + 2 SD | Best fit |
| Sensitivity, % (95% CI) | 37.9 (25.5-51.6) | 24.1 (13.9-37.2) | 15.5 (7.3-27.4) | 37.9 (25.5-51.6) |
| Specificity, % (95% CI) | 83.3 (68.6–93.0) | 88.1 (74.4–96.0) | 95.2 (83.8–99.4) | 88.1 (74.4–96.0) |
| PPV, % | 75.9 | 73.7 | 81.8 | 81.5 |
| NPV, % | 49.3 | 45.7 | 44.9 | 50.7 |
| Efficiency, % | 57.0 | 51.0 | 49.0 | 59.0 |
| Relative riskb | 1.5 | 2.5 | 3.3 | 3.2 |
SD, Standard deviation, CI, confidence intervals; PPV, positive predictive value; NPV, negative predictive value.
aCutoffs were calculated for each marker using mean of all 100 FP samples plus 1, 1.5, and 2 SD; PPV; and NPV.
bRelative risk of patient positive for at least one marker among the four markers for having second relapse in up to 24 months versus negative patients.
Discussion
A diagnostic or prognostic biomarker involving a simple serological test would represent a significant advance in the management of relapsing MS. There are numerous candidate serum antibodies that are purported to be useful as MS biomarkers. Of these, it is notable that a number of anti-glycan antibodies have been considered [2,3,10]. As a result of systematic screening using the GlycoChip® glycan array, we previously found significantly elevated levels of anti-GAGA4 IgM antibodies in MS patients compared to OND patients. These levels differentiated MS from OND with 57% sensitivity and 85% specificity [6].
The current work extends these observations by examining how early in the course of disease the antibodies can be found and determining whether their titers are predictive of disease activity.
Testing a total of 311 frozen sera samples taken from FP patients at or near the time of their first neurological event, and 129 samples from OND patients, we showed that MS patients express higher levels of anti-GAGA4 IgM antibodies, indicating that anti-glycan reactivity probably occurs very early in the disease course. More importantly, we were able to demonstrate that FP patients with higher levels of a panel of anti-α-glucose IgM antibodies had a higher probability for having a second attack within 24 months. In fact, patients who are positive for at least one of the anti-α-glucose IgM antibodies had significantly higher cumulative risk (Kaplan–Meier) for having an earlier relapse, identifying about a third of all the early relapsers. An interesting categorical analysis revealed that anti-GAGA6 status alone (positive or negative) had the strongest predictive value of an early relapse.
In the initial discovery phase [6] we screened 40 different glycans and found that IgM (not IgG or IgA) antibodies to α-glucose antigens could distinguish MS patients from OND controls. This type of IgM response to carbohydrates is most likely produced by self-replenishing B-1 B cells, which respond poorly to protein, but much better to carbohydrate antigens [11]. In general, B1 B-cells require a high amount of antigen for induction and play an important role as a first line of defense against invading pathogens, removal of senescent cells, cell debris, and other self-antigens [12,13]. Interestingly, serum-derived human IgM monoclonal antibodies were found to accumulate in areas of CNS damage and promote remyelination in demyelinated mice [14,15]. This possibly reflects a type of “house-keeping” role, a recognized property of these antibodies [12]. Also, in agreement with the present study, higher levels of IgM antibodies in CSF were found to predict a more severe MS course [16]. It would, therefore, be worthwhile to also test for the presence of anti-α-glucose IgM antibodies in the CSF of MS patients; although, a simple blood test would still be more preferable, especially if it needed to be repeated.
The biological basis of a humoral response to α-glucose antigen is still unclear, but it is of interest that this particular carbohydrate (α-glucose) is found within the type IV collagen matrix of the blood–brain barrier (BBB) [17]. A common structural feature of type IV collagen is hydroxyllysine-linked disaccharides that are comprised of α-glucose and β-galactose subunits (Glc(α1,2)Gal(β)) [18]. This disaccharide was previously reported to be the most important immunogenic antigen of patients having anti-glomerular basement membrane antibody–mediated glomerulonephritis [19]. As immune cells traverse the BBB, facilitated by the release of metalloproteases that help to further breakdown the BBB extracellular matrix, the ongoing inflammatory response can lead to the release of this carbohydrate antigen, thus stimulating an immune reaction. The subsequent development of IgM antibodies could then also contribute to further damage to the BBB by attacking the antigen in situ. Interestingly, type IV collagen deposits can also be found within MS plaques [20]. Also, similar to the present study, an IgM antibody response to glycans released from degrading collagen was reported for rheumatoid arthritis [21], where authors claimed that the natural IgM antibodies were produced against the glycosaminoglycans, including glucose molecules, which were degraded and released from the cartilage matrix. In addition, α-glucose–based polysaccharides are found in the cell wall of several pathogenic fungi [22] and bacteria [23,24]. This homology between known pathogens and a human α-glucose glycan may suggest that IgM antibodies could arise through the mechanism of molecular mimicry, triggering a cross-reactive response that targets the same glycan in the BBB [25].
As this was a retrospective study, we did not uniformly perform timely MRI studies as is the case today for making a definitive diagnosis based on the new McDonald criteria [26,27]. It might have been of interest to compare early MRI parameters predictive of disease to antibody levels to formulate an overall prediction of an early first relapse (i.e. CDMS). Analysis of the Early Treatment of MS (ETOMS) study population (308 FP patients and an abnormal MRI) showed that out of the 121 patients who converted to CDMS within 2 years of follow-up, 112 (93%) had ≥3 modified Barkhof MRI criteria [28]. However, 155 out of the 187 patients (83%) who didn't convert to CDMS within 24 months also had ≥3 modified Barkhof MRI criteria [26–30], yielding a 93% sensitivity, but only 17% specificity, PPV 42%, and NPV 78% for MRI predicting early CDMS conversion. MRI seems more sensitive at predicting ultimate vs. imminent conversion to CDMS. Although this cannot be directly compared to the diagnostic performance of antibody measurement in our retrospective study of FP patients (37% sensitivity, 88% specificity, 81% PPV, and 50% NPV), it suggests that measuring anti-α-glucose IgM levels could provide an independent and more specific predictive factor for early conversion to CDMS (within 24 months). Finding higher levels of serum anti-GAGA2, -GAGA3, -GAGA4, or -GAGA6 IgM antibodies in FP patients seems to predict, with high specificity, those who will convert to CDMS within 2 years. Such information might be invaluable for physicians having some difficulty in deciding upon a course of early therapy for their FP patients. Definitive conclusions can only be drawn, however, from a prospective study on additional cohorts that measures anti-glycan antibodies together with MRI and clinical outcomes.
Acknowledgments
Nir Dotan and Avinoam Dukler are employees and share holders in Glycominds Ltd., and have filed a patent regarding the use of anti-GAGA2, -GAGA3, -GAGA4, and -GAGA6, for diagnosis and prognosis of MS. Rom T. Altstock was a Glycominds Ltd. employee from July 2001 to September 2007. MSF received funds from Glycominds to offset the cost of preparing, coding and shipping samples for this study. The authors would like to acknowledge Dr. Jennifer Yarden for her assistance in preparation and reviewing of the manuscript, as well as for contributing the hypothesis regarding the source of anti-α-glucose antigens.
References
- 1.Freedman MS, Thompson EJ, Deisenhammer F, et al. Recommended standard of cerebrospinal fluid analysis in the diagnosis of multiple sclerosis: a consensus statement. Arch Neurol 2005;62:865–870 [DOI] [PubMed] [Google Scholar]
- 2.Lolli F, Mulinacci B, Carotenuto A, et al. An N-glucosylated peptide detecting disease-specific autoantibodies, biomarkers of multiple sclerosis. Proc Natl Acad Sci USA 2005;102:10273–10278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lolli F, Mazzanti B, Pazzagli M, et al. The glycopeptide CSF114(Glc) detects serum antibodies in multiple sclerosis. J Neuroimmunol 2005;167:131–137 [DOI] [PubMed] [Google Scholar]
- 4.Berger T, Rubner P, Schautzer F, et al. Antimyelin antibodies as a predictor of clinically definite multiple sclerosis after a first demyelinating event. N Engl J Med 2003;349:139–145 [DOI] [PubMed] [Google Scholar]
- 5.Kuhle J, Pohl C, Mehling M, et al. Lack of association between antimyelin antibodies and progression to multiple sclerosis. N Engl J Med 2007;356:371–378 [DOI] [PubMed] [Google Scholar]
- 6.Schwarz M, Spector L, Gortler M, et al. Serum anti-Glc(alpha1,4)Glc(alpha) antibodies as a biomarker for relapsing-remitting multiple sclerosis. J Neurol Sci 2006;244:59–68 [DOI] [PubMed] [Google Scholar]
- 7.Poser CM, Paty DW, Scheinberg L, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 1983;13:227–231 [DOI] [PubMed] [Google Scholar]
- 8.Schwarz M, Spector L, Gargir A, et al. A new kind of carbohydrate array, its use for profiling antiglycan antibodies, and the discovery of a novel human cellulose-binding antibody. Glycobiology 2003;13:749–754 [DOI] [PubMed] [Google Scholar]
- 9.Thomas DC, Clayton DG. Betting odds and genetic associations. J Natl Cancer Inst 2004;96:421–423 [DOI] [PubMed] [Google Scholar]
- 10.Menge T, Lalive PH, von Budingen HC, Cree B, Hauser SL, Genain CP. Antibody responses against galactocerebro-side are potential stage-specific biomarkers in multiple sclerosis. J Allergy Clin Immunol 2005;116:453–459 [DOI] [PubMed] [Google Scholar]
- 11.Goldsby RA, Kindt TJ, Osborne BA. Kuby Immunology. 4th ed. New York, NY, W.H. Freeman and Company; 2000 [Google Scholar]
- 12.Binder CJ, Shaw PX, Chang MK, et al. The role of natural antibodies in atherogenesis. J Lipid Res 2005;46:1353–1363 [DOI] [PubMed] [Google Scholar]
- 13.DeFranco AL, Locksley RM, Robertson M. Immunity: the immune response to infectious and inflammatory disease. London; New Science Press; 2007 [Google Scholar]
- 14.Pirko I, Ciric B, Gamez J, et al. A human antibody that promotes remyelination enters the CNS and decreases lesion load as detected by T2-weighted spinal cord MRI in a virus-induced murine model of MS. FASEB J 2004;18:1577–1579 [DOI] [PubMed] [Google Scholar]
- 15.Warrington AE, Bieber AJ, Ciric B, Pease LR, Van Keulen V, Rodriguez M. A recombinant human IgM promotes myelin repair after a single, very low dose. J Neurosci Res 2007;85:967–976 [DOI] [PubMed] [Google Scholar]
- 16.Mandrioli J, Sola P, Bedin R, Gambini M, Merelli E. A multifactorial prognostic index in multiple sclerosis. Cerebrospinal fluid IgM oligoclonal bands and clinical features to predict the evolution of the disease. J Neurol 2008;255:1023–1031 [DOI] [PubMed] [Google Scholar]
- 17.Steinman L. Multiple sclerosis: a two-stage disease. Nat Immunol 2001;2:762–764 [DOI] [PubMed] [Google Scholar]
- 18.Spiro RG. Characterization and quantitative determination of the hydroxylysine-linked carbohydrate units of several collagens. J Biol Chem 1969;244:602–612 [PubMed] [Google Scholar]
- 19.Mahieu PM, Lambert PH, Maghuin-Rogister GR. Primary structure of a small glycopeptide isolated from human glomerular basement membrane and carrying a major antigenic site. Eur J Biochem 1973;40:599–606 [DOI] [PubMed] [Google Scholar]
- 20.van Horssen J, Bö L, Dijkstra CD, de Vries HE. Extensive extracellular matrix depositions in active multiple sclerosis lesions. Neurobiol Dis 2006;24:484–491 [DOI] [PubMed] [Google Scholar]
- 21.Gyorgy B, Tothfalusi L, Nagy G, et al. Natural autoantibodies reactive with glycosaminoglycans in rheumatoid arthritis. Arthritis Res Ther 2008; 10: R110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Masuoka J. Surface glycans of Candida albicans and other pathogenic fungi: physiological roles, clinical uses, and experimental challenges. Clin Microbiol Rev 2004;17:281–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hellerqvist CG, Lindberg B, Sigfrid S, Holme T, Lindberg AA. Structural studies on the O-specific sidechains of the cell-wall lipopolysaccharide from Salmonella typhimurium 395 ms. Carbohydr Res 1968;8:43–55 [Google Scholar]
- 24.Lind S, Lindberg AA. Epitope size, specificity and equilibrium constant for four monoclonal antibodies binding to the O:4 polysaccharide antigen of Salmonella sero-group B bacteria. Mol Immunol 1992;29:1013–1023 [DOI] [PubMed] [Google Scholar]
- 25.Bach JF. Infections and autoimmune diseases. J Autoimmun 2005; 25(Suppl.): 74–80 [DOI] [PubMed] [Google Scholar]
- 26.McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 2001;50:121–127 [DOI] [PubMed] [Google Scholar]
- 27.Polman CP, Reingold SC, Edan G, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 2005;58:840–846 [DOI] [PubMed] [Google Scholar]
- 28.Barkhof F, Rocca M, Francis G, et al. Validation of diagnostic magnetic resonance imaging criteria for multiple sclerosis and response to interferon beta1a. Ann Neurol 2003;53:718–724 [DOI] [PubMed] [Google Scholar]
- 29.Barkhof F, Filippi M, Miller DH, et al. Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain 1997;120:2059–2069 [DOI] [PubMed] [Google Scholar]
- 30.Tintoré M, Rovira A, Martínez MJ, et al. Isolated demyelinating syndromes: comparison of different MR imaging criteria to predict conversion to clinically definite multiple sclerosis. AJNR Am J Neuroradiol 2000;21:702–706 [PMC free article] [PubMed] [Google Scholar]