Abstract
Individuals who experience one type of trauma often experience other types, yet few studies have examined the clustering of trauma. This study examines the clustering of traumatic events and associations of trauma with risk for single and co-occurring major depressive disorder (MDD) and panic attack for 20 years after first trauma. Lifetime histories of MDD, panic attack, and traumatic events were obtained from participants in an Australian twin sample. Latent class analysis was used to derive trauma classes based on each respondent’s trauma history. Associations of the resulting classes and of parental alcohol problems and familial effects with risk for a first onset of single and co-occurring MDD and panic attack were examined from the year of first trauma to 20 years later. Traumatic events clustered into three distinct classes characterized by endorsement of little or no trauma, primarily nonassaultive, and primarily assaultive events. Individuals in the assaultive class were characterized by a younger age at first trauma, a greater number of traumatic events, and high rates of parental alcohol problems. Members of the assaultive trauma class had the strongest and most enduring risk for single and co-occurring lifetime MDD and panic attack. Assaultive trauma outweighed associations of familial effects and nonassaultive trauma with risk for 10 years following first trauma.
Keywords: trauma, depression, panic, latent class analysis
Experience of traumatic events is not uncommon in the population, and individuals who experience one event often experience several types of trauma (Breslau et al., 1998). Individuals with histories of childhood abuse, in particular, are likely to report additional traumatic events (Edwards et al., 2003; Kessler et al., 1997) and other markers of early adversity, such as parental alcohol problems, inter-parental violence and parental divorce (Dong et al., 2004; Anda et al., 2002; Dube et al., 2001). Childhood trauma is associated with increased risk for mood and anxiety disorders in cross-sectional (Dinwiddie et al., 2000; Edwards et al., 2003; Kessler et al., 1997; McCutcheon et al., 2009; Nelson et al., 2002) and longitudinal studies (Copeland et al., 2007; Fergusson et al., 2008). Associations of single events, such as childhood sexual or physical abuse, with the onset of mood and anxiety disorders is diminished when controlling for other early adversities such as parental separation and parental alcohol use (Kessler et al., 1997). This attenuation suggests that the clustering of different types of adversity, rather than the unique effects of individual events, accounts for the increased risk for mood and anxiety disorders among individuals with histories of childhood trauma (Kessler et al., 1997).
Anxiety symptoms and disorders often occur with depression (Kessler et al., 1994; Robins & Regier, 1991). Depression-panic disorder comorbidity is a frequent mood-anxiety disorder diagnosis in both treatment and community samples (Kessler et al., 1998; Merikangas et al., 1996; Merikangas et al., 1998). Panic attacks, the requisite symptom for panic disorder, also occur in the context of mood disorders (American Psychiatric Association, 2000), and have been conceptualized as severity markers for major depressive disorder (MDD; Kessler et al., 1998). Twenty-two per cent of individuals with lifetime MDD have experienced a panic attack and 10% meet criteria for panic disorder; rates of lifetime MDD among individuals with histories of panic attack or disorder are also high, 56% and 51%, respectively (Kessler et al., 1998). Individuals with lifetime histories of both MDD and panic attacks experience an earlier onset and more severe course of disorder than individuals with a history of either disorder alone (Kessler et al., 1998; Andrade et al., 1996; Roy-Byrne et al., 2000).
Traumatic events are associated with increased risk for MDD (Anda et al., 2002; Dinwiddie et al., 2000; Kendler et al., 2000; Kessler et al., 1997) and panic attacks (Dinwiddie et al., 2000; Kendler et al., 2000; Kessler et al., 1997), and the association between MDD and panic attack is reduced when controlling for events such as rape, life-threatening accidents or natural disasters, and early adversities like parental depression or alcoholism (Kessler et al., 1998). These findings, in combination with evidence that early trauma can induce physiological changes that increase vulnerability to stress and subsequent risk for psychopathology (Heim & Nemeroff, 2001; Gutman & Nemeroff, 2003) suggest that early trauma may contribute to a general risk for co-occurring disorders.
The aims of the current study were to (1) examine the clustering of trauma in a population-based twin sample using latent class analysis, and (2) test associations of trauma classes with risk for MDD and panic attack for 20 years following first trauma, and whether these associations varied as a function of single versus co-occurring lifetime disorder and as a function of time since the occurrence of first trauma, while controlling for parental alcohol problems and familial effects on risk.
Methods
Subjects
Subjects were from twin pairs born between 1964 and 1971 in Australia and recruited into the Australian Twin Register via mass media and school system appeals to their parents between 1980–1982. Participants completed a structured diagnostic interview (Bucholz et al., 1994) administered via telephone during 1996–2000 from which data for the current study were derived. Informed consent was obtained from all participants prior to the interview. The institutional review boards of Washington University School of Medicine, St. Louis, MO, USA, and of the Queensland Institute of Medical Research, Brisbane, Queensland, Australia, approved the informed consent procedure.
Of 4262 twin pairs enrolled in the young adult cohort of the twin panel, 6% could not be located for participation despite efforts to locate family members. Of the remaining 4010 twin pairs that were located and solicited for telephone interviews, both members of 2765 pairs (69% pair-wise response rate) and one member only of 735 pairs completed interviews, an overall response rate of 78% (Lynskey et al., 2003; Lynskey et al., 2002; Nelson et al., 2002). Data from 2590 twin pairs with complete data on depression, panic attack, and traumatic event items were included in these analyses, comprising 1118 monozygotic (MZ) pairs (659 female and 459 male pairs) and 1472 dizygotic (DZ) pairs (486 female, 370 male, and 616 opposite-sex pairs). The median age at time of interview was 30, with a range of 24 to 36. Twins excluded from the analysis due to missing data had significantly higher rates of childhood neglect (4% vs. 1%, OR = 3.2, 95% CI = 2.1–4.8), childhood physical abuse (6% vs. 3%, OR = 2.3, 95% CI = 1.6–3.1), severe physical assault (11% vs. 9%, OR = 1.3, 95% CI = 1.0–1.6), being threatened with a weapon or kidnapped (11% vs. 7%, OR = 1.6, 95% CI = 1.3–2.0), and MDD (32% vs. 28%, OR = 1.3, 95% CI = 1.1–1.5), compared to the analysis sample.
Assessment
The Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) (Bucholz et al., 1994; Hesselbrock et al., 1999) was adapted for telephone use in Australia and administered by trained lay interviewers. Lifetime MDD and panic disorder were retrospectively assessed during the interview and were defined according to DSM-IV criteria (American Psychiatric Association, 1994). Because the prevalence of panic disorder in the sample was too low to provide reliable estimates of risk (1.8 %), we used history of panic attack as our dependent variable. Panic attack was defined as at least 2 attacks with 4 or more panic symptoms which began suddenly and reached a peak within 10 minutes (American Psychiatric Association, 1994). We created a 4-level variable representing lifetime history of MDD only, panic attack only, MDD + panic attack, and neither. Age at onset of MDD and panic attack were defined as age of first major depressive episode or panic attack, respectively. For individuals with lifetime histories of both MDD and panic attack, age at onset was defined as age at first major depressive episode or panic attack, whichever occurred first.
Lifetime experience of traumatic events was assessed using items from the NCS (Kessler et al., 1995) which qualified as traumatic events according to DSM-III-R (American Psychiatric Association, 1987) criteria for posttraumatic stress disorder. Ages at first and last experience of each endorsed traumatic event were obtained. Childhood sexual abuse was coded positive if the respondent reported rape or sexual molestation before age 18 during the traumatic event section or endorsed an item from the home environment section of the interview about forced sexual contact inside or outside of family before age 16 (Nelson et al., 2006; Nelson et al., 2002). The minimum age at onset from these items was used as the age at onset for CSA. Rape and molestation that occurred at age 18 and older were coded as adult events.
Alcohol problems in the respondent’s biological mother or father were assessed with two questions: ‘Did drinking ever cause your mother/father to have problems with health, family, job, police, or other problems?’ and ‘Did you ever feel that your mother/father was an excessive drinker?’ This method of measuring alcohol problems in respondent’s parents has been found to have good interrater reliability with no evidence of bias due to respondent’s own alcohol use or history of anxious or depressed states (Slutske et al., 1996).
Trauma Classes
Latent class analysis (LCA, McCutcheon, 1987; Neuman et al., 1999) was used to estimate trauma classes based on each individual’s reported traumatic experiences. Latent class analysis is a categorical variant of factor analysis that helps to determine whether the observed correlation between measured items (e.g., traumatic events) is the effect of an unmeasured variable or set of variables. Classes resulting fom LCA are mutually exclusive and individuals within each class are assumed to share some underlying, unobserved factor which explains their class assignment. In the current analysis, individuals were assigned to classes based on the types and numbers of traumatic events endorsed. Since respondents were instructed to report each traumatic event only once (e.g., childhood physical abuse could not also be reported as physical assault), any clustering of traumatic events would imply that more individuals were experiencing multiple traumatic events than would be predicted by chance alone. The Bayesian Information Criterion was used to assess the fit of models estimating from 2 to 12 classes.
For purposes of discussion, the terms ‘assaultive’ and ‘nonassaultive’ events, following previous work on posttraumatic stress disorder (Breslau et al., 1998), were used in the results and discussion sections. Assaultive events comprised CSA and physical abuse and neglect, adult rape and sexual molestation, severe physical assault, and being threatened with a weapon or kidnapped. Although childhood neglect is not by definition assaultive, its frequent co-occurrence with early assaultive events warrants its inclusion in this category (Dong et al., 2004). Nonassaultive events comprised life-threatening accident, witnessing injury or killing, and natural disaster.
Statistical Methods
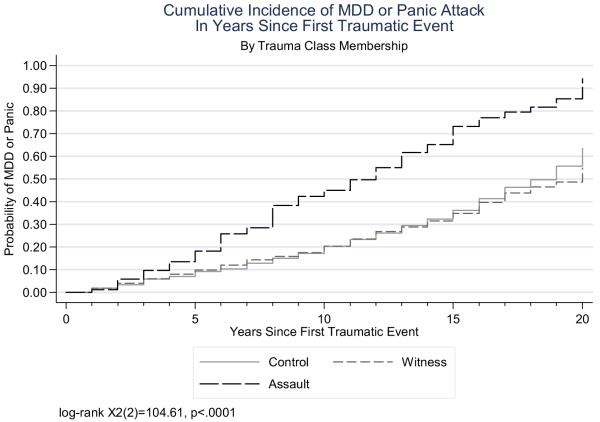
The 4-level variable representing lifetime history of MDD and panic attack served as the dependent variable in multinomial logistic regressions, with the no-MDD, no-panic attack category as the reference group. We tested the association of trauma class membership with risk for single and co-occurring MDD and panic attack during the year of first reported trauma and 1, 5, 10, 15, and 20 years following first trauma occurrence. The beginning of the risk period for individuals who endorsed trauma was age at first reported event; for individuals who endorsed no trauma, the risk period was not restricted by age. At each time point, the risk set for a first onset of depression or panic attack included only individuals with no prior onset by that point in time. Wald chi-square tests were used to test differences in associations of trauma classes with MDD-only versus panic attack-only versus MDD + panic attack. Survival analysis was used to compute Kaplan-Meier failure curves to visually represent the cumulative risk for onset of MDD or panic attack in years since first traumatic event, using age at first reported trauma as the beginning of the risk period. The assumption that the risks of the classes were proportional over time was tested using Schoenfeld residuals (Grambsch & Therneau, 1994), while controlling for gender. The assumption was not violated (χ2(3) = .91, p = .82).
Familial effects, a broad estimate of genetic influences on risk, were modeled as the interaction between twin pair zygosity and co-twin lifetime status on MDD or panic attack. A single variable representing co-twin history of MDD or panic attack (coded ‘1’ if history of either) was created to model familial effects on respondent risk because data on panic attack were too sparse to permit estimation of separate interaction terms. A significant interaction of co-twin history of MDD or panic attack with zygosity reflects greater familial risk among MZ than DZ twins. Since MZ twins share 100% of their genetic material while DZ twins share on average 50%, this suggests a genetic efffect on risk.
Variables and datasets were created using SAS software, Version 9.0. (2004). Multinomial logistic regression analyses were performed using the Stata Statistics and Data Analysis Package (Stata Corporation, 2004) with adjustment for the non-independence of observations in twin data. Wald chi-square tests were used to test differences between trauma classes, diagnostic categories, and genders. Statistical significance was designated as a p-value of .05 or less.
Results
Trauma Class Characteristics
Fifty-three per cent of the sample as a whole reported at least one traumatic event. A three class solution provided the best fit to the traumatic event data based on evaluation of Bayesian Information Criterion (BIC) for 2 through 12 classes, with the 3-class solution having the lowest BIC value (2 classes: 27590.6, 3 classes: 27483.7, 4 classes: 27510.6). Eighty-two per cent of the sample was assigned to a class in which fewer than half (43%) of individuals endorsed a traumatic event. All individuals who reported no history of trauma were assigned to this class. Women comprised the majority of this class (60%) in which nonassaultive events and CSA were the most frequently endorsed events (Table 1). This ‘Control’ class was the comparison group for the other two classes. The next most populous class (13% of the sample) was 74% male and characterized by high endorsement of nonassaultive events. Eighty-seven per cent of individuals assigned to this ‘Witness’ class endorsed having witnessed an injury or killing.
Table 1.
Sample Characteristics and Trauma Endorsement for Total Sample and by Trauma Class
| Trauma Classes (class prevalence) | ||||
|---|---|---|---|---|
| Total Sample (n = 5180) |
Control (.82) (n = 4257) |
Witness (.13) (n = 689) |
Assault (.05) (n = 234) |
|
| Assaultive events, % | ||||
| Childhood physical abuse | 3.0 | 1.1 | 1.0 | 44.1 |
| Childhood sexual abuse | 11.1 | 7.9 | 8.7 | 72.6 |
| Childhood neglect | 1.2 | 0 | 0 | 27.3 |
| Rape (≥ age 18) | 2.3 | 1.7 | 0.9 | 18.4 |
| Sexual molestation (≥ age 18) | 1.5 | 0.6 | 1.6 | 16.7 |
| Serious physical assault | 9.4 | 3.1 | 33.7 | 53.0 |
| Threatened with weapon or kidnapped | 7.3 | 2.9 | 29.2 | 23.9 |
| Nonassaultive events, % | ||||
| Witness to injury or killing | 23.0 | 12.1 | 86.6 | 33.8 |
| Life-threatening accident | 18.9 | 11.6 | 58.5 | 33.3 |
| Fire, flood or natural disaster | 9.2 | 9.2 | 39.5 | 18.8 |
| Age at first event, M (SD) | 15.4 (7.2)A | 16.7 (7.3)B | 14.4 (5.8) | 8.4 (5.2) |
| Number events endorsed, M (SD) | 1.7 (1.0)A | 1.2 (0.4)B | 2.6 (0.8) | 3.4 (1.3) |
| MDD and/or panic attack | ||||
| MDD only | 23.0 | 21.6 | 25.5 | 41.0 |
| Panic attack only | 3.1 | 3.0 | 3.3 | 4.5 |
| MDD + panic attack | 5.0 | 3.9 | 6.7 | 20.9 |
| No MDD or panic attack | 68.9 | 71.5 | 64.4 | 33.7 |
| Alcohol dependence | 21.6 | 18.7 | 33.4 | 38.0 |
| Antisocial personality symptoms (2 or more) | 19.8 | 15.0 | 41.6 | 42.7 |
| Parental alcohol problems, % | 24.9 | 22.8 | 30.2 | 48.7 |
based on 2764 individuals who endorsed trauma
based on men (n = 822) and women (n = 1019) who endorsed trauma
The remaining 5% of the sample was assigned to a predominantly female (74%) ‘Assault’ class characterized by a young age at first trauma and high endorsement of assaultive events, particularly CSA, childhood physical abuse and serious physical assault. Seventy-eight percent of the members of this class experienced their first trauma before age 13. Alcohol dependence, symptoms of antisocial personality, and parental alcohol problems were common in this class. Eleven percent of individuals in the Assault class reported both parents had alcohol problems, versus 2.2% in the Witness and 1.5% in the Control classes. Fewer individuals in the Assault class than in the Control and Witness classes reported being raised by both biological parents (68% vs. 85% and 84%, respectively), and more reported being financially worse off than other families in their childhood neighborhoods (31% vs. 9% and 11%, respectively).
A majority (66%) of individuals in the Assault class met criteria for MDD, panic attack, or both, with particularly high rates of co-occurring MDD + panic attack; 19% of co-occurring cases were in this class which comprised just 5% of the sample. Ages at onset of MDD and panic were younger in the Assault class than in the Control and Witness classes. By age 12, 14% of individuals in the Assault class had experienced their first major depressive episode or panic attack, versus 4% and 2% in the Witness and Control classes, respectively. By age 18, these numbers were 35% (Assault), 13% (Witness), and 8% (Control). First panic attack occurred earlier than first major depressive episode in each of the classes (M [sd] for panic attack, MDD: Control: 19.9 [6.5], 22.8 [5.2]; Witness: 18.2 [7.9], 22.4 [5.5]; Assault: 17.1 [6.8], 19.8 [6.2]).
Displayed in Figure 1 are Kaplan-Meier curves representing the cumulative risk for a first onset of MDD or panic attack by trauma class membership, using age at first trauma as the beginning of the risk period. Time is thus measured in number of years since first traumatic event, rather than age at onset of MDD or panic. Individuals in the Control class who endorsed no trauma were excluded. The accumulation of risk in the Assault class was greater than accumulation in the Control or Witness classes (χ2(2) = 104.61, p < .0001), and the difference in risk persisted until 20 years after first reported trauma. There was no significant difference in risk between the Control and Witness classes (χ2(1) = 0.4, p = .51).
Figure 1.
Kaplan-Meier curves of cumulative onset of MDD and panic attack since first reported trauma, by trauma class membership.
Note: Control class limited to individuals who reported traumatic event, N = 2764
Associations With Risk for MDD and Panic Attack
Global Wald tests (Long & Freese, 2003) comparing all coefficients in the MDD-only and panic attack-only categories indicated that they could be collapsed from the year of first trauma (χ2(9) = 1.4, p = .99), and at each time point tested thereafter up to fifteen years following first trauma (χ2(9) = 10.3, p = .32; equations included familial effects, trauma classes and control variables). The following results up to fifteen years after first trauma are thus based on multinomial regressions with a 3-level dependent variable (no MDD or panic attack [referent], MDD or panic attack only, MDD + panic attack).
Presented in Table 2 are results showing associations of trauma classes, parental alcohol problems, and familial effects with MDD or panic attack only and with MDD + panic attack from year of first trauma until 20 years following first traumatic event. Assault class membership was associated with risk for single and co-occurring MDD and panic attack for 20 years following first reported trauma. The association of the Assault class with risk for co-occurring MDD and panic attack was stronger than its association with either disorder alone from the year of first trauma (χ2(1) = 11.52, p < .0001) until 5 years later (χ2(1) = 5.7, p < .05), and its association with risk for co-occurring MDD + panic attack outweighed Witness class membership, familial effects, and parental alcohol problems from year of first trauma (χ2(3) = 29.3, p < .0001) until 10 years later (χ2(3) = 9.3, p < .05). By 20 years after first trauma the data were too sparse to estimate single and co-occurring MDD and panic attack separately, so the categories were collapsed. Twenty years after first reported trauma, Assault class membership still outweighed the influence of familial effects, parental alcohol problems, and Witness class membership on risk for MDD or panic attack (χ2(3) = 15.5, p = .0014).
Table 2.
Multinomial Regressions Showing Associations of Trauma Classes, Parental Alcohol Problems and Familial Effects with Single and Co-Occurring Lifetime MDD and Panic Attack at 0, 1, 5, 10, 15, and 20 Years After First Traumatic Event
| MDD or panic attack only | MDD + panic attack | ||
|---|---|---|---|
| Years since first trauma | N1 | RR (95% CI) | RR (95% CI) |
| 0 | 4325 | ||
| Assault class 2 | 6.0 (4.3 – 8.4)** | 14.3 (8.4 – 24.5)** | |
| Witness class | 2.8 (2.2 – 3.5)** | 3.9 (2.3 – 6.7)** | |
| Parental alcohol problems | 1.6 (1.3 – 2.0)** | 2.3 (1.5 – 3.5)** | |
| Familial effect 3 | 2.6 (1.6 – 4.2)** | 2.5 (1.0 – 6.0)* | |
| 1 | 4287 | ||
| Assault class | 6.4 (4.5 – 9.0)** | 14.7 (8.5 – 25.4)** | |
| Witness class | 2.8 (2.2 – 3.5)** | 3.7 (2.2 – 6.5)** | |
| Parental alcohol problems | 1.7 (1.4 – 2.0)** | 2.4 (1.6 – 3.6)** | |
| Familial effect | 2.8 (1.7 – 4.5)** | 2.3 (0.9 – 5.8) | |
| 5 | 4130 | ||
| Assault class | 7.0 (4.8 – 10.0)** | 14.2 (7.7 – 26.3)** | |
| Witness class | 3.0 (2.3 – 4.0)** | 3.2 (1.6 – 6.5)** | |
| Parental alcohol problems | 1.6 (1.3 – 2.0)** | 2.4 (1.5 – 4.0)** | |
| Familial effect | 2.9 (1.7 – 4.9)** | 2.1 (0.7 – 5.9) | |
| 10 | 3930 | ||
| Assault class | 7.4 (4.9 – 11.1)** | 9.8 (4.3 – 22.4)** | |
| Witness class | 3.1 (2.3 – 4.3)** | 2.3 (0.8 – 6.9) | |
| Parental alcohol problems | 1.5 (1.2 – 2.0)** | 2.8 (1.4 – 5.7)** | |
| Familial effect | 3.0 (1.7 – 5.4)** | 2.4 (0.5 – 10.7) | |
| 15 | 3734 | ||
| Assault class | 7.6 (4.4 – 13.1)** | 3.5 (1.0 – 12.3)* | |
| Witness class | 3.3 (2.1 – 5.2)** | 1.7 (0.4 – 6.8) | |
| Parental alcohol problems | 1.6 (1.1 – 2.3)* | 4.0 (1.5 – 10.5)** | |
| Familial effect | 3.3 (1.5 – 7.2)** | 0.9 (0.1 – 6.4) | |
| 20 a | 3625 | ||
| Assault class | 11.8 (5.7 – 24.4)** | ||
| Witness class | 3.4 (1.7 – 6.8)** | ||
| Parental alcohol problems | 1.7 (0.9 – 2.9) | ||
| Familial effect | 1.9 (0.6 – 6.0) | ||
Ns decrease as individuals with a first onset of MDD or panic attack before the beginning of the next time interval are removed from the risk set;
Control class is the reference category
familial effect modeled as interaction of twin zygosity (monozygotic = 1, dizygotic = 0) with co-twin status on MDD or panic attack (‘1’ if either)
MDD-only, panic attack-only, and MDD + panic attack categories were combined due to too few individuals left in risk sets for panic attack or MDD-only and MDD + panic attack to permit separate estimation. All regressions adjusted for respondent zygosity, gender, alcohol dependence, antisocial personality symptoms, and co-twin status on MDD and panic attack
p < .05
p < .01
Discussion
In the current study, childhood and assaultive trauma clustered into one class comprising five percent of the sample in which lifetime MDD, MDD-panic attack co-occurrence and parental alcohol problems were over-represented. Individuals in this assaultive trauma class had increased risk for a first onset of MDD or panic attack that persisted for 20 years after the first reported traumatic event, and were at especially high risk for co-occurring MDD and panic attack.
The clustering of traumatic events into three distinct classes is consistent with evidence that traumatic events are not randomly distributed in the population (Breslau et al., 1998; Kessler et al., 1997; Kessler et al., 1995). The differing trauma profiles of the classes suggest underlying contextual differences between them that are captured by the types of trauma endorsed by their respective members. For example, individuals assigned to the Witness class, with its high prevalence of life-threatening accidents and witnessing injury, may have in common a temperamental predisposition to thrill-seeking (Scarr & McCartney, 1983) and reckless driving, which puts them at risk for car accidents. Family dysfunction might be the underlying factor common to individuals assigned to the Assault class, with its high rates of childhood abuse and neglect. Parental alcohol problems, most prevalent in this class, are associated with increased risk for early trauma (Anda et al., 2002; Dinwiddie et al., 2000; Fergusson et al., 1996), and thus may contribute to the contextual risk associated with class membership. Another study in which a latent class analysis of trauma was performed included an array of early risk factors in the classes in addition to childhood sexual, physical and emotional abuse (Menard et al., 2004). In that study, the class with the highest probability of childhood trauma also had the highest probabilities of low parental warmth, parental suicidal behavior and mental illness, substance abuse by a household member, and presence of non-nuclear family members in the household (Menard et al., 2004). In the current study, parental alcohol problems, especially in both parents, were over-represented in the Assault class, and a majority of individuals in this class experienced their first trauma before age 13, consistent with an interpretation of heightened childhood risk due to the family environment.
The persistent association of Assault class membership with risk for MDD or panic attack and their co-occurrence is in accord with evidence that trauma may increase vulnerability to a range of disorders. A recent example of the association of childhood adversity with long-term risk for psychiatric disorder came from a study using data the National Comorbidity Survey (NCS; Kessler et al., 2008). Childhood physical and sexual abuse and neglect and parental substance disorder reported during the first NCS were associated in the follow-up survey, approximately ten years later, with first-onset of generalized anxiety disorder into adolescence and with first-onset of major depressive disorder into adulthood; childhood abuse also predicted the persistence of both disorders (Kessler et al., 2008).
Because PTSD was not assessed in the current study we were unable to examine associations of trauma classes with risk for MDD-PTSD co-occurrence. However, recent prospective studies have found associations of early trauma with increased risk for childhood-onset PTSD symptoms, anxiety and depressive disorders (Copeland et al., 2007) and with increased risk for depression into adulthood (Maercker et al., 2004; Spatz Widom et al., 2007). A study of PTSD-MDD comorbidity found that trauma-exposed individuals had increased risk for MDD subsequent to trauma only if they had previous PTSD; those with no history of PTSD had no increased risk for MDD (Breslau et al., 2000). The authors suggest that common vulnerabilities may influence the development of PTSD and MDD in trauma victims and also may exacerbate pre-existing vulnerabilities which then increase risk for subsequent disorder (Breslau et al., 2000). In the same study, traumatic event data from the NCS were analyzed to examine whether different types of trauma had differential effects on risk for first-onset MDD following trauma among individuals with and without a history of PTSD. The authors found little evidence for differential effects by type of trauma (Breslau et al., 2000), but the analysis excluded childhood physical abuse and neglect, two events with strong associations with MDD risk (McCutcheon et al., 2009). The current study did find differential effects of trauma class membership with risk for first-onset MDD or panic attack for 10 years after first trauma, with the Assault class having a stronger association with risk than the Witness class. This difference is due in part to the use of latent class analysis as opposed to examining each traumatic event in isolation. The trauma classes, based on each individual’s aggregate experience of trauma, also represent the underlying context in which trauma occurs. This context may contribute to an enhanced vulnerability, or may be a marker for an existing vulnerability that is not detected when examining events in isolation.
This study’s limitations include its reliance on retrospective recall of traumatic events, depressive symptoms and panic attack and their ages at occurrence. However, the similarity of these findings with those from prospective studies (Copeland et al., 2007; Maercker et al., 2004) increases our confidence that recall bias has not inflated our results. The group excluded from analysis due to missing data endorsed higher rates of trauma and MDD, but strong effects of assaultive trauma were found despite the exclusion of this high-risk group. The convergence of findings from this study with those from other studies of trauma as it influences psychiatric risk (Anda et al., 2002; Dinwiddie et al., 2000; Kendler et al., 2000), along with evidence of physiological changes associated with early trauma (De Bellis & Kuchibhatla, 2006; Heim et al., 2001; Teicher et al., 2004) contributes to a growing body of evidence that early experience can have long-term effects on mental health.
The latent class analysis of trauma items in this study specified a minority of individuals at particularly high risk for early trauma and who have a persistent risk for MDD and panic attack. Future work will include greater specification of factors associated with trauma classes at different time points which may provide clues to preventive interventions to reduce the risk of trauma exposure or to reduce the risk of developing illness following trauma exposure.
Acknowledgments
Supported by grants AA07728, AA11998, AA10248, AA13446, T32 AA07580, T32 MH19960, F31 MH071039-01. Portions of this paper were presented at the annual meeting of the American Psychopathological Association meeting in March, 2006.
Footnotes
Corresponding and contributing authors have no conflicts of interest to report.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-III-R) American Psychiatric Association; Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-IV) American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, Williamson DF. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric Services. 2002;53:1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- Andrade L, Eaton WW, Chilcoat HD. Lifetime co-morbidity of panic attacks and major depression in a population-based study: Age of onset. Psychological Medicine. 1996;26:991–996. doi: 10.1017/s0033291700035315. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder-major depression connection. Biological Psychiatry. 2000;48:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of the SSAGA. Journal of Studies on Alcohol and Drugs. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Kuchibhatla M. Cerebellar volumes in pediatric maltreatment-related posttraumatic stress disorder. Biological Psychiatry. 2006;60:697–703. doi: 10.1016/j.biopsych.2006.04.035. [DOI] [PubMed] [Google Scholar]
- Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PA, Slutske WS, Bierut LJ, Statham DB, Martin NG. Early sexual abuse and lifetime psychopathology: A co-twin-control study. Psychological Medicine. 2000;30:41–52. doi: 10.1017/s0033291799001373. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect. 2004;28:771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Croft JB, Edwards VJ, Giles WH. Growing up with parental alcohol abuse: Exposure to childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect. 2001;25:1627–1640. doi: 10.1016/s0145-2134(01)00293-9. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse and Neglect. 2008;32:607–619. doi: 10.1016/j.chiabu.2006.12.018. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. Childhood sexual abuse and psychiatric disorder in young adulthood: I. Prevalence of sexual abuse and factors associated with sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1355–1364. doi: 10.1097/00004583-199610000-00023. [DOI] [PubMed] [Google Scholar]
- Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- Gutman DA, Nemeroff CB. Persistent central nervous system effects of an adverse early environment: Clinical and preclinical studies. Physiology and Behavior. 2003;79:471–478. doi: 10.1016/s0031-9384(03)00166-5. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Bonsall R, Miller AH, Nemeroff CB. Altered pituitary–adrenal axis responses to provocative challenge tests in adult survivors of childhood abuse. American Journal of Psychiatry. 2001;158:575–581. doi: 10.1176/appi.ajp.158.4.575. [DOI] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA: A comparison with the SCAN. Addiction. 1999;94:1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Comorbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychological Medicine. 2008;38:365–374. doi: 10.1017/S0033291707002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang PE, Wittchen HU, Ustun TB, Roy-Burne PP, Walters EE. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Archives of General Psychiatry. 1998;55:801–808. doi: 10.1001/archpsyc.55.9.801. [DOI] [PubMed] [Google Scholar]
- Long JS, Freese J. Regression models for categorical dependent variables using Stata, Revised edition. Stata Press; College Station, TX: 2003. [Google Scholar]
- Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, Statham DJ, Martin NG. Escalation of drug use in early-onset cannabis users vs. co-twin controls. Journal of the American Medical Association. 2003;289:427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Heath AC, Nelson EC, Bucholz KK, Madden PA, Slutske WS, Statham DJ, Martin NG. Genetic and environmental contributions to cannabis dependence in a national young adult twin sample. Psychological Medicine. 2002;32:195–207. doi: 10.1017/s0033291701005062. [DOI] [PubMed] [Google Scholar]
- Maercker A, Michael T, Fehm L, Becker ES, Margraf J. Age of traumatisation as a predictor of post-traumatic stress disorder or major depression in young women. British Journal of Psychiatry. 2004;184:482–487. doi: 10.1192/bjp.184.6.482. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Latent class analysis. Sage; Newbury Park, CA: 1987. Sage university paper series on quantitative applications in the social sciences, No. 07–064. [Google Scholar]
- McCutcheon VV, Heath AC, Nelson EC, Bucholz KK, Madden PA, Martin NG. Accumulation of trauma over time and risk for depression in a twin sample. Psychological Medicine. 2009;39:431–441. doi: 10.1017/S0033291708003759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menard CB, Bandeen-Roche KJ, Chilcoat HD. Epidemiology of multiple childhood traumatic events: Child abuse, parental psychopathology, and other family-level stressors. Social Psychiatry and Psychiatric Epidemiology. 2004;39:857–865. doi: 10.1007/s00127-004-0868-8. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Angst J, Eaton W, Canino G, Rubio-Stipec M, Wacker H, Wittchen HU, Andrade L, Essau C, Whitaker A, Kraemer H, Robins LN, Kupfer DJ. Comorbidity and boundaries of affective disorders with anxiety disorders and substance misuse: Results of an international task force. British Journal of Psychiatry Supplement. 1996;30:58–67. [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: Results of the International Consortium in Psychiatric Epidemiology. Addictive Behaviors. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Lynskey MT, Bucholz KK, Madden PA, Statham DJ, Martin NG. Childhood sexual abuse and risks for licit and illicit drug-related outcomes: A twin study. Psychological Medicine. 2006;36:1473–1483. doi: 10.1017/S0033291706008397. [DOI] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, Glowinski A, McLaughlin T, Dunne MP, Statham DJ, Martin NG. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: Results from a twin study. Archives of General Psychiatry. 2002;59:139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- Neuman RJ, Todd RD, Heath AC, Reich W, Hudziak JJ, Bucholz KK, Madden PA, Begleiter H, Porjesz B, Kuperman S, Hesselbrock V, Reich T. Evaluation of ADHD typology in three contrasting samples: A latent class approach. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:25–33. doi: 10.1097/00004583-199901000-00016. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Stang P, Wittchen HU, Ustun B, Walters EE, Kessler RC. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Association with symptoms, impairment, course and help-seeking. British Journal of Psychiatry. 2000;176:229–235. doi: 10.1192/bjp.176.3.229. [DOI] [PubMed] [Google Scholar]
- SAS Institute . SAS Statistical Software: Release 9.1. SAS Institute, Inc.; Cary, NC: 2004. [Google Scholar]
- Scarr S, McCartney K. How people make their own environments: a theory of genotype greater than environment effects. Child Development. 1983;54:424–435. doi: 10.1111/j.1467-8624.1983.tb03884.x. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Heath AC, Madden PA, Bucholz KK, Dinwiddie SH, Dunne MP, Statham DJ, Martin NG. Reliability and reporting biases for perceived parental history of alcohol-related problems: Agreement between twins and differences between discordant pairs. Journal of Studies on Alcohol. 1996;57:387–395. doi: 10.15288/jsa.1996.57.387. [DOI] [PubMed] [Google Scholar]
- Spatz Widom C, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Stata Corporation . Stata Statistical Software: Release 8.0. Stata Corporation; College Station, TX: 2004. [Google Scholar]
- Teicher MH, Dumont NL, Ito Y, Vaituzis C, Giedd JN, Andersen SL. Childhood neglect is associated with reduced corpus callosum area. Biological Psychiatry. 2004;56:80–85. doi: 10.1016/j.biopsych.2004.03.016. [DOI] [PubMed] [Google Scholar]