Abstract
Purpose:
To present clinical results of toric intraocular lens (IOL) implantation for preexisting astigmatism correction and determine the time of any postoperative rotation.
Patients and methods:
Twenty-nine eyes of 19 patients underwent uncomplicated phacoemulsification and were implanted with an Acrysof © toric IOL. Uncorrected visual acuity, residual astigmatism, and postoperative rotation of the IOL were estimated one and six months after the operation.
Results:
Uncorrected visual acuity was ≥0.5 in 26 of 29 eyes (89.7%) and ≥0.8 in 19 of 29 patients (65.5%). The mean toric IOL axis rotation was 2.2 ± 1.5° (range 0.6–7.8°) one month postoperation and 2.7 ± 1.5° (range 0.9–8.4°) six months postoperation.
Conclusion:
Implantation of one-piece hydrophobic acrylic toric IOLs appears to have acceptable stability, which encourages visual outcome and emerges as an attractive alternative for correction of refractive astigmatism.
Keywords: astigmatism, cataract, stability, implantation
Introduction
According to numerous estimations, 15% to 29% of patients with cataract have ≥1.5 diopters (D) of refractive astigmatism.1,2 Cataract surgeons usually prefer to treat cataract and correct refractive (spherical and astigmatic) disorders at the time of the surgery. Corneal incision (astigmatic keratotomy) and peripheral corneal relaxing incisions (PCRIs) were performed to treat these disorders.3,4 The main drawbacks of these approaches are that the outcome depends on multiple factors as the patient’s age, the depth and length of the incision, complications related to wound healing, epithelial defects, or induction of dry-eye symptoms. These parameters affect the visual outcome in a unpredictable way so the corneal incisions are not considered a reliable method for astigmatism correction.
Toric intraocular lens (IOLs) implantation was introduced in the 1990’s as an option for astigmatism correction in cataract patients. Initially they presented the disadvantage of postoperative rotation that decreased the visual outcome.5–8
New toric IOL designs (Acrysof © toric IOL; Alcon, Fort Worth, TX), approved by the US Food and Drug Administration (FDA) at the end of 2005, have been found to be more stable and appear to be the preferred IOL for correcting preexisting astigmatism in conjunction with cataract surgery.9,10 The Acrysof © IOLs are available in three options: T3, T4, and T5 of astigmatic correction 1.5, 2.25, 3.00 D, respectively (at the IOL plane).
The aim of this study is to report the clinical results of Acrysof © toric IOLs implantation for preexisting astigmatism correction and compare the postoperative rotation of the IOLs one and six months postoperatively.
Material and methods
This prospective study included eyes that had cataract surgery at the Papageorgiou General Hospital, Thessaloniki, Greece, between May 2008 and December 2008. The study was conducted according to the tenets of the Declaration of Helsinki and patients gave informed consent after the nature and intent of the study had been fully explained to them.
Inclusion criteria were: cataract, age 70 years or younger, and preoperative regular corneal astigmatism greater than 1.00 D. Exclusion criteria were: glaucoma, corneal disease, previous corneal or intraocular surgery, macular degeneration or retinopathy, and history of ocular inflammation.
Each patient had a complete ophthalmologic examination, including visual acuity (VA), slit-lamp examination, intraocular pressure (IOP) measurement, and dilated fundus examination. Lens photographs were obtained. Topography (Magellan Mapper; Nidek Technologies, Padova, Italy), automated refractometry (RK600; Reichert, Inc., Depew, NY), and ultrasonic immersion biometry (Ocuscan Rxp; Alcon) were performed to determine the appropriate IOL spherical power. Cylindrical power and axis placement to achieve emmetropia were calculated using an online toric IOL calculator program (available from http://www.acrysoforiccalculator.com/).
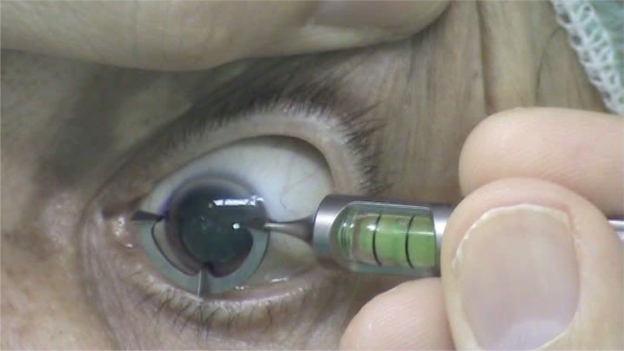
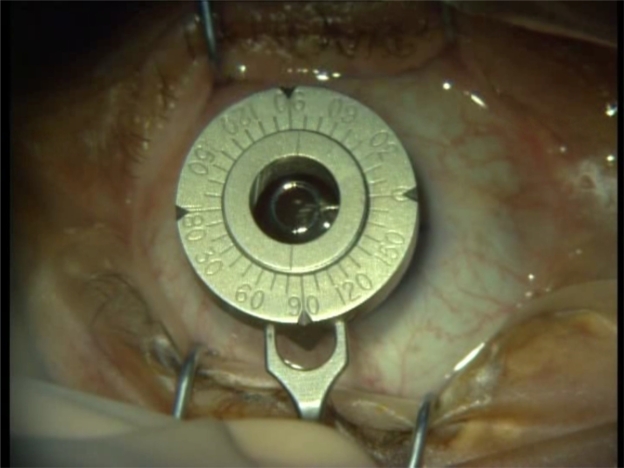
The 0–180° axis was marked with the patient in a sitting position to avoid cyclotorsion using the Nuijts/Lane preoperative toric reference corneal marker (AE-2791TBL; ASICO, Westmont, IL) (Figure 1). Intraoperatively, the desired implantation axis was marked using an Intra-Op Toric Axis Marker II (AE-2794; ASICO) (Figure 2). A foldable IOL was implanted in the capsular bag through a 2.75 mm limbal incision on 110°. The toric IOL was injected with a Monarch-II injector (Alcon) and placed around 10–15° off axis before the ophthalmic viscosurgical device (sodium hyaluronate 1%) was removed. After ophthalmic viscosurgical device removal, the IOL was rotated to its final position by exactly aligning the toric reference marks with the limbal implantation axis marks.
Figure 1.
Preoperative marking of the horizontal axis.
Figure 2.
Intraoperative marking of the implantation desired axis.
All surgeries were performed by the same experienced surgeon (IT) using topical anesthesia and a standard divide-and-conquer phacoemulsification technique.
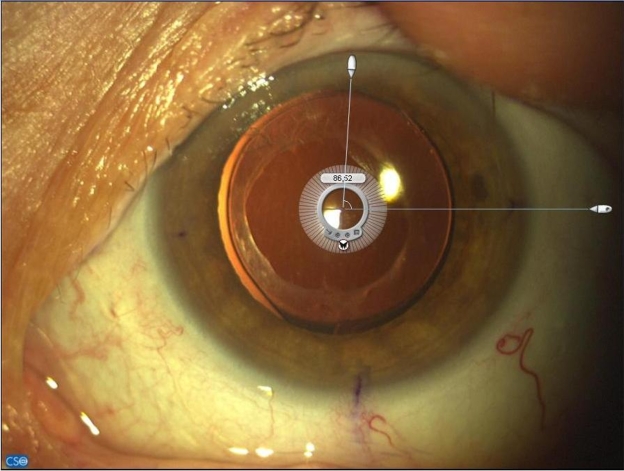
Because of the intraoperative marker design and the pen mark fading during the operation in several cases, it was difficult to assess the proper alignment of the IOL after its placement. Because of this difficulty, an image was captured from the real-time streaming recording of the surgery and was assessed blindly by a second operator using a commercially available software (Screen Protractor; Iconico, NY, USA) (Unpublished data).
To overcome this difficulty we consider that the use of the marker set consisting of Beveled Degree Gauge (AE-1590; ASICO) and Maloney Astigmatism Axis Marker (AE-2741; ASICO) is more appropriate for the whole procedure because it allows maximum visibility. The on-screen assessment of the axis remains a useful tool for postoperative evaluation of the IOL location (Figure 3).
Figure 3.
Postoperative estimation of toric intraocular lens position.
Measurements of visual acuity (using the Snellen opto-type at a six-meter distance), IOP, and comprehensive slit lamp examination were performed at one-day and one- and six-month postoperative visits. At the one- and six-month follow-up, a digital photograph and corneal topography (only at the one-month visit) were obtained to estimate the postoperative rotation of the IOL using the software tools mentioned above (Figure 1). Outcomes of interest included uncorrected VA, cylindrical astigmatism power before and after IOL implantation, and the possible rotation of the IOL one and six months after the operation (when the initial desired place was at 0°). Absolute values of the rotation used for the analysis after detecting rotation was not under investigation. All data were collected during a mean follow-up of 5.6 months.
Completed data forms were analyzed with Microsoft Excel 2007 (Microsoft Corporation, Redmond, WA) and SPSS software (version 16.0; SPSS Inc., Chicago, IL).
Results
Twenty-nine eyes of 19 patients (mean age 63.03 ± 5.42 years) were enrolled in this study. Uncorrected VA was found to be 5/10 or more in 26 of 29 eyes (89.7%) and 8/10 or more in 19 of 29 patients (65.5%).
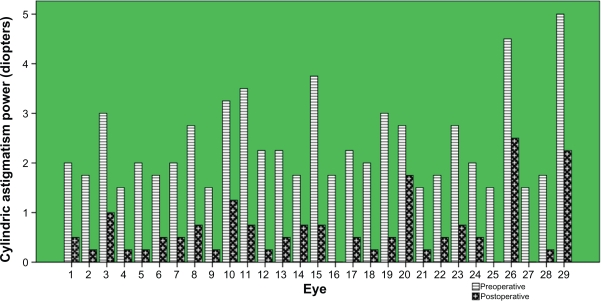
Preoperative and postoperative corneal topography showed significant reduction of refractive astigmatism in all eyes after the surgery. Mean power of the astigmatism was 2.38 ± 0.91 D (range 1.5–5 D) preoperatively and 0.64 ± 0.61 D (range 0–2.5 D) postoperatively (Figure 4).
Figure 4.
Reduction of astigmatism after the toric intraocular lens implantation.
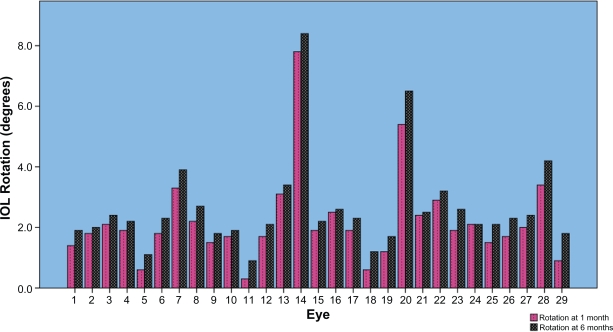
One month postoperation, the mean toric IOL axis rotation was 2.2 ± 1.5° (range 0.6–7.8°). Rotation was 5° or less in 27 of 29 eyes (93.1%). Six months postoperation, the mean toric IOL axis rotation was 2.7 ± 1.5° (range 0.9–8.4°). The later rotation occurred between one and six months, and was found to be more than one degree (1.1°) only in one eye (3%) and in all other cases was less than this value (Figure 5).
Figure 5.
Comparison of intraocular lens rotation at one and six months postoperative.
It is known that one degree of deviation causes 3.3% reduction of the IOL cylindrical power. Calculated reduction of the desired correction (in diopters) because of the observed rotation (mean value, one and two standard deviations) for the three IOL models is shown in Table 1.
Table 1.
Cylindrical power reduction for intraocular lens (IOL) models due to observed off axis postoperative rotation
| Rotation at six months: percentage of IOL cylindrical power reduction |
Reduction of IOL cylindrical power at IOL plane (corneal plane) in diopters for T3, T4, T5 models |
||
|---|---|---|---|
| T3 | T4 | T5 | |
| 2.7°, 7.26% (mean value) | 0.13 (0.09) | 0.2 (0.14) | 0.27 (0,18) |
| 4.2°, 13.86% (one standard deviation) | 0.21 (0.14) | 0.31 (0.21) | 0.41 (0.29) |
| 5.7°, 18.81% (two standard deviations) | 0.28 (0.19) | 0.42 (0.29) | 0.56 (0.39) |
No eye had secondary surgery to reposition the IOL axis within the six-month postoperative period. There was no significant IOL rotation (>10°) in any patient.
Discussion
The results of our study corroborate previous studies,11 which demonstrates that proper selection and preoperative examination of patients followed by uncomplicated IOL implantation of one-piece hydrophobic acrylic toric IOLs results in acceptable stability and visual outcome.
In particular, the postoperative rotation of toric IOLs appears to occur in the early postoperative period (≤1 month) and remains constant later than six months. The lens rotates until a fibronectin and collagen adhesion develops between the IOL and the posterior capsule, which prevents any further rotary motion.12
The amount of cylindrical correction reduction due to postoperative rotation was not large enough13 to affect the expected end result in final uncorrected distance VA.
Conclusion
Acrysof © one-piece hydrophobic acrylic toric IOLs implantation shows satisfactory stability, acceptable clinical results, and is an exceptional option for correction of refractive astigmatism.
Footnotes
Disclosures
The authors report no conflicts of interest in this work.
References
- 1.Ninn-Pedersen K, Stenevi U, Ehinger B. Cataract patients in a defined Swedish population 1986–1990. II. Preoperative observations. Acta Ophthalmol (Copenh) 1994;72:10–15. doi: 10.1111/j.1755-3768.1994.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 2.Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980;90:360–368. doi: 10.1016/s0002-9394(14)74917-7. [DOI] [PubMed] [Google Scholar]
- 3.Inoue T, Maeda N, Sasaki K, et al. Factors that influence the surgical effects of astigmatic keratotomy after cataract surgery. Ophthalmology. 2001;108:1269–1274. doi: 10.1016/s0161-6420(01)00629-7. [DOI] [PubMed] [Google Scholar]
- 4.Muller-Jenson K, Fischer P, Siepe U. Limbal relaxing incisions to correct astigmatism in clear corneal cataract surgery. J Refract Surg. 1999;15:586–589. doi: 10.3928/1081-597X-19990901-12. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen TM, Miller KM. Digital overlay technique for documenting toric intraocular lens axis orientation. J Cataract Refract Surg. 2000;26:1496–1504. doi: 10.1016/s0886-3350(00)00442-9. [DOI] [PubMed] [Google Scholar]
- 6.Sun X, Vicary D, Montgomery P, et al. Toric intraocular lenses for correcting astigmatism in 130 eyes. Ophthalmology. 2000;107:1776–1782. doi: 10.1016/s0161-6420(00)00266-9. [DOI] [PubMed] [Google Scholar]
- 7.Chang DL. Early rotational stability of the longer Staar toric intraocular lens: fifty consecutive cases. J Cataract Refract Surg. 2003;29:935–940. doi: 10.1016/s0886-3350(02)01843-6. [DOI] [PubMed] [Google Scholar]
- 8.Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000;11:47–50. doi: 10.1097/00055735-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Mendicute J, Irigoyen C, Aramberri J, Ondarra A, Montés-Micó R. Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg. 2008;34:601–607. doi: 10.1016/j.jcrs.2007.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Mendicute J, Irigoyen C, Ruiz M, Illarramendi I, Ferrer-Blasco T, Montés-Micó R. Toric intraocular lens versus opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg. 2009;35:451–458. doi: 10.1016/j.jcrs.2008.11.043. [DOI] [PubMed] [Google Scholar]
- 11.Zuberbuhler B, Signer T, Gale R, Haefliger E. Rotational stability of the Acrysof SA60TT toric intraocular lenses: A cohort study. BMC Ophthalmology. 2008;8:8. doi: 10.1186/1471-2415-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linnola RJ, Sund M, Ylönen R, Pihlajaniemi T. Adhesion of soluble fibronectin, laminin, and collagen type IV to intraocular lens materials. J Cataract Refract Surg. 1999;25:1486–1491. doi: 10.1016/s0886-3350(99)00238-2. [DOI] [PubMed] [Google Scholar]
- 13.Remón L, Tornel M, Furlan WD. Visual acuity in simple myopic astigmatism: influence of cylinder axis. Optom Vis Sci. 2006;83:311–315. doi: 10.1097/01.opx.0000216099.29968.36. [DOI] [PubMed] [Google Scholar]