Abstract
Abdominal wall pathology is a frequently overlooked cause of acute abdomen. Increasing use of antiplatelet and anticoagulant therapies has led to an increase in the incidence of spontaneous rectus sheath hematoma (RSH). A high index of suspicion is needed for diagnosis as it can closely mimic other causes of acute abdomen. Herein, we report a case of RSH presenting with abdominal pain in which there was a significant delay in diagnosis. We wish to highlight the need to increase awareness among primary and emergency physicians about considering RSH in the initial differential diagnoses of abdominal pain.
INTRODUCTION
Rectus sheath hematoma (RSH) is a known complication of abdominal trauma, surgery and excessive strain on the abdominal musculature. The increasing use of antiplatelet and anticoagulant therapies has led to an increase in RSH in patients without obvious precipitating events.1, 2 We report one such case of spontaneous RSH presenting with abdominal pain to an urgent care clinic. Abdominal wall pathology is a frequently overlooked cause of acute abdomen leading to delays in diagnosis.3 We emphasize the need to consider this increasingly common entity in the initial differential diagnoses of patients presenting with abdominal pain.
CASE
A 78-year-old Caucasian male with hypertension, coronary artery disease, history of mitral valve replacement for severe mitral regurgitation and congestive heart failure presented to the urgent care clinic with abdominal pain of one-day duration. He reported poor appetite but denied fever, nausea, vomiting, change in bowel habit, cough or abdominal trauma. He was on lisinopril, carvedilol, warfarin, low dose aspirin and furosemide. Examination revealed no obvious abdominal swelling, masses or ecchymosis. Mild tenderness and guarding were noted in the left lower quadrant. Bowel sounds were normal. Testing revealed a normal metabolic panel, serum amylase, serum lipase, urine analysis and abdominal X-ray. He had mild leukocytosis with normal differential count and an INR of 1.9. Stool occult blood test was negative. Patient was provisionally diagnosed to have diverticulitis and treated with intravenous fluid, antibiotics and one dose of morphine (2 mg). Significant improvement in symptoms was noted within a few hours. Abdominal computed tomography (CT) scan was deferred in view of his mild symptoms and clinical improvement. He was recommended a high fiber diet, oral antibiotics and outpatient follow up. However, he complained of recurrent pain and acute onset dyspnea immediately prior to discharge. At this time, his blood pressure dropped to 70/40 mm of Hg and a repeat hemogram revealed a fall in hemoglobin from 10 to 8.4 g/dl. Abdominal examination revealed increased tenderness in the left lower quadrant and mild tenderness in the infraumbilical area. At this juncture, the lack of overt gastrointestinal or external blood loss raised the suspicion of RSH vs. retroperitoneal or intraperitoneal bleeding. Patient was promptly resuscitated with crystalloid and packed red blood cells (RBC). Emergent abdominal ultrasound revealed a large complex fluid collection in the lower abdominal wall with extension into the pelvis (Figure 1). Noncontrast abdominal CT scan confirmed the pelvic fluid collection and also demonstrated a thickened rectus sheath. These findings were consistent with RSH (Figures 2 and 3). Patient was admitted to the intensive care unit and anticoagulation was reversed with 1 mg of vitamin K orally and two units of fresh frozen plasma. Over the next six hours, patient’s symptoms improved rapidly and repeat INR was 1.1. Angiographic embolization was planned as a back up; however, patient’s symptoms and blood pressure improved with conservative therapy alone. Warfarin was restarted on day 3 of hospitalization along with intravenous unfractionated heparin for bridging therapy. There were no further complications and heparin was discontinued after a stable therapeutic INR (2.6) was achieved.
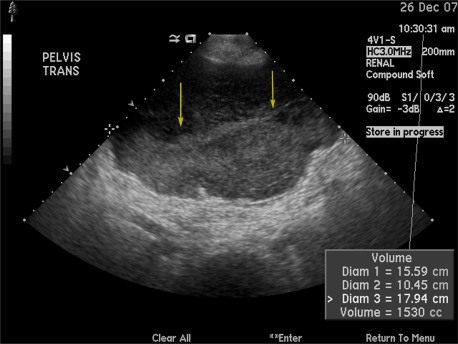
Figure 1.
Pelvic ultrasound showing a complex fluid collection in the pelvis. Arrows denote the complex pelvic fluid collection.
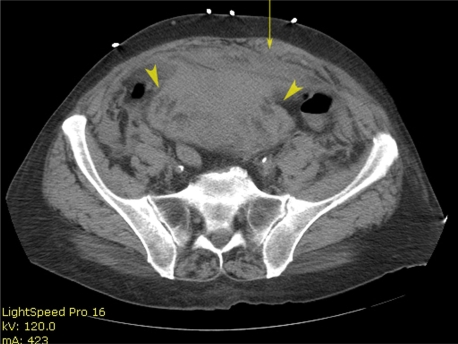
Figure 2.
Noncontrast CT scan image of lower abdomen. Arrow points to thickened left rectus muscle and sheath. Arrowheads point to the complex heterogeneous collection posterior to the anterior abdominal wall.
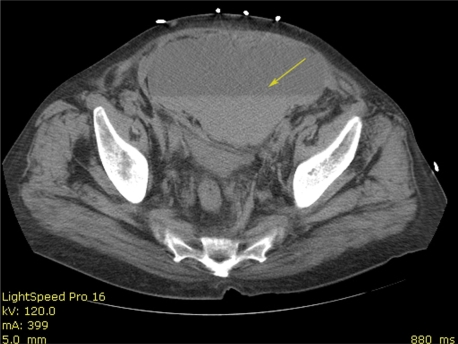
Figure 3:
Noncontrast CT scan image of pelvis. Arrows denote complex fluid collection with layering consistent with hematoma.
DISCUSSION
RSH denotes a collection of blood in the rectus sheath secondary to disruption of blood vessels coursing through it or injury to the muscle itself. Blunt or penetrating trauma, surgical trauma, pregnancy, collagen vascular disorders, degenerative muscle diseases, blood dyscrasias and strenuous exercise are known predisposing factors. RSH occurring in patients without antecedent history of trauma is referred to as spontaneous RSH. It is more frequent in females and the elderly.1,2 Unnoticed trauma, such as straining during defecation or cough, is one of the proposed etiologies for spontaneous RSH. The precise incidence and temporal trends of RSH are not known; however, we believe that the increased use of anticoagulant and antiplatelet therapies is a potential reason for the increased reporting of spontaneous RSH. The high frequency of anticoagulant use and absence of overt trauma in a recently reported series of RSH lend support to this premise.1
RSH above the arcuate line is generally caused by damage to the superior epigastric artery. Patients present with a unilateral, small and spindle-shaped mass. It is usually self-limited because the hematoma is tamponaded between the rectus sheath and the tendinous inscriptions of the rectus muscles. Hematomas below the arcuate line are caused by damage to the inferior epigastric artery. They bleed more profusely, dissect the tissue planes extensively and often extend across the midline. This is due to the absence of a tendinous posterior sheath wall in this area. Here, the rectus abdominis muscle is supported only by the transversalis fascia and the parietal peritoneum. Extension into pelvic cavity may not be noticed leading to frequent underestimation of the blood loss.
Abdominal pain and fall in hemoglobin with presence of risk factors (especially anticoagulation) constitute important clinical clues to the diagnosis. Common presenting symptoms are listed in Table 1. Physical examination reveals tenderness and swelling in the parietal wall. Generally, the abdominal mass in RSH does not cross the midline and, in contrast to an intraperitoneal mass, it remains conspicuous on tensing the abdominal wall musculature by head or leg raising. This is referred to as Fothergill’s sign.4 Similarly, tenderness remains the same or increases with head raising and is referred to as Carnett’s sign.4,5 Ecchymoses can be noted in the flanks or periumbilical areas, especially late in the course, and are referred to as Gray Turner’s and Cullen’s sign, respectively. Ultrasonography is a useful initial test due to its wide availability and portability.6, 7 However, noncontrast CT scan is more sensitive and specific, and is the diagnostic modality of choice.7 RSH can be classified into three subtypes based on CT appearance.4, 8 Management strategy depends on the clinical condition and CT severity grade (Table 2).1, 4
Table 1.
Clinical features of rectus sheath hematoma, modified and reprinted with permission from Cherry WB et al.1 © Wolters Kluwer Health.
|
Common |
| Abdominal pain |
| Abdominal swelling/mass |
| Fall in hemoglobin |
|
Less common |
| Nausea/vomiting |
| Tachycardia |
| Orthostatic symptoms |
| Hypotension |
| Ecchymosis |
| Syncope |
| Peritoneal signs |
| Fever |
Table 2.
Computed Tomography severity grades and suggested management strategy, modified and reprinted with permission from Osinbowale O et al.4 © Sage publications.
| Grade | Anatomic extension | Symptoms | Management |
|---|---|---|---|
| I | Intramuscular, unilateral, does not dissect along fascial planes. | Mild to moderate pain. No drop in hemoglobin. | Conservative; usually outpatient follow up only. |
| II | Bilateral, some dissection between the muscle and transversalis fascia; no extension into the prevesical space. | Minor drop in hemoglobin. | Observation, short hospital stay. May need transfusion. |
| III | Bilateral, large, dissects between the transversalis fascia and muscle into the peritoneum and prevesical space. | Significant drop in hemoglobin and hemodynamic instability. | Reversal of anticoagulants and blood transfusion. Angiographic interventions may be needed. |
Timely reversal of coagulopathy is the most important aspect of management. Otherwise, management is usually conservative as the natural course of this problem is self-limiting. RBC transfusion is recommended in the presence of hemodynamic compromise or significant fall in hemoglobin. Invasive procedures or surgery are rarely needed for securing hemostasis and stabilizing hemodynamics. Surgical management is associated with significant morbidity due to the advanced age and multiple co-morbidities in these patients. Hence, it is reserved for the most severe cases. Coil or gel foam embolization (of the epigastric arteries) has been successfully used in patients with refractory bleeding despite reversal of coagulopathy.9 When diagnosed promptly, prognosis is usually good and resolution without sequelae is the rule. Spontaneous complete resolution, especially in large hematomas, may take up to several months. Therapeutic pulsed ultrasound may be used for hastening the resolution.10 Need for anticoagulation should be weighed against the risk of re-bleeding once the patient is stabilized.
Medical training adequately emphasizes the recognition of common surgical and non-surgical intra-abdominal emergencies, such as appendicitis and pancreatitis. However, there is a relative lack of emphasis and hence of awareness about abdominal wall problems presenting as acute abdomen. Moreover, RSH is a great masquerader and can mimic most other abdominal emergencies, such as acute appendicitis, diverticulitis, pancreatitis, or ruptured aortic aneurysm. These factors often lead to delays in the recognition of RSH, translating frequently into increased morbidity and occasionally into increased mortality.
CONCLUSION
The incidence of spontaneous RSH is increasing as more and more elderly patients are being treated with antiplatelet and anticoagulant therapies. RSH can frequently mimic other common abdominal emergencies leading to delayed diagnosis. Physicians should consider RSH in the initial differential diagnosis of abdominal pain even in the absence of abdominal trauma or strain. Timely diagnosis can prevent unnecessary diagnostic tests and also decrease the morbidity and mortality.
Footnotes
Supervising Section Editor: Christopher A. Kahn MD
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Cherry WB, Mueller PS. Rectus sheath hematoma. Review of 126 cases at a single institution. Medicine. 2006;85:105–110. doi: 10.1097/01.md.0000216818.13067.5a. [DOI] [PubMed] [Google Scholar]
- 2.Linhares MM, Lopes Filho GJ, Bruna PC, et al. Spontaneous hematoma of the rectus abdominis sheath: a review of 177 cases with report of 7 personal cases. Int Surg. 1999;84:251–257. [PubMed] [Google Scholar]
- 3.Hershfield NB. The abdominal wall. A frequently overlooked source of abdominal pain. J Clin Gastroenterol. 1992;14:199–202. [PubMed] [Google Scholar]
- 4.Osinbowale O, Bartholomew JR. Rectus sheath hematoma. Vasc Med. 2008;13:275–279. doi: 10.1177/1358863X08094767. [DOI] [PubMed] [Google Scholar]
- 5.Thomson H, Francis DM. Abdominal-wall tenderness: A useful sign in the acute abdomen. Lancet. 1977;2:1053–1054. doi: 10.1016/s0140-6736(77)91885-2. [DOI] [PubMed] [Google Scholar]
- 6.Klingler PJ, Wetscher G, Glaser K, et al. Use of ultrasound to differentiate rectus sheath hematoma from other acute abdominal disorders. Surg Endosc. 1999;13:1129–1134. doi: 10.1007/s004649901188. [DOI] [PubMed] [Google Scholar]
- 7.Moreno Gallego A, Aguayo JL, Flores B, et al. Ultrasonography and computed tomography reduce unnecessary surgery in abdominal rectus sheath hematoma. Br J Surg. 1997;84:1295–1297. [PubMed] [Google Scholar]
- 8.Berná JD, Garcia-Medina V, Guirao J, et al. Rectus sheath hematoma: diagnostic classification by CT. Abdom Imaging. 1996;21:62–4. doi: 10.1007/s002619900011. [DOI] [PubMed] [Google Scholar]
- 9.Rimola J, Perendreu J, Falcó J, et al. Percutaneous arterial embolization in the management of rectus sheath hematoma. AJR Am J Roentgenol. 2007 Jun;188(6):W497–502. doi: 10.2214/AJR.06.0861. [DOI] [PubMed] [Google Scholar]
- 10.Berná-Serna JD, Sánchez-Garre J, Madrigal M, et al. Ultrasound therapy in rectus sheath hematoma. Phys Ther. 2005;85:352–357. [PubMed] [Google Scholar]