Abstract
Purpose
The objective of this study is to evaluate the therapeutic efficacy of ethylenediaminetetraacetic acid (EDTA) chelation and excimer laser phototherapeutic keratectomy (PTK) combined with amniotic membrane transplantation (AMT) for the treatment of band keratopathy (BK).
Methods
Eleven eyes in ten patients with BK received combined PTK (ablation zone of central 7.0-7.5 mm, depth of 50 µm), EDTA chelation (0.05 M, 3 minutes), and amniotic membrane transplantation using fibrin glue. Preand postoperative best corrected visual acuities, symptom changes, reepithelialization time, cosmesis, recurrence, and complications were analyzed.
Results
Visual acuity improved in three eyes (27.3%) and did not change in eight eyes (72.7%). Symptoms improved in all patients, and the mean reepithelialization time was 10.6±5.3 days. The cosmetic results were good in eight eyes (72.7%) and were fair in three eyes (27.3%). During the mean follow-up period of 11.4±6.1 months (range, 6 to 23 months), no postoperative complications or recurrences were observed.
Conclusions
The combination of EDTA chelation, PTK, and AMT is safe and effective for the treatment of band keratopathy.
Keywords: Amion, Chelating agents, Excimer lasers
Band keratopathy (BK) is a chronic corneal degeneration characterized by the deposition of calcific materials throughout the epithelium, basement membrane, Bowman's layer, and superficial stroma. It may be associated with systemic conditions such as sarcoidosis or chronic renal failure or with chronic ocular inflammations such as chronic uveitis or long-standing interstitial keratitis [1,2].
The most widely used treatments for BK are ethylenediaminetetraacetic acid (EDTA) chelation and superficial keratectomy, which remove calcium deposits, restore the corneal surface, and improve ocular comfort [3-5]. However, complete removal of deeply impacted calcium plaques in the anterior stroma is difficult with these conventional methods [6]. In addition, these procedures have several problems, including severe pain, low visual acuity, long rehabilitation time, and recurrence after surgery [4-6]. Phototherapeutic keratectomy (PTK) can be used to treat many corneal diseases, including BK [7-10]. PTK is effective in treating pathologies at the deeper levels of Bowman's layer and superficial stroma, which are not amenable to EDTA chelation or superficial keratectomy. However, PTK also has shortcomings, such as postoperative pain and iatrogenic change in refractive error [6-8].
The amniotic membrane (AM), which consists of a basement membrane and stroma, contains many materials that facilitate corneal and conjunctival rehabilitation [11,12]. Amniotic membrane transplantation (AMT) has been widely used for ocular surface reconstruction as it facilitates epithelialization while suppressing ocular surface inflammation, neovascularization, and scarring of the stroma [13-17]. In addition, the amniotic membrane provides a mechanical bandage that protects corneal wounds, absorbs inflammatory cytokines, and reduces pain during corneal wound healing [13-15]. This information has been used to develop treatments for BK using a combination of surgical keratectomy with or without EDTA chelation followed by AMT [18,19].
In the present study, we retrospectively investigated the therapeutic efficacy of EDTA chelation and excimer laser PTK combined with AMT for the treatment of BK found beneath the Bowman's layer and in the anterior stroma.
Materials and Methods
Patients
We retrospectively reviewed the medical records of 11 eyes of ten patients with BK involving the anterior stroma who underwent EDTA chelation and excimer laser PTK combined with AMT at Chonnam National University Hospital between January 2003 and June 2007. The minimum follow-up period for inclusion was six months. Preoperative data including age, gender, cause, associated conditions, best corrected visual acuity, symptoms, and signs were collected. All of the recruited patients were treated by a single surgeon (KCY). Informed consent for the procedures was obtained from each patient. Institutional review board/ethics committee approval was obtained from the Chonnam National University Medical School Institutional Review Board, and the study protocol followed the guidelines of the Declaration of Helsinki.
Ethylenediaminetetraacetic acid chelation
After instillation of topical proparacaine (Alcaine; Alcon, Fort Worth, TX, USA), the corneal epithelium overlying calcium plaques was removed with a spatula or cotton-tipped applicator. A cellulose sponge soaked in EDTA (0.05 M) was applied on the band for 3 to 5 minutes, depending on the density of the calcium. After the EDTA had adequately infiltrated into the lesion, the calcium deposits were rubbed off.
Excimer laser phototherapeutic keratectomy
Excimer laser PTK was performed to remove remaining calcium plaques in the anterior stroma after EDTA chelation using a Technolas 217z Zyopticx™ (Bausch & Lomb, Feldkirchen, Germany) excimer laser system with an average energy density of 120 mJ/cm2 and a pulse repetition rate of 50 Hz. The central ablation zone was 7.0-7.5 mm in diameter and 40-50 µm in depth, depending on the extent of the lesion. After central ablation, the peripheral cornea was ablated with a diameter of 2.0 mm for removal of the remaining calcium deposits.
Preparation and preservation of the human amniotic membrane
Preparation and preservation of the AM were performed as previously described [12-14,18,19]. The human placenta was obtained, with consent, after an elective cesarean section from donors that were seronegative for infectious diseases, such as human immunodeficiency virus, hepatitis B and C virus, and syphilis. The amnion was separated from the rest of the chorion by blunt dissection and was cleaned of the remaining blood clots with a sterile balanced salt solution (Alcon, Fort Worth) containing 50 ng/mL penicillin, 50 mg/mL streptomycin, 100 ng/mL neomycin, and 2.5 mg/mL amphotericin B. After cleansing, the amnion was flattened onto 0.45 µm nitrocellulose filter paper with the epithelium and basement membrane surface up and was stored at -80℃ in a medium containing Dulbecco's modified Eagle medium (GIBCO BRL, Grand Island, NY, USA) and glycerol (Baxter Healthcare Corporation, Deerfield, IL, USA) until use.
Amniotic membrane transplantation
EDTA chelation and excimer laser PTK were followed by AMT. Under local anesthesia, the preserved AM was cut to approximately 8.0 mm in diameter using a trephine blade and was placed over the epithelial defect as a graft, with the stromal side facing down. The AM was fixed onto the corneal surface using fibrin glue (Greenplast®; Green Cross, Seoul, Korea). Postoperatively, all patients were treated with topical ofloxacin (Ocuflox®; Samil, Seoul, Korea) and fluorometholone (Ocumetholone®, Samil) eyedrops four times a day and hyaluronic acid (Hyalein®; Santen, Osaka, Japan) frequently until epithelialization was complete and the ocular surface was stable.
Postoperative management and evaluation of results
Follow-up examinations were performed daily for two weeks postoperative, and thereafter at 1-2 week intervals. We analyzed visual acuity, symptom improvement, healing time for epithelial defects, cosmetic results, recurrence, and complications at the last follow-up visit. The cosmetic results were divided into three grades: good (clear cornea), fair (mild haze, but acceptable cosmesis), and poor (moderate to severe haze). Wilcoxon's rank sum test was used to assess changes in visual acuity pre- and postoperatively.
Results
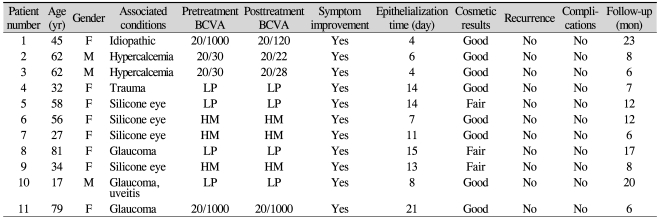
Patient characteristics are presented in Table 1. Of the ten patients (11 eyes) with BK, two were men and eight were women. The mean age was 50.3±21.0 years (range, 17 to 81 years), and the mean duration of follow-up was 11.4±6.1 months (range, 6 to 23 months). The causes of BK were prior retinal surgery using silicone oil in four eyes (36.4%), glaucoma in three eyes (27.3%), hypercalcemia in two eyes (18.2%), trauma in one eye (9.1%), and idiopathic in one eye (9.1%). Preoperatively, all patients had visual disturbances, foreign body sensation, and tearing, and one patient had photophobia.
Table 1.
Characteristics of patients with band keratopathy and treatment results after ethylenediaminetetraacetic acid chelation and phototherapeutic keratectomy combined with amniotic membrane transplantation
BCVA=best corrected visual acuity; LP=light perception; HM=hand movement.
Postoperatively, the best corrected visual acuity remained unchanged in eight eyes (72.7%) and improved in three eyes (27.3%). There was no significant difference between the preoperative and postoperative best corrected visual acuities (p=0.11). Symptoms were noticeably improved in all patients. The mean time for complete healing of the cornea was 10.6±5.3 days after surgery: 8 to 14 days in five eyes (45.5%), seven days or less in four eyes (36.4%), and 15 days or more in two eyes (18.2%). The cosmetic results were good in eight eyes (72.7%) and fair in three eyes (27.3%).
Calcium plaques were removed completely in all cases. Although we performed sutureless AM transplantations using fibrin glue, there were no early detachments of the AM. There were no recurrences or complications associated with the surgery during the follow-up period. At the last visit, a good corneal state was established in all patients (Fig. 1). However, in one patient with glaucoma (patient 8), evisceration was required because of uncontrolled intraocular pressure at postoperative month 17.
Fig. 1.
Pre- and postoperative slit lamp photographs of a patient with band keratopathy who underwent combined ethylene diamine tetraacetic acid chelation, phototherapeutic keratectomy, and permanent amniotic membrane transplantation. (A) Preoperatively, extensive calcium deposition with an irregular surface was detected in the central cornea. (B) Two weeks after surgery, the amniotic membrane was well attached to the cornea. (C) Six months after surgery, the corneal surface was smooth and stable with mild stromal opacity and neovascularization at the inferior cornea.
Discussion
The goals of surgical treatment for BK are to provide a regular surface and a clear cornea, as well as to improve ocular comfort by removal of calcific deposits and correction of surface instability. Various methods have been used in the treatment of BK, including EDTA chelation, diamond burr, superficial keratectomy, Nd:YAG laser, and PTK [3-5,7,8,20-22].
Calcium removal by EDTA chelation is by far the most widely used method [3-5,7,8,20-22]. Najjar et al. [3] reported partial or complete symptomatic relief and improvement by two or more lines of visual acuity after EDTA chelation in 90% and 33% of patients, respectively. Because treatment using EDTA mainly focuses on the removal of calcium plaques in the epithelial layer, the removal of deeply impacted calcium deposits in the stromal layer is difficult to achieve using this method [4,7,18,19,21]. When the calcium plaques are thick or deeply positioned, the procedure is performed mainly to improve ocular comfort, not to improve vision; in this case, the recurrence rate is higher than that for other treatment procedures [3-5,19]. Moreover, calcium plaques resistant to EDTA may remain after treatment, causing an irregular corneal surface [7]. Therefore, EDTA chelation has the limitation of requiring additional procedures, such as PTK [5,19].
PTK has been used effectively for various superficial corneal disorders, such as recurrent corneal erosion, corneal opacity, and bullous keratopathy [9,10]. The indiscriminate ablative action of PTK that removes the corneal surface involving the superficial stroma is useful for treatment of BK with deeply situated calcium plaques and for restoring a regular surface [7,8]. O'Brart et al. [7] reported improvement of symptoms in 95% of patients and of visual acuity in 88% of patients with smooth-band keratopathy after PTK. Stewart and Morrell [8] also reported that symptoms were relieved in 83% of the nonvisual group and visual acuity improved or remained unchanged in 55% of the visual group after excimer laser PTK. However, several complications with PTK have been reported, including severe pain from the healing of the epithelium and variable refractive changes [7,8].
AMT has recently been performed to complement conventional treatments for BK [18,19]. Many previous studies have reported on the beneficial properties of AM that facilitate corneal epithelialization and suppress ocular surface inflammation and opacity, both in vivo and in vitro [11,17]. AM can protect stromal defects by replacing the removed basement membrane and stroma after superficial keratectomy or excimer laser PTK, resulting in a decrease in surgically-induced pain, corneal haze, neovascularization, and apoptosis [16,19]. Anderson et al. [18] performed AMT after surgical removal of calcific deposits with or without the use of EDTA in 16 eyes of 15 patients with BK. Symptoms resolved in all cases, and epithelialization was achieved in 93.7% of cases with a mean healing time of 15.2 days. Visual acuity improved in 44% and remained unchanged in 56%. Kwon et al. [19] treated two patients with AMT following EDTA chelation and superficial lamellar keratectomy. They reported that complete re-epithelialization was achieved in 9-10 days without any symptoms, complications, or recurrence.
Our strategy for the treatment of BK consists of the combination of three techniques: EDTA chelation and excimer laser PTK followed by AMT. In the present study, complete healing of corneal defects was achieved in all patients with a mean time of 10.6±5.3 days after surgery. This healing time is satisfactory considering that the corneal defects after PTK were deep to the anterior stroma in our patients. Symptoms such as pain, foreign body sensation, tearing, and photophobia noticeably improved in all cases without complications or recurrences during the follow-up period. Best corrected visual acuity improved in the 27.3% of patients that had systemic diseases or an idiopathic cause, whereas it remained unchanged in the 72.7% that had associated ocular diseases. Consistent with previous reports, this finding suggests that postoperative visual acuity may not improve with BK caused by concurrent ocular pathology, despite treatment [8,18,21]. Spherical equivalents could not be measured preoperatively because of thick calcium depositions at the anterior stroma, and so no data about refractive changes after PTK were available. The cosmetic results were generally satisfactory.
We performed a sutureless AM surgery using fibrin glue. This procedure has several advantages, including low-grade irritation and scar formation, a low frequency of graft loss by atrophic changes, and a shorter operation time compared to that of the suture techniques [23,24]. In addition, the technique does not require suture removal after surgery. Our combined approach for the treatment of BK has drawbacks of a longer operation time and greater expense. However, the combined procedure can prevent additional costs and time spent on reoperation due to recurrent lesions. That we saw no recurrence in our study may be explained by two factors: first, compared with previous reports [3], the mean follow-up period in this study was shorter. Second, in contrast to single procedures [3,7], the combined procedure may inhibit lesion recurrence [19]. In the future, a long term follow-up study with a large sample size will be needed.
In conclusion, because of the limitations of conventional techniques, we suggest that a combined treatment of EDTA chelation and PTK followed by AMT using fibrin glue for deeply situated calcium deposits in band keratopathy can induce symptom relief, reduce healing time, and prevent recurrence. Therefore, the combined procedure can be a safe and reliable approach to manage band keratopathy. Further studies with a prospective randomized design and a larger sample size with a control group are needed.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Chang RI, Ching SS. Corneal and conjunctival degenerations. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. 2nd ed. St. Louis: Mosby; 2005. pp. 996–997. [Google Scholar]
- 2.Barouch FC, Colby K. Corneal and conjunctival degenerations. In: Foster CS, Azar DT, Dohlman CH, editors. Smolin and Thoft's the cornea: scientific foundations and clinical practice. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 875–877. [Google Scholar]
- 3.Najjar DM, Cohen EJ, Rapuano CJ, Laibson PR. EDTA chelation for calcific band keratopathy: results and long-term follow-up. Am J Ophthalmol. 2004;137:1056–1064. doi: 10.1016/j.ajo.2004.01.036. [DOI] [PubMed] [Google Scholar]
- 4.Bokosky JE, Meyer RF, Sugar A. Surgical treatment of calcific band keratopathy. Ophthalmic Surg. 1985;16:645–647. [PubMed] [Google Scholar]
- 5.Wood TO, Walker GG. Treatment of band keratopathy. Am J Ophthalmol. 1975;80:550. [PubMed] [Google Scholar]
- 6.Hersh PS, Klein SR, Wagoner MD. Phototherapeutic keratectomy. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. 2nd ed. St. Louis: Mosby; 2005. pp. 1735–1748. [Google Scholar]
- 7.O'Brart DP, Gartry DS, Lohmann CP, et al. Treatment of band keratopathy by excimer laser phototherapeutic keratectomy: surgical techniques and long term follow up. Br J Ophthalmol. 1993;77:702–708. doi: 10.1136/bjo.77.11.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart OG, Morrell AJ. Management of band keratopathy with excimer phototherapeutic keratectomy: visual, refractive, and symptomatic outcome. Eye. 2003;17:233–237. doi: 10.1038/sj.eye.6700327. [DOI] [PubMed] [Google Scholar]
- 9.Gartry D, Kerr Muir M, Marshall J. Excimer laser treatment of corneal surface pathology: a laboratory and clinical study. Br J Ophthalmol. 1991;75:258–269. doi: 10.1136/bjo.75.5.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moniz N, Fernandez ST. Efficacy of phototherapeutic keratectomy in various superficial corneal pathologies. J Refract Surg. 2003;19:S243–S246. doi: 10.3928/1081-597X-20030302-15. [DOI] [PubMed] [Google Scholar]
- 11.Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995;14:473–484. [PubMed] [Google Scholar]
- 12.Tseng SC, Prabhasawat P, Lee SH. Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol. 1997;124:765–774. doi: 10.1016/s0002-9394(14)71693-9. [DOI] [PubMed] [Google Scholar]
- 13.Azuara-Blanco A, Pillai CT, Dua HS. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophthalmol. 1999;83:399–402. doi: 10.1136/bjo.83.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dua HS, Azuara-Blanco A. Amniotic membrane transplantation. Br J Ophthalmol. 1999;83:748–752. doi: 10.1136/bjo.83.6.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hori J, Wang M, Kamiya K, et al. Immunological characteristics of amniotic epithelium. Cornea. 2006;25:S53–S58. doi: 10.1097/01.ico.0000247214.31757.5c. [DOI] [PubMed] [Google Scholar]
- 16.Choi YS, Kim JY, Wee WR, Lee JH. Effect of the application of human amniotic membrane on rabbit corneal wound healing after excimer laser photorefractive keratectomy. Cornea. 1998;17:389–395. doi: 10.1097/00003226-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Wang MX, Gray TB, Park WC, et al. Reduction in corneal haze and apoptosis by amniotic membrane matrix in excimer laser photoablation in rabbits. J Cataract Refract Surg. 2001;27:310–319. doi: 10.1016/s0886-3350(00)00467-3. [DOI] [PubMed] [Google Scholar]
- 18.Anderson DF, Prabhasawat P, Alfonso E, Tseng SC. Amniotic membrane transplantation after the primary surgical management of band keratopathy. Cornea. 2001;20:354–361. doi: 10.1097/00003226-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Kwon YS, Song YS, Kim JC. New treatment for band keratopathy: Superficial lamellar keratectomy, EDTA chelation and amniotic membrane transplantation. J Korean Med Sci. 2004;19:611–615. doi: 10.3346/jkms.2004.19.4.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baltatzis S, Papaefthimiou J. Treatment of calcific band keratopathy by Nd:YAG laser. Eur J Ophthalmol. 1992;2:27–29. doi: 10.1177/112067219200200106. [DOI] [PubMed] [Google Scholar]
- 21.Maloney RK, Thompson V, Ghiselli G, et al. A prospective multicenter trial of excimer laser phototherapeutic keratectomy for corneal vision loss. Am J Ophthalmol. 1996;122:149–160. doi: 10.1016/s0002-9394(14)72006-9. [DOI] [PubMed] [Google Scholar]
- 22.Dogru M, Katakami C, Miyashita M, et al. Ocular surface changes after excimer laser phototherapeutic keratectomy. Ophthalmology. 2000;107:1144–1152. doi: 10.1016/s0161-6420(00)00113-5. [DOI] [PubMed] [Google Scholar]
- 23.Hick S, Demers PE, Brunette I, et al. Amniotic membrane transplantation and fibrin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea. 2005;24:369–377. doi: 10.1097/01.ico.0000151547.08113.d1. [DOI] [PubMed] [Google Scholar]
- 24.Szurman P, Warga M, Grisanti S, et al. Sutureless amniotic membrane fixation using fibrin glue for ocular surface reconstruction in a rabbit model. Cornea. 2006;25:460–466. doi: 10.1097/01.ico.0000183493.00884.8f. [DOI] [PubMed] [Google Scholar]