Abstract
Small bowel injury resulting from unforeseen penetration of the anterior annulus fibrosus and longitudinal ligament is a rare complication of lumbar microdiscectomy. The patient complained of abdominal tenderness and distention immediately after microdiscectomy for L4-5 and L5-S1 disc herniation. Using abdominal computed tomography, we found several foci of air overlying the anterior aspect of the vertebral body at the L5-S1 level. Segmental resection of the small bowel including small tears and primary anastomosis of the jejunum were performed. Here, we present a case of intestinal perforation after lumbar microdiscectomy and discuss technical methods to prevent this complication with a review of literature.
Keywords: Bowel injury, Complication, Lumbosacral region, Microdiscectomy
INTRODUCTION
Since Mixter and Barr's original article describing the procedure for disc excision in Mixter and Barr10) laminectomy with removal of the lumbar disc still remains the standard for treatment of disabling nerve root impingement commonly caused by degenerative disc disease. While the incidence and description of common complications related to this procedure are well known, isolated intestinal injury after lumbar discectomy is a rare but distressing complication. There have been reports of 18 cases of bowel injury as a complication of lumbar discectomy6-8,12,15-17). This paper documents an additional case with relevant imaging findings and presents the diagnostic, etiological and preventive aspects of this complication.
CASE REPORT
A 47-year-old man presented with a 5-months history of left buttock pain that radiated down the lateral aspect of the left leg to the ankle and bottom of the foot. The past medical history was unremarkable; there was no prior history of any operation. Neurological examination revealed moderate weakness of the plantar flexors of the great toe. There was also a decreased ankle jerk, and a positive straight-legraising test on the left. But, there was no sensory deficit. Magnetic resonance (MR) imaging demonstrated a left posterolateral disc herniation at L5-S1, and central disc protrusion at L4-5, with degenerative disc changes without anterior annulus thinning and perforation. The routine laboratory tests were within normal limits. Conservative therapy, including limited activity and analgesics, were unsuccessful in relieving patient's symptoms.
Under general anesthesia, hemipartial laminectomy and medial facetectomy at the L5-S1 level were performed with a high-speed drill and Kerrison rongeurs. Using an operative microscope, the ligament flavum was incised and reflected downward. The S1 nerve root was swollen and infero-posterioly displaced by a bean sized protruded disc compressing the shoulder portion of the S1 nerve root. During removal of the nucleus pulposus a straight pituitary rongeur was passed to more deeply than ordinary cases. A Small amount of fat-contained soft tissue was grasped with the instrument despite immediate withdrawal. Although any unusual operative field was not observed, there was only partial retrieval of the saline used to irrigate the wound at the end of the operation. An additional procedure was performed at L4-5 level without any other instance.
Six hours after the operation, the patient complained of lower abdominal pain, nausea and vomiting. The physical examination demonstrated an acute abdomen with diminished bowel sound, abdominal guarding and rebound tenderness. The abdominal computed tomography (CT) revealed several foci of air overlying the anterior aspect of the vertebral body at the L5-S1 level without definitive injury of vessel structures (Fig. 1). An exploratory laparotomy noted a 1 × 0.5 cm sized perforation in the midjejunum, lying on the antimesenteric border 120 cm apart from the Treiz ligament, and close to the retroperitoneum adjacent to the L5-S1 level. The segment of the small bowel containing perforation site was resected, and then primary anastomosis of the jejunum was performed. The postoperative course was uneventful. The patient was discharged and returned to work without significant neurological deficit or late discitis.
Fig. 1.
Small bowel injury in a 47-year-old man after the microdiscectomy at the L5-S1 level. Six hours later after surgery, contrast-enhanced abdominal image shows multiple small extraluminal air densities around distal ileum, both common internal and external iliac arteries (anterior aspect of the vertebral body).
DISCUSSION
The anterior portion of the annulus fibrosus generally is much thicker than the posterior portion, and along with the anterior longitudinal ligament, might be expected to provide a strong barrier to anterior penetration by instruments during discectomy. However, the barrier effect of these structures may not be allowed in patients with anterior disc herniation or degeneration. Especially, the fact that anterior disc herniation due to perforation of the annulus and the anterior longitudinal ligament can occur with a higher prevalence rate of 29.2% in MR imaging study emphasizes that anterior perforation may occur frequently, without warning even in experienced surgeons9). Intraoperative vascular injury, the most potentially life-threatening complication due to anterior perforation, may become evident if brisk bleeding produces hypotension or shock. It is estimated that symptomatic vascular injuries, during lumbar disc surgery, occurs in 1.6-4.5 per 10.000 cases14,17). The two most common vascular injuries are tearing of the left common iliac artery, and creation of an arteriovenous fistula between the right common iliac artery and the inferior vena cava5). About 80% of vascular injuries are associated with operation at the L4-5 disc space, as the left common iliac artery crosses directly from left to right over this disc.
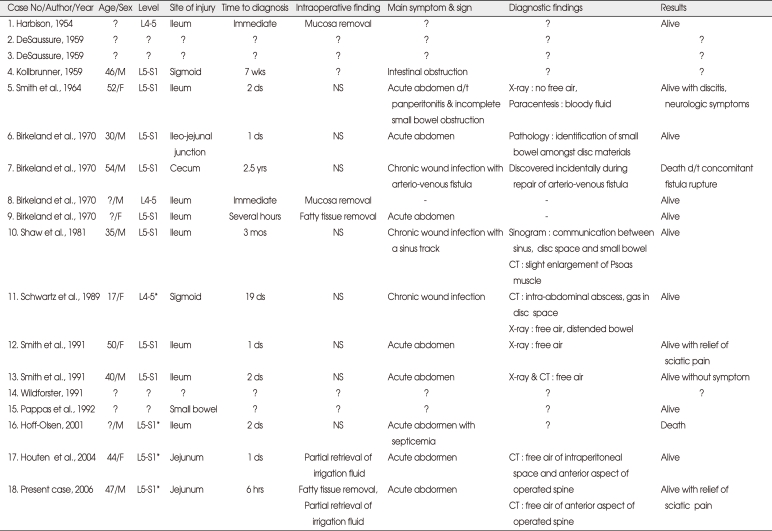
Isolated intestinal injury after lumbar discectomy is less common than vascular injury because the bowel is far to the disc. Even though it is difficult to determine its incidence, a large scaled study presented by the German Society of Neurological Surgery reported an incidence of 0.0015% (1 case in a series of 68,329 patients)14). Since Harbison6) in 1954, first reported a bowel injury, in a series of major vascular complications after intervertebral disc surgery, eighteen case reports have been published, including this one, describing isolated bowel injury during lumbar discectomy (Table 1)6-8,12,15-17).
Table 1.
Summary of reported cases with intestinal perforation after lumbar discectomy
*: microscopic, ? : not defined, - : not checked. F : female, hrs : hours, M : male, NS : nonspecific, mos : months, yrs : years, wks : weeks
After the review of the reported cases it was observed that bowel injuries most commonly occur with operation at the L5-S1 level and involve the small intestine, as in our case. Anatomically, since the root of the mesentery of the small bowel arising in front of the vertebral column extends obliquely from the second lumbar vertebra to the right sacroiliac joint, the small bowel is more likely to be injured than the large bowel. An inadvertent penetration with an instrument, into the peritoneal cavity, is more likely to cause overt intestinal injury if the intra-abdominal contents are compressed against the anterior aspect of the lumbosacral disc, as in prone position of obese and short patient, in addition to the defect of the annulus and the anterior longitudinal ligament. Generally, the microsurgical discectomy would be superior in visualization operative field and reducing of complication rate compared with conventional discectomy. However, four cases of bowel injury following lumbar microdiscectomy were reported. The long-term neurologic outcomes of conventional open lumbar discectomy and microdiscectomy have been reported to be quite similar2,13). Moreover, microscopic discectomy has not revealed a benefit in reducing the bowel injury during the lumbar discectomy.
In contrast to vascular injury, bowel injuries have been uncommonly recognized in the operating room. Based on this review, however, careful assessment of fat-contained mucosa in removed disc materials and estimation of retrieval volume of the irrigated saline for the disc space may be employed as useful intraoperative maneuvers to identify the occurrence of an anterior perforation. Patients generally complain of acute abdomen, abdominal tenderness and rebound tenderness with distension over the course of several days. In these cases, plain radiography or abdominal CT scans confirmed free air in abdominal cavity and the anterior portion of the spine at the location of surgery. However, in a few instances, the diagnosis of bowel injury was delayed for months to years after the initial operation; in these cases the presentation was as chronic wound infection and intestinal obstruction.
Although the prognosis of bowel injury after lumbar discectomy is not dismal compared to that of vascular injury, the fatal course was led by generalized peritonitis with septisemia7) or concomitant vascular injury possibly induced by chronic infection. Considering delay in diagnosis is associated with a high morbidity and mortality rate after bowel injury, especially with small bowel perforation3), exploratory laparotomy following prompt diagnostic evaluation should be performed to repair the injured intestine using a primary suture or resection and anastomosis.
There are certain precautions that can be considered that may help prevent this complication4,11). Most of all, careful review of radiological studies enables identification of defects in the integrity of the anterior annulus fibrosus and anterior longitudinal ligament, and allows for the estimation of the degree of disc degeneration. In cases with these structural changes, the barrier effect of these structures cannot prevent anterior perforation. To prevent close proximity between the bowel and the operated disc in prone position, the pillows placed under the abdomen should not be used. Depth marking of instruments is useful for surgeons to estimate the relationship between inserted instrument and disc space. As a general rule no instrument should be inserted more than 3 cm into a lumbar disc space. In addition, using a pituitary rongeur, the jaw should be opened maximally immediately after introducing it into the disc space. This technique can reduce the chance of the instrument passing through the annulus anteriorly. According to Balderston et al.1) a removal of only the displaced fragment or a limited discectomy can be used to reduce the chance of deep placement of instruments in the disc space and the risk of anterior perforation.
CONCLUSION
We described a rare case of intestinal injury after lumbar microdiscectomy. Although this complication is very rare, it can lead to the fatal course by general peritonitis with septicemia or chronic infection including the vertebral column. Therefore, further discussing and presentation of technical microdiscectomy method will help to prevent this complication and spinal neurosurgeons must keep in mind of this complication.
References
- 1.Balderston RA, Gilyard GG, Jones AA, Wiesel SW, Spengler DM, Bigos SJ, et al. The treatment of lumbar disc herniation : simple fragment excision versus disc space curettage. J Spinal Disord. 1991;4:22–25. [PubMed] [Google Scholar]
- 2.Barrios C, Ahmed M, Arrótegui J, Björnsson A, Gillström P. Microsurgery versus standard removal of the herniated lumbar disc. A 3-year comparison in 150 cases. Acta Orthop Scand. 1990;61:399–403. doi: 10.3109/17453679008993549. [DOI] [PubMed] [Google Scholar]
- 3.Dixon JM, Lumsden AB, Piris J. Small bowel perforation. J R Coll Surg Edinb. 1985;30:43–46. [PubMed] [Google Scholar]
- 4.Döşoglu M, Iğ M, Pehlivan M, Yildiz KH. Nightmare of lumbar disc surgery : iliac artery injury. Clin Neurol Neurosurg. 2006;108:174–177. doi: 10.1016/j.clineuro.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Goodkin R, Laska LL. Vascular and visceral injuries associated with lumbar disc surgery : medicolegal implications. Surg Neurol. 1998;49:358–370. doi: 10.1016/s0090-3019(97)00372-8. discussion 370-372. [DOI] [PubMed] [Google Scholar]
- 6.Harbison SP. Major vascular complications of intervertebral disc surgery. Ann Surg. 1954;140:342–348. doi: 10.1097/00000658-195409000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoff-Olsen P, Wiberg J. Small bowel perforation as a complication of microsurgical lumbar discectomy : a case report and brief review of the literature. Am J Forensic Med Pathol. 2001;22:319–321. doi: 10.1097/00000433-200109000-00025. [DOI] [PubMed] [Google Scholar]
- 8.Houten JK, Frempong-Boadu AK, Arkovitz MS. Bowel injury as acomplication of microdiscectomy : case report and literature review. J Spinal Disord Tech. 2004;17:248–250. doi: 10.1097/00024720-200406000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Jinkins JR, Whittemore AR, Bradley WG. The anatomic basis of vertebrogenic pain and the autonomic syndrome associated with lumbar disk extrusion. AJR Am J Roentgenol. 1989;152:1277–1289. doi: 10.2214/ajr.152.6.1277. [DOI] [PubMed] [Google Scholar]
- 10.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–215. [Google Scholar]
- 11.Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, Tsolakis JA. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002;24:189–195. doi: 10.1053/ejvs.2002.1682. [DOI] [PubMed] [Google Scholar]
- 12.Pappas CT, Harrington T, Sonntag VK. Outcome analysis in 654 surgically treated lumbar disc herniations. Neurosurgery. 1992;30:862–866. doi: 10.1227/00006123-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Postacchini F, Cinotti G, Perugia D. Microdiscectomy in treatment of herniated lumbar disc. Ital J Orthop Traumatol. 1992;18:5–16. [PubMed] [Google Scholar]
- 14.Ramirez LF, Thisted R. Complications and demographic characteristics of patients undergoing lumbar discectomy in community hospitals. Neurosurgery. 1989;25:226–230. doi: 10.1097/00006123-198908000-00012. discussion 230-231. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz AM, Brodkey JS. Bowel perforation following microsurgical lumbar discectomy. A case report. Spine (Phila Pa 1976) 1989;14:104–106. doi: 10.1097/00007632-198901000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Smith EB, DeBord JR, Hanigan WC. Intestinal injury after lumbar discectomy. Surg Gynecol Obstet. 1991;173:22–24. [PubMed] [Google Scholar]
- 17.Wildförster U. [Intraoperative complications in lumbar intervertebral disk operations. Cooperative study of the spinal study group of the German Society of Neurosurgery] Neurochirurgia (Stuttg) 1991;34:53–56. doi: 10.1055/s-2008-1052055. [DOI] [PubMed] [Google Scholar]