Abstract
Aims
The demographics, ethnicity, symptoms, lifestyle characteristics, and treatment outcomes are analyzed in participants of a study designed to evaluate uterine leiomyoma growth and correlate symptoms and outcomes in a clinically relevant population of women (Fibroid Growth Study).
Methods
Women included in the Fibroid Growth Study (FGS) completed a medical history and physical examination, underwent T1-weighted and T2-weighted magnetic resonance image (MRI) scans, provided urine and blood samples at each scheduled MRI, and responded to an initial extensive telephone-administered questionnaire followed by abbreviated monthly questionnaire updates. Summary scores were developed to quantify stress, pain, and bleeding. The Wilcoxin test was used for statistical comparisons between study participant characteristics and tumor-related characteristics.
Results
Participants included 116 premenopausal women, ranging in age from 20 to 54 years; 48% were black women, 41% were white women, 10% were women of other or multiple racial backgrounds, and 1% did not self-identify. Over 90% of participants had multiple leiomyomas, and nearly a third had more than 10. Black women were younger and had more fibroids, but no differences were found in the proportions of black and white women choosing an intervention; 44% of black women and 40% of white women chose intervention during the study.
Conclusions
There was no correlation between number of leiomyomas or uterine size and choosing treatment. However, women who opted for treatment were more symptomatic, with higher bleeding and pain scores, compared with the women with no intervention. Consequently, our study suggests that once women are symptomatic, black and white women choose surgery as a treatment method for the same reasons and at about the same rates. Moreover, our data suggest that bleeding and pain, not the size or multiplicity of fibroids, determine the choice for intervention. Therefore, aggressive management of pain and bleeding may be effective in reducing the need for surgical intervention.
Introduction
Uterine leiomyomas (fibroids) are the most common reproductive tract tumor in women and a significant health concern in premenopausal women.1 Although the tumors are not malignant, they are the leading cause for hysterectomy in the United States.2,3 Leiomyoma-related healthcare accounted for about 320 thousand hospital procedures and an estimated total direct cost of more than 2 billion dollars per year, primarily related to hysterectomy costs.2 Previous studies found that among women with leiomyomas and uterine size of ≥8 weeks gestational age, about 20% had hysterectomies within a year.4 Among newly diagnosed cases of uterine fibroids in the Nurses' Health Study, about 15% had hysterectomy within 21 months.5 In a more general population of women diagnosed with leiomyomas, only about one third had surgery within 5 years.6 Factors possibly associated with increased likelihood of hysterectomy included large uterine size, excessive bleeding, and prior surgery for pelvic adhesions or gallbladder removal.
Black women are at a particularly high risk for developing fibroids. Ultrasound screening for leiomyomas in randomly selected members of a large urban healthcare plan estimated that black women had over an 80% cumulative incidence of leiomyomas by age 50, and white women had nearly a 70% cumulative incidence of leiomyomas by the same age.7 A number of studies have shown that black women have leiomyomas at younger ages and have more hysterectomies and myomectomies at earlier ages than white women.3,5,7
Women typically have more than one leiomyoma, which may or may not cause similar problems or grow at similar rates, complicating conclusions about tumor characteristics and clinical outcomes. Most leiomyomas grow slowly and remain asymptomatic for prolonged periods. However, anecdotal reports suggest that individual leiomyomas may undergo episodes of rapid growth and become clinically symptomatic in a short time period. Fast-growing, large leiomyomas appear to be the most problematic. Given that 70%–80% of women have leiomyomas but not all are symptomatic, a clinically relevant question is: What causes leiomyomas to grow and cause symptoms?
The Fibroid Growth Study (FGS) was designed to investigate the growth dynamics of uterine leiomyomas over time and correlate symptoms and outcomes in a clinically relevant population of women. A clinically relevant population was defined as premenopausal women with preexisting large fibroids (initially as ≥5 cm diameter and a uterus enlarged to the size of gestational week 12 of pregnancy), predicting that this population of women would likely have symptoms associated with fibroids and be more likely to choose a therapeutic intervention. Because surgical intervention is the most common treatment for uterine leiomyomas, we anticipated that about one third of the women enrolled in the study would elect to have either a hysterectomy or a myomectomy. Consequently, we planned to follow participants for 1 year or until surgery (myomectomy or hysterectomy). Although the selection criteria were set to recruit women with large tumors and clinical symptoms, surgery was not a requirement for study inclusion. The ability to have magnetic resonance imaging (MRI) data over a 1-year period for women who did not have surgery was considered highly important and informative. Another important aspect of the study was to investigate leiomyoma growth in women of minority populations. The goal of recruitment was to ensure that half of the study population represented the minority population most affected by the condition (i.e., black women).
This paper presents the participant demographics, lifestyle, and symptoms related to fibroids and our analysis of the determinants for choosing therapeutic intervention during the course of the study.
Materials and Methods
The FGS was conducted at the General Clinical Research Center (GCRC) at University of North Carolina (UNC) Medical Center, Chapel Hill, and approved by the human subjects review boards at the National Institute of Environmental Health Sciences (NIEHS) and UNC. The inclusion criteria for participant enrollment were (1) age >18 years, (2) premenopausal, (3) not currently pregnant, (4) willing and able to have (MR) (weight <350 pounds, waist <52 inches, and no IUD) at the UNC Medical Center, (4) not on gonadotropin-releasing hormone (GnRH) therapy, and (5) ultrasound-confirmed diagnosis of leiomyomas of ≥5 cm in diameter and a uterus enlarged to the size of gestational week 12 of pregnancy. To obtain fibroids of smaller sizes for the growth analysis component of the study, the size criterion was amended in the last few months of the study to include women with leiomyomas ≥2 cm in diameter and at least an 8-week gestational uterus size. The 4 women enrolled with this smaller size criterion were included in this analysis to represent the entire population of women enrolled in the FGS. After enrollment and informed consent, MRI scans were conducted at the first visit and then conducted approximately 3, 6, and 12 months later. Women were asked to bring all current medications for recording. If a participant chose one of the major treatment options for fibroid-related problems (embolization or surgery) and the last MRI took place >2 months prior, the patient was scheduled for a presurgery MRI. Participants having myomectomy had the option to remain in the study postsurgery; participants who had hysterectomy or embolization were not followed posttreatment. During each scheduled MRI visit, participants underwent a pelvic examination, provided urine and blood samples, and responded to interview questions about medical history (initial visit) and medication use (initial visit) Data on demographics, lifestyle factors, and symptoms were collected with an initial telephone interview. The symptom data were updated with monthly telephone interviews. Women who elected surgery were contacted with a follow-up telephone-administered questionnaire to assess reasons for surgery.
Study recruitment
Because the study was based at the UNC Medical Center, most participants were recruited through the physician network within the UNC Hospitals' system. The majority were referred from the obstetrics/gynecology ultrasound clinic. Family practice physicians in the network received brochures, and a grand rounds presentation described the study. Additional recruitment came from women responding to the website, word of mouth, press releases, public service announcements on the radio, and informational study bookmarks placed at area libraries.
Symptom monitoring
During the initial enrollment interview, women were asked about their general health, current symptom status, stress, pelvic pain and discomfort, and vaginal bleeding. The questions about stress, pelvic pain, and bleeding were also asked at each subsequent monthly telephone interview. A stress index was calculated by combining answers to eight questions about economic difficulties, time pressures, experiencing “too much to handle,” and the impact of this stress on sleep and daily life. Each question had four choices rated from 0 to 3 (low to high stress). These values were summed for all eight questions to yield a score ranging from 0 to 24. The score was then multiplied by 100/24 to convert it to a 100-point scale. Similarly, a pain score was calculated by combining answers from two questions assessing the amount of pain or discomfort, with four choices rated 0–3; two questions were about number of days experiencing pain (rated 0–8) or discomfort (rated 0–4), and one question was about days stayed home because of pain (rated 0–6). A scale was also developed to assess whether bleeding was a problem (perceived bleeding problem scale), including whether vaginal bleeding limited daily responsibilities or social activities. Finally, a 100-point amount-of-bleeding scale was developed based on number of days of bleeding, number of days of spotting, pad/tampon use on heavy bleeding days, gushing-type bleeding, clots, needing extra means of protection beyond pads and tampons, and frequency of menses. As validation, we evaluated the correlation between the amount-of-bleeding score and hematocrit or hemoglobin levels. The specific questions used for all the symptom scales can be found in the enrollment questionnaire (www.niehs.nih.gov/fibroids/home).
Statistical analysis
Statistical tests included Wilcoxin test and two-sided Mann-Whitney to compare participant and tumor-related variables, except for the hormone use variable, which was tested with the chi-square test. Spearman correlation was used for associations among bleeding scores, hematocrit level, and hemoglobin level.
Results
Of 151 women initially evaluated in the study, 116 women met all requirements and completed at least one MRI. Women were excluded because they began taking lupron (n = 1) or were not eligible based on review of the first MRI (n = 4). Participants withdrew because they were planning pregnancy or because of other study-related concerns, such as claustrophobia or scheduling difficulties (n = 22). Only 8 women dropped out or were excluded because of noncompliance (4 African Americans, 2 white women, and 2 women of other heritage). Among the 116 participants included in the study, 30 women opted for treatment after one MRI, 8 women opted for treatment after their second MRI, 4 had treatment after their third MRI, and 6 women had treatment after their fourth MRI while still in the study. The study ended before 25 women completed a fourth MRI. Women who had a hysteroscopic resection or a myomectomy before completing the study (n = 22) were invited to continue in the study after treatment; 20 completed further monthly questionnaires, and 17 completed additional MRIs, as well.
Characteristics of study participants
The demographic and lifestyle characteristics of the 116 participants in the FGS are shown in Table 1. Nearly half self-identified as African American/black or black with other heritage (subsequently referred to as black participants), 48 self-identified as white/Caucasian (subsequently referred to as white participants), and 11 were of other heritages. Most participants were college educated and employed and had health insurance. Fewer black participants had postbaccalaureate degrees and high household incomes compared with white participants. Black participants were also slightly younger (p = 0.037) compared with white participants. The average age for black participants was 38 years and for whites was 40 years.
Table 1.
Characteristics of Participants in Fibroid Growth Study, Enrollment 2001–2004a
| Characteristic | Total1 (n = 116) n (%) | Black (n = 57) n (%) | White (n = 48) n (%) |
|---|---|---|---|
| Age, years | |||
| <30 | 9 (8) | 4 (7) | 4 (8) |
| 30–34 | 24 (21) | 16 (29) | 8 (17) |
| 35–39 | 23 (20) | 12 (22) | 6 (12) |
| 40–44 | 33 (28) | 16 (29) | 13 (27) |
| 45+ | 27 (23) | 7 (13) | 17 (35) |
| p = 0.372 | |||
| Educationb | |||
| High school | 26 (23) | 14 (25) | 6 (12) |
| College | 42 (37) | 22 (40) | 17 (35) |
| Postbaccalaureate degree | 47 (41) | 19 (35) | 25 (52) |
| Missing | 1 | ||
| Household incomec | |||
| <$40,000 | 19 (17) | 11 (22) | 5 (11) |
| $40,000–59,999 | 26 (24) | 14 (27) | 11 (23) |
| $60,000–99,999 | 48 (44) | 27 (47) | 18 (38) |
| ≥$100,000 | 17 (15) | 2 (4) | 13 (28) |
| Missing | 6 | 4 | 2 |
| Employed | |||
| No | 19 (17) | 10 (18) | 8 (17) |
| Part-time (<37 hours/week) | 19 (17) | 9 (16) | 7 (15) |
| Full-time | 77 (67) | 36 (65) | 33 (69) |
| Missing | 1 | ||
| Married or living as married | |||
| Yes | 55 (48) | 22 (41) | 28 (58) |
| No | 59 (52) | 32 (59) | 20 (42) |
| Missing | 2 | 1 | |
| Health insurance | |||
| Yes | 107 (95) | 53 (95) | 46 (96) |
| No | 6 (5) | 3 (5) | 2 (4) |
| Missing | 3 | 1 | |
| BMI | |||
| <25 | 43 (37) | 16 (29) | 23 (48) |
| 25–29 | 37 (32) | 20 (36) | 12 (25) |
| 30–34 | 17 (15) | 8 (15) | 8 (17) |
| 35+ | 19 (16) | 11 (20) | 5 (10) |
| Smoking | |||
| Never | 83 (73) | 41 (75) | 34 (71) |
| Past | 22 (19) | 8 (15) | 11 (23) |
| Current | 9 (8) | 6 (11) | 3 (6) |
| Missing | 2 |
Total sample includes 11 participants in the Other category for ethnicity.
High school includes those with some training beyond high school but no college degree; college degree includes those with some postbaccalaureate education but no further degree.
Household income is adjusted for number of people in household and indexed to a household of two.
Fibroid and symptom characteristics of the participants are shown in Table 2. Over 90% of participants had multiple leiomyomas, with nearly a third having more than 10. Black participants had slightly more leiomyomas than white participants (p = 0.04). Most participants were first diagnosed with leiomyomas within the last 5 years. Ten had prior surgery for leiomyomas (5 women had myomectomies, 5 women had hysteroscopic resections). Two women enrolled in the study within 1 year of their last surgery, 6 women enrolled within 1–5 years, and 2 women enrolled > 5 years after their last surgery. Although black participants had slightly more leiomyomas than white participants, symptom scores were similar between black and white participants (Table 2). About 90% of both black and white participants considered themselves to be in good to excellent health, but less than half were satisfied with their current symptom status. No differences were found between black and white participants having treatment or in their symptoms, including pain or bleeding. Of the 48 participants who had surgical or embolization treatment, 25 (44%) were black and 19 (40%) were white (Table 2). The most common intervention was myomectomy.
Table 2.
Fibroid and Symptom Characteristics for Participants in Fibroid Growth Study, Enrollment 2001–2004a
| Characteristic | Total (n = 116) n (%) | Blacks (n = 57) n (%) | Whites (n = 48) n (%) |
|---|---|---|---|
| Time since initial diagnosis of fibroids (years) | |||
| <1 | 33 (29) | 14 (25) | 17 (37) |
| 1–2 | 26 (23) | 14 (25) | 9 (20) |
| 3–5 | 19 (17) | 9 (16) | 8 (17) |
| 5–9 | 19 (17) | 11 (20) | 7 (15) |
| 10+ | 15 (13) | 8 (14) | 5 (11) |
| Missing | 4 | 1 | 2 |
| p = 0.21b | |||
| Uterine volume (cm3)c | |||
| <100 | 9 (8) | 3 (5) | 6 (12) |
| 100–249 | 47 (41) | 24 () | 19 (40) |
| 250–499 | 23 (20) | 12 (21) | 9 (19) |
| 500–999 | 23 (20) | 11 (19) | 8 (17) |
| 1000+ | 14 (12) | 7 (12) | 6 (12) |
| p = 0.31 | |||
| Number of fibroidsd | |||
| 1 | 9 (8) | 2 (4) | 5 (10) |
| 2 | 14 (12) | 6 (11) | 8 (17) |
| 3–5 | 23 (20) | 11 (19) | 10 (21) |
| 6–10 | 35 (30) | 19 (33) | 12 (25) |
| >10 | 35 (30) | 19 (33) | 13 (27) |
| p = 0.04 | |||
| General health | |||
| Excellent to very good | 62 (54) | 28 (49) | 27 (56) |
| Good | 43 (38) | 22 (39) | 19 (40) |
| Fair | 9 (8) | 6 (11) | 2 (4) |
| Poor | 1 (1) | 1 (2) | 0 (0) |
| Missing | 1 | ||
| p = 0.44 | |||
| Hormone use | |||
| None | 86 (74) | 51 (75) | 35 (73) |
| Oral contraceptives for contraception | 11 (9) | 7 (10) | 4 (8) |
| Oral contraceptives for irregular period or symptoms | 13 (11) | 5 (7) | 8 (17) |
| Other hormone | 5 (4) | 4 (7) | 1 (2) |
| Missing | 1 | ||
| p = 0.30 | |||
| Tolerance of current symptoms | |||
| Satisfied | 48 (42) | 19 (33) | 23 (48) |
| Mixed feelings | 31 (27) | 18 (32) | 11 (23) |
| Dissatisfied | 19 (17) | 10 (18) | 8 (17) |
| Very dissatisfied | 17 (15) | 10 (18) | 6 (12) |
| Missing | 1 | ||
| p = 0.19 | |||
| Stress scale | |||
| Mean | 32.2 | 36.0 | 29.1 |
| SD | 17.6 | 20.1 | 13.8 |
| Range | 0–75 | 0–75 | 4.2–66.7 |
| Missing | 2 | 1 | |
| p = 0.11 | |||
| Pain scale | |||
| Mean | 31.9 | 33.6 | 30.0 |
| SD | 25.1 | 24.2 | 25.0 |
| Range | 0–100 | 0–83 | 0–88 |
| Missing | 3 | 1 | 1 |
| p = 0.50 | |||
| Bleeding-problem scale | |||
| Mean | 32.9 | 37.5 | 27.3 |
| SD | 30.4 | 31.4 | 28.1 |
| Range | 0–100 | 0–100 | 0–89 |
| Missing | 2 | 1 | |
| p = 0.08 | |||
| Amount-of-bleeding scale | |||
| Mean | 18.4 | 17.9 | 18.5 |
| SD | 14.8 | 13.8 | 15.9 |
| Range | 0–56 | 0–56 | 0–51 |
| Missing | 3 | 1 | 1 |
| p = 0.94 | |||
| Treatment | |||
| None | 68 (59) | 32 (56) | 29 (60) |
| GnRH agonist in preparation for surgery | 7 | 2 | 3 |
| Hysteroscopic resection | 4 | 1 | 3 |
| Embolization | 2 | 1 | 1 |
| Myomectomy | 20 | 12 | 7 |
| Hysterectomy | 15 | 9 | 5 |
| Missing | 0 | ||
| p = 0.58 |
Total sample includes 11 participants in the Other category for ethnicity.
p values are based on comparing the entire distribution of the variables in African Americans and whites using the nonparametric Wilcoxon rank sum test, except for the hormone use and treatment variables, which were tested with the chi-square test.
Uterine volume was calculated from ultrasound data on uterine length, width, and AP diameter using the ellipsoid formula (0.52 × L × W × AP); when ultrasound uterine diameters were not available, the uterine volume was determined based on the pelvic examination estimated weeks of gestation.
Number of fibroids was assessed by counting fibroids observable on the first visit MRI. In the few cases when first visit MRI were of poor quality because the patient moved, the count was made on the second visit MRI.
Comparisons of participants who opted for therapeutic intervention
Because no differences were found between blacks and whites in having treatment or in symptoms, we combined ethnicities in comparing those who chose intervention and those who did not choose intervention (Table 3). Time since first diagnosis of leiomyomas, uterine size, and number of leiomyomas were similar for the 48 participants who opted for intervention (hormonal, surgical, or others combined) compared with the 68 participants who did not choose intervention (Table 3). Stress scale scores were also similar for women opting for treatment and women not opting for treatment. However, participants choosing treatment were more concerned with their symptoms (p < 0.01) and had higher scores on pain (p = 0.02). Participants choosing treatment also had higher bleeding scores (p < 0.001) compared with women who did not choose treatment (Table 3). Moreover, scores for perceived bleeding and amount of bleeding increased over time with respect to first diagnosis (p = 0.013 and p = 0.029, respectively). The accuracy of the bleeding scores was supported by the strong overall (all races combined) correlation found between the amount of bleeding reported and clinical measurements of hematocrit and hemoglobin. Specifically, the correlation between the amount of bleeding and hematocrit was −0.2427 (p = 0.0096) and −0.2995 for amount of bleeding and hemoglobin (p = 0.0013). The overall mean hematocrit values for treated and untreated participants were 36.6875 (±SE 0.4972) and 37.202 (SE ± 0.3752), respectively, and mean hemoglobin values were 12.3583 (±SE 0.2125) and 12.5662 (SE ± 0.1586), respectively.
Table 3.
Fibroid and Symptom Characteristics for Treated and Untreated Participants in Fibroid Growth Study, Enrollment 2001–2004a
| Characteristic | Nontreatment n (%) | Treatment n (%) | Characteristic | Nontreatment n (%) | Treatment n (%) |
|---|---|---|---|---|---|
| Age | Tolerance of current symptoms | ||||
| <30 | 5 (7) | 4 (8) | Satisfied | 34 (50) | 14 (30) |
| 30–34 | 14 (21) | 10 (21) | Mixed feelings | 20 (29) | 11 (23) |
| 35–39 | 9 (13) | 14 (29) | Dissatisfied | 10 (15) | 9 (19) |
| 40–44 | 18 (26) | 15 (21) | Very dissatisfied | 4 (6) | 13 (28) |
| 45+ | 22 (32) | 5 (10) | Missing | 0 | 1 |
| p = 0.12 | p < 0.01 | ||||
| Time since initial diagnosis of fibroids (years) | Stress scale | ||||
| <1 | 21 (32) | 12 (26) | Mean | 31.4 | 33.3 |
| 1–2 | 16 (25) | 10 (21) | SD | 17.0 | 18.6 |
| 3–5 | 9 (14) | 10 (21) | Range | 4–67 | 0–75 |
| 5–9 | 10 (15) | 9 (19) | Missing | 0 | 0 |
| 10+ | 9 (14) | 6 (13) | p = 0.68 | ||
| Missing | 4 | ||||
| p = 0.65 | |||||
| Uterine volume (cm3)b | Pain scale | ||||
| <100 | 5 (7) | 4 (8) | Mean | 27.0 | 38.7 |
| 100–299 | 30 (44) | 17 (35) | SD | 23.4 | 25.9 |
| 300–499 | 14 (21) | 9 (19) | Range | 0–100 | 0–87.5 |
| 500–999 | 12 (18) | 11 (23) | Missing | 2 | 1 |
| 1000+ | 7 (10) | 7 (15) | p = 0.02 | ||
| p = 0.42 | |||||
| Number of fibroidsc | Bleeding-problem scale | ||||
| 1 | 5 (7) | 4 (8) | Mean | 23.7 | 46.6 |
| 2 | 9 (13) | 5 (10) | SD | 24.1 | 33.8 |
| 3–5 | 15 (22) | 8 (17) | Range | 0–100 | 0–100 |
| 6–10 | 20 (29) | 15 (31) | Missing | 0 | 2 |
| >10 | 19 (28) | 16 (33) | p < 0.001 | ||
| p = 0.58 | |||||
| Hormone use | Amount-of-bleeding scale | ||||
| None | 51 (75) | 35 (74) | Mean | 14.6 | 23.7 |
| Oral contraceptives for contraception | 6 (9) | 5 (11) | SD Range | 11.60–46 | 17.10–56 |
| Oral contraceptives for irregular period or symptoms | 8 (12) | 5 (11) | Missing | 2 | 2p < 0.01 |
| Other hormone | 3 (4) | 2 (4) | |||
| Missing | 0 | ||||
| p = 0.94 | |||||
| General health | |||||
| Excellent to very good | 38 (56) | 24 (51) | |||
| Good | 24 (35) | 19 (40) | |||
| Fair | 6 (9) | 3 (6) | |||
| Poor | 0 | 1 (2) | |||
| Missing | 0 | 1 | |||
| p = 0.65 |
p values are based on comparing the entire distribution of the variables in treated and not treated participants with the nonparametric Wilcoxon rank sum test except for the hormone use variable, which was tested with the chi-square test.
Uterine volume was calculated from ultrasound data on uterine length, width, and AP diameter using the ellipsoid formula (0.52 × l × w × AP), and when ultrasound uterine diameters were not available, the uterine volume was determined based on the pelvic examination estimated weeks of gestation.
Number of fibroids was assessed by counting fibroids observable on the first visit MRI. In the few cases when first visit MRI were of poor quality because the patient moved, the count was made on the second visit MRI.
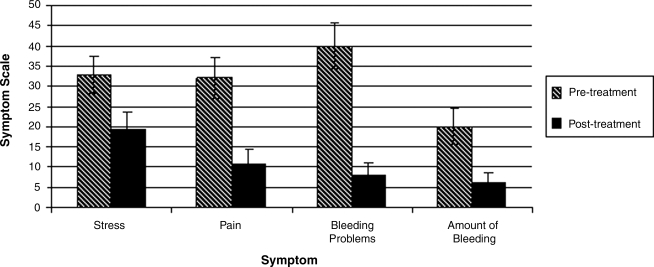
Twenty participants opting for surgery were followed for an average of 7.5 months (±0.8) after surgery. The 20 women followed after treatment showed similar pretreatment scores on the symptom scales as at the initial interview, but their scores decreased markedly after treatment (Fig. 1).
FIG. 1.
Comparisons of clinical symptoms in FGS participants before and after treatment. Symptom scales were calculated by summing assigned values to specific questionnaire responses and converting the sums to a 100-point scale. Stress, pain, bleeding problems, and amount of bleeding were identified as significant factors related to treatment in the overall FGS population. These symptoms are further compared prior to and after treatment in the subset of participants (n = 20) who had treatment and were available for a follow-up questionnaire after treatment.
Discussion
We sought to understand the characteristics of premenopausal women with large fibroids and the factors underlying a choice for therapeutic intervention. Rigorous review of the data from 151 women who initially enrolled in the FGS determined that 116 participants met all criteria for inclusion into the study analysis. Of the 116 participants included in this present analysis, 48 participants opted for intervention. We found that the primary determinants for seeking treatment were pain and bleeding. Importantly, we validated the self-reported bleeding data by comparing clinical measurements of hematocrit and hemoglobin to find highly significant relationships. Other physical factors, including time since initial diagnosis, number of fibroids, and hormone use, were similar between FGS participants choosing treatment and those who did not. A previous study found that bleeding symptoms were associated with greater odds of having a hysterectomy.6 Weber et al. also reported an interaction between age and uterine size with greater odds of hysterectomy, an interaction that we did not find in our study. The difference may be a reflection of the selected population in the FGS, as well as the inclusion of other treatments (embolization, myomectomy) in addition to hysterectomy. We also found a significant difference in the tolerance of symptoms between FGS participants choosing treatment and those who did not; however, no differences were found between these two groups in perceived stress levels or assessment of their general health. Based on analysis of the extensive questionnaires participants completed at each visit and during monthly telephone interviews, the main symptoms experienced by these FGS participants included dissatisfaction with general health, discomfort, pain, and bleeding.
Another important aspect of the study was to investigate leiomyoma growth in women of minority populations. The goal of recruitment was to ensure that half of the study population represented the minority population most affected by the condition (i.e., black women). Indeed, about half (49%) of the participants were black, 9% identified as other or multiple racial backgrounds, and 41% were white. The success of recruitment was largely attributed to the general characteristics of the patient population at UNC Hospitals' system. Secondary methods of recruitment were initiated to maintain diversity. These included distributions of brochures to local obstetrics/gynecology and family practices and placing of informational study bookmarks at area libraries and of press releases and public service announcements on the radio.
Previous studies have shown that African American women have leiomyomas at younger ages, have more leiomyomas, and have more hysterectomies and myomectomies than do white women.5 In our study, black participants were younger and had more leiomyomas compared with white participants. However, we found no differences in symptom scores or surgery rates between black and white participants. This apparent difference between our study population and other reports is likely a result of our emphasis on recruiting women who had larger leiomyomas and who were more likely to be symptomatic. Consequently, our data suggest that once women are symptomatic, black and white women choose surgery as a treatment method for the same reasons and at about the same rates. Moreover, our data suggest that bleeding and pain, not the size or multiplicity of fibroids, determine the choice for intervention. Therefore, aggressive management of pain and bleeding may be effective in reducing the need for surgical intervention in both black and white women.
In summary, of the 116 premenopausal women who completed requirements for the FGS, about half self-identified as either black or white, most had multiple leiomyomas (about one third had > 10 tumors), and most were in good to excellent health, college educated, employed with health insurance, had a BMI >25, were never smokers, and were not using hormones. Black participants were slightly younger and had slightly more leiomyomas than white participants, but similar numbers of black and white participants opted for treatment of uterine leiomyoma. Myomectomy was the most common intervention, and the primary reason for treatment was pain and bleeding.
Acknowledgments
This study was conducted through the General Clinical Research Center at UNC, Chapel Hill, under NIH grant number M01RR00046. Financial support was provided jointly by NIEHS and the National Center for Research on Minority Health and Health Disparities, NIH (Clinical Trial Registry: www.clinicaltrials.com).
We gratefully acknowledge Drs. Richard Semelka, Diane Armao, Xiaoyu Ding, Stephen Aylward, Bruce Lessey, Kimberly Cummings, Jane Schroeder, David Walmer, and Ray Tice and Mr. Jean-Philippe Guyon for their contributions in study design and data analysis and acknowledge the critical contributions of Ms. Martha Turvey, who was the study nurse. Dr. Ronald Herbert, Ms. Mary Wood, Ms. Paulette Daniel, Ms. Andrea Emmanuel, and Dr. Pamela Blackshear were also involved in additional study conduct, data collection, and analysis. We gratefully acknowledge the input on our study design and questionnaires of members of the National Uterine Fibroid Foundation.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Stewart EA. Uterine fibroids. Lancet. 2001;357:293–298. doi: 10.1016/S0140-6736(00)03622-9. [DOI] [PubMed] [Google Scholar]
- 2.Flynn M. Jamison M. Datta S. Myers E. Heath care resource use for uterine fibroid tumors in the United States. Am J Obstet Gynecol. 2006;195:955–964. doi: 10.1016/j.ajog.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 3.Kjerulff KH. Langenberg P. Seidman JD. Stolley PD. Guzinski GM. Uterine leiomyomas. Racial differences in severity, symptoms, and age at diagnosis. J Reprod Med. 1996;41:483. [PubMed] [Google Scholar]
- 4.Carlson KJ. Miller BA. Fowler FJ., Jr The Maine Women's Health Study: II. Outcomes of nonsurgical management of leiomyomas, abnormal bleeding, and chronic pelvic pain. Obstet Gynecol. 1994;83:566–572. doi: 10.1097/00006250-199404000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Marshall LM. Spiegelman D. Barbieri RL, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967–973. doi: 10.1016/s0029-7844(97)00534-6. [DOI] [PubMed] [Google Scholar]
- 6.Weber AM. Mitchinson AR. Gidwani GP. Mascha E. Walters MD. Uterine myomas and factors associated with hysterectomy in premenopausal women. Am J Obstet Gynecol. 1997;176:1213–1219. doi: 10.1016/s0002-9378(97)70337-5. [DOI] [PubMed] [Google Scholar]
- 7.Baird D. Dunson DB. Hill MC. Cousins D. Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: Ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]