Abstract
Background
Allogeneic hematopoietic stem cell transplantation (HSCT) generates multiple problems that vary in complexity and create significant distress for both patients and their caregivers. Interventions that address patient and caregiver distress during allogeneic HSCT have not been tested.
Objective
To evaluate the feasibility of conducting an individualized dyadic problem-solving education (PSE) intervention during HSCT and estimate a preliminary effect size on problem-solving skills and distress. Intervention/Methods: The PSE intervention consisted of four sessions of the Prepared Family Caregiver PSE model. Data were collected with an interventionist log, subject interviews and standardized questionnaires.
Results
Of the thirty-four adult dyads screened, twenty-four were ineligible primarily due to non-English speaking (n=11) and inconsistent caregivers (n=10). Ten dyads (n=20) were enrolled and eight dyads (n=16) completed the intervention. Of the thirty-one sessions, 29 were completed (94%). Worsening patient condition was the primary reason for sessions to be incomplete. Patients attended 90% of the sessions; caregivers attended 74%. Reasons for missed sessions included patient symptom distress and limited caregiver availability. Dyads reported being very satisfied (4.8±0.61; range 1–5) stating “an opportunity to talk” and “creative thinking” were most beneficial.
Conclusion
Results suggest that dyads can participate in PSE during HSCT and view it as beneficial. Participants identified the active process of solving problems as helpful.
Implications for Practice
Targeted interventions that promote effective, meaningful behaviors are needed to guide patients and caregivers through HSCT. Future research recommendations include: testing a version of PSE with fewer sessions, including spousal and non-spousal caregivers and those who are non-English speaking.
Allogeneic hematopoietic stem cell transplantation (HSCT) has become an established and curative treatment for various hematologic malignancies. Different from an autologous HSCT where a patient’s own hematopoietic stem cells are returned following intense chemo- and radio-therapy, an allogeneic HSCT involves the collection of hematopoietic stem cells from healthy donors that are administered to eradicate and/or replace diseased bone marrow in patients with hematological diseases. Although the possible benefits of this treatment are extraordinary, allogeneic HSCT is not without major complications 1.
During early recovery (first 100 days) the major complications arise from chemo- and radio-therapy along with the healthy hematopoietic stem cells which generate a new immune system for the patient. These include infection, organ dysfunction, and acute graft versus host disease, a toxicity where the donor stem cells identify the host (patient) tissue as foreign and initiate an immune attack. This unique complication is characterized by a skin rash, liver dysfunction and/or gastrointestinal diarrhea which will often trigger a hospital admission for immediate clinical management. These complications, along with others, can be significantly burdensome, physically and emotionally, and in some cases, life threatening (e.g. infection during neutropenia). Consequently, during the early transplant phase, patients experience a high level of distress associated with these complications including symptoms such as worry, sleep disturbance, fatigue, nausea, and changes in bowel function and appetite2.
Cancer patients reporting higher symptom distress have been shown to require more support from the health care team 3. Specifically, patients receiving an allogeneic HSCT compared to those receiving autologous HSCT are more likely to be readmitted following transplant4. Therefore, allogeneic HSCT patients are required to remain in the vicinity of the transplant center during the first 3–4 months following transplant for close monitoring and specialized care5. Family members frequently serve as the primary caregivers for the patient during this time and may be a factor in receiving and surviving the allogeneic HSCT6–9. The establishment of this partnership is encouraged by the transplant team during the evaluation phase and required prior to initial discharge or when in the outpatient setting.
Providing information to family members relative to the caregiving responsibilities and experience is fundamental10–12. Caregivers request education to prepare for caregiving12, symptom management10, 11, managing the overall patient needs11, 12, facing challenges12, developing supportive strategies12, and discovering unanticipated rewards and benefits12. The complexities of the caregiving experience however are not limited to the problems directly linked to the HSCT recipient. Caregivers often carry additional responsibilities including the management of a primary residence, finances, and children or pets. Consider the following example that describes the context of one allogeneic HSCT caregiving experience.
Mr. Smith is a 55 y.o. male with progressive non-Hodgkin’s disease proceeding with an allogeneic HSCT. He and his wife are self-employed and have two adult children. They decide that his wife will be his caregiver. As they approach the transplant procedure, they state a fear of this “uncharted territory” and readily identify a number of problems that “worry” them. These include: Temporary relocation (primary resident 500 miles from center); oversight of their primary home, pets, and business; financial resources for two residences and sustenance; identification of alternate caregivers, relationship with new staff and center; treatment compliance; complications of HSCT; and fear of death.
The impact of the transplant experience on family caregivers is not well understood. Although family caregiver psychological distress has been shown to improve over time, studies suggest that caregivers have levels of psychological distress that are equal to, and in some cases, higher when compared to the patient and healthy groups13–16 and may indicate serious psychological illness16, 17. Factors that influence the psychosocial distress of HSCT caregivers have been explored. Higher levels of psychosocial distress experienced by HSCT caregivers are influenced by higher levels of objective burden or activities 18, subjective burden or affective concerns 18, poor patient physical wellbeing 15, greater patient psychological distress 15, and less satisfaction of caregivers with patient needs being met 11.
Current literature provides little to guide interventions for cancer caregivers 19, specifically those caring for patients receiving allogeneic HSCT. Meta-analyses examining the effect of various interventions intended to treat the psychosocial problems of cancer patients, conclude significant beneficial effects 20–22. In addition to improvements in psychological distress, beneficial effects on measures of treatment- and disease related symptoms were also documented 20, 21. More recent studies with cancer patients and their family continue to support the beneficial effect of interventions based on cognitive-behavioral therapy 3, 23, 24.
Social Problem-Solving Therapy (SPST) is an established cognitive-behavioral therapy defined as “a meta-cognitive process by which individuals understand the nature of problems in living and direct their efforts at altering the difficult nature of the situations themselves, their reaction to them, or both” 25. Problem-solving skills have long been recognized as an important resource for coping 26 with problem-solving therapy as an effective intervention for psychological distress outside of cancer 27–30 along with cancer patients and their families 31–34.
In summary, allogeneic HSCT generates multiple problems that can vary in complexity and create significant burden and distress for both the transplant patient and their caregiver. Although their distress can be clinically significant, no interventions including the transplant caregiver, have been tested in this population. Guided by the stress and coping model of Lazarus & Folkman (1984), this study was designed to evaluate the feasibility of conducting a problem-solving education (PSE) intervention in patient and family caregiver dyads during allogeneic HSCT. The secondary objectives were to estimate the effect of the intervention on problem-solving skills and distress, explore the relationships of baseline psychological distress and family functioning to the change in problem solving-skills following PSE, and explore the symptom experience of HSCT family caregivers. The study was approved by an Institute Review Board prior to subject enrollment.
Method
Design
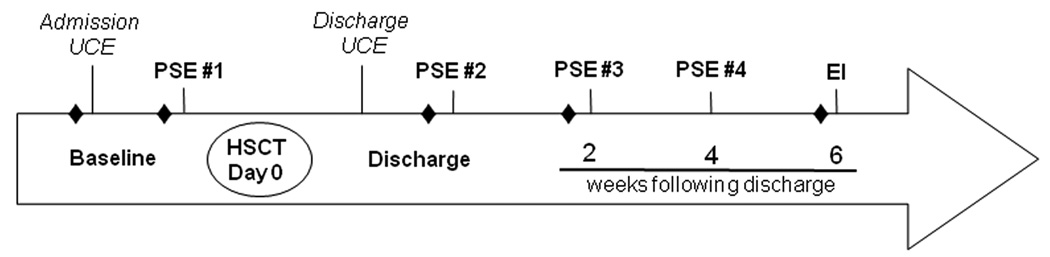
A single group repeated-measures mixed-method design was used to assess the feasibility of a four session problem-solving education intervention during allogeneic HSCT (Figure 1). The study intervention included four PSE sessions: PSE #1 - prior to allogeneic HSCT, PSE #2 - at time of discharge, PSE#3 – two weeks after discharge, and PSE #4 - four weeks after discharge. Dyads also attended admission and discharge transplant education classes [usual care education (UCE)] provided by the hospital, which were consistent across subjects. The UCE addressed unit procedures, the transplant process, common complications and prevention measures, and organizational resources via discussion and written materials. Study data were collected at five time-points during the study. Two baseline questionnaires were administered prior to PSE #1 (pre- and post- the admission education class) to capture any effect of UCE, at two time- points during the intervention period (PSE #2 and #3), and two weeks after the last study intervention session (6 weeks after discharge).
Figure 1.
Study Design and Procedures
Note: UCE: Usual Care Education, PSE: Problem-Solving Education, HSCT: Hematopoietic Stem Cell Transplantation, EI: Exit Interview
♦ = questionnaire administration
Subjects and recruitment
Potential subjects were identified through the accrual process for allogeneic HSCT clinical research protocols at a single site between February and November 2008. Consecutive adult patients, literate in English, were invited to participate prior to admission for transplant if an adult family member was serving as a consistent caregiver through 100 days following transplant. If there was agreement to participate, the consent process was completed, and the patient and family caregiver completed baseline questionnaires.
Procedure
The PSE intervention was adapted from the Prepared Family Caregiver model specifically for individuals experiencing an allogeneic HSCT 31, 32. This model can be summarized in the acronym C.O.P.E: Creativity, Optimism, Planning, and Expert Information and includes the Home Care Guide outlining plans for common cancer problems. The C.O.P.E model, first administered to a group of patients with advanced cancer and their family caregivers 34, is aimed at empowering dyads to cope with cancer and cancer treatments using two major processes from the social problem-solving literature: Problem orientation and problem-solving skills.
The PSE sessions provided an opportunity to apply the problem-solving model, C.O.P.E., to an active problem identified by each dyad. The first session started with an introduction of the problem-solving model with each subsequent session including some degree of review appropriate to the dyad’s retention from the initial session. Once the problem-solving method was reviewed, the dyad had an opportunity to apply the C.O.P.E. method in the presence of the clinician interventionist. The clinician interventionist guided the dyad in the identification of a problem that was creating distress, review of the expert information or knowledge related to the problem, and the development of a plan to address the problem. An optimistic approach to managing the problem and permission to be creative was reinforced throughout the session.
Individualized dyadic PSE was provided by one of 3 clinicians with advanced degrees (clinical nurse specialist, nurse scientist and licensed independent clinical social worker) trained by a C.O.P.E expert, Matthew Loscalzo, MSW. The Principal Investigator took several measures to ensure the integrity and consistency of the intervention including: a script for the PSE session, peer supervision, and session audiotape to monitor for compliance with the script.
Measures
Data were collected with an interventionist log and subject interviews to address the primary objective. Session feasibility data were recorded by each clinician to include session attendance, session length and any reason for variation in the intervention. Subject feedback was collected for each individual session as well as for the intervention as a whole (exit interview) using a semi-structured interview that addressed issues affecting the ability to participate, satisfaction (1= least helpful; 5=most helpful), and application of the problem-solving strategy. All interviews were audio taped for transcription by a trained transcriber. A second transcriber completed quality monitoring on 100% of the tapes against the first transcription. The audio-tape data were also compared with the field notes to ensure data accuracy and completeness.
To address the secondary objectives, study questionnaires were completed by subjects as outlined by the study design and included the following:
Psychological Distress was measured with the Brief Symptom Inventory-18 (BSI-18). The BSI is a 18-item self-report measure that produces a global symptom index (GSI) 35. Each item is rated on a 5-point scale of distress (0–4), ranging from not at all (0) to extremely (4) with the GSI ranging from 0–72; higher scores indicate more psychological distress. Internal consistency reliability (Cronbach’s alpha) ranged from 0.71 – 0.74 in this study sample.
Problem Solving was measured by the Social Problem-Solving Inventory (SPSI-R). The SPSI-R is a 25-item self-report measure of cognitive, effective, and behavioral responses to real-life problem-solving situations 36. The measure yields a total score (0–20) with items scored on a 5-point scale ranging from not at all true of me (0) to extremely true of me (4). Higher scores represent more effective problem-solving ability. Internal consistency reliability (Cronbach’s alpha) ranged from 0.71 – 0.84 in this study sample.
Family Function was measured by the Family Adaptability and Cohesion Evaluation Scale (FACES IV). The FACES IV is a 62-item self-report measure that was developed in relation to the Circumplex Model 37. This measure yields the Circumplex Total Ratio (CTR) score with the higher the ratio score is above 1, the healthier the family system.
Symptom Distress was measured by the Symptom Distress Scale (SDS) 38. The SDS is a 13-item self-report measure presenting a list of 11 symptoms on which the patient rates distress (1=normal, no distress and 5=extensive distress). Higher scores indicate greater symptom distress. Internal consistency reliability (Cronbach’s alpha) ranged from 0.74 – 0.87 in this study sample.
Analysis
Descriptive statistics characterized the sample at baseline. To evaluate the feasibility of conducting the study intervention, data from the clinicians’ implementation log were summarized. Additional data relative to the feasibility of the study intervention were gathered from the transcripts of subjects’ interviews. These data included quantitative questions (e.g. on a scale of 1 – 5) as well as structured open-ended questions [e.g. What aspect of the session was most (and least) helpful?]. The quantitative responses were summarized with descriptive statistics. All qualitative responses, including the problems identified by each dyad, were analyzed to identify the themes, considering the choice and meaning of the words, and the context and consistency of responses. The principal investigator used qualitative computer software (NVivo, QSR International [Americas] Inc., Cambridge, MA) to index and cross-reference the thematic analysis 39.
Exploratory data analyses to address the secondary objectives of the study were performed separately for patients and family caregivers. The effect size for the intervention was computed using the first of the baseline scores on the SPSI-R and the BSI as the pre-test scores and scores at study end (6 weeks) for the post-test scores. A Spearman rho correlation coefficient was computed to explore the relationship between baseline psychological distress and baseline family functioning to the change in problem-solving skills. Descriptive statistics (mean and standard deviation) were used to describe the symptom experience (SDS) of subjects.
Results
Subject Demographic and Clinical Characteristics
Thirty-four dyads were screened for participation with 24 dyads ineligible due to non-English speaking (n=11), inconsistent family caregivers (n=10), inability to read English (n=1), family caregiver unavailability (n=1), or perceived burden (n=1). Ten dyads (n=20) were enrolled and eight (n=16) completed the intervention (Table 1). All dyads were husband and wife pairs. Incomplete study participation was due to patient death (n=1) and inconsistent responses (n=1). The initial in-patient admission (from HSCT to discharge) was a median of 14.5 (range 11–29) days. Sixty-three percent (n=5) of the patients required hospital re-admission during the study period for a median of 2 (range 1–34) days. The total hospital days, in-patient plus readmission days, revealed a median of 16 (range 12–63) days during the study period. Overall, subjects and caregivers reported a level of symptom distress suggesting low symptom burden (SDS scores <25) at all study time-points. Problems identified by the dyad fit into three categories: physical distress of the patient (e.g. fatigue, appetite, and sexual concerns), psychological distress of family caregivers (e.g. anxiety, role balance) and relationship challenges [e.g. communication (with the transplant team and each other), marital tension].
Table 1.
Sample Demographic and Clinical Characteristics
| Patient | Caregiver | |
|---|---|---|
| Age, Mean (SD) | 56.5 (7.93) | 53.9 (9.67) |
| n (%) | n (%) | |
| Gender, Male | 6 (75) | 3 (37.5) |
| Race/Ethnicity | ||
| White/non-Hispanic | 7 (87.5) | 7 (87.5) |
| White/Hispanic | 1(12.5) | 1 (12.5) |
| Married | 8 (100) | 8 (100) |
| Education | ||
| < High school | 1 (12.5) | ----- |
| High school graduate | 1 (12.5) | 2 (25.0) |
| Some college, no degree | 1 (12.5) | 2 (25.0) |
| Bachelor’s degree | 3 (37.5) | 2 (25.0) |
| Graduate/professional degree | 2 (25.0 | 2 (25.0) |
| Primary disease | ||
| AML | 1 (12.5) | ----- |
| CLL | 2 (25) | ----- |
| Non-Hodgkin’s disease | 4 (50) | ------ |
| Solid Tumor | 1 (12.5) | ----- |
| Type of transplant | ||
| Non-Myeloablative related | 6 (75) | ----- |
| Non-Myeloablative unrelated | 1 (12.5) | ----- |
| Myeloablative | 1 (12.5) | ----- |
| ECOG | ||
| 0 | 3 (37.5) | ----- |
| 1 | 4 (50) | ----- |
| 2 | 1 (12.5) | ----- |
Note: SD-standard deviation, AML-Acute Myelogenous Leukemia, CLL-Chronic Lymphocytic Leukemia, ECOG-Eastern Cooperative Oncology Group
Feasibility Outcomes
Of the thirty-one sessions scheduled, 29 were completed (94%) (Table 2). Worsening patient condition was the primary reason for sessions to be incomplete. Overall, patients attended 90% of the scheduled sessions; family caregivers attended 74%. Reasons for missed sessions included patient symptom distress and limited family caregiver availability (e.g. working). Limited caregiver availability was of greatest concern if the dyad had permanent residence in the vicinity and maintained their job during the transplant experience. Session length was a median of 45 (range 15 – 60) minutes with time decreasing over the trajectory of the study sessions.
Table 2.
Problem Solving Intervention: Session Characteristics
| PSE 1 | PSE 2 | PSE 3 | PSE 4 | |
|---|---|---|---|---|
| Visit Type, (na, %) | ||||
| In-patient | 5 (62.5%) | 6 (75.0%) | 4 (50.0%) | 1 (14.3%) |
| Out-patient | 3 (37.5%) | 2 (25.0%) | 4 (50.0%) | 6 (85.7%) |
| Length (minutes) | ||||
| (Mean, SD) | 47.8 (7.68) | 42.9 (6.36) | 40.0 (11.40) | 35.7 (11.34) |
| Satisfactionb (Mean, SD) | ||||
| Patient | 4.8 (0.71) | 4.8 (0.71) | 5.0 (0.0) | 4.7 (0.82) |
| Caregiver | 4.6 (0.74) | 5.0 (0.0) | 5.0 (0.0) | 4.6 (0.89) |
| Attendance (n, %) | ||||
| Patient | 7 (87.5%) | 8 (100%) | 6 (75.0%) | 7 (100%) |
| Caregiver | 8 (100%) | 7 (87.5%) | 4 (50.0%) | 4 (57.1%) |
Note: PSE-Problem-Solving Education session; SD-Standard Deviation
n=7 dyads at time 4;
Range 1 = not satisfied to 5 = very satisfied
Sessions were provided in the in-patient and out-patient settings depending on the patient’s clinical course. The PSE sessions were scheduled in advance to accommodate the dyad and the clinician, however, if only one member arrived, the intervention was still administered. There were two sessions scheduled where both dyad members did not arrive and rescheduling was not an option. Appointments were often adjusted throughout the duration of the study for reasons that were primarily associated with the clinical course of the patient. However, rescheduling was only considered if the dyad and the clinician were available within the constraints of the study design (e.g. during scheduled week) without additional burden to the dyad (e.g. additional trip to the hospital) or the clinician (e.g. conflicting patient or program priorities). Clinicians reported the scheduling of the PSE sessions as the greatest challenge.
Subjects rated their satisfaction with each session (Table 2) as well as the overall program. Dyads reported being very satisfied with the individual sessions with those closest to the initial discharge (PSE #2 & #3) receiving the highest satisfaction scores. Data from the interviews identified three major categories of benefit that were labeled based on subject quotes: “an opportunity to talk”, “expert information”, and “creative thinking”. The major categories that identified components that were perceived as least helpful included “survey completion” and the length and repetitiveness of the “home care guide” which included content similar to the UCE.
The overall program evaluation focused on the appropriate number of sessions, use of problem-solving strategies, the home care guide, and overall helpfulness of the intervention. The majority (75%) of subjects (n = 16) present for the exit interview reported the number of sessions as just right. One “would have liked fewer [sessions]” while two subjects (one dyad) responded “not useful at all”. Family caregivers reported the problem-solving strategies as slightly more helpful (M = 4.5±1.8) than did patients (M = 4.4±1.5), but reported the home care guide as least helpful (M = 3.8 ± 1.9 vs. 4.3±1.0, respectively). Overall, subjects reported that the program was very helpful with family caregivers giving a slightly higher score compared to the patients (M = 5.0±0 vs. 4.5±0.5, respectively).
Study Intervention Effect
Outcome data collected from subjects across the study time-points are reported in Table 3. Subjects completed two surveys prior to PSE #1, pre- and post- the admission education class. Because the SPSI-R scores at these two time-points did not differ for the patients [t=−1.778(6), p=0.126] or family caregivers [t =−0.510(7), p =0.626], the first baseline scores were used to estimate the effect size (ES). The ES for problem-solving skill was larger for patients (ES =0.324, M =16.48±1.49 vs. 17.02±2.4) as compared to the family caregivers (ES =0.067, M =14.18±2.7 vs. 14.09±2.6). Subjects’ SPSI-R mean scores were within the normative group range, suggesting an ability to solve problems effectively prior to the study intervention. Similarly, the BSI-18 scores did not significantly differ between the two baseline time-points [patient t= 0.834(6), p=0.436 or family caregivers [t=1.183(7), p=0.275], therefore, the first baseline scores were used to estimate the ES. The effect size for caregiver distress was small (ES =0.128, M =5.1±3.8 vs. 4.7±3.3) with scores slightly lower following the intervention. For the patients, the ES was larger (ES=0.508, M = 5.7±2.1 vs. 8.4±5.3) with scores slightly higher following the intervention period.
Table 3.
Descriptive Data for Measures across Study Time-Points
| Pre-UCE Baseline |
Post-UCE Baseline |
Discharge | Week 2 | Week 6 | |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| BSI | |||||
| Patient | 5.5 (5.2) | 3.4 (1.7)* | ----- | ----- | 8.4 (5.3)* |
| Family caregiver | 5.6 (3.8) | 6.6 (5.0) | ----- | ----- | 4.7 (3.3)* |
| SPSI-R | |||||
| Patient | 16.5 (1.5)* | 17.1 (1.8)* | 16.4 (2.8) | 16.4 (3.0) | 16.4 (2.9) |
| Family caregiver | 14.2 (2.7) | 14.4 (2.7) | 13.8 (3.0) | 14.1 (2.9) | 14.1 (2.7) |
| FACES-IV | |||||
| Patient | 2.6 (0.8) | ----- | ----- | ----- | ----- |
| Family caregiver | 2.4 (0.5) | ----- | ----- | ----- | ----- |
| SDS | |||||
| Patient | 21.9 (6.5) | 19.3 (5.5)* | 24.1 (5.1) | 22.9 (6.0) | 23.9 (8.6) |
| Family caregiver | 22.1 (3.4) | 20.5 (4.7) | 21.6 (4.4) | 20.6 (5.0) | 20.9 (4.4) |
Note: N=8 (patients); N=8 (family caregiver); UCE = Usual Care Education; SD=Standard Deviation; BSI-Brief Symptom Inventory; SPSI-R-Social Problem-Solving Inventory-Revised; FACES IV-Family Adaptability and Cohesion Evaluation Scale; SDS-Symptom Distress Scale.
n=7
Relationship with Baseline Factors
Relationships of baseline distress (BSI) and family function (FACES-IV ratio scores) to the change in SPSI-R scores (pre-post intervention) also were explored. Only patient baseline distress was related to the change in SPSI-R scores (rs =0.80, p = 0.031). Neither baseline family caregiver distress or family caregiver and patient family function were related to the change in SPSI-R scores. At baseline, the majority of patients (88%) and all family caregivers scored within the normal range for distress with one patient considered a “case” for depression. All subjects were classified as “healthy” relative to family function.
Discussion
The results from this pilot study suggest, despite the complexities of the early phase of recovery, it is feasible to administer a problem-solving education intervention to adults undergoing allogeneic HSCT and their family caregivers. Dyads reported that the “transplant process carries a lot of uncertainty” therefore the successful implementation of an education intervention into an acute clinical environment can seem daunting. However, providing the session during a scheduled hospital visit added to the convenience for the dyads and permitted 90% attendance of the sessions with high levels of program satisfaction. This came at a cost to the clinicians who serve as study interventionists in addition to the full-time professional positions in the hospital. Despite the scheduling challenges, the length of the intervention was maintained as projected by the study team. No session exceeded 60 minutes which was considered a reasonable amount of time based on other educational forums well tolerated by cancer patients.
Although the implementation of the intervention was considered feasible, the accrual experience from this study provides guidance to improve the study intervention for future research. The caregiving process during allogeneic HSCT is not limited to a spouse as the sole caregiver. Therefore the caregiving network should be further defined and interventions that provide potential benefit to all those actively caregiving should be pursued40. This will challenge the research team to consider alternative ways to involve individuals who have competing priorities such as work, or are not in the vicinity until further along in the transplant trajectory. However, the effort to capture this reality of the allogeneic HSCT caregiving experience is essential. In addition, an awareness of the cultural diversity in our healthcare system demands consideration of this factor in our research. The limitations to this end include both human (e.g. bilingual investigators) and fiscal (e.g. funding for translation of measures) resources leaving the knowledge relative to the feasibility and ultimately the efficacy of a clinical intervention incomplete. Harmonizing the research on transplant caregivers with the reality of the experience will improve our ability to translate findings from intervention research into the clinical setting.
The number of sessions appropriate during the acute transplant period is less clear. The majority of the subjects reported there were “an appropriate number of sessions”, however less time to complete progressive sessions and decreasing participation suggests fewer sessions may be appropriate. Data suggest that discharge from the hospital, a time when the dyad is preparing to independently manage many aspects of the recovery experience, is when the education was most meaningful. Therefore the number of sessions may be less important if the timing of each session is meaningful in the context of the transplant trajectory (e.g. time of discharge).
The components of the intervention that determine its meaning were best elucidated by the dyad. Subjects described the COPE method as a “broad problem-solving structure” that “translates [problems] into something that’s useful”. “Going through a list of things with another mind [helped] come up with ideas…things I hadn’t thought of”. This active process of solving the identified problem is guided by the clinician and discourages avoidance coping which is associated with higher levels of distress in caregivers 16, 41, 42. Additionally, a more active strategy involving “taking control” is associated with longer survival in HSCT patients 43. Overall, subjects reported that “sitting down and talking [about a problem]” “forced us to have communication [with each other]” and “exchange views”. This dyadic communication encourages collaborative coping which can improve psychological outcomes 44. In contrast, the study material (Home Care Guide) was perceived as less beneficial and might be improved if limited to a concise summary of the problem-solving methodology; the C.O.P.E. method.
Although the overall perception of patients and family caregivers suggested a benefit from the intervention, the impact on problem-solving skills and distress was small. In the patient group, there was a small improvement in problem-solving skills which suggests benefit. However, the family caregiver group demonstrated almost no change with a slight decrease in the post intervention score. This finding is likely the result of a small sample size as well as the higher level of problem-solving skill in this sample suggesting that all subjects were effective problems solvers prior to the intervention. A ceiling effect with the SPSI-R also deserves consideration since other cancer populations have also been deemed “effective problemssolvers”41, 42, 45. Therefore, problem-solving skill (SPSI-R) as the primary outcome may need to be re-evaluated along with consideration to an adequate sample size for the variability within selected measures.
Previous work suggests that individuals with higher levels of distress may have greater benefit from a problem-solving intervention 46 which was supported by these results. Subjects in this study with a higher level of distress at baseline were found to experience improvement in problem- solving skills post PSE. Despite this potential benefit relative to problem-solving skills, patients reported a moderate increase in their distress level following the intervention. On the other hand, family caregivers reported a slight improvement in their scores which supports their report of benefit. In this sample, the symptom burden of the patients was also low which may reflect fewer problems contributing to distress 47.
These findings relative to effect size and baseline distress and problem-solving skills of the sample provides guidance for the determination of sample size during the design of future research involving problem solving education. First, the overall effect size for improvement in problem solving skills and distress is likely small and varies between patients and family caregivers. Concerns about the small effect sizes for psychosocial outcomes are well documented following psychosocial interventions 48; however, potential moderators that influence outcomes are less well studied 49. In the setting of HSCT potential moderators include the timing of the intervention, the type/number of participants (e.g. family members), the acuity of the HSCT patient, and the provider of the intervention. In addition, self-efficacy has been documented to improve following interventions directed at helping cancer 50 and non-cancer 51, 52 caregivers which might influence the intervention’s effect on distress.
The results of this pilot study must be considered in light of two major limitations: small sample size and the number and selection of measures administered. First, the sample size was determined based on the primary objective, intervention feasibility, therefore the findings associated with the secondary objectives (e.g. effect sizes) may be the result of the small sample size and should be tested in a study designed specifically for this purpose. In addition, because of the small sample, the number of meaningful exploratory analyses to evaluate how subgroups such as patients and family caregivers responded was difficult. Second, although the constructs determined appropriate for this study were based on previous research, their application in this population is not well understood. In addition, since the effects of allogeneic HSCT is complex, additional constructs to assess these multidimensional effects should be further explored and systematically balanced with the sample size to allow for a comprehensive analysis.
Research Implications
Despite the sample size limitation, the results of this pilot study can inform future research on problem-solving education for transplant recipients and their caregiver(s). Findings suggest that changes in intervention implementation should be considered to improve overall participation and strengthen the educational process specific to the C.O.P.E method of problem solving. First, offer the intervention to all caregivers identified pre-transplant, rather than a single caregiver, a change which might require telephone conference calling or other technology resources to address distance learning and involvement 53. Second, decrease the number of early sessions and consider focusing on the time of discharge. Caregiver and patient participants in this study reported that the first intervention session (pre-HSCT) was least helpful due to more imminent concerns related to the patient’s admission and transplant procedure. Third, provide materials that are specific to the C.O.P.E method of problem-solving rather than comprehensive materials that were reported by both caregiver and patient participants to be duplicative and cumbersome. One dyad reported that it would be helpful to have a pocket-sized resource to carry with them as a reminder of C.O.P.E. Finally, consider including measures that: 1) offer alternative outcomes such as patient and caregiver self-efficacy and 2) expand our understanding of additional factors such as patient acuity that might influence patient and caregiver outcomes.
Conclusion
The acute phase of allogeneic HSCT is plagued with competing clinical priorities and high levels of uncertainty. A caregiver is therefore required to not only be available to the patient but to actively participate in their care. The negative consequence of this burden to the family caregivers is recognized while the consequences of an unprepared or distressed caregiver on the patient are not well understood. Targeted interventions that promote effective, meaningful behaviors are needed to guide patients and caregivers through this treatment experience together. A successful process of education for patients and family caregivers can increase confidence and trust in care, 10 and improve overall adaptation 16.
Acknowledgments
The authors thank the following individuals for their assistance in recruitment of participants: Laura Musse, Michael Krumlauf, and Rose Goodwin. The authors are grateful to the following physicians for supporting this study: Drs John Barrett, Richard Childs, Daniel Fowler, and Michael Bishop. In addition, the authors are indebted to Gwenyth Wallen for her guidance and invaluable feedback on the manuscript. We also acknowledge the funding by the Intramural Research Program of the NIH, Clinical Center.
Reference List
- 1.Tabbara IA, Zimmerman K, Morgan C, Nahleh Z. Allogeneic hematopoietic stem cell transplantation: Complications and results. Arch Intern Med. 2002;162(14):1558–1566. doi: 10.1001/archinte.162.14.1558. [DOI] [PubMed] [Google Scholar]
- 2.Bevans MF, Mitchell SA, Marden S. The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT) Support Care Cancer. 2008;16(11):1243–1254. doi: 10.1007/s00520-008-0420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurtz ME, Kurtz JC, Given C, Given B. Effects of a symptom control intervention on utilization of health care services among cancer patients. Med Sci Monit. 2006;12(7):319–324. [PubMed] [Google Scholar]
- 4.Grant M, Cooke L, Bhatia S, Forman SJ. Discharge and unscheduled readmissions of adult patients undergoing hematopoietic stem cell transplantation: Implications for developing nursing interventions. Oncol Nurs Forum. 2005;32(1):E1–E8. doi: 10.1188/05.onf.e1-e8. [DOI] [PubMed] [Google Scholar]
- 5.Pallera AM, Schwartzberg LS. Managing the toxicity of hematopoietic stem cell transplant. J Support Oncol. 2004;2(3):223–237. [PubMed] [Google Scholar]
- 6.Fife BL, Huster GA, Cornetta KG, Kennedy VN, Akard LP, Broun ER. Longitudinal study of adaptation to the stress of bone marrow transplantation. J Clin Oncol. 2000;18(7):1539–1549. doi: 10.1200/JCO.2000.18.7.1539. [DOI] [PubMed] [Google Scholar]
- 7.Foster LW, McLellan LJ, Rybicki LA, Sassano DA, Hsu A, Bolwell BJ. Survival of patients who have undergone allogeneic bone marrow transplantation: The relative importance of in-hospital lay care-partner support. J Psychosoc Oncol. 2004;22(2):1–20. [Google Scholar]
- 8.Frey P, Stinson T, Siston A, et al. Lack of caregivers limits use of outpatient hematopoietic stem cell transplant program. Bone Marrow Transplant. 2002;30(11):741–748. doi: 10.1038/sj.bmt.1703676. [DOI] [PubMed] [Google Scholar]
- 9.Weaver C, Schiech L, Held-Warmkessel J, et al. Risk for unplanned hospital readmission of patients with cancer: results of a retrospective medical record review. Oncol Nurs Forum. 2006;33(3):E44–E52. doi: 10.1188/06.ONF.E44-E52. [DOI] [PubMed] [Google Scholar]
- 10.Griffiths BA. Needs of patients and families undergoing autologous peripheral blood stem cell transplantation. Can Oncol Nurs J. 2005;15(3):151–160. doi: 10.5737/1181912x153151155. [DOI] [PubMed] [Google Scholar]
- 11.Grimm PM, Zawacki KL, Mock V, Krumm S, Frink BB. Caregiver responses and needs: An ambulatory bone marrow transplant model. Cancer Pract. 2000;8(3):120–128. doi: 10.1046/j.1523-5394.2000.83005.x. [DOI] [PubMed] [Google Scholar]
- 12.Stetz KM, McDonald JC, Comptom K. Needs and experiences of family caregivers during marrow transplantation. Oncol Nurs Forum. 1996;23(9):1422–1427. [PubMed] [Google Scholar]
- 13.Siston AK, List MA, Daugherty CK, et al. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001;27(11):1181–1188. doi: 10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- 14.Langer S. Mood disturbance in the cancer setting: Effects of gender and patient/spouse role. Semin Clin Neuropsychiatry. 2003;8(4):276–285. [PubMed] [Google Scholar]
- 15.Keogh F, O'Riordan J, McNamara C, Duggan C, McCann SR. Psychosocial adaptation of patients and families following bone marrow transplantation: A prospective, longitudinal study. Bone Marrow Transplant. 1998;22(9):905–911. doi: 10.1038/sj.bmt.1701443. [DOI] [PubMed] [Google Scholar]
- 16.Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplant. doi: 10.1038/bmt.2008.405. In press. [DOI] [PubMed] [Google Scholar]
- 17.Carter PA, Acton GJ. Personality and coping: predictors of depression and sleep problems among caregivers of individuals who have cancer. J Gerontol Nurs. 2006;32(2):45–53. doi: 10.3928/0098-9134-20060201-11. [DOI] [PubMed] [Google Scholar]
- 18.Foxall MJ, Gaston-Johansson F. Burden and health outcomes of family caregivers of hospitalized bone marrow transplant patients. J Adv Nurs. 1996;24(5):915–923. doi: 10.1111/j.1365-2648.1996.tb02926.x. [DOI] [PubMed] [Google Scholar]
- 19.Harding R, Higginson IJ. What is the best way to help caregivers in cancer and palliative care? A systematic literature review of interventions and their effectiveness. Palliat Med. 2003;17(1):63–74. doi: 10.1191/0269216303pm667oa. [DOI] [PubMed] [Google Scholar]
- 20.Devine EC, Westlake SK. The effects of psychoeducational care provided to adults with cancer: Meta-analysis of 116 studies. Oncol Nurs Forum. 1995;22(9):1369–1381. [PubMed] [Google Scholar]
- 21.Meyer TJ, Mark MM. Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychol. 1995;14(2):101–108. doi: 10.1037//0278-6133.14.2.101. [DOI] [PubMed] [Google Scholar]
- 22.Sheard T, Maguire P. The effect of psychological interventions on anxiety and depression in cancer patients: Results of two meta-analyses. Br J Cancer. 1999;80(11):1770–1780. doi: 10.1038/sj.bjc.6690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen M, Kuten A. Cognitive-behavior group intervention for relatives of cancer patients: A controlled study. J Psychosom Res. 2006;61(2):187–196. doi: 10.1016/j.jpsychores.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Cimprich B, Janz NK, Northouse LL, Wren PA, Given B, Given C. Taking charge: A self-management program for women following breast cancer treatment. Psychooncology. 2005;14(9):707–717. doi: 10.1002/pon.891. [DOI] [PubMed] [Google Scholar]
- 25.Nezu AM, Nezu CM, Houts PS, Friedman SH, Faddis S. Relevance of problem-solving therapy to psychosocial oncology. J Psychosoc Oncol. 1999;16(3–4):5–26. [Google Scholar]
- 26.Lazarus R, Folkman S. Stress, Appraisal, and Coping. New York, NY: Macmillan Publishers Limited; 1984. [Google Scholar]
- 27.Arean PA, Perri MG, Nezu AM, Schlossman RL, Cirera E, Kaasa S. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatment for depression in older adults. J Consult Clin Psychol. 1993;61(6):1003–1010. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- 28.Nezu AM. Efficiacy of a social problem-solving theray approach for unipolar depression. J Consult Clin Psychol. 1986;54(2):196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- 29.Nezu AM, Perri MG. Social problem-sovling therapy for unipolar depression: An initial dismantling study. J Consult Clin Psychol. 1989;57(3):408–413. [PubMed] [Google Scholar]
- 30.Nezu CM, Nezu AM, Arean PA. Assertiveness and problem-solving therapy for mildly mentally retarded persons with dual diagnoses. Res Dev Disabil. 1991;12(4):371–386. doi: 10.1016/0891-4222(91)90033-o. [DOI] [PubMed] [Google Scholar]
- 31.Houts PS, Nezu AM, Nezu CM, Bucher JA. The prepared family caregiver: A problem-solving approach to family caregiver education. Patient Educ Couns. 1996;27(1):63–73. doi: 10.1016/0738-3991(95)00790-3. [DOI] [PubMed] [Google Scholar]
- 32.Loscalzo MJ, Bucher JA. The COPE model: Its clinical usefulness in solving pain-related problems. J Psychosoc Oncol. 1999;16(3–4):93–117. [Google Scholar]
- 33.McMillan SC, Small BJ, Weitzner M, et al. Impact of coping skills intervention with family caregivers of hospice patients with cancer: A randomized clinical trial. Cancer. 2006;106(1):214–222. doi: 10.1002/cncr.21567. [DOI] [PubMed] [Google Scholar]
- 34.Bucher JA, Loscalzo M, Zabora J, Houts PS, Hooker C, Brintzenhofeszoc K. Problem-solving cancer care education for patients and caregivers. Cancer Pract. 2001;9(2):66–70. doi: 10.1046/j.1523-5394.2001.009002066.x. [DOI] [PubMed] [Google Scholar]
- 35.Derogatis LR. Brief Symptom Inventory (BSI) administration, scoring, and procedures manual. 3rd ed. Minneapolis, MN: National Computer Systems; 1994. [Google Scholar]
- 36.D'Zurilla TJ, Nezu AM, Maydeau-Olivares AM. Social Problem Solving Inventory-Revised. North Tonawanda, NY: Multi-Health Systems Inc; 2002. [Google Scholar]
- 37.Olson DH, Gorall DM, Tiesel JW. FACES IV Package: Administration Manual. Minneapolis, MN: Life Innovations; 2006. [Google Scholar]
- 38.McCorkle R, Cooley ME, Shea JA. A user's manual for the Symptom Distress Scale. Philadelphia, PA: University of Pennsylvania; 1998. [Google Scholar]
- 39.Morgan DL. Computerized analysis. In: Krueger RA, editor. Analyzing & reporting focus groups. Thousand Oaks, CA: Sage Publications, Inc; 1998. pp. 89–93. [Google Scholar]
- 40.Case P. Social opportunity in the face of cancer: Understanding the burden of the extended caregiver network. Illn Crisis Loss. 2006;14(4):299–318. [Google Scholar]
- 41.Ko CM, Malcarne VL, Varni JW, et al. Problem-solving and distress in prostate cancer patients and their spousal caregivers. Support Care Cancer. 2005;13(6):367–374. doi: 10.1007/s00520-004-0748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malcarne VL, Banthia R, Varni JW, Sadler GR, Greenbergs HL, Ko CM. Problem-solving skills and emotional distress in spouses of men with prostate cancer. J Cancer Educ. 2002;17(3):150–154. doi: 10.1080/08858190209528823. [DOI] [PubMed] [Google Scholar]
- 43.Grulke N, Bailer H, Chele H, Bunjes D. Psychological distress of patients undergoing intensified conditioning with radioimmunotherapy prior to allogeneic stem cell transplantation. Bone Marrow Transplant. 2005;35(11):1107–1111. doi: 10.1038/sj.bmt.1704971. [DOI] [PubMed] [Google Scholar]
- 44.Berg CA, Wiebe DJ, Butner J, et al. Collaborative coping and daily mood in couples dealing with prostate cancer. Psychol Aging. 2008;23(3):505–516. doi: 10.1037/a0012687. [DOI] [PubMed] [Google Scholar]
- 45.Hawes SM, Malcarne VL, Ko CM, et al. Identifying problems faced by spouses and partners of patients with prostate cancer. Oncol Nurs Forum. 2006;33(4):807–814. doi: 10.1188/06.ONF.807-814. [DOI] [PubMed] [Google Scholar]
- 46.Toseland RW, Blanchard CG, McCallion P. A problem solving intervention for caregivers of cancer patients. Soc Sci Med. 1995;40(4):517–528. doi: 10.1016/0277-9536(94)e0093-8. [DOI] [PubMed] [Google Scholar]
- 47.Given B, Given CW, Sikorskii A, Jeon S, Sherwood P, Rahbar M. The impact of providing symptom management assistance on caregiver reaction: Results of a randomized trial. J Pain Symptom Manage. 2006;32(5):433–443. doi: 10.1016/j.jpainsymman.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 48.Coyne JC, Lepore SJ, Palmer SC. Efficacy of psychosocial interventions in cancer care: Evidence is weaker than it first looks. Ann Behav Med. 2006;32(2):104–110. doi: 10.1207/s15324796abm3202_5. [DOI] [PubMed] [Google Scholar]
- 49.Zimmermann T, Heinrichs N, Baucom DH. "Does one size fit all?" Moderators in psychosocial interventions for breast cancer patients: A meta-analysis. Ann Behav Med. 2007;34(3):225–239. doi: 10.1007/BF02874548. [DOI] [PubMed] [Google Scholar]
- 50.Northouse LL, Mood DW, Montie JE, et al. Living with prostate cancer: Patients' and spouses' psychosocial status and quality of life. J Clin Oncol. 2007;25(27):4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- 51.Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW. A randomized, controlled trial of a home environmental intervention: Effect on efficacy and upset in caregivers and on daily function of persons with dementia. Gerontologist. 2001;41(1):4–14. doi: 10.1093/geront/41.1.4. [DOI] [PubMed] [Google Scholar]
- 52.Gitlin LN, Winter L, Burke J, Chernett N, Dennis MP, Hauck WW. Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: a randomized pilot study. Am J Geriatr Psychiatry. 2008;16(3):229–239. doi: 10.1097/JGP.0b013e318160da72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chelf JH, Agre P, Axelrod A, et al. Cancer-related patient education: an overview of the last decade of evaluation and research. Oncol Nurs Forum. 2001;28(7):1139–1147. [PubMed] [Google Scholar]