Abstract
Objective
Dizziness presentations pose many clinical challenges. The objective of this study is to broadly summarize the evidence base that supports clinical decisions in dizziness presentations.
Methods
MEDLINE (1966 to September 2007), Web of Science, and The Cochrane Library were searched for articles with clinical relevance on topics concerning dizziness. Additional sources were also searched for clinical practice guidelines. The following information was abstracted from each article: year of publication, journal type, type of article, and the topics of the article.
Results
Of nearly 3000 articles identified, 1244 articles met the inclusion criteria. The most common article type was a case report or case series, followed by expert opinion or review articles, studies of medical tests, and clinical trials. Meta-analyses and systematic reviews were found on benign paroxysmal positional vertigo and Meniere’s disease, but only a few other topics. No clinical practice guidelines were found that focus specifically on dizziness.
Conclusions
The evidence base for the evaluation and management of dizziness seems to be weak. Future work to establish or summarize evidence in clinically meaningful ways could contribute to efforts to optimize patient care and healthcare utilization for one of the most common presenting symptoms.
Keywords: Dizziness, vertigo, evaluation, management, evidence-based medicine
Introduction
Physicians are often faced with difficult decisions when evaluating and managing patients with dizziness. Diagnosing a specific cause can be a challenge since the symptom descriptions are often vague and examination findings overlap among potential causes.1–3 Once a differential diagnosis is formulated, it is not clear what tests – if any – will add clinical value.4–7 Finally, decisions about therapies must weight potential benefit against potential harm.
Evidence-based medicine guides clinical decision-making by integrating the best research evidence with clinical expertise.8 The main platform for evidence-based medicine is the medical literature. In the current study, we sought to take a “30,000 foot view” of the medical literature to broadly describe the evidence base for the evaluation and management of dizziness; a common9, 10 condition for which concerns regarding effectiveness and quality of care exist.11–13 This type of broad investigation is an important early step in the efforts to optimize patient care and healthcare utilization.
Methods
Search Strategies
With the help of a medical librarian, the English language literature was searched for articles on the topic of dizziness from 1966 through September 27, 2007, using MEDLINE and Web of Science. The MEDLINE database was searched using two search sets of Medical Subject Heading (MeSH) terms that were exploded and then combined: 1] dizziness, vestibular diseases, and gait disorders, neurologic; and 2] physical examination, disease attributes, diagnosis, randomized controlled trials, decision support techniques, and sensitivity and specificity. These two sets were limited to humans and English language, then combined by AND. The search was limited to case reports, classical articles, clinical conferences, clinical trials, comparative studies, consensus development conferences, evaluation studies, guidelines, meta-analyses, multi-center studies, review, or validation studies. Web of Science was searched by using two search sets: 1] dizziness, vertigo, and imbalance; and 2] examination, diagnosis, disease attribute, randomized controlled trial, decision rule, and sensitivity and specificity. The two Web of Science search sets were then combined by AND. The Cochrane Library was also searched for systematic reviews using dizziness, vertigo, or imbalance as search terms. Relevant clinical guidelines were sought using the following sources: National Guideline Clearinghouse, the American College of Physicians Clinical Practice Guidelines, the Agency for Healthcare Research and Quality (AHRQ) Clinical Practice Guidelines Online, the Department of Veterans Affairs Clinical Practice Guidelines, the American Academy of Neurology Practice Guidelines & Tools, and the American Academy of Otolaryngology – Head and Neck Surgery.
Study selection
We included studies with clinical relevance for patients with dizziness. Articles were excluded when the principal topic was syncope, falling, the auditory system, surgical approaches, or surgical outcomes.
Data abstraction & analysis
Abstracts of all relevant articles were reviewed and data were extracted by one author (KAK) into a database that included the following: first author, year of publication, journal name, journal type (e.g., otolaryngology, neurology, general medicine, other), type of article, and up to three clinical topics. Standard definitions of study design were used to classify each article type.14 Articles were classified as a study of a medical test whenever the objective was to investigate the clinical usefulness of a test – ranging from phase I studies of medical tests (i.e., case-control design) to phase IV studies of medical tests (i.e., randomized controlled trial design with the test considered to be the intervention).15 The categories of clinical topics included both specific disorders (e.g., benign paroxysmal positional vertigo [BPPV], Meniere’s disease, cerebrovascular disease) and also broader categories such as general dizziness presentation. Descriptive statistics were used to summarize the findings.
Results
A total of 2966 articles were identified by the search. After review, 1244 met inclusion criteria. More than half (55%) of all identified articles were published in otolaryngology specialty journals. An additional 21% of articles were published in neurology specialty journals. Only 10% of articles were published in the general medical literature. The remaining 14% of articles were published in other specialty journals.
Types of articles
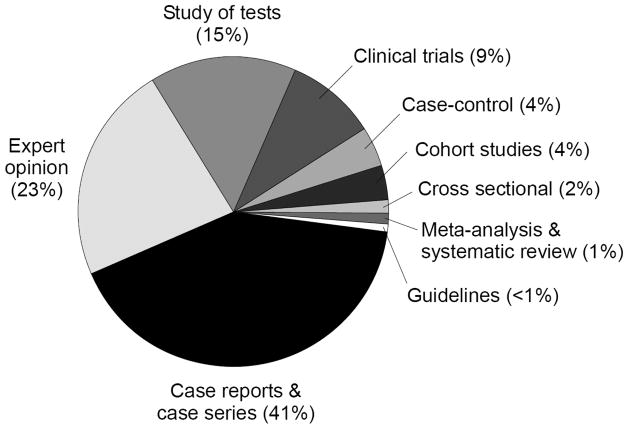
The distribution of article types is shown in the Figure. Case report/series (41%) and expert opinion/review articles (23%) were the most common types of articles identified. Clinical trials comprised 9% of the articles. Meta-analyses/systematic reviews (1%) and guideline statements (<1%) were the least commonly identified.
Figure.
Distribution of article type for clinically relevant article pertaining to dizziness. (Total articles, 1244)
Topics of articles
General dizziness presentation was the most common topic (32%) (Appendix). The most common specific disorder topics were benign paroxysmal positional vertigo (13%), cerebrovascular disease (8%), and Meniere’s disease (5%). Among clinical trials, BPPV was the most common topic. Cerebrovascular disease was the most common specific topic of case reports or case series. Most studies of diagnostic tests evaluated vestibular tests (e.g., electronystagmography, rotational chair testing, posturography).
Appendix.
Types of articles for various dizziness topics (Total 1244)
| Clinical trials (n= 115) | Cohort studies (n= 44) | Case-control studies (n= 54) | Cross-sectional studies (N=20) | Case report & case series (n=512) | Study of tests (n=192) | Expert opinion (n=285) | Meta-analysis & systematic review (n= 14) | Guidelines (n= 8) | |
|---|---|---|---|---|---|---|---|---|---|
| Clinical Topic | |||||||||
| Peripheral vestibular | |||||||||
| BPPV | 44 | 14 | 14 | 1 | 70 | 17 | 19 | 3 | – |
| Vestibular neuritis | 6 | 6 | 4 | – | 11 | 7 | 6 | – | – |
| Meniere’s disease | 6 | 5 | 5 | 2 | 19 | 16 | 18 | 3 | 1 |
| Acoustic Neuroma | – | 1 | – | – | 28 | 2 | 1 | – | 1 |
| Vestibular fistula | 1 | 2 | – | – | 36 | 4 | 10 | – | |
| Other PV | 16 | 4 | 6 | – | 84 | 37 | 26 | – | 1 |
| Central nervous system | |||||||||
| Cerebrovascular | 3 | 1 | 6 | 3 | 87 | 10 | 7 | 1 | 1 |
| CNS tumor | – | – | – | – | 13 | – | – | – | – |
| Multiple sclerosis | – | – | – | – | 9 | 2 | 4 | – | – |
| Ataxia syndrome | – | – | – | – | 14 | 2 | 3 | – | – |
| Chiari malformation | – | – | – | – | 7 | – | – | – | – |
| Other CNS | 1 | 1 | 1 | – | 31 | 4 | 4 | – | – |
| Migraine | 2 | 3 | 4 | 1 | 30 | 6 | 12 | – | – |
| General medical | – | 1 | 7 | 2 | 42 | 1 | 9 | – | – |
| Psychiatric | 2 | 4 | 7 | 1 | 7 | 2 | 8 | – | – |
| Cervicogenic | 2 | – | – | – | – | 2 | 3 | 1 | – |
| Trauma | 2 | 1 | 2 | – | 14 | 3 | 4 | – | – |
| General Presentations | 38 | 13 | 16 | 13 | 116 | 94 | 159 | 4 | 1 |
| Tests | |||||||||
| Vestibular tests | 132 | 1 | 2 | ||||||
| Audiogram | 4 | – | – | ||||||
| Imaging | 20 | 1 | 1 | ||||||
| History & physical exam | 26 | – | – | ||||||
| Other tests | 17 | – | – |
BPPV = benign paroxysmal positional vertigo; PV = peripheral vestibular; CNS = central nervous system
Meta-analyses & Systematic reviews
Six meta-analyses were found (Table 1), four of which assessed the effects of an intervention.16–19 Three of the meta-analyses assessed the efficacy of the canalith repositioning maneuver for treatment of BPPV.17–19 Of the articles that did not assess a treatment intervention, one was on the topic of posturography20 and the other reported on the prevalence of dizziness symptoms and cerebellopontine angle mass lesions.20 Eight systematic reviews were found; five of these assessed the effects of an intervention (Table 1).21–25 The reviews that did not assess an intervention were on the following topics: accuracy and reliability of symptoms and findings on neurological examination in patients with suspected stroke or transient ischemic attacks (dizziness was a minor topic),26 causes of vertigo in the primary care setting,27 and the etiology, prognosis, and diagnostic evaluation of dizziness.28
Table 1.
Meta-analyses, systematic reviews, and guidelines pertaining to dizziness evaluation and management.
| Publication Category | First author (or organization), year | Clinical topic | Intervention | Conclusion or comment |
|---|---|---|---|---|
| Meta-analyses | ||||
| Schneider, 2005 | General dizziness presentation | Vertigoheel | Treatment non-inferior to control group therapies. | |
| Woodworth, 2004 | BPPV | Canalith repositioning maneuver | Evidence supports efficacy of maneuver. | |
| Hilton, 2004 | BPPV | Canalith repositioning maneuver | Evidence supports that the maneuver is a safe and effective treatment. | |
| Hilton, 2002 | BPPV | Canalith repositioning maneuver | Evidence supports that the maneuver is a safe and effective treatment. | |
| Systematic reviews | ||||
| Thirlwall, 2006 | Meniere’s disease | Diuretics | Insufficient evidence to determine the efficacy. | |
| Reid, 2005 | Cervicogenic vertigo | Manual therapy | Insufficient evidence to determine the efficacy. | |
| James, 2006 | Meniere’s disease | Medical treatment, dietary changes, & physical therapy | Either no evidence or insufficient evidence to determine efficacy. | |
| Wayne, 2004 | Vestibulopathy | Tai Chi | Insufficient evidence to determine the efficacy. | |
| James, 2001 | Meniere’s disease | Betahistine | Insufficient evidence to determine the efficacy. | |
| Guidelines | ||||
| Institutes for Clinical Systems Improvements, 2006 & 2007 | Ischemic stroke | General evaluation and management | Vestibular neuritis briefly addressed as a stroke mimicker. | |
| Multi-specialty expert panel, 2007 | Herpes Zoster (Ramsay-Hunt Syndrome) | Anti-viral and corticosteroid therapy. | Anti-viral therapy is recommended. Corticosteroids can be considered. | |
| American College of Radiology Committee, 2006 | Imaging | NA | Guide for choice of imaging study in various clinical scenarios. | |
| European Federation of Neurological Societies, 2004 | Nystagmus and oscillopsia | General management | Numerous recommendations for treatment made. | |
| American Academy of Neurology, 2000 | Vestibular testing techniques | NA | Tests are established and recommended techniques for evaluating patients with vertigo and dizziness. | |
| American Academy of Neurology, 1996 | Electronystagmography | NA | Test is considered an established test of vestibular-ocular function that is both safe and effective, based upon Class III evidence. | |
| American Association of Otolaryngology-Head and Neck Surgery, 1995 | Meniere’s disease | NA | Criteria for the diagnosis of Meniere’s disease. | |
| National Institutes of Health Consensus Development Program, 1991 | Acoustic Neuroma | General evaluation and management | A consensus statement regarding treatment options and other clinical questions. | |
BPPV = benign paroxysmal positional vertigo; NA = not applicable.
Guidelines
Eight guidelines of clinical relevance were found (Table 1).29–36 No guideline broadly addresses dizziness presentations. One guideline offers criteria for the diagnosis of Meniere’s disease.30 Evaluation and management guidelines that address dizziness were found on the following topics: ischemic stroke,35 herpes zoster (including the Ramsay-Hunt vestibulo-cochlear syndrome),36 nystagmus,33 and acoustic neuroma.29 Three additional guidelines focused on the use of medical tests (i.e., electronystagmogram, vestibular tests, and imaging).31, 32, 34
Discussion
Physicians rely on the medical literature to inform decisions, but our study suggests that the evidence base for dizziness evaluation and management is weak. Meta-analyses and systematic reviews are particularly important to clinicians because these study designs minimize bias and summarize evidence in a manner useful to clinicians.8 Other than BPPV and Meniere’s disease, meta-analyses and systematic reviews were only found on alternative interventions and some other non-interventional topics.
Clinicians must also rely on the medical literature to decide about the usefulness of diagnostic tests. Most studies of medical tests pertaining to dizziness evaluate vestibular tests. Two guidelines both give consensus support of the clinical utility of vestibular tests.31, 32 The guidelines, however, do not summarize important measures of diagnostic accuracy (e.g., sensitivity, specificity, and likelihood ratios) – the information which is the most useful when making medical decisions.8 When the sensitivity and specificity of posturography was assessed by a meta-analysis design, both of these operating characteristics were only about 50% for identifying vestibular disorders20 – indicating that the test results do not influence the probability of the outcome. Imaging studies are increasingly used in dizziness evaluations, but no meta-analysis was found that measures the operating characteristics of these tests in dizziness presentations. The guideline on the topic of imaging studies in dizziness directs the choice of test after the decision has been made to order one,34 but does not offer guidance about who needs an imaging study.
We did not find a guideline of consensus recommendations for the evaluation and management of dizziness presentations. In fact, none of the guidelines found in this study were even intended to be a clinical practice guideline for dizziness. The main purpose of the guideline on Meniere’s disease was to establish design and reporting criteria for research studies.30 The statement on acoustic neuroma29 stems from a National Institutes of Health Consensus Development Conference – which aim to present useful consensus information to health professionals, but not are not intended to be clinical practice guidelines. The guideline on ischemic stroke only briefly addresses dizziness.35
Limitations
Consensus grading of article quality was not performed because it was beyond the scope of the current study. Although the reliability of the article classifications was not assessed because only one reviewer classified the articles, this potential source of bias is minimal since only basic descriptive information was abstracted from each article.
Conclusions
The evidence base for the evaluation and management of dizziness appears to be weak. Research should address questions such as, “Which dizziness patients are likely to benefit from having a brain image, vestibular test, audiogram, or blood work?” – since these tests are expensive, inconvenient and often bothersome to patients, and are generally of very low yield.4 Evidence for interventions – other than re-positioning for BPPV – is either insufficient or absent entirely. Thus, more empirical studies, systematic reviews and meta-analyses on relevant dizziness topics are needed so that evidence is established in a way that will inform clinicians and also research agendas. Guideline statements can then be developed to translate evidence into actual recommendations for clinical care. With these goals as priorities, future work could make an important contribution to the efforts to optimize patient care and healthcare utilization for one of the most common symptom presentations in all of medicine.
Acknowledgments
This work was supported by NIH K23RR024009
References
- 1.Newman-Toker DE, Cannon LM, Stofferahn ME, Rothman RE, Hsieh YH, Zee DS. Imprecision in patient reports of dizziness symptom quality: a cross-sectional study conducted in an acute care setting. Mayo Clin Proc. 2007;82(11):1329–40. doi: 10.4065/82.11.1329. [DOI] [PubMed] [Google Scholar]
- 2.Lee H, Sohn SI, Cho YW, Lee SR, Ahn BH, Park BR, Baloh RW. Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurology. 2006;67(7):1178–83. doi: 10.1212/01.wnl.0000238500.02302.b4. [DOI] [PubMed] [Google Scholar]
- 3.Cnyrim CD, Newman-Toker D, Karch C, Brandt T, Strupp M. Bedside differentiation of vestibular neuritis from central “vestibular pseudoneuritis”. J Neurol Neurosurg Psychiatry. 2008;79(4):458–60. doi: 10.1136/jnnp.2007.123596. [DOI] [PubMed] [Google Scholar]
- 4.Colledge NR, Barr-Hamilton RM, Lewis SJ, Sellar RJ, Wilson JA. Evaluation of investigations to diagnose the cause of dizziness in elderly people: a community based controlled study. Bmj. 1996;313(7060):788–92. doi: 10.1136/bmj.313.7060.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colledge N, Lewis S, Mead G, Sellar R, Wardlaw J, Wilson J. Magnetic resonance brain imaging in people with dizziness: a comparison with non-dizzy people. J Neurol Neurosurg Psychiatry. 2002;72(5):587–9. doi: 10.1136/jnnp.72.5.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simmons Z, Biller J, Adams HP, Jr, Dunn V, Jacoby CG. Cerebellar infarction: comparison of computed tomography and magnetic resonance imaging. Ann Neurol. 1986;19(3):291–3. doi: 10.1002/ana.410190312. [DOI] [PubMed] [Google Scholar]
- 7.Wasay M, Dubey N, Bakshi R. Dizziness and yield of emergency head CT scan: is it cost effective? Emerg Med J. 2005;22(4):312. doi: 10.1136/emj.2003.012765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Straus SE, Richardson WS, Glasziou P, Haynes RB. Evidence-based medicine: How to practice and teach EBM. New York: Elsevier; 2005. [Google Scholar]
- 9.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86(3):262–6. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 10.Kerber KA, Meurer WJ, West BT, Fendrick AM. Dizziness presentations in U.S. Emergency Departments: 1996–2004. Acad Emerg Med. doi: 10.1111/j.1553-2712.2008.00189.x. ([In press]) [DOI] [PubMed] [Google Scholar]
- 11.Kwong EC, Pimlott NJ. Assessment of dizziness among older patients at a family practice clinic: a chart audit study. BMC Fam Pract. 2005;6(1):2. doi: 10.1186/1471-2296-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Savitz SI, Caplan LR, Edlow JA. Pitfalls in the diagnosis of cerebellar infarction. Acad Emerg Med. 2007;14(1):63–8. doi: 10.1197/j.aem.2006.06.060. [DOI] [PubMed] [Google Scholar]
- 13.von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78(7):710–5. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing clinical research. Philadelphia: Lippincott Wiliams & Williams; 2007. [Google Scholar]
- 15.Sackett DL, Haynes RB. The architecture of diagnostic research. In: Knottnerus JA, editor. The evidence base of clinical diagnosis. London: BMJ Books; 2002. pp. 19–38. [Google Scholar]
- 16.Schneider B, Klein P, Weiser M. Treatment of vertigo with a homeopathic complex remedy compared with usual treatments: a meta-analysis of clinical trials. Arzneimittelforschung. 2005;55(1):23–9. doi: 10.1055/s-0031-1296821. [DOI] [PubMed] [Google Scholar]
- 17.Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2004;(2):CD003162. doi: 10.1002/14651858.CD003162.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2002;(1):CD003162. doi: 10.1002/14651858.CD003162. [DOI] [PubMed] [Google Scholar]
- 19.Woodworth BA, Gillespie MB, Lambert PR. The canalith repositioning procedure for benign positional vertigo: a meta-analysis. Laryngoscope. 2004;114(7):1143–6. doi: 10.1097/00005537-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Di Fabio RP. Meta-analysis of the sensitivity and specificity of platform posturography. Arch Otolaryngol Head Neck Surg. 1996;122(2):150–6. doi: 10.1001/archotol.1996.01890140036008. [DOI] [PubMed] [Google Scholar]
- 21.James AL, Burton MJ. Betahistine for Meniere’s disease or syndrome. Cochrane Database Syst Rev. 2001;(1):CD001873. doi: 10.1002/14651858.CD001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wayne PM, Krebs DE, Wolf SL, Gill-Body KM, Scarborough DM, McGibbon CA, Kaptchuk TJ, Parker SW. Can Tai Chi improve vestibulopathic postural control? Arch Phys Med Rehabil. 2004;85(1):142–52. doi: 10.1016/s0003-9993(03)00652-x. [DOI] [PubMed] [Google Scholar]
- 23.Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Man Ther. 2005;10(1):4–13. doi: 10.1016/j.math.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 24.James AL, Thorp M. Meniere’s disease. BMJ Clinical Evidence. 2006;15:797–803. [PMC free article] [PubMed] [Google Scholar]
- 25.Thirlwall AS, Kundu S. Diuretics for Meniere’s disease or syndrome. Cochrane Database Syst Rev. 2006;3:CD003599. doi: 10.1002/14651858.CD003599.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldstein LB, Simel DL. Is this patient having a stroke? JAMA. 2005;293(19):2391–402. doi: 10.1001/jama.293.19.2391. [DOI] [PubMed] [Google Scholar]
- 27.Hanley K, O’Dowd T, Considine N. A systematic review of vertigo in primary care. Br J Gen Pract. 2001;51(469):666–71. [PMC free article] [PubMed] [Google Scholar]
- 28.Hoffman RM, Einstadter D, Kroenke K. Evaluating dizziness. Am J Med. 1999;107(5):468–78. doi: 10.1016/s0002-9343(99)00260-0. [DOI] [PubMed] [Google Scholar]
- 29.Nance WE, Bailey BJ, Broaddus WC, et al. Acoustic neuroma. NIH Consensus Statement. 1991;9:1–24. [Google Scholar]
- 30.Committee on Hearing and Equilibrium. Guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. Otolaryngol Head Neck Surg. 1995;113(3):181–5. doi: 10.1016/S0194-5998(95)70102-8. [DOI] [PubMed] [Google Scholar]
- 31.Furman JM, Baloh RW, Hain TC, Hirsch BE, Parker SW. Assessment: electronystagmography. Report of the Therapeutics and Technology Assessment Subcommittee. Neurology. 1996;46(6):1763–6. doi: 10.1212/wnl.46.6.1763. [DOI] [PubMed] [Google Scholar]
- 32.Fife TD, Tusa RJ, Furman JM, Zee DS, Frohman E, Baloh RW, Hain T, Goebel J, Demer J, Eviatar L. Assessment: vestibular testing techniques in adults and children: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2000;55(10):1431–41. doi: 10.1212/wnl.55.10.1431. [DOI] [PubMed] [Google Scholar]
- 33.Straube A, Leigh RJ, Bronstein A, Heide W, Riordan-Eva P, Tijssen CC, Dehaene I, Straumann D. EFNS task force--therapy of nystagmus and oscillopsia. Eur J Neurol. 2004;11(2):83–9. doi: 10.1046/j.1468-1331.2003.00754.x. [DOI] [PubMed] [Google Scholar]
- 34.Turski PA, Seidenwurm DJ, Davis PC, et al. Vertigo and hearing loss. American College of Radiology; 2006. [(accessed 30 September 2007)]. Available at: http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria.aspx. [PubMed] [Google Scholar]
- 35.Anderson D, Larson D, Koshnick R, et al. Diagnosis and initial treatment of ischemic stroke. Institute for Clinical Systems Improvement; 2007. [(accessed 30 September 2007)]. Available at: http://www.icsi.org/guidelines_and_more/gl_os_prot/cardiovascular/stroke/stroke__ischemic__diagnosis_and_initial_treatment_of_.htm. [Google Scholar]
- 36.Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. 2007;44(Suppl 1):S1–26. doi: 10.1086/510206. [DOI] [PubMed] [Google Scholar]