Abstract
This article provides practical advice on healthy exercise prescription for children. There is growing scientific evidence about the abilities and limits of child athletes in both recreational and competitive environments. As exercise becomes essential for the prevention of illness and maintenance of health, the counselling for an exercise prescription requires enhanced knowledge. The latest recommendations on safe strength, resistance and weight training are presented in a concise format for office use.
Keywords: Athletes, Excercise, Resistance training, Strength training, Weight training
RÉSUMÉ :
Le présent article donne des conseils pratiques sur des prescriptions d’exercice sain pour les enfants. Les preuves scientifiques s’accumulent quant aux capacités et aux limites des enfants athlètes dans des milieux de loisirs et de compétition. Puisque l’exercice devient essentiel pour la prévention de la maladie et la préservation de la santé, il faut plus de connaissances pour faire du counseling relativement à une prescription d’exercice. Les dernières recommandations sur l’entraînement sécuritaire en force, en résistance et avec des poids sont présentées sous forme concise afin d’être facilement utilisées en cabinet.
Sara is 13 years old. She is a bright, well-rounded scholar who excels at all sports. She would like to focus on her athletics through an Academic Assistance Program that would allow her flexibility in attendance and deadlines at school so that she could meet both athletic and academic commitments. She wants to start a weight training program because many of her friends ‘work out’ at the gym.
Michael is 15 years old. He took grade nine physical education because he needed one compulsory credit. He is not athletically inclined but enjoys volleyball, and because he is not enrolled in a formal physical education class, he thought he might like to join an intramural team but feels that his skills are not advanced enough.
Our youth need to develop good physical activity and sport habits so that they will be lifelong exercisers. Sara and Michael in the vignettes are examples of the diversity of sport participation in youth. The intensity of involvement can vary from elite competitive training to sporadic recreational activities, and with this variation comes a variety of needs and demands on the youth’s lifestyle. The intensity of their activity may change through different phases of their life; however, the desire to remain fit and active should remain a priority. Involvement in sport may take the form of physical education classes, organized sporting events, recreational community exercise programs and individual and family physical activity. The key is motivating our youth from an early age to appreciate and enjoy the benefits of physical activity.
Sport medicine encompasses the prevention of injury, the diagnosis and rehabilitation of injury, and the continued training to maintain high performance levels. Many professional disciplines are involved in sports medicine including primary care physicians, orthopedic surgeons, physiotherapists, athletic therapists, nutritionists, psychologists and kinesiologists. Of equal importance are the coach, teacher and paren, the key individuals who encourage, support and monitor whether the goals of the student are being met through the sport of choice. It does not matter whether the sport is recreational or competitive; the adolescent participant needs positive reinforcement of his or her participation.
Children have always been perceived to be energetic, fit and strong because they are young. A healthy child enjoys movement, socializes through sports and activity, and is rewarded by personal accomplishments in self-esteem and skill acquisition. Yet, the reality is young people are not adopting healthy lifelong exercise.
Children are spending increasingly more time in sedentary activities such as using computers, playing video games and watching television. The educational system has changed the compulsory requirements for physical education; for example, only one secondary school credit in physical education or health is required in Ontario. The level and availability of extracurricular sport activities vary across the country and often depend on funding or volunteer parent support. Parents’ concerns over neighbourhood safety have restricted kids gathering in the local park for an informal game of baseball. Many children are enrolled in organized recreational and competitive sport through leagues and associations. This involves a commitment of money and time on the part of the parents and may not allow children to experiment comfortably with their bodies and their preferences for types of activities.
The instruction and education that parents give their children makes an impact if children continue to remain active as adults and gain the health benefits associated with exercise. The Ontario Ministry of Tourism and Recreation conducted a research survey on physical patterns in adult years and found that the 18- to 29-year-old group was more active than the older adults but not to the degree expected (1). In the 18- to 29-year-old group, 30% of the participants were inactive, 24% only exercised once weekly, which is of questionable benefit, and 46% exercised two to four times weekly. That means, that less than half of the adolescents who graduate into adulthood actually start with healthy exercise patterns. When tracked over a four-year period, younger adults only increased their level of physical activity by 4% while older adults increased by 15%.
The Ontario Ministry of Health produced a report “Just Ask Us: What We Want to Know About Health” (2) that details the health interests and questions of children from age eight to 15 years. In the area of fitness and exercise children wanted to know the following.
When do they have to start getting fit?
Is getting fit and playing sports the same thing?
How long should they exercise every day?
Why is exercise good for them?
Boys wanted to know how to make themselves stronger.
Girls wanted to know how to lose weight through exercise.
Taking the lead from these questions, the goals of a safe exercise program are clear. We need to educate our young on the why, how and what to do. We need to address the myths and concerns of body image, self-esteem and healthy bodies.
CONDITIONING AND EXERCISE
Sports injuries comprise 18% to 39% of school-aged children visits to their physician, admissions to the emergency room as reported on sport-specific surveys (3–6). The incidence has increased 10-fold over the past 10 years as organized and recreational sport has gained popularity (3,6). The majority of injuries are overuse syndromes stemming from training and technique errors in conditioning programs (3). The occurrence of youth sport injuries has been directly correlated to the quality of adult coaching and supervision (7). Strength training is a key component of sports conditioning aimed at preventing potential injuries and increasing skill and ability (4). Supervised strength training programs have been researched in the paediatric population and have been found to be effective in increasing dynamic strength and safe for growing muscles, bones and growth plates (7–10). Injuries to a skeletally immature athlete are common, but most of the injuries do not have long term implications. There is no risk-free sport, and children tend to select the sports that they wish to participate in based on their own desire, peer pressure and their own talent regardless of the injury rate (8,10,11). A preparticipation athletic examination is helpful for identifying adolescents at risk of orthopaedic injury, and guidelines developed by the American Academy of Pediatrics provide the most current source on which conditions disqualify athletes from specific sports (6).
Early studies in pre- and postpubescent children found no significant strength gains after a monitored training program (12). Numerous studies from 1985 to 1995 have proven that children can increase muscular strength (8–10,13). The physiological mechanism for strengthening may not be muscle hypertrophy as it is in adults. Neural adaptation of motor unit activation and intrinsic muscle function measured in twitch torque appear to produce positive changes in motor skill coordination resulting in improved strength tests (8,14). Neural adaptation occurs when there is an increased ability to activate and coordinate the relevant muscles as opposed to muscular adaptation where there is an increase in muscle size and specific tension.
Research performed on children participating in specific sports such as running studied aerobic capacity and found only a 6% improvement in measured ventilatory oxygen uptake after a 12-week supervised program (15,16). The expected improvement from a similar program in the adult population is 18% to 20%. Physiological differences in children, such as smaller organs in proportion to body size and less efficient metabolism and heat transfer, may contribute to lower training effects (5,15). The physical benefits of exercise include increased bone density, decreased lipid profiles, healthy body composition, improved posture and reduced injury occurrence (5,17).
Psychological benefits for children and adolescents include improved self-concept, mental discipline, acquisition of social skills and improved lifestyle attitudes. There have many studies whose results display a trend in improved school performance with regular exercise (8).
The question regarding the psychological effects of exercise usually centres around the issue that competitive sport may create unhealthy stress in children. Stress in sport can be divided into the categories of state anxiety, trait anxiety and burn-out. State anxiety refers to a stress reaction that occurs during sport participation (5,18). Trait anxiety refers to the intrinsic personality characteristics of the child that may be compounded in situational stress. For example, all batters in a baseball game will experience anxiety symptoms such as increased heart rate, perspiration and twitchiness. These symptoms will subside in the majority of players once batting has finished. Children with trait anxiety have personality characteristics that lend to worry, self-criticism and anxiety. These children worry about the game the night before, are unable to eat dinner on the day of the game and still experience increased stress at the time of batting. Their symptoms may not subside after the game is over, and they may have sleep disturbance or withdrawal.
Burn-out is a reaction to the stresses of training and competition that manifests as emotional exhaustion, withdrawal and decreased physical performance. This can be a result of imbalance between physical demands and age-appropriate capabilities. Burn-out avoidance strategies such as having a recreational sport, taking productive breaks, treating physical injuries early and keeping winning and losing in perspective can reduce its incidence and severity (5).
The Committee on Sports Medicine of the American Academy of Pediatrics wrote a position statement entitled “Assessing Physical Activity and Fitness in the Office Setting” (19). This document outlines the relevant assessment techniques that enhance physicians’ understanding of their patients’ physical activity demands and needs. Some of the recommendations include the following.
Assess, using a history, the frequency, type and duration of physical activities during any health supervision visit for a child three years of age and older.
Teach the importance of regular moderate to vigorous physical activity as a way to prevent illness in adult life.
Encourage parents to serve as role models by participating in regular physical activity, ideally with their child as a family.
Serve as role models by participating in regular physical activity.
Work with community schools, supporting daily physical education in these schools, and promoting moderate to vigorous activity tasks in physical education classes.
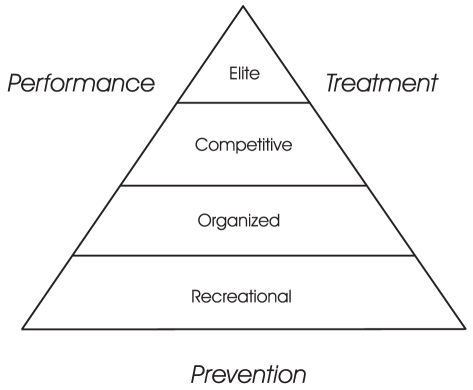
Each child must be evaluated for readiness for competition and coping skills for situational anxiety. This can be done by an experienced coach, insightful parents, a physician or psychologist. The assessor should be unbiased and interested in the child’s welfare, not the secondary gain of winning. More complex cases where high injury rates, growth or weight alterations, fluctuation in school performance, or emotional instability are seen should be assessed by a physician. Generally, in the earlier years of childhood, participation should be recreational, with skill acquisition, socialization and physical development the primary goals. Some children may be ready for intense competition by age eight or nine years while others may not be ready until age 12 or 13 years. Key questions and considerations of the assessment are listed in Tables 1 and 2. There is a sequence of escalating skills and demands that should be followed to ensure that a child is ready and prepared for the next level of sport participation (Figure 1).
TABLE 1:
Key questions to include in the assessment of readiness of children for competitive sport
| Questions | Recreational answer | Competitive answer |
|---|---|---|
| Who wants the child to participate in the sport? | Parents want child to try Child wants a trial – first time |
Child has been involved in sport and wants to continue |
| What are the goals for learning the skills of the sport? | Gain basic technical skill | Refine skill Enjoys analysis of performance |
| What does the child enjoy socially about the sport? | Likes to meet new friends Building social skills |
Builds his or her own character Enjoys a few close, long term friends |
| How much time does the family have? | One to two times a week to a total of 4 to 5 h | Five to six times a week with a total of 16 to 25 h |
| How many other activities does the child have? | Seasonal variations May have multiple activities |
One dominant activity; may have a second that is usually complementary in some way |
TABLE 2:
The win/lose side of competition
| Psychological factor | Negative | Positive |
|---|---|---|
| Competitive stress | Anxiety disorder, identifies self as winner or loser, no fun involved | Develops coping skills for a competitive world |
| Self-esteem | Failure is a consequence of their own action, feelings of incompetence | Achievement of realistic, personal goals |
| Motivation | Repeated failure leading to fear of failure and lack of risk-taking | Tremendous challenge that motivates excellence, internal gratification |
| Competitiveness | Irrationally competitive, win at all costs | Cooperative and competitiveness mixed together |
| Moral development | Poor sportsmanship – cheating, violence, intimidation | Positive role models, rule organization, used appropriately |
| Attitudes | Criticism, exercise punishment | Healthy bodies, healthy lifestyle |
| Responsibility | External control, no independence | Strategy and decision making skills |
Figure 1).
Sequence of skill acquisition for safe sport participation
SAFE STRENGTH, RESISTANCE AND WEIGHT TRAINING
Strength training is a general term that pertains to submaximal resistance exercise, weight lifting of increasing values and power-lifting of excessive weight. In this article submaximal lifts of resistance in children and early adolescents are defined as increasing from theraband to body resistance to external weight. Submaximal is defined as below the available boundary of energy expenditure.
Parents and physicians have traditionally been concerned about growth plate fractures and the risk of growth arrest. The literature suggested that epiphyseal fractures occurred more often in pubescents and postpubescents than in prepubescents (20–22). Micheli in his 1986 study (3) indicated that prepubescent growth plates may be less prone to fracture because they may be stronger and more resistant to sheer stress than growth plates in the later stages of development where the hormone activity level is higher.
The majority of injuries appear to be preventable when conditioning techniques, equipment and rate of exercise progression are supervised. Movements such as improper lifting techniques, excessive loading, rapid progression of weight and ballistic movements all result in greater sheer forces at the joint. In prospective resistance training studies, where close supervision is integrated into training, the incidence of injury drops significantly to the relatively rare category (9,11,22). Furthermore, follow-up studies of growth plate fractures appear to have no detrimental effect on growth when diagnosed early and properly treated (23). Strength training programs should be tailored to the child’s growth and development. Guidelines from Committee on Sports Medicine in Pediatrics (20) stated that children are encouraged to strength train using submaximal weights but should avoid any practice of weight lifting, power lifting and body building until they have reached a level of Tanner stage 5 in developmental maturity.
STRENGTH AND WEIGHT TRAINING PRESCRIPTION
Guidelines for safe strength training include the components of frequency (how many times per week), intensity (number of exercises and repetitions), type (method of resistance and scope of exercise) and time (length of session and progression) (Table 3). This is often referred to as the FITT formula. Some of the key difference between adults and children include: lower numbers of repetition, submaximal weights, exercising through the full range of motion and only doing a resistance program two to three times per week.
TABLE 3:
Exercise prescription for children and adolescents
| Frequency | Intensity | Type | Time |
|---|---|---|---|
| Two to three times per week | Upper body: Choose four to five muscle groups and use eight to 12 repetitions of each group in one to three sets | Submaximal resistance | Start with no weight |
| At least one rest day between work-outs | Lower body: Choose four to six muscle groups, use nine to 15 repetitions of each group in one to three sets | Integrate with conditioning in flexibility/cardiovascular strength | Add weight gradually to an initial maximum of six repetitions, add one to two repetitions per training session to a maximum of 12 to 15 repetitions |
| Use the full range of motion | Increase weight by 0.5 to 1 kg (1 to 3 lbs). Increments every third training session No maximum lifts Each session should be 20 to 30 mins |
The first step to defining a program is to choose the muscle groups that require training. This should be determined by the sport involved, and the exercises should be for sport-specific training or development of weak areas to create improved muscle balance. Generally, the lower body has a few more muscle groups to exercise. Then, within each muscle group, determine the maximum capacity and set the actual weight below that. Maximum capacity can be determined by increasing weight until the participant feels muscle fatigue, shakiness or reduced ability to complete range. The strength training program should always be integrated into a full fitness regimen including aerobic exercise and flexibility stretching. Supervision is recommended, especially in the first 12 to 18 months of training. This monitoring provides correction of technique, approval for weight progressions, integration into the whole program and position advice.
TREATING THE CHILD ATHLETE
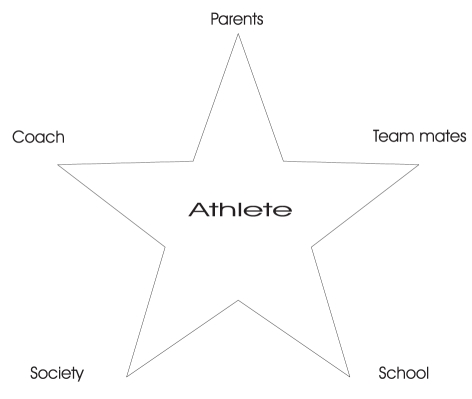
When a child athlete attends your office for evaluation there are many influences and factors that affect the compliance and adherence to recommended treatment strategies. The athlete is receiving information from multiple sources including the coach, parents and team mates. Often, a note to the coach or a call from the teacher are common occurrences. Information and influences are abundant from parents, television, the internet and the sports sector of society. This can be supportive or it may be confusing. Understanding the dynamics in a child’s life and the ‘team’ that they bring with them is often the key to successful communication and implementation of treatment (Figure 2). The child’s safety and health should be the foremost consideration of the physician, and this perspective needs to be presented clearly in a sensitive manner to the child and parents.
Figure 2).
When treating a child athlete, often a full team of influences act upon the athlete’s life
EXERCISE PRESCRIPTION FOR CHILDREN WITH SPECIAL NEEDS
Children with an illness or a disability should be encouraged to exercise on a regular schedule and with supervision initially. The fitness program components do not change but the intensity, progression and choice of equipment may need to be modified. Good exercise programs are available for children with asthma, obesity and developmental special needs. Encouraging family exercise programs assists in the normal socialization process. Equipment may need to be modified, such as ski-tip clips that hold alpine skis in a wedge position for better control with a special needs child. Supervision in exercise progression occurs in walking and swimming programs for asthmatics. Balance can be challenged by horse-back riding programs and sports such as bowling and curling.
CONCLUSIONS
Our youngsters are slowly but surely heading in two directions. Those who do exercise and do so with intensity and those who do not exercise and progressively decrease their daily activity levels. Each group requires advice and counselling, while parents, children and coaches look to the medical profession for guidance and credibility.
The once taboo subject of weight training in children has been researched and shows that safe exercise can be prescribed. The key to success lies in the exercise technique, proper progression and safe equipment. Supervision is a vital component. Training can serve to improve performance in many daily activities such as socialization, school performance and sport. Children with illness and disability are encouraged to participate in individual exercise and team sport to develop strength and reduce injury.
The Canadian Academy of Sport Medicine’s Sport Safety Committee is working on a position paper on safe strength training. It is expected to be released in spring 1999.
REFERENCES
- 1.Physical Activity Patterns in Ontario, Ministry of Tourism and Recreation. Toronto: Publications Service Section, Ministry of Tourism and Recreation; 1983. [Google Scholar]
- 2.Corlett S. Just Ask Us: What We Want to Know About Health. Toronto: Ontario Ministry of Health; 1983. [Google Scholar]
- 3.Micheli L. Pediatric and adolescent sports injuries: recent trends. Exerc Sports Sci Rev. 1986;14:359–74. [PubMed] [Google Scholar]
- 4.Zito M. The adolescent athlete: a musculoskeletal update. J Orthop Sports Phys Ther. 1983 Jul;:20–25. doi: 10.2519/jospt.1983.5.1.20. [DOI] [PubMed] [Google Scholar]
- 5.Reider B. Sports Medicine: The School-Age Athlete. Philadelphia: WB Saunders; 1991. [Google Scholar]
- 6.Report of the Board of Trustees Group on Science and Technology, American Medical Association. Athletic preparticipation examinations for adolescents. Arch Pediatr Adolesc Med. 1994;148:93–8. [PubMed] [Google Scholar]
- 7.Weltman A, Janney C, Rians CB, et al. Effects of hydraulic resistance strength training in prepubertal males. Med Sci Sports Exerc. 1986;8:629–38. [PubMed] [Google Scholar]
- 8.Blimkie CJR. Resistance training in preadolescence: issues and controversies. Sports Med. 1993;15:389–407. doi: 10.2165/00007256-199315060-00004. [DOI] [PubMed] [Google Scholar]
- 9.Ozmun JC, Mikesky AE, Surburg PR. Neuromuscular adaptations following prepubescent strength training. Med Sci Sports Exerc. 1994;26:510–4. [PubMed] [Google Scholar]
- 10.Faigenbaum AD, Wescott WL, Micheli LJ, et al. The effects of strength training and detraining on children. J Strength Conditioning Res. 1996;10:109–14. [Google Scholar]
- 11.Sallis JF, Patrick K. Physical activity guidelines for adolescents: consensus statement. Pediatr Exerc Sci. 1994;6:302–14. [Google Scholar]
- 12.Vrijens J. Muscle strength development in the pre and postpubescent age. Med Sport. 1978;11:99–103. [Google Scholar]
- 13.DeRenne C, Hetzler RK, Buxton BP, Ho KW. Effects of training frequency on strength maintenance in pubescent baseball players. J Strength Conditioning Res. 1996;10:8–14. [Google Scholar]
- 14.Blimkie CJR. Resistance training during pre- and early puberty: efficacy, trainability, mechanisms, and persistence. Can J Sport Sci. 1992;17:264–79. [PubMed] [Google Scholar]
- 15.Cahill BR, Pearl AJ. American Orthopaedic Society for Sports Medicine, Intensive Participation in Children’s Sports. Champagne: Human Kinetics Publishers; 1993. [Google Scholar]
- 16.Rowland T, Goff D, DeLuca P, Popowski B. Cardiac effects of a competitive road race in trained child runners. Pediatrics. 1997;100:e2. doi: 10.1542/peds.100.3.e2. [DOI] [PubMed] [Google Scholar]
- 17.Kraemer WJ, Fleck SJ. Strength Training in Young Athletes. Champaign: Human Kinetics; 1993. [Google Scholar]
- 18.Faigenbaum AD. Psychosocial benefits of prepubescent strength training. Strength Conditioning. 1995;17:28–32. [Google Scholar]
- 19.Committee on Sports Medicine, American Academy of Pediatrics Assessing physical activity and fitness in the office setting. Pediatrics. 1994;93:686–9. [PubMed] [Google Scholar]
- 20.American Academy of Pediatrics Committee on Sports Medicine: Strength training, weight and power lifting, and body building by children and adolescents. Pediatrics. 1990;86:801–3. [PubMed] [Google Scholar]
- 21.Brady TA, Cahill BR, Bodnar MD. Weight training related injuries in the high-school athlete. Am J Sport Med. 1982;10:1–4. doi: 10.1177/036354658201000101. [DOI] [PubMed] [Google Scholar]
- 22.Bernhardt DT, Landry GL. Sports injuries in young athletes. Adv Pediatr. 1995;42:465–500. [PubMed] [Google Scholar]