Abstract
A case of Epstein-Barr virus-related acute giant cell myocarditis in a 16-year-old boy is reported. Fulminant heart failure was successfully treated with extracorporeal membrane oxygenation as a bridge to urgent heart transplantation, and was again necessary after transplantation because of acute right heart failure. Clinical management and postoperative surveillance of this unusual problem are presented and discussed.
Keywords: ECMO, Giant cell myocarditis, Heart transplantation
Abstract
Les auteurs rendent compte du cas d’un garçon de 16 ans atteint d’une myocardite aiguë à cellules géantes liée au virus d’Epstein-Barr. On a traité l’insuffisance cardiaque fulminante par oxygénation extracorporelle dans l’attente d’une greffe cardiaque d’urgence, puis on a repris ce traitement après la greffe en raison d’une insuffisance aiguë du cœur droit. La prise en charge clinique et la surveillance postopératoire de ce problème inhabituel sont présentées et exposées.
CASE PRESENTATION
A 16-year-old boy presented with hemodynamic instability due to ventricular tachycardia, and required respiratory and inotropic support. Left ventricular function was severely reduced (ejection fraction 15%). Myocardial biopsy revealed acute giant cell myocarditis (GCM) with extensive myocardial necrosis (Figure 1). Real-time polymerase chain reaction analysis demonstrated evidence of Epstein-Barr virus-specific DNA. Intravenous immunoglobulin therapy (Gamunex, Bayer, Germany) was given without any noticeable effect. Due to further deterioration, veno-arterial extracorporeal membrane oxygenation (ECMO) was initiated, with subsequent heart transplantation within 26 h. The patient developed acute right heart failure after transplantation and, despite the use of catecholamines and inhaled nitric oxide, ECMO support was required for another 28 h. He was successfully weaned from ECMO thereafter and discharged from the hospital on the 36th postoperative day. The patient was treated postoperatively with triple-regimen immunosuppressive therapy, guided by frequent myocardial biopsies (Table 1). The most recent follow-up at 60 weeks postoperatively revealed that the patient was in good health with no signs of giant cell recurrence.
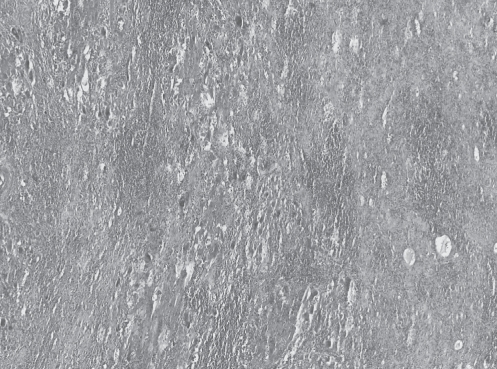
Figure 1).
Extensive multifocal necrosis with infiltration of lymphocytes, granulocytes and formation of giant cells in the myocardium of a 16-year-old boy
TABLE 1.
Results of endomyocardial biopsies after heart transplantation for acute giant cell myocarditis in a 16-year-old boy
| Weeks after transplantation | Immunosuppressive medication | ISHlT 1990 grade |
|---|---|---|
| 1.5 | Cyclosporin/MMF/steroids | 1A |
| 3 | Cyclosporin/MMF/steroids | 1A |
| 6 | Tacrolimus/MMF/steroids | 1A |
| 8 | Tacrolimus/MMF/steroids | 1A |
| 10 | Tacrolimus/MMF/steroids | 1A |
| 12 | Tacrolimus/MMF/steroids | 1B |
| 14 | Tacrolimus/MMF/steroids | 1B |
| 16 | Tacrolimus/MMF/steroids | 1B |
| 20 | Tacrolimus/everolimus/steroids | 1A |
| 22 | Tacrolimus/everolimus/steroids | 1A |
| 26 | Tacrolimus/everolimus/steroids | 1A |
| 30 | Tacrolimus/everolimus/steroids | 0 |
| 36 | Tacrolimus/everolimus/steroids | 1A |
| 42 | Tacrolimus/everolimus/steroids | 2 |
| 46 | Tacrolimus/everolimus/steroids | 1B |
| 52 | Tacrolimus/everolimus/steroids | 1A |
| 56 | Tacrolimus/everolimus/steroids | 1A |
ISHLT International Society for Heart and Lung Transplantation; MMF Mycophenolate mofetil
DISCUSSION
GCM is frequently associated with a fulminant clinical course, and the need for immediate mechanical assistance and heart transplantation (1,2). Only 18 cases of pediatric GCM have been reported, of which only five patients were successfully treated with transplantation (3). The Multicenter Giant Cell Myocarditis Study Group (1) recorded 63 patients in whom the rate of death or cardiac transplantation was 89% (1).
Therapeutic options for GCM include immunosuppression, implantation of a left ventricular assist device and/or heart transplantation (1–3). Evidence-based recommendations are not currently available due to the small number of described cases.
In our patient, ECMO was applied as a bridge to transplantation due to fulminant heart failure, as well as a bridge from transplantation due to isolated right heart failure. To our knowledge, the present article is the first reported case of ECMO support before and after heart transplantation in children, particularly in a patient suffering from GCM.
The presence of GCM along with altered immune function (4) emphasizes the importance of post-transplantation immunosuppressive management, especially because a GCM recurrence rate of 25% in the transplanted heart has been described (1). Although our patient did achieve grade 0 rejection once during postoperative surveillance, we consider his immunosuppressive treatment to be successful because there was no recurrence of giant cells in the transplanted heart (Table 1). Therefore, we believe that frequent endomyocardial biopsies allowed us to carefully monitor his immunosuppressive management. Based on this limited experience, we believe that a triple-immunosuppressive regimen is a reasonable protocol for such patients.
The etiology of GCM is unknown, but an association with immune disorders and viral triggers has been reported (4,5). To the best of our knowledge, the present article is the first reported case of GCM associated with Epstein-Barr virus. It is important to emphasize, however, that this is simply an association and no conclusions can be drawn regarding causation.
It is known that GCM may recur in a significant proportion of patients. Because our patient had no recurrence 60 weeks postoperatively, we believe the aggressive surgical treatment and postoperative immunosuppression was justified. More cases will need to be reported and observed, however, to make more definitive recommendations on the management of this rare clinical problem.
REFERENCES
- 1.Cooper LT, Jr, Berry GJ, Shabetai R, Multicenter Giant Cell Myocarditis Study Group Investigators Idiopathic giant-cell myocarditis – natural history and treatment. N Engl J Med. 1997;336:1860–6. doi: 10.1056/NEJM199706263362603. [DOI] [PubMed] [Google Scholar]
- 2.Davies RA, Veinot JP, Smith S, Struthers C, Hendry P, Masters R. Giant cell myocarditis: Clinical presentation, bridge to transplantation with mechanical circulatory support, and long term outcome. J Heart Lung Transplant. 2002;21:674–9. doi: 10.1016/s1053-2498(02)00379-0. [DOI] [PubMed] [Google Scholar]
- 3.Das BB, Recto M, Johnsrude C, et al. Cardiac transplantation for pediatric giant cell myocarditis. J Heart Lung Transplant. 2006;25:474–8. doi: 10.1016/j.healun.2005.11.444. [DOI] [PubMed] [Google Scholar]
- 4.Laufs H, Nigrovic PA, Schneider LC, et al. Giant cell myocarditis in a 12-year-old girl with common variable immunodeficiency. Mayo Clin Proc. 2002;77:92–6. doi: 10.4065/77.1.92. [DOI] [PubMed] [Google Scholar]
- 5.Drut RM, Drut R. Giant-cell myocarditis in a newborn with congenital herpes simplex virus (HSV) infection: An immunohistochemical study on the origin of giant cells. Pediatr Pathol. 1986;6:431–7. doi: 10.3109/15513818609041557. [DOI] [PubMed] [Google Scholar]