A 53-year-old man visiting from India came to us for an outpatient cardiology visit. His medical history was significant for hypertension and dyslipidemia, along with an anterior-wall myocardial infarction sustained a few months before his arrival in the United States. According to the patient, an attempt in India to perform acute percutaneous coronary intervention had been unsuccessful.
The results of physical examination, including examination of the patient's vital signs, were normal, except for minimally decreased bilateral basal breath sounds upon auscultation. Because the patient refused invasive cardiac catheterization, a myocardial perfusion scan was performed; it showed a reversible defect of the anterior myocardial wall. Subsequently, multidetector computed tomography of the heart (64-slice MDCT) was performed to evaluate the coronary arteries. This revealed occlusion of the proximal left anterior descending coronary artery (LAD), with distal reappearance of the vessel. The distal segment was thought to be filled by collateral vessels. In addition, there was greater than 70% stenosis of the proximal left circumflex coronary artery (LCx) and moderate disease of the right coronary and left main coronary arteries. Coronary artery bypass grafting was recommended.
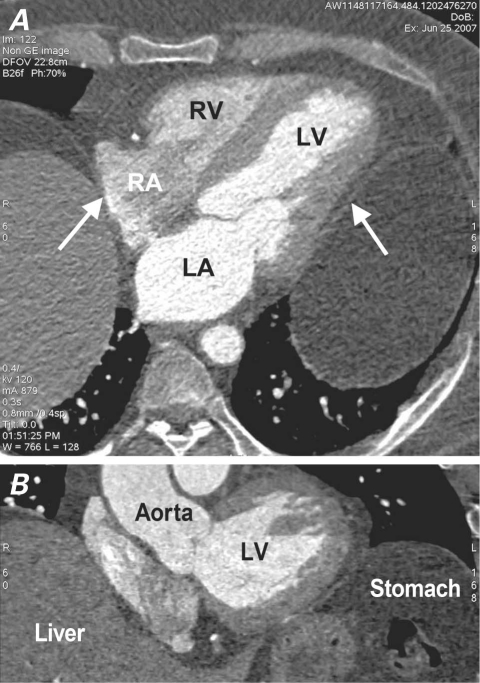
An additional finding upon examination of the cardiac computed tomographic images was prominent bilateral diaphragmatic elevation and compression of the patient's heart by the 2 domes of the diaphragm (Fig. 1). The diaphragmatic elevation was also visible in the scout chest film done before the MDCT. The patient, however, had no signs or symptoms of myocardial or coronary compression from outside pressure, as reported by Schoen and colleagues1 in another case. No other disorder of the chest and upper abdomen was seen on the computed tomographic images.
Fig. 1 Axial (A) and coronal (B) images on cardiac computed tomographic angiography show compression of the heart by the 2 elevated domes (arrows) of the diaphragm.
LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle
Comment
Bilateral diaphragmatic elevation can occur due to local causes above the diaphragm (for example, lung collapse or atelectasis), within the diaphragm (for example, phrenic nerve palsy or diaphragmatic eventration), or below the diaphragm (for example, abdominal tumor, enlargement of abdominal viscera, or obesity).2 Conditions that can mimic elevated hemidiaphragms might involve subpulmonic effusions, diaphragmatic hernia, or rupture and tumor of the pleura or diaphragm. The origin of the condition in our asymptomatic patient is unknown, but he is unlikely to have experienced bilateral diaphragmatic paralysis, because the diaphragm is a muscle crucial to respiration: such patients typically present with respiratory failure3 and frequently require long-term ventilatory assistance.4,5
On the follow-up visit 1 month after coronary artery bypass grafting (left internal mammary artery to LAD and radial artery to proximal LCx), the patient remained asymptomatic. This experience illustrates that one should be alert to extracardiac structures within the field of vision of cardiac computed tomography.
Footnotes
Address for reprints: Yasmin S. Hamirani, MD, Department of Cardiology, Los Angeles Biomedical Research Institute at Harbor-UCLA, 1124 W. Carson St., Torrance, CA 90502
E-mail: yasminshamshuddin@yahoo.com
References
- 1.Schoen SP, Altmann O, Strasser RH. Elevation of left-sided diaphragm leading to myocardial infarction by compression of the left circumflex artery. J Invasive Cardiol 2008;20(8): E250–2. [PubMed]
- 2.Slone RM, Gutierrez FR, Fisher AJ. Thoracic imaging: a practical approach. 1st ed. New York: McGraw-Hill; 1999. p. 49.
- 3.Gibson GJ. Diaphragmatic paresis: pathophysiology, clinical features, and investigation. Thorax 1989;44(11):960–70. [DOI] [PMC free article] [PubMed]
- 4.Kumar N, Folger WN, Bolton CF. Dyspnea as the predominant manifestation of bilateral phrenic neuropathy. Mayo Clin Proc 2004;79(12):1563–5. [DOI] [PubMed]
- 5.Ben-Dov I, Kaminski N, Reichert N, Rosenman J, Shulimzon T. Diaphragmatic paralysis: a clinical imitator of cardiorespiratory diseases. Isr Med Assoc J 2008;10(8–9):579–83. [PubMed]