Abstract
In recent years, researchers have investigated the relationship between biological markers of inflammation and prognosis in patients who experience acute coronary syndromes; however, the association between plasma fibrinogen and coronary heart disease is still not clear. We studied the prognostic value of fibrinogen, an acute-phase protein that is directly involved in thrombotic processes, by measuring plasma fibrinogen levels serially in 136 patients who had acute coronary syndromes, 142 patients who had stable coronary heart disease, and 82 healthy control participants.
Plasma fibrinogen levels were significantly higher in the patients with acute coronary syndromes (302 ± 90 mg/dL) than in the patients with stable coronary heart disease (274 ± 61 mg/dL) and the control group (243 ± 55 mg/dL) (both P <0.05). We also found significantly higher plasma fibrinogen levels in patients who developed clinical events than in those who did not, at 30 days and 2 years (P <0.05). Cox regression analysis showed that high C-reactive protein values and plasma fibrinogen levels ≥350 mg/dL were predictors of poor long-term prognosis. The adjusted odds ratio (95% confidence interval) for patients who had higher levels of plasma fibrinogen was 5.207.
Plasma fibrinogen level can be used as an independent predictor of major adverse cardiac events during short- and long-term follow-up (P <0.01). The association is independent of other classical risk factors, such as age and sex.
Key words: Acute-phase proteins, biological markers/blood, cardiovascular diseases/blood/etiology, coronary disease/complications/physiopathology, fibrinogen/analysis/classification, logistic models, multivariate analysis, predictive value of tests, prognosis, risk factors, survival analysis
Over the past 30 years, coronary heart disease (CHD) has been a leading cause of death in developed countries. Among all types of CHD, patients with acute coronary syndrome (ACS) constitute a major proportion of persons who require admission to cardiac units for urgent care (including invasive treatment, and aggregate anticoagulant and antiplaque drug therapy).1 To determine prognoses and appropriate treatments, physicians need to evaluate patients' risk of ACS within a short time of admission, which requires awareness of certain risk predictors. The association between inflammation and atherosclerosis has been confirmed, and studies have shown that the plasma level of acute-phase reactants such as C-reactive protein (CRP) and fibrinogen are significantly increased in most patients with ACS.2,3 We sought to determine the relationship between plasma levels of fibrinogen and the occurrence of major adverse cardiac events (MACEs) at 30 days and 2 years—including death, recurrent ischemia, or reocclusion of the infarct-related artery—among patients who were admitted to the hospital with suspected ACS.
Patients and Methods
Patients
We performed a retrospective study of 278 patients who were confirmed via coronary angiography to have CHD (defined as the presence of ≥50% stenosis of any of the main coronary arteries, according to the American College of Cardiology/American Heart Association lesion classification) and who received percutaneous coronary intervention treatment; and 82 healthy control participants. All were referred from 2005 through 2007. Patients who had experienced unstable angina pectoris, ST-elevation myocardial infarction, or non-ST-elevation myocardial infarction were considered to have ACS. Of the 278 patients who had CHD, 136 patients were diagnosed with ACS and 142 with stable angina pectoris.
We excluded individuals who had a history of recent surgery, trauma, peripheral arteriopathy, hepatic insufficiency (prothrombin ratio, <50%), renal insufficiency (creatinine, >1.5 mg/dL), malignancy, febrile disorders, or acute or chronic inflammatory disease at the time of study enrollment; persons who had autoimmune diseases with or without immunosuppressive therapy, or a prior myocardial infarction and ACS; and anyone who was undergoing anticoagulant treatment.
A follow-up period of 2 years was enabled by telephone interviews and reviews of clinical histories. Follow-up was obtained for 100% of the ACS patients at 30 days and in 84% at 2 years; 22 patients were lost to long-term follow-up. The MACEs involved death or reocclusion of an infarct-related artery. The study was approved by the Ethics Committee of the Zhejiang University School of Medicine, and each study participant provided informed written consent.
Laboratory Investigation of Blood Samples
Blood samples for fibrinogen and other biochemical analyses were taken before any treatment was initiated. All analyses were performed in our hospital laboratory. Plasma fibrinogen levels were determined via the Clauss method4 and use of a BBL™ semiautomated fibrometer (BD Diagnostic Systems; Sparks, Maryland). Other biochemical measurements were determined by standard laboratory methods.
Statistical Analysis
All laboratory data were collected from the patients' records. Data were expressed as mean ± SD. Continuous variables among the 3 groups were compared via 1-way analysis of variance for parametric data and the Kruskal-Wallis test for nonparametric data. Frequency variables were compared by means of the χ2 test. Also, predictive factors were sought by stepwise logistic regression analysis of variables that were considered to be relevant from a clinical point of view. The variables in the study were age, sex, CRP level, white blood cell (WBC) count, plasma fibrinogen level, diabetes mellitus, dyslipidemia, arterial hypertension, and smoking. Plasma fibrinogen level and WBC count were dichotomized into binary predictors. The cutoff points were 1.0 × 109/L for WBC count and ≥350 mg/dL for plasma fibrinogen level. A Kaplan-Meier analysis (log-rank test) was performed in order to analyze the relationship between survival time and plasma fibrinogen level by comparing survival rates without combined cardiac events in the high- and low-fibrinogen-level groups. To study the effects of other variables, we performed a multivariate Cox regression analysis, including those variables that had a P value of less than 0.05 upon stepwise logistic analysis. Confidence intervals (CIs) corresponded to the 95% level. Differences were considered to be significant when the P value was less than 0.05. The data conformed to each test by which they were analyzed. All statistical analysis was performed with use of SPSS version 16.0 software (SPSS, Inc.; Chicago, Ill) on a Windows XP platform.
Results
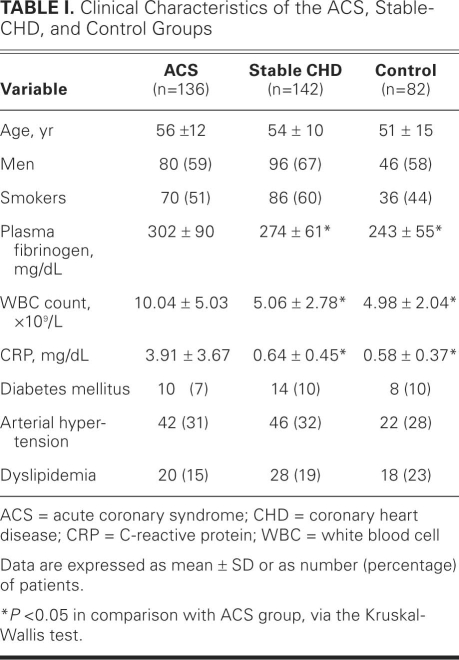
Table I shows the relevant baseline data on the study population. No significant differences were observed in terms of age, sex, or creatinine level between the ACS, stable-CHD, and control groups. Of all 360 study participants, 110 had arterial hypertension (30.5%), 32 had diabetes mellitus (9%), and 66 had dyslipidemia (18%). Incidences of arterial hypertension, diabetes mellitus, and dyslipidemia were similar among the 3 groups.
TABLE I. Clinical Characteristics of the ACS, Stable-CHD, and Control Groups
Comparison of Plasma Fibrinogen Levels between the Groups
The plasma fibrinogen levels of the 3 groups were compared (Table I). The mean levels upon hospital admission were 302 ± 90 mg/dL in the ACS group, 274 ± 61 mg/dL in the stable-CHD group, and 243 ± 55 mg/dL in the control group. There were significant differences between the ACS group and the other 2 groups in plasma fibrinogen level (both P <0.05). Significant differences were also found between the ACS group and each of the other 2 groups in WBC counts and CRP values.
Plasma Fibrinogen Levels and the Development of Clinical Events
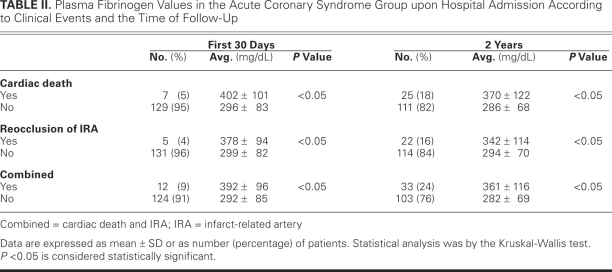
Table II shows the plasma fibrinogen levels of ACS patients who developed clinical events during the 1st month and by the 2nd year. During a follow-up period of 2 years, 33 patients (24%) with combined MACEs (reocclusion of infarct-related artery, and death) were recorded. Among these patients, 7 deaths (5%) and 5 cases of reocclusion (4%) were reported in the first 30 days; in comparison, 25 deaths (18%) and 22 cases of reocclusion (16%) were reported upon long-term (2-year) follow-up. Our study showed that ACS patients who developed clinical events had significantly higher fibrinogen levels than those who did not (P <0.05), and that the difference was more apparent between patients who developed clinical events during the first 30 days and those who did not.
TABLE II. Plasma Fibrinogen Values in the Acute Coronary Syndrome Group upon Hospital Admission According to Clinical Events and the Time of Follow-Up
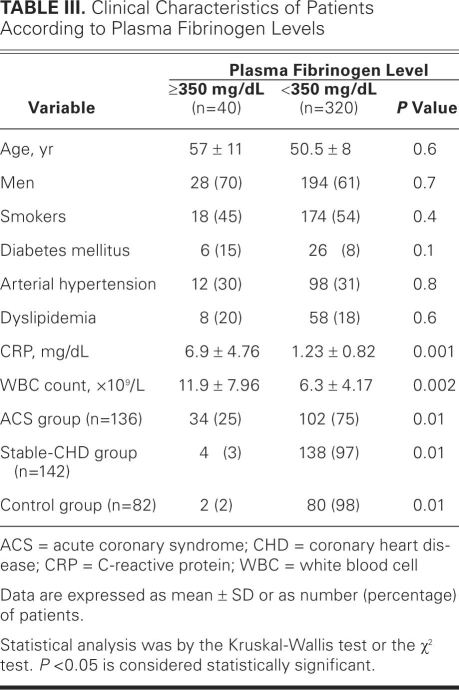
Comparison of Clinical Characteristics According to Plasma-Fibrinogen-Level Subgroups
Table III shows the clinical characteristics among patients who had higher levels of plasma fibrinogen (≥350 mg/dL), and those who had lower levels (<350 mg/dL) at baseline. A significantly higher percentage of patients with ACS (25%) were in the higher-level plasma fibrinogen category than were patients in the stable-CHD group (3%) and the control group (2%) (both P <0.05). In addition, patients who had higher fibrinogen levels generally had a higher WBC count (11.9 ± 7.96 × 109/L) and CRP value (6.9 ± 4.76 mg/dL) than did patients who had lower fibrinogen levels (WBC count, 6.3 ± 4.17 × 109/L; CRP value, 1.23 ± 0.82 mg/dL; both P <0.05). No significant differences were found with respect to age, sex, and other cardiovascular risk factors.
TABLE III. Clinical Characteristics of Patients According to Plasma Fibrinogen Levels
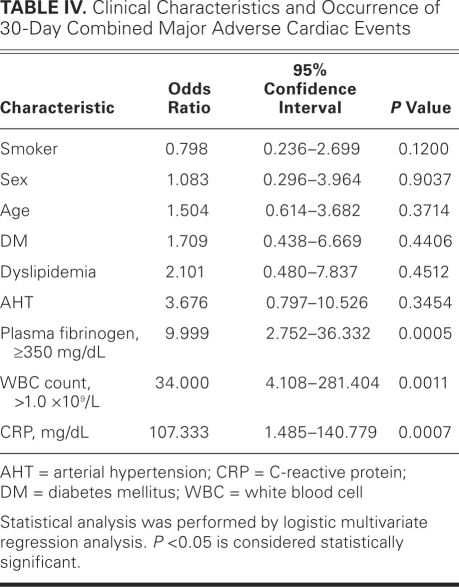
Thirty-Day Clinical Outcomes and Independent Predictors of Combined Endpoints
In a logistic regression analysis, CRP was a significant risk factor that had predictive value, with an odds ratio of 107.333 (95% CI, 1.485–140.779; P=0.0007) (Table IV). In addition, high WBC count (≥1.0 × 109/L) and high plasma fibrinogen level (≥350 mg/dL) were associated with poor short-term prognosis, with respective odds ratios of 34.000 (95% CI, 4.108–281.404; P= 0.0011) and 9.999 (95% CI, 2.752–36.332; P=0.0005). Other variables, such as age, sex, smoking, and a history of diabetes mellitus or arterial hypertension or dyslipidemia, were not significant in this logistic regression analysis.
TABLE IV. Clinical Characteristics and Occurrence of 30-Day Combined Major Adverse Cardiac Events
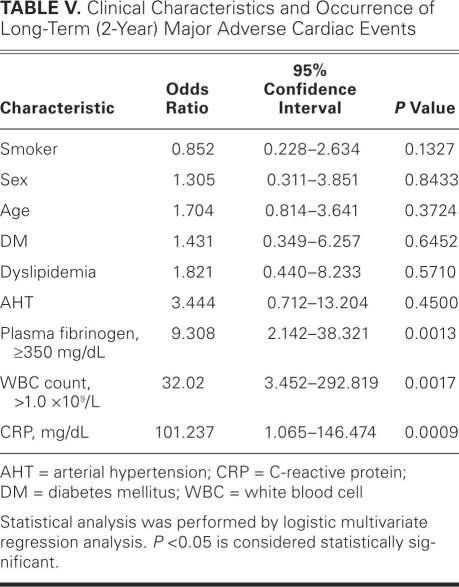
Two-Year Clinical Outcomes and Independent Predictors of Combined Endpoints
In a logistic regression analysis, a fibrinogen level ≥350 mg/dL represented an odds ratio of 9.308 (95% CI, 2.142–38.321; P=0.0013) (Table V). The CRP value maintained its significance in predicting combined MACEs, with an odds ratio of 101.237 (95% CI, 1.065–146.474; P=0.0009). In addition, WBC count of more than 1.0 × 109/L was a significant risk factor to have predictive value, with an odds ratio of 32.02 (95% CI, 3.452–292.819; P=0.0017). Age, sex, and other risk factors were not significant in this logistic regression analysis.
TABLE V. Clinical Characteristics and Occurrence of Long-Term (2-Year) Major Adverse Cardiac Events
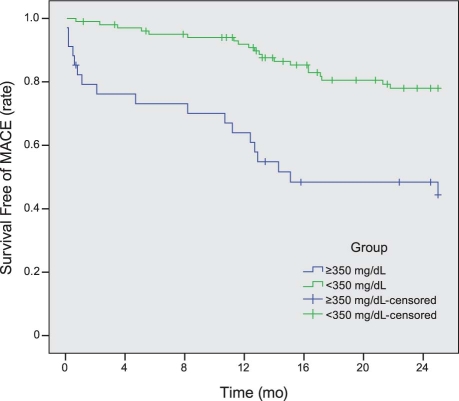
Comparison of Clinical Outcomes on the Basis of Plasma Fibrinogen Level
As seen in Figure 1, a survival analysis (Kaplan-Meier, log-rank by level) showed that patients who had higher levels of fibrinogen had a much worse prognosis than did patients who had lower fibrinogen levels. The increasing progression in the occurrence of MACEs from the lower to higher fibrinogen level is in accord with the results shown in Tables I through V. Figure 1 also shows a significantly higher MACE-free survival rate in patients with lower levels of fibrinogen (P=0.001).
Fig. 1 Fibrinogen level and combined major adverse cardiac events (MACEs) at follow-up. Statistical analysis was performed by Kaplan-Meier analysis (log-rank test).
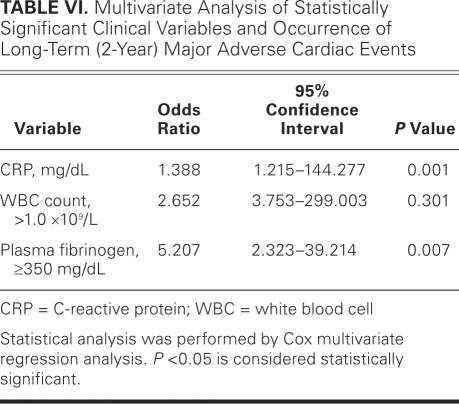
Multivariate Analysis of 2-Year Independent Predictors of Combined Endpoints
In the aforementioned logistic stepwise regression analysis, we evaluated the individual contribution of various risk factors that could have been relevant to the prognosis of patients in the study. Next, in order to determine the predictive value of variables that had a P value of less than 0.05 upon logistic stepwise regression analysis (WBC count, CRP value, and plasma fibrinogen level), we performed a multivariate Cox regression analysis. As Table VI shows, CRP and fibrinogen maintained their significance in predicting MACEs.
TABLE VI. Multivariate Analysis of Statistically Significant Clinical Variables and Occurrence of Long-Term (2-Year) Major Adverse Cardiac Events
Discussion
Although previous studies have reported a strong correlation between plasma fibrinogen concentration and cardiovascular disease risk,5,6 little attention has been paid to the prognostic importance of plasma fibrinogen level in ACS patients. In our study, we found that an elevated baseline fibrinogen level predicts an increased risk of long-term (2-year) MACEs and a worse prognosis in patients who are admitted for the treatment of ACS.
Several epidemiologic studies have confirmed that fibrinogen is a cardiovascular risk factor. In a 2005 meta-analysis of 31 studies with a total of 7,087 CHD cases (in a Western and North American population), a 1-g/L increase in baseline fibrinogen level rendered an age- and sex-adjusted hazard ratio of 2.42 for CHD (95% CI, 2.24–2.6) and a hazard ratio for CHD of approximately 1.8 after further adjustment for measured values of several established vascular risk factors.7 One study from India showed that individuals with fibrinogen levels above 300 mg/dL have an odds ratio of 4.4 (95% CI, 2.4–19) for CHD, which further confirms an association between fibrinogen and CHD.8
Numerous investigations have confirmed the close relationship between inflammation and ACS.9,10 In the development of ACS, impaired vascular walls attract inflammatory cells, such as monocytes and T-lymphocytes.11,12 The interaction between leukocytes and endothelial cells promotes the release of various cytokines (for example, interleukin-6), which stimulate hepatic synthesis of acute-phase reactive proteins, including CRP and fibrinogen.13 The results of our study were in accord with this hypothesis, showing that the plasma fibrinogen level was significantly higher in ACS patients than in stable-CHD patients or healthy control participants. However, further studies are needed to investigate the expression level of other acute-phase reactive proteins—such as factor VIII and von Willebrand factor—in ACS.
Because CRP has long been recognized as a marker that reliably predicts the occurrence of clinical events in ACS patients14,15 (which was further confirmed in our study), plasma fibrinogen may also portend the severity of ACS events. Moreover, because fibrinogen is genetically regulated and directly involved in multiple mechanisms that mediate atherothrombotic processes,16 it becomes an effective predictor of clinical events. For example, fibrinogen can promote endothelial-cell migration17 and extracellular accumulation of low-density lipoproteins.18 Fibrinogen can promote platelet aggregation by interacting with GPIIb/IIIa receptors on the platelet membrane.19 In addition, an elevated level of plasma fibrinogen increases blood viscosity, which causes impaired microcirculatory flow, endothelial shear-stress damage, and predisposition to thrombosis.20 Therefore, an increased level of plasma fibrinogen—participating in thrombosis after rupture of vulnerable plaque—might exacerbate the development of ACS. In accordance with previous studies,21,22 our study showed that patients with ACS who developed clinical events typically had significantly higher fibrinogen levels than did patients who did not experience clinical events. We also demonstrated an association between elevated fibrinogen concentration upon hospital admission and a higher incidence of 2-year MACEs.
Moreover, we observed that WBC count was positively related to ACS. White blood cell count is a long-recognized marker of inflammation, and a high WBC count typically indicates a substantial inflammatory response. Previous studies have shown that elevation of WBC count in acute myocardial infarction is associated with adverse outcomes.23 Our study confirmed a relationship between WBC count and 2-year MACE. We also found higher WBC counts in patients with ACS than in the stable-CHD and control groups, which might indicate a more intense inflammatory response in ACS than in stable CHD, as reflected by CRP value and fibrinogen level.
Conclusion
We found that elevated levels of CRP, WBCs, and plasma fibrinogen are associated with a worse long-term prognosis in patients who have ACS. However, our study is limited by its number of study subjects and by its retrospective nature. Further multicenter clinical and epidemiologic investigations with large populations are needed in order to verify our conclusions.
Acknowledgments
We thank Dr. Tieer Gan of our Department of Pathophysiology for her assistance in data processing and our medical college students for their assiduous data collection.
Footnotes
Drs. Wu and Shi contributed equally to this paper.
Address for reprints: Geng Xu, MD, PhD, Department of Cardiology, Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310009, PRC
E-mail: zjudoctorxugeng@yahoo.cn
References
- 1.Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008;118(17): 1768–75. [DOI] [PubMed]
- 2.Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med 1994;331(7):417–24. [DOI] [PubMed]
- 3.Biasucci LM, Liuzzo G, Grillo RL, Caligiuri G, Rebuzzi AG, Buffon A, et al. Elevated levels of C-reactive protein at discharge in patients with unstable angina predict recurrent instability. Circulation 1999;99(7):855–60. [DOI] [PubMed]
- 4.Clauss A. Rapid physiological coagulation method in determination of fibrinogen [in German]. Acta Haematol 1957;17(4): 237–46. [DOI] [PubMed]
- 5.Fibrinogen as a risk factor in cardiovascular disease. N Engl J Med 1985;312(2):120–1. [DOI] [PubMed]
- 6.Stec JJ, Silbershatz H, Tofler GH, Matheney TH, Sutherland P, Lipinska I, et al. Association of fibrinogen with cardiovascular risk factors and cardiovascular disease in the Framingham Offspring Population. Circulation 2000;102(14):1634–8. [DOI] [PubMed]
- 7.Fibrinogen Studies Collaboration, Danesh J, Lewington S, Thompson SG, Lowe GD, Collins R, et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA 2005;294(14):1799–809. [DOI] [PubMed]
- 8.Jose J, Selvakumar D, Selvakumar R, Kanagasapabathy AS, Jeyaseelan L. Plasma fibrinogen–an independent risk factor for ischaemic heart disease. Indian Heart J 1998;50(1):45–8. [PubMed]
- 9.Mehta JL, Saldeen TG, Rand K. Interactive role of infection, inflammation and traditional risk factors in atherosclerosis and coronary artery disease. J Am Coll Cardiol 1998;31(6): 1217–25. [DOI] [PubMed]
- 10.Becker AE, de Boer OJ, van Der Wal AC. The role of inflammation and infection in coronary artery disease. Annu Rev Med 2001;52:289–97. [DOI] [PubMed]
- 11.Neri Serneri GG, Prisco D, Martini F, Gori AM, Brunelli T, Poggesi L, et al. Acute T-cell activation is detectable in unstable angina. Circulation 1997;95(7):1806–12. [DOI] [PubMed]
- 12.Hosono M, de Boer OJ, van der Wal AC, van der Loos CM, Teeling P, Piek JJ, et al. Increased expression of T cell activation markers (CD25, CD26, CD40L and CD69) in atherectomy specimens of patients with unstable angina and acute myocardial infarction. Atherosclerosis 2003;168(1):73–80. [DOI] [PubMed]
- 13.Castell JV, Gomez-Lechon MJ, David M, Fabra R, Trullenque R, Heinrich PC. Acute-phase response of human hepatocytes: regulation of acute-phase protein synthesis by interleukin-6. Hepatology 1990;12(5):1179–86. [DOI] [PubMed]
- 14.Rebuzzi AG, Quaranta G, Liuzzo G, Caligiuri G, Lanza GA, Gallimore JR, et al. Incremental prognostic value of serum levels of troponin T and C-reactive protein on admission in patients with unstable angina pectoris. Am J Cardiol 1998;82 (6):715–9. [DOI] [PubMed]
- 15.Blake GJ, Ridker PM. C-reactive protein and other inflammatory risk markers in acute coronary syndromes. J Am Coll Cardiol 2003;41(4 Suppl S):37S–42S. [DOI] [PubMed]
- 16.Humphries SE. Genetic regulation of fibrinogen. Eur Heart J 1995;16 Suppl A:16–20. [DOI] [PubMed]
- 17.Dejana E, Languino LR, Polentarutti N, Balconi G, Ryckewaert JJ, Larrieu MJ, et al. Interaction between fibrinogen and cultured endothelial cells. Induction of migration and specific binding. J Clin Invest 1985;75(1):11–8. [DOI] [PMC free article] [PubMed]
- 18.Retzinger GS, DeAnglis AP, Patuto SJ. Adsorption of fibrinogen to droplets of liquid hydrophobic phases. Functionality of the bound protein and biological implications. Arterioscler Thromb Vasc Biol 1998;18(12):1948–57. [DOI] [PubMed]
- 19.Bodary SC, Napier MA, McLean JW. Expression of recombinant platelet glycoprotein IIbIIIa results in a functional fibrinogen-binding complex. J Biol Chem 1989;264(32):18859–62. [PubMed]
- 20.Lowe GD, Fowkes FG, Dawes J, Donnan PT, Lennie SE, Housley E. Blood viscosity, fibrinogen, and activation of coagulation and leukocytes in peripheral arterial disease and the normal population in the Edinburgh Artery Study. Circulation 1993;87(6):1915–20. [DOI] [PubMed]
- 21.Toss H, Lindahl B, Siegbahn A, Wallentin L. Prognostic influence of increased fibrinogen and C-reactive protein levels in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. Circulation 1997;96(12):4204–10. [DOI] [PubMed]
- 22.Becker RC, Cannon CP, Bovill EG, Tracy RP, Thompson B, Knatterud GL, et al. Prognostic value of plasma fibrinogen concentration in patients with unstable angina and non-Q-wave myocardial infarction (TIMI IIIB Trial). Am J Cardiol 1996;78(2):142–7. [DOI] [PubMed]
- 23.Pellizzon GG, Dixon SR, Stone GW, Cox DA, Mattos L, Boura JA, et al. Relation of admission white blood cell count to long-term outcomes after primary coronary angioplasty for acute myocardial infarction (The Stent PAMI Trial). Am J Cardiol 2003;91(6):729–31. [DOI] [PubMed]