Abstract
Reduced door-to-balloon time in primary percutaneous coronary intervention for the treatment of ST-elevation myocardial infarction has been associated with lower cardiac mortality rates. However, it remains unclear whether door-to-balloon time is predominantly a surrogate for overall peri-myocardial infarction care and is not independently predictive of outcomes, particularly when differences in door-to-balloon time have narrowed and previous studies have contained myocardial infarction-selection bias.
We analyzed 179 consecutive patients who presented emergently at our cardiac catheterization laboratory with ST-elevation myocardial infarction within 12 hours of symptom onset and who underwent primary percutaneous coronary intervention within 3 hours of presentation. Our curve estimation regression model used the natural logarithm (ln) of area under the curve (AUC) of creatine kinase to evaluate the effect of door-to-balloon time on cardiac biomarker levels. We correlated ln (AUC–creatine kinase) with improvement of left ventricular ejection fraction at follow-up and with the intermediate-term mortality rate.
Median door-to-balloon time was 87 minutes (interquartile range, 65–113 min). The ln (AUC–creatine kinase) correlated significantly with door-to-balloon time (r=0.2, P=0.02). Upon propensity-score analysis, door-to-balloon time remained a significant independent predictor of ln (AUC–creatine kinase) (β=0.15, P=0.03). Upon use of a Cox regression model, ln (AUC–creatine kinase) independently predicted death (P=0.04) and recovery of left ventricular function (P=0.001) at follow-up (mean, 14 mo).
Longer door-to-balloon time independently predicts increased myocardial cell damage, and ln (AUC–creatine kinase) predicts improvement in left ventricular systolic function and intermediate-term death after ST-elevation myocardial infarction.
Key words: Angioplasty, transluminal, percutaneous coronary/standards/statistics & numerical data; linear models; multivariate analysis; myocardial infarction/mortality/physiopathology/therapy; myocardial reperfusion/methods; myocardial revascularization/utilization; practice guidelines as topic/standards; regression analysis; time factors; treatment outcome
Primary percutaneous coronary intervention (PCI) is the preferred method of treatment for ST-elevation myocardial infarction (STEMI) if it can be performed in a timely manner. The American College of Cardiology/American Heart Association guidelines for the treatment of STEMI state that PCI is the favored approach if an institution can achieve a door-to-balloon time (DBT) of no longer than 90 minutes.1 This benchmark time is derived from multiple studies that show that shorter DBTs are associated with improved clinical outcomes.2–14 However, nearly all of these studies have been multicenter trials, which makes it unclear whether DBT is a surrogate of volume and overall institutional expertise rather than an independent predictor of outcomes. It has been shown that high-volume cardiac-care institutions have shorter DBTs, which may drive the primary results of multicenter data.15 Primary PCI volume also strongly correlates with post-myocardial infarction (MI) survival. Since all-cause death is typically the endpoint and is a variable that often depends upon overall quality of care in STEMI, institutional expertise in MI management is a strong confounder and a hidden predictor in these studies. For instance, when comparing off-hours care with weekday care (during which in-hospital MI care would be similar within the same institution), previous studies have reported similar outcomes despite significantly longer DBTs in the off-hours patient groups.16,17 Moreover, many of these trials have included patients with DBTs of longer than 3 hours, which likely adds MI-selection bias.5,9,10
In this study, we have considered the amount of myocardial necrosis, as measured by the creatine kinase (CK) area under the curve (AUC), to be the most accurate measure of the direct, independent, and immediate benefit of reduced DBT. Moreover, by analyzing outcomes from a single institution and narrowing the criteria to include only truly emergent STEMI cases with early intervention, we have eliminated both the confounder of the treating institution and that of MI-selection bias. We sought to determine whether DBT is independently predictive of myocardial necrosis after STEMI and whether that myocardial necrosis predicts intermediate-term death and recovery of left ventricular ejection fraction (LVEF).
Patients and Methods
Using our institution's PCI registry, we analyzed a study population of 179 consecutive STEMI patients who presented at our emergency department from January 2005 through December 2008 in whom primary PCI was performed. Patients were selected for analysis if their symptoms were of no longer than 12 hours' duration and their DBT was shorter than 3 hours. Patients were included only when there was documented electrocardiographic evidence of ST-segment elevations of more than 1 mm in 2 contiguous leads, ST-segment depression of more than 1 mm in leads V1 and V2 (with R>S in lead V1 or V2), or a documented new left bundle branch block. Serial, timed CK levels were obtained for all patients and plot-fitted, and the AUC was integrated and measured. A curve estimation regression model18 using the natural logarithm (ln) of AUC was used to evaluate the effect of DBT on the cardiac biomarker level of CK. Angiographic and clinical variables, including the presence of multivessel coronary artery disease (defined as >2 epicardial vessels with stenoses ≥70%), baseline LVEF on ventriculography, infarct location (anterior or other), and Thrombolysis in Myocardial Infarction (TIMI) risk score for STEMI were recorded. Body surface area was calculated for all patients in accordance with the DuBois method. Chest pain-to-presentation time (CPT) was also recorded for all patients. Follow-up LVEF (obtained at least 1 month after the index infarct) was determined with the use of echocardiography or nuclear imaging so that the degree of LVEF recovery could be measured. In order to determine the independent effect of the continuous variable DBT on ln (AUC–CK), we used multiple linear regression in which we included clinical and angiographic variables. We performed a propensity-score analysis in order to predict the likelihood of a patient's having a DBT of longer than 90 minutes on the basis of available baseline characteristics and actual DBTs. This predicted probability was a separate variable that we also entered into the regression model in an effort to reduce MI-selection bias further. Standardized β-coefficients were calculated to reflect the relative weight of each significant variable in the overall model. Using multivariate regression analysis, we then determined whether ln (AUC–CK) was predictive of death and of recovery of LVEF at follow-up. All P values less than 0.05 were considered statistically significant. We used SPSS version 12.0 software (SPSS, Inc.; Chicago, Ill) for all statistical analyses.
Results
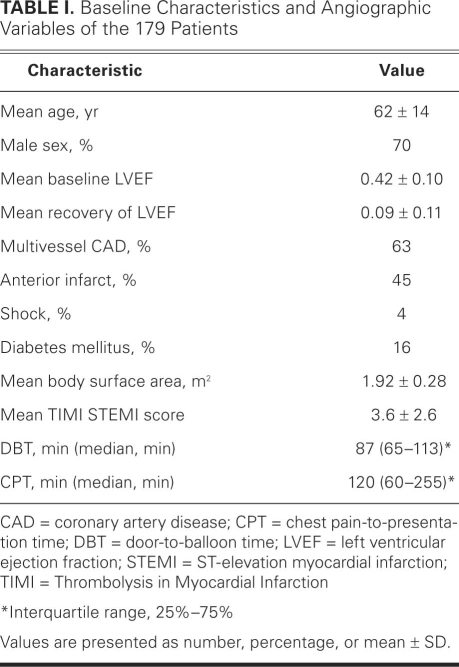
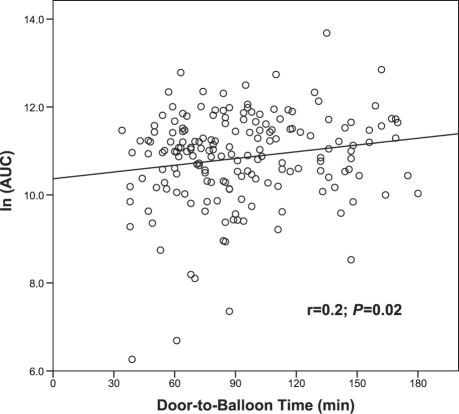
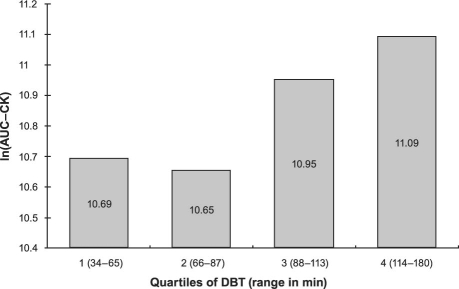
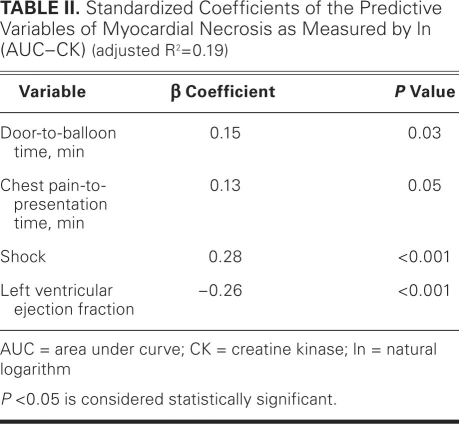
Table I shows the mean TIMI STEMI scores for the 179 patients, and the frequencies and means of the clinical and angiographic variables. Mortality rate data were obtained for all patients, and LVEF recovery data were determined for 79% of the patients. The median DBT was 87 minutes (interquartile range, 65–113 min) and the mean TIMI STEMI risk score was 3.6 ± 2.6. Figure 1 shows the relationship between DBT and ln (AUC–CK), and the significant, linear correlation of ln (AUC–CK) with respect to DBT (r=0.2, P=0.02). Figure 2 shows the mean ln (AUC–CK) for the DBT quartiles. Upon propensity-score analysis with multiple linear regression of variables (including CPT, multivessel disease, anterior infarct and hemodynamic status, and TIMI STEMI risk score), DBT remained a significant independent predictor of ln (AUC–CK) (β=0.15, P=0.03), as did CPT (β=0.13, P=0.05). Table II shows the standardized coefficients of the model (β). Upon the use of a multivariate Cox regression model, ln (AUC–CK) was a significant independent predictor of recovery of LVEF (P=0.001) and of death (P=0.04) at a mean follow-up time of 14 months (Table III).
TABLE I. Baseline Characteristics and Angiographic Variables of the 179 Patients
Fig. 1 Curve estimation model of the natural logarithm of the area under curve (ln [AUC]) of creatine kinase versus door-to-balloon time.
Fig. 2 Categorical relationship of the natural logarithm of the area under curve of creatine kinase (ln [AUC–CK]) versus door-to-balloon time (DBT).
TABLE II. Standardized Coefficients of the Predictive Variables of Myocardial Necrosis as Measured by ln (AUC–CK) (adjusted R2=0.19)
TABLE III. Multivariate Predictors of Intermediate-Term Death
Discussion
Our analysis is the first to rigorously evaluate the direct predictive value of DBT on myocardial necrosis, as measured by the AUC of CK, by avoiding biases due to quality of care, institutional expertise, and PCI volume. The lower ln (AUC–CK) observed in patients with shorter DBTs translates into an improvement of LVEF at follow-up and to a reduction in the intermediate-term mortality rate.
Substantial resources have been used by PCI centers to improve outcomes in STEMI, with a particular emphasis on DBT.19,20 Door-to-balloon time is easily measurable, and it has been used as a marker of quality of care. The preponderance of the clinical evidence regarding treatment times in STEMI suggests that a shorter DBT translates directly into a more favorable outcome. Numerous studies have shown a correlation between DBT and death. The “time is myocardium” mantra makes intuitive sense, because it is logical to conclude that the more quickly an artery can be opened and the coronary flow restored, the less myocardial damage will occur. This correlation is nearly indisputable, but the presence of a strong direct causation between DBT and outcomes is less clear, particularly if differences in DBT are narrowed to minutes.21 All prior DBT trials have been retrospective studies that have involved large, multicenter databases, or they have been post hoc analyses of randomized trials.2–25 The ethics of randomizing patients to a delayed-treatment approach in STEMI are clearly prohibitive, so our data must come from the existing analyses. The results enable us to conclude that cases with short DBTs are associated with superior outcomes.
Nevertheless, the desirability of attaining short DBT should not obfuscate the heavy selection bias that is involved in all of the data to date. Confounders are present in these analyses, foremost among which is whether DBT is simply a surrogate variable for institutional level of expertise. Many studies have shown that centers with higher primary PCI volume or greater expertise in STEMI achieve shorter DBTs.15 It has also been shown that high-volume institutions have lower mortality rates in primary PCI.22 These same institutions tend to adhere more to clinical guidelines for overall MI management and have lower mortality rates for cardiac disease in general. However, in the models of these studies, a center's level of expertise is rarely considered to be a confounder—and, as a result, the independent effect of DBT is less certain. For example, an analysis involving only hospitals that participated in the American Heart Association's “Get With the Guidelines” program16 (motivated, high-volume centers) showed that patients who presented with MI during off-hours had longer DBTs but similar rates of major acute cardiac events in comparison with patients who presented during weekday hours. This suggests that outcomes have more to do with overall hospital care (which should be similar whether the initial presentation is during off-hours or on a weekday) rather than with DBT itself. Our study involves only a single institution and eliminates this confounder. Scientifically, a more direct endpoint should be used when attempting to define a DBT effect on outcomes. Our endpoint is not tied to confounders and is more strictly a result of time to coronary reperfusion. Moreover, in our analysis, the higher ln (AUC–CK) that resulted from longer DBT translates to a higher intermediate-term mortality rate and lack of improvement in LVEF.
Selection bias in the analysis of DBT cohorts is inherently present in all of the prior analyses. Multiple studies have shown that patients with longer DBTs tend to be more ill overall.2,3,9,23 Patients with DBTs of longer than 90 minutes are approximately 3 times more likely to be categorized as baseline Killip class ≥2 than are patients whose DBT is 60 minutes or shorter.2 It is generally more difficult to intervene quickly in patients who are in more unstable condition and more critically ill, given the potential need to stabilize these patients from a hemodynamic or respiratory standpoint before angiography. Most of the large databases are unable to correct for this selection bias, and this bias may account for higher mortality rates when DBTs are longer. Moreover, some studies have found a U-shaped response of time-related outcomes, with lower peak CK levels and mortality rates in patients who had either very short or very long DBTs—again indicating an uncorrected selection bias.3,4,24 Our study's propensity-score analysis minimizes this bias and confirms that DBT is independently predictive. In addition, previous reports that dealt with myocardial necrosis and DBT included patients who experienced very long DBTs (>3 hr).25 Our DBTs were fairly narrow (interquartile range, within 113 min) because our analysis excluded patients whose DBTs were longer than 3 hours.
Intuitively, CPT predicts outcome just as strongly as does DBT. Although many studies have considered CPT,5–8,15 few have determined its interaction with DBT and its significance with respect to outcomes. Door-to-balloon time is typically a fraction of CPT—CPT more accurately reflects the overall time of coronary artery occlusion. Even with the introduction of CPT into our model, CPT and DBT both remained strong predictors of myocardial necrosis. The standardized β-coefficients of DBT and CPT are approximately half the weight of those of shock and LVEF, indicating the relative importance of the first 2 variables compared with the second 2. Of note, our study considered only patients whose DBTs were shorter than 3 hours, unlike other studies, which directly analyzed myocardial necrosis and included outlying DBTs.25 Despite our tighter temporal distribution of DBT, there was still a significant linear association of DBT to ln (AUC–CK).
Our study has several important limitations. Because the study is a single-center analysis, the sample size is relatively small and may not fully account for the heterogeneity in infarct size, CK levels, infarct location, and differences in TIMI flow among STEMIs. Although we factored in body surface area, differences in cardiac size among patients may also contribute to differences in enzyme levels.
Footnotes
Address for reprints: Robert M. Minutello, MD, 525 E. 68th St., F-439, New York Presbyterian Hospital (Cornell Campus), New York, NY 10065
E-mail: RMM2002@med.cornell.edu
References
- 1.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published erratum appears in J Am Coll Cardiol 2008;51(9):977]. J Am Coll Cardiol 2008; 51(2):210–47. [DOI] [PubMed]
- 2.Berger PB, Ellis SG, Holmes DR Jr, Granger CB, Criger DA, Betriu A, et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation 1999;100(1):14–20. [DOI] [PubMed]
- 3.Brodie BR, Stuckey TD, Muncy DB, Hansen CJ, Wall TC, Pulsipher M, Gupta N. Importance of time-to-reperfusion in patients with acute myocardial infarction with and without cardiogenic shock treated with primary percutaneous coronary intervention. Am Heart J 2003;145(4):708–15. [DOI] [PubMed]
- 4.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol 2003;92(7):824–6. [DOI] [PubMed]
- 5.Zijlstra F, Patel A, Jones M, Grines CL, Ellis S, Garcia E, et al. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2–4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J 2002;23(7):550–7. [DOI] [PubMed]
- 6.Antoniucci D, Valenti R, Migliorini A, Moschi G, Trapani M, Buonamici P, et al. Relation of time to treatment and mortality in patients with acute myocardial infarction undergoing primary coronary angioplasty. Am J Cardiol 2002;89(11): 1248–52. [DOI] [PubMed]
- 7.De Luca G, Suryapranata H, Zijlstra F, van 't Hof AW, Hoorntje JC, Gosselink AT, et al. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol 2003;42 (6):991–7. [DOI] [PubMed]
- 8.McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2006;47(11):2180–6. [DOI] [PubMed]
- 9.Brodie BR, Hansen C, Stuckey TD, Richter S, Versteeg DS, Gupta N, et al. Door-to-balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol 2006;47(2):289–95. [DOI] [PubMed]
- 10.Brodie BR, Stone GW, Cox DA, Stuckey TD, Turco M, Tcheng JE, et al. Impact of treatment delays on outcomes of primary percutaneous coronary intervention for acute myocardial infarction: analysis from the CADILLAC trial. Am Heart J 2006;151(6):1231–8. [DOI] [PubMed]
- 11.Nallamothu B, Fox KA, Kennelly BM, Van de Werf F, Gore JM, Steg PG, et al. Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart 2007;93(12):1552–5. [DOI] [PMC free article] [PubMed]
- 12.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM; NRMI Investigators. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation 2005; 111(6):761–7. [DOI] [PubMed]
- 13.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004;109(10):1223–5. [DOI] [PubMed]
- 14.Nallamothu BK, Antman EM, Bates ER. Primary percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: does the choice of fibrinolytic agent impact on the importance of time-to-treatment? Am J Cardiol 2004;94(6):772–4. [DOI] [PubMed]
- 15.Nallamothu BK, Wang Y, Magid DJ, McNamara RL, Herrin J, Bradley EH, et al. Relation between hospital specialization with primary percutaneous coronary intervention and clinical outcomes in ST-segment elevation myocardial infarction: National Registry of Myocardial Infarction-4 analysis. Circulation 2006;113(2):222–9. [DOI] [PubMed]
- 16.Jneid H, Fonarow GC, Cannon CP, Palacios IF, Kilic T, Moukarbel GV, et al. Impact of time of presentation on the care and outcomes of acute myocardial infarction. Circulation 2008;117(19):2502–9. [DOI] [PubMed]
- 17.Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 2005;294(7):803–12. [DOI] [PubMed]
- 18.Turer AT, Mahaffey KW, Gallup D, Weaver WD, Christenson RH, Every NR, Ohman EM. Enzyme estimates of infarct size correlate with functional and clinical outcomes in the setting of ST-segment elevation myocardial infarction. Curr Control Trials Cardiovasc Med 2005;6:12. [DOI] [PMC free article] [PubMed]
- 19.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 2006;355(22): 2308–20. [DOI] [PubMed]
- 20.Le May MR, So DY, Dionne R, Glover CA, Froeschl MP, Wells GA, et al. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med 2008; 358(3):231–40. [DOI] [PubMed]
- 21.Zahn R, Vogt A, Zeymer U, Gitt AK, Seidl K, Gottwik M, et al. In-hospital time to treatment of patients with acute ST elevation myocardial infarction treated with primary angioplasty: determinants and outcome. Results from the registry of percutaneous coronary interventions in acute myocardial infarction of the Arbeitsgemeinschaft Leitender Kardiologischer Krankenhausarzte. Heart 2005;91(8):1041–6. [DOI] [PMC free article] [PubMed]
- 22.Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283(22):2941–7. [DOI] [PubMed]
- 23.Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation 2006;114(19):2019–25. [DOI] [PubMed]
- 24.Boersma E; Primary Coronary Angioplasty vs. Thrombolysis Group. Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. Eur Heart J 2006;27(7):779–88. [DOI] [PubMed]
- 25.Stone GW, Dixon SR, Grines CL, Cox DA, Webb JG, Brodie BR, et al. Predictors of infarct size after primary coronary angioplasty in acute myocardial infarction from pooled analysis from four contemporary trials. Am J Cardiol 2007;100(9): 1370–5. [DOI] [PubMed]