Abstract
A 91-year-old woman, presenting with flu-like symptoms, developed a brief episode of polymorphic ventricular tachycardia in the emergency department. The arrhythmia resolved spontaneously, and a subsequent electrocardiogram revealed Q waves and ST-segment elevation in the anterior precordial leads, along with a prolonged QT interval. The presumed diagnosis was ST-segment–elevation myocardial infarction with ischemia-induced ventricular tachycardia. Emergent coronary artery angiography revealed only minimal luminal irregularities. It was discovered that the patient had been taking levofloxacin and, apparently as a result, developed drug-induced torsades de pointes. The case of this patient is an example of the difficulties that are occasionally encountered in differentiating ST-segment–elevation myocardial infarction from nonischemic ST elevation.
Key words: Aged, 80 and over; antibacterial agents/adverse effects; arrhythmias, cardiac/chemically induced; electrocardiography; fluoroquinolones/adverse effects; myocardial infarction/diagnosis; torsades de pointes/chemically induced/etiology
An elderly woman presented at the emergency department with nonspecific flu-like symptoms. During an electrocardiogram (ECG), she developed polymorphic ventricular tachycardia, which resolved spontaneously. A subsequent ECG revealed ST-segment elevation in the anterior precordial leads, along with a prolonged QT interval. Herein, we discuss the reasons behind the ECG irregularities and note the difficulties that are occasionally encountered in differentiating ST-segment–elevation myocardial infarction from nonischemic ST elevation.
Case Report
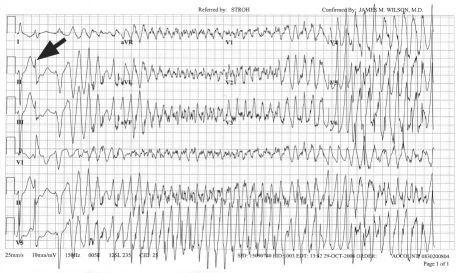
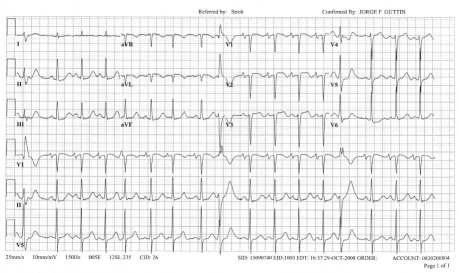
In October 2008, a 91-year-old woman without any relevant medical history presented at the hospital with nausea and epigastric discomfort. She had experienced flu-like symptoms for a few days. Her grandson, a physician, had prescribed a course of levofloxacin 2 days earlier. Upon her arrival at the emergency room, she was alert and hemodynamically stable. During a 12-lead ECG, she lost consciousness. The ECG showed wide QRS-complex tachycardia that spontaneously converted to sinus rhythm after 20 seconds, whereupon the patient regained consciousness (Fig. 1). An immediately repeated ECG showed Q waves in leads aVL and V1 through V2 with ST elevation in leads aVL and V1 through V3 (Fig. 2). No prior ECGs were available. In accordance with the presumed diagnosis of ST-elevation myocardial infarction, the catheterization laboratory was activated. Emergent coronary artery angiography revealed only minimal luminal irregularities and no evidence of an occlusive thrombus. Cardiac markers were not elevated, and an echocardiogram showed no regional wall-motion abnormalities.
Fig. 1 Initial portion of an electrocardiogram shows a premature ventricular beat that fell on the end of the preceding T wave (arrow), which initiated an episode of polymorphic ventricular tachycardia.
Fig. 2 An electrocardiogram, obtained after the ventricular tachycardia resolved, shows Q waves in leads aVL and V1 through V2, with ST-segment elevation in leads aVL and V1 through V3. Sinus rhythm with premature ventricular beats can be seen, along with a markedly prolonged QT interval.
Discussion
Before catheterization, the episode of ventricular arrhythmia was believed to have been precipitated by myocardial ischemia, given the ST-segment elevations on the 2nd ECG. Upon closer inspection of the initial ECG, it appeared that the polymorphic ventricular tachycardia was preceded by a premature ventricular beat that fell on the preceding T wave (R-on-T phenomenon). Indeed, on the 2nd ECG, the corrected QT interval was markedly prolonged, establishing the diagnosis of torsades de pointes. In this instance, prolongation of the QT interval was likely induced by a fluoroquinolone antibiotic1 and exacerbated by hypomagnesemia (the magnesium level upon presentation was 1.4 mg/dL). Female sex is also a risk factor for torsades de pointes—in particular, elderly women are much more likely than are elderly men to develop drug-induced QT prolongation.2
The cause of the anterior ST-segment changes is more difficult to explain. Repolarization changes associated with left ventricular hypertrophy can produce a similar pattern. Although the ECG did not meet voltage criteria, a transthoracic echocardiogram did reveal mild concentric left ventricular hypertrophy. The presence of Q waves in leads V1 through V2 may indicate persistent ST changes from a remote Q-wave myocardial infarction. The echocardiogram, however, did not show any regional wall-motion abnormalities. Accordingly, it might be that the “septal” Q waves were related to left ventricular hypertrophy.
Occasionally, ST-segment elevation is seen after transthoracic cardioversion.3 In this instance, however, the ventricular arrhythmia reverted to sinus rhythm spontaneously, and electric cardioversion was not required. Nevertheless, mild nonischemic ST elevation in the precordial leads is commonly seen, and in many cases it is difficult to differentiate ST-elevation myocardial infarction from nonischemic ST elevation.4 An ECG that was performed before the patient's discharge from the hospital revealed persistence of the ST changes and normalization of the QT interval.
Footnotes
Address for reprints: Yochai Birnbaum, MD, Department of Medicine, Section of Cardiology, Suite 9.32, BCM 620, Baylor College of Medicine, 1709 Dryden Rd., Houston, TX 77030
E-mail: ybirnbau@bcm.edu
References
- 1.Falagas ME, Rafailidis PI, Rosmarakis ES. Arrhythmias associated with fluoroquinolone therapy. Int J Antimicrob Agents 2007;29(4):374–9. [DOI] [PubMed]
- 2.Paran Y, Mashav N, Henis O, Swartzon M, Arbel Y, Justo D. Drug-induced torsades des pointes in patients aged 80 years or more. Anadolu Kardiyol Derg 2008;8(4):260–5. [PubMed]
- 3.Ben-Dov IZ, Leibowitz D, Weiss AT. ST-segment elevation post cardioversion: a current of injury without injury. Int J Cardiol 2006;106(2):255–6. [DOI] [PubMed]
- 4.Jayroe JB, Spodick DH, Nikus K, Madias J, Fiol M, De Luna AB, et al. Differentiating ST elevation myocardial infarction and nonischemic causes of ST elevation by analyzing the presenting electrocardiogram. Am J Cardiol 2009;103(3):301–6. [DOI] [PubMed]