Abstract
The idea that traction on the subcutaneous musculoaponeurotic system (SMAS) deepens the nasolabial crease has been propagated through the plastic surgery literature. This notion is contrary to the senior author’s experience. The purpose of the present study was to investigate the effects of mobilization of the SMAS on the nasolabial fold and crease. Intraoperative examination on the effect of traction on the SMAS was performed. Ten consecutive primary facelift patients underwent facelift procedures with SMAS support. Following mobilization of the SMAS, traction was placed on the SMAS without traction on the skin. In all cases, the nasolabial fold was effaced and the nasolabial crease did not deepen. The authors concluded that traction on the SMAS did not deepen the nasolabial crease.
Keywords: Nasolabial crease, Nasolabial fold, SMAS
Abstract
La notion selon laquelle une traction exercée sur le système musculo-aponévrotique sous-cutané approfondit le pli nasogénien s’est propagée dans la littérature en chirurgie plastique. Or, cette notion ne concorde pas avec les observations de l’auteur principal. Le but de la présente étude était d’évaluer les effets d’une mobilisation du système musculo-aponévrotique sous-cutané sur le pli et le sillon nasogéniens. L’auteur a procédé à un examen peropératoire de l’effet de la traction sur le système. Dix patients consécutifs soumis à un redrapage facial primaire on subit l’intervention avec soutien du système. Après mobilisation du système, la traction a été exercée sur le système, et non sur la peau. Dans tous les cas, le pli nasogénien a été effacé et le sillon nasogénien ne s’est pas approfondi. Les auteurs en ont conclu que la traction exercée sur le système musculo-aponévrotique sous-cutané n’a pas approfondi le pli nasogénien.
Facelift surgery has evolved significantly over the past century. In the early 20th century, facelifting largely consisted of skin excision with or without skin undermining. Skoog (1) ushered in the era of subcutaneous musculoaponeurotic system (SMAS) surgery following the publication of his textbook in 1974. The effect of the Skoog facelift allowed for a more vascularized flap along with distinct improvement in the jawline (2). It may have also produced a longer lasting and more predictable result (3). However, there are limitations to the Skoog procedure, which include a decreased amount of effect in the anterior cheek, nasolabial fold and periorbital areas (2).
Treatment of the nasolabial fold has received a great deal of attention in the literature, even garnering a complete issue of Clinics in Plastic Surgery (4). There have been many publications and letters (2–11) examining the treatment of the nasolabial fold and the relationship of the SMAS to the nasolabial fold. In many of these publications, the authors have stated that traction on the SMAS results in a deepening of the nasolabial crease. At the 2008 Annual Meeting of the American Society for Aesthetic Plastic Surgery, held in San Diego, California (USA), one of the panelists reviewing nasolabial fold treatment stated that traction on the SMAS layer resulted in deepening of the nasolabial fold.
The experiences of these surgeons are clearly in contrast with that of the senior surgeon, who has performed more than 1000 SMAS facelift procedures over the past decade. The purpose of the present study is to report on the effects of SMAS surgery on the nasolabial fold.
METHODS
The surgical technique has been published elsewhere and will be reviewed briefly in the present article (12). The temporal and occipital incisions are planned based on the amount of skin shift associated with the facelift. The preauricular incision follows the curve of the helical rim, and then runs along the margin of the tragus to the colour change at the inferior aspect of the tragus. At the inferior aspect of the tragus, the incision turns perpendicular and then turns perpendicular again to run inferior adjacent to the earlobe. A small cuff of skin is left attached to the inferior aspect of the earlobe. The postauricular incision extends close to the postauricular sulcus until it turns to join the occipital incision. A submental incision is placed posterior to the submental crease. The skin is undermined anteriorly only as far as necessary to permit a different directional shift of the skin from the directional shift of the SMAS, which is usually in a more superior direction. The anterior cheek, which has connections from the SMAS to the skin, is not undermined because this would lose a major support of the SMAS to the incisions in the temporal area and would not result in the pleasing concavity that occurs when the attachments from the anterior SMAS to the skin are left intact. The rotation point of the SMAS is planned so that there is an enhancement of the projection over the malar area. The neck is dissected caudally to below the level of the cricoid cartilage. Through the submental incision, the submental crease and the osseocutaneous mandibular ligaments are released. No attempt is made to release the mandibular ligaments in the sub-SMAS plane.
The SMAS flap is then elevated. The amount of release is performed based on the preoperative assessment of the patient’s needs. The transverse limb of the SMAS incision is typically above or at the superior border of the zygomatic arch and extends medially through some of the inferior portion of the orbicularis oculus muscle and out to the malar pivot point. The inferior limb of the SMAS incision runs approximately 1 cm anterior to the tragus and extends inferiorly into the neck within 1 cm of the anterior border of the sternocleidomastoid muscle. Division of the SMAS is performed between two Allis clamps that lift the SMAS to avoid injury to the facial nerve. The SMAS is then grasped with the Allis clamps, and the SMAS flap is raised before releasing the zygomatic ligaments and masseteric cutaneous ligaments. When the desired effect occurs with traction on the SMAS, the undermining is discontinued. The SMAS flap can then be advanced posteriorly and superiorly and stapled temporarily into position. The flap may be bifurcated or trifurcated as needed.
Once the SMAS flap has been mobilized, modifications to the neck are performed. These modifications include transection of the platysma, defatting of the neck with open liposuction or direct defatting, removal of subplatysmal fat, tangential resection of the digastric muscle and reduction of the submandibular glands. The submental fascia is approximated and invaginated to prevent hollowing under the neck.
The SMAS flaps are then overlapped superiorly to the temporal fascia. The donor site of the preauricular SMAS flap rotated in the occipital area is equivalent to a SMASectomy, and the occipital flap is rotated below the angle of the jaw to suture to the fascia over the mastoid. Drains are placed and the excess tissue is moved in a direction that produces an effect. The excess skin is excised and sutured into place.
The following procedure was performed in 10 consecutive patients. The SMAS flap was elevated as described above. The depth of the nasolabial crease was noted, and a photograph of the area of the nasolabial crease and fold was taken. Traction on the SMAS layer was then performed with Allis clamps in a posterior and superior direction. There was no traction or tension placed onto the skin. Another photograph was then taken of the area of the nasolabial crease and fold with traction on SMAS.
RESULTS
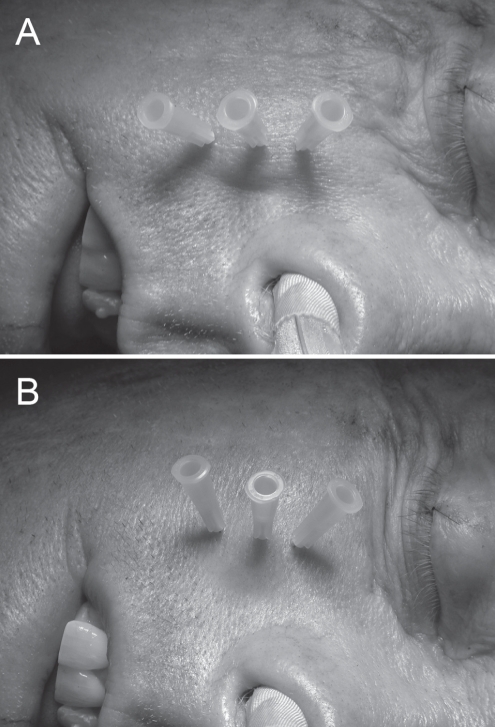
The intraoperative photographs demonstrate the effect of superolateral traction on the SMAS. The applied force was only applied to the SMAS, with no tension applied to the overlying skin layer. The photographs clearly demonstrate that traction on the SMAS alone results in a flattening of the nasolabial fold and a reduction in the depth of the nasolabial crease (Figures 1 and 2). Traction on the fascia of the zygomaticus major and zygomaticus minor muscles resulted in deepening of the nasolabial crease.
Figure 1).
A Intraoperative photograph of the nasolabial fold before subcutaneous musculoaponeurotic system elevation and mobilization. B Intraoperative photograph of the nasolabial fold following subcutaneous musculoaponeurotic system elevation and insetting without any traction on the skin demonstrating clear effacement of the nasolabial fold. The nasolabial crease has not deepened
Figure 2).
A Intraoperative photograph of the nasolabial fold before subcutaneous musculoaponeurotic system elevation and mobilization. B Intraoperative photograph of nasolabial fold following subcutaneous musculoaponeurotic system elevation and insetting without any traction on the skin. Again, the nasolabial fold is flatter and the nasolabial crease has not deepened
DISCUSSION
The treatment of the nasolabial fold has garnered a great deal of attention in the literature. Many different techniques have been applied to either flatten the fold or to fill the nasolabial crease in an effort to improve this area of the face. Appropriately, the proper terminology should be used for description of the anatomy of this region. The nasolabial crease is the line that defines the junction between the nasolabial fold laterally and the upper lip medially. Webster et al (5) have termed the nasolabial crease as the buccolabial groove. Descriptions in the literature have frequently used the term nasolabial fold for both the crease and the fold of tissue lateral to the crease, often in the same publication (8,13,14). In their paper on the nasolabial fold, Yousif et al (8) describe two effects following elevation of the SMAS with subsequent traction on the SMAS. The first effect they noted was that the upper lip was elevated; the second effect was that the nasolabial fold was made deeper. However, if the nasolabial fold was deepened (ie, made less superficial), then the appearance would actually be improved and the nasolabial fold would be flattened. Rubin et al (13) performed an anatomical study of the nasolabial fold; however, the area designated as the nasolabial fold was clearly the nasolabial crease.
Webster et al (5,6) have been credited as being among some of the first investigators to propagate the idea that traction on the SMAS deepens the nasolabial crease. Larson (3) supports this point of view in a historical review of rhytidectomy, stating “in the early years of SMAS surgery, it was apparent that excessive traction of the SMAS could further aggravate the accentuation of the nasolabial groove”. Yousif et al (8) also support this idea, stating “when the release of the deep attachments of the SMAS to bone was accomplished by dividing the zygomatic ligament lateral to the inferior orbital rim and upward pull was applied to the SMAS, not only was the upper lip elevated but the nasolabial fold also appeared to deepen. Obviously, placing more traction on the SMAS was not the answer to the ptotic cheek and deep nasolabial fold”.
Webster and Yousif have also maintained the idea that differential traction on the skin and subcutaneous tissues overlying the SMAS is the only way to flatten the nasolabial fold and not deepen or enhance the nasolabial crease (5–8). Barton (2,9) has reported that after initially starting in the sub-SMAS plane, dissection is continued until the lateral border of the zygomaticus major is reached, then the investing fascia overlying the zygomaticus major must be opened and dissection must be continued over the superficial surface of the muscle to obtain improvement in the nasolabial fold and medial cheek area. All of these authors indicate that traction on the skin and subcutaneous tissues is responsible for ameliorization of the nasolabial fold.
The idea presented in the current study is quite simple: what is the effect of traction on the SMAS in a superior and posterior direction after mobilization in vivo? The SMAS flap was mobilized as much as necessary according to the preoperatively assessed goals of the procedure. At no time was the SMAS mobilized significantly anterior to the zygomaticus major muscle. When a more superior vector of mobilization was required to elevate the corner of the mouth, the upper SMAS was then occasionally mobilized anteriorly over the origin of the zygomaticus major muscle. To improve viability of the skin flap, the attachments of the skin and SMAS to the medial cheek are not disrupted and, with traction on the SMAS, an aesthetically desirable hollowing in the cheek under the zygomatic arch is achieved (12). When traction was placed onto the SMAS following the described mobilization, the effect was a flattening of the nasolabial fold with no deepening of the nasolabial crease medial to the fold. A differential movement with a stronger pull on the skin and subcutaneous tissues, compared with the SMAS, was not required to achieve effacement of the nasolabial fold.
Yousif (14) performed an examination of the effects of aging on the nasolabial fold and crease. He found that the soft tissues of the midface descend in inferior, lateral and anterior directions with aging. The descent of the cheek mass to the fixed nasolabial crease is responsible for the increase in the nasolabial fold, and this fullness of the nasolabial fold creates the illusion of depth in the nasolabial crease. These observations lead one to question the goal of the facelift procedure – is the goal to flatten the nasolabial fold or to restore the patient to a more youthful appearance? Preoperative analysis of patient photos taken in their youth demonstrate that many of the patients had deep nasolabial creases in their late teens and early 20s. Thus, focusing on complete effacement of the nasolabial folds is not consistent with attempting to restore a youthful appearance.
The reason that other investigators have found that traction on the SMAS results in deepening of the nasolabial creases is not clear. Rubin et al (13) have shown that the nasolabial crease is a dynamic function related to the muscles of facial expression. Surgical manoeuvres that pull or tighten the muscles of facial expression would have the effect of deepening the nasolabial crease. Because the SMAS is superficial to the muscular insertions of the nasolabial crease, it is not clear how traction on the SMAS would deepen the crease. Our observations are that traction on a mobilized SMAS flap has the effect of flattening the nasolabial crease. Rubin has also made the same observation and found that the improvement in the nasolabial fold was observed for much longer using an SMAS flap that was mobilized past the parotid gland and sutured above the zygomatic arch compared with wide undermining of the skin over the nasolabial fold and onto the upper lip (13). He believed that the SMAS was continuous with the fascia of the fold, and traction on the SMAS resulted in a pull on the superior aspect of the fold, which resulted in a flatter appearance.
REFERENCES
- 1.Skoog T. Plastic Surgery – New Methods and Refinements. Philadelphia: WB Saunders; 1974. pp. 300–31. [Google Scholar]
- 2.Barton FE., Jr Rhytidectomy and the nasolabial fold. Plast Reconstr Surg. 1992;90:601–7. doi: 10.1097/00006534-199210000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Larson DL. An historical glimpse of the evolution of rhytidectomy. Clin Plast Surg. 1995;22:207–12. [PubMed] [Google Scholar]
- 4.Yousif NJ, Larson DL. Clinics in Plastic Surgery. Philadelphia: WB Saunders; 1995. [Google Scholar]
- 5.Webster RC, Smith RC, Papsidero MJ, Karolow WW, Smith KF. Comparison of SMAS plication with SMAS imbrication in face lifting. Laryngoscope. 1982;92:901–12. [PubMed] [Google Scholar]
- 6.Webster RC, Hamdan US, Fuleihan NS, Gaunt JM, Wooldridge DW, Smith RC. The considered and considerate face lift part II: SMAS plication vs. imbrication, theory of SMAS anatomy and dynamics, and conservation of platysma. Am J Cosmetic Surg. 1985;2:1–5. [Google Scholar]
- 7.Fuliehan NS. The nasolabial fold and the SMAS. Plast Reconstr Surg. 1994;94:1091–2. [PubMed] [Google Scholar]
- 8.Yousif NJ, Gosain AK, Matloub HS, Sanger JR, Madiedo G, Larson DL. The nasolabial fold: An anatomic and histological reappraisal. Plast Reconstr Surg. 1994;93:60–9. [PubMed] [Google Scholar]
- 9.Barton FE., Jr The SMAS and the nasolabial fold. Plast Reconstr Surg. 1992;89:1054–7. [PubMed] [Google Scholar]
- 10.Millard DR, Yuan RTW, Devine JW. A challenge to the undefeated nasolabial folds. Plast Reconstr Surg. 1987;80:37–46. doi: 10.1097/00006534-198707000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Mendelson BC. Surgery of the superficial musculoaponeurotic system: Principles of release, vectors, and fixation. Plast Reconstr Surg. 2001;107:1545–52. [PubMed] [Google Scholar]
- 12.Connell BF, Marten TJ. Facial rejuvenation: Facelift. In: Cohen MM, editor. Mastery of Plastic Surgery. Boston: Little, Brown and Co; 1994. pp. 1873–902. [Google Scholar]
- 13.Rubin LR, Mishriki Y, Lee G. Anatomy of the nasolabial fold: The keystone of the smiling mechanism. Plast Reconstr Surg. 1989;83:1–8. doi: 10.1097/00006534-198901000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Yousif NJ. Changes of the midface with age. Clin Plast Surg. 1995;22:213–26. [PubMed] [Google Scholar]