Abstract
BACKGROUND:
Acute coronary syndrome (ACS) is one of the most frequent reasons for hospitalization worldwide. Although substantial advances have been made in the prevention and treatment of coronary artery disease, their impact on the rates of ACS hospitalization is unclear.
METHODS:
Data from the Canadian Institute for Health Information Discharge Abstract Database were used to estimate secular trends in ACS hospitalization. A total of 1.3 million ACS hospitalizations in Canada from April 1, 1994, to March 31, 2006, were examined. Overall hospitalization rates were standardized for age and sex using 1991 Canadian census data, and hospitalization rates were also stratified by age group, sex and Canadian province to assess trends in each subgroup.
RESULTS:
The Canadian age- and sex-standardized ACS hospitalization rate was 508 per 100,000 persons in 1994, and 317 per 100,000 persons in 2005 – a relative reduction of 37.8% and an average annual relative reduction of 3.9% per year. Declines in ACS hospitalization rates were observed among men (annual relative reduction 3.9%, relative reduction 39.0%) and women (annual relative reduction 3.8%, relative reduction 35.8%). Declining trends were also observed among patients of different age groups and among patients hospitalized across all Canadian provinces.
INTERPRETATION:
Over the past decade, a substantial decline in ACS hospitalization rates occurred, which has not been previously observed. This finding is likely due to improvements in primary and secondary prevention of coronary artery disease. The present study’s data should provide important insights and guidance for future health care planning in Canada.
Keywords: Acute coronary syndrome, Hospitalization rates, Secular trends
Abstract
HISTORIQUE :
Le syndrome coronarien aigu (SCA) est l’une des principales causes d’hospitalisation de par le monde. Même si on a réalisé des progrès considérables dans la prévention et le traitement de la coronaropathie, on ne connaît pas clairement ses répercussions sur le taux d’hospitalisations attribuables au SCA.
MÉTHODOLOGIE :
Les données de la base de données sur les congés des patients de l’Institut canadien d’information sur la santé ont permis d’évaluer les tendances séculaires d’hospitalisations attribuables au SCA. Au total, on a examiné 1,3 million de ces hospitalisations au Canada entre le 1er avril 1994 et le 31 mars 2006. Les taux d’hospitalisation globaux ont été normalisés selon l’âge et le sexe à l’aide des données du recensement canadien de 1991, et les taux d’hospitalisation ont également été stratifiés selon le groupe d’âge, le sexe et la province canadienne pour évaluer les tendances de chaque sous-groupe.
RÉSULTATS :
Les taux d’hospitalisations attribuables au SCA au Canada, normalisés selon l’âge et le sexe, correspondaient à 508 personnes par tranche de 100 000 habitants en 1994, et à 317 personnes par tranche de 100 000 habitants en 2005, soit une réduction relative de 37,8 % et une réduction relative annuelle moyenne de 3,9 % par année. On observait un fléchissement de ces taux d’hospitalisation chez les hommes (réduction annuelle relative de 3,9 % et réduction relative de 39,0 %) et chez les femmes (réduction annuelle relative de 3,8 % et réduction relative de 35,8 %), de même qu’une tendance à la baisse chez les patients de divers groupes d’âge et chez ceux hospitalisés dans les diverses provinces canadiennes.
INTERPRÉTATION :
Depuis dix ans, on observe pour la première fois un fléchissement substantiel des hospitalisations attribuables au SCA. Cette constatation découle probablement des améliorations à la prévention primaire et secondaire de la coronaropathie. Les données de la présente étude devraient donner un aperçu important et une orientation quant à la future planification des soins au Canada.
Coronary artery disease continues to be the leading cause of morbidity and mortality worldwide (1–4). It places a large economic burden on the health care system because acute coronary artery disease is also one of the most frequent reasons for hospitalization (1,2,5). While one might hypothesize that significant improvements in prevention and treatment of coronary artery disease have reduced the burden of cardiovascular disease, little information is available on the secular trends of acute coronary syndrome (ACS) hospitalization in Canada.
Previous studies on trends of acute coronary artery disease have yielded divergent results. The World Health Organization Multinational MONItoring of trends and determinants in CArdiovascular disease (WHO MONICA) project (6), which examined 37 populations across four continents, found that the incidence of coronary artery disease hospitalizations had modestly declined from the mid-1980s to the mid-1990s. Conversely, data from the United States showed a slight increase in incidence over a similar period (7). It is uncertain how trends in Canada would compare with other jurisdictions because there are unique aspects to the demographic composition of Canada and the nature of the health care system. Furthermore, previous studies focusing on acute myocardial infarction ignored a large proportion of patients hospitalized with unstable angina without evidence of heart damage or infarction. In addition, the definition of acute myocardial infarction has changed dramatically in the past decade, emphasizing the use of sensitive cardiac biomarkers (8). Therefore, ACS is currently accepted as the most appropriate operational term to describe an acute presentation of coronary artery disease, encompassing both ST segment elevation myocardial infarction, non-ST segment elevation myocardial infarction and unstable angina (9).
An understanding of the secular trends in ACS hospitalization rates will provide important insights into the incidence and prevalence of acute coronary artery disease, and also enable us to evaluate the impact of primary and secondary prevention at the population level. Accordingly, the main objective of the project was to estimate trends in ACS hospitalizations in Canada.
METHODS
Data sources
The Canadian Institute for Health Information (CIHI) Discharge Abstract Database includes demographic and clinical information of all patients who are hospitalized to acute care hospitals in Canada. Trained hospital staff transcribe information from each medical chart using standardized International Classification of Diseases (ICD) codes. Using the CIHI Discharge Abstract Database, all patients who were hospitalized with ACS were identified from April 1, 1994, to March 31, 2006, based on the ICD – Ninth Revision (ICD-9) codes 410, 411 and 413, and the ICD – 10th Revision (ICD-10) codes I20, I21, I22, I23.82 and I24 (2,10). Patients presenting to the emergency room for chest pain evaluation without hospitalization were not included.
Study sample
All patients 20 years of age or older with a diagnosis of ACS were included in the study sample. Patients with previous ACS hospitalizations were not excluded; thus, the study sample included patients with incident and recurrent events. To avoid double-counting patients who received care at more than one hospital for the same incident event, provincial health card numbers were used to create unique episodes of care. As a result, some provincial data (Nova Scotia in fiscal year 1994, Saskatchewan for fiscal years 1994 to 1997, Manitoba for fiscal years 2001 to 2003, and Quebec in fiscal year 2005) were excluded from the rate calculations due to missing health card numbers. This problem occurred because several provinces were not required to submit health card information to the CIHI Discharge Abstract Database at the time.
Revision of ICD codes
ICD codes are modified every 10 to 20 years to reflect changes in medical technology, diagnosis or terminology. Canadian provinces adopted the conversion of ICD-9 to ICD-10 version codes at different times during the study period: British Columbia, Newfoundland and Labrador, Nova Scotia, Prince Edward Island and Saskatchewan in 2001; Alberta and Ontario in 2002; New Brunswick in 2003; and Manitoba in 2004. Quebec used ICD-9 codes throughout the study period. The Charlson comorbidity index, a composite comorbidity score based on 17 medical conditions, was used to examine comorbid disease burden (11). A previous study (12) has shown the Charlson comorbidity index to provide similar estimates of comorbidity prevalence using ICD-9 or ICD-10 version codes.
To ensure comparability of ICD-9 and ICD-10 version codes for capturing ACS diagnoses, data from the Global Registry of Acute Coronary Events (GRACE) were used for validation (13). The GRACE registry is a prospective clinical registry of patients hospitalized with ACS, and has been described in detail elsewhere (13). Ontario patients who were enrolled in the GRACE registry were first linked to the CIHI Discharge Abstract Database using admission date, date of birth and sex (14). The coding accuracy of a CIHI most responsible diagnosis of myocardial infarction and unstable angina was determined using ICD-9 or ICD-10 codes with the same discharge diagnosis in the GRACE registry as the gold standard (13). The coding accuracy of ICD-9 and ICD-10 codes was similar. For example, ICD-9 code 410 had a sensitivity of 83%, a specificity of 73% and a positive predictive value of 84%, and ICD-10 codes I21 and I22 had a sensitivity of 87%, a specificity of 76% and a positive predictive value of 87% for the diagnosis of myocardial infarction, comparable with previous validation studies (14).
Statistical analysis
Age- and sex-standardized hospitalization rates per 100,000 persons were calculated by direct standardization using the 1991 Canadian population as the standard. This method of standardization was consistent with previous epidemiological studies in Canada and represents a standard that allows rates from different studies to be directly comparable (5). ACS hospitalization rates were then stratified by age group, sex and province to examine specific trends in these subgroups. The data did not include postal codes of each patient and, therefore, assessment of hospitalization trends by socioeconomic status was not possible. Average annual relative percentage change in hospitalization rates was calculated by linear regression of the log rates. Potential differences in temporal trends within prespecified subgroups were examined by including an interaction term between the specified subgroups (age, sex, province) and the variable denoting time. Because none of the interaction terms were statistically significant, they were dropped from the regression models. Relative change in hospitalization rates was calculated by comparing rates in fiscal year 2005 with those in 1994 as a reference. CIs of the relative change estimates were calculated using the bootstrapping method.
Two-sided P≤0.05 was considered as statistically significant. SAS version 9.1 (SAS Institute Inc, USA) was used for statistical analyses.
RESULTS
Baseline characteristics
From fiscal year 1994 to 2005, a total of 1.3 million ACS hospitalizations were evaluated. In 1994, the mean age of ACS patients was 67 years and 30% were older than 75 years. In 2005, the mean age was 69 years and 40% were older than 75 years (Table 1). An increasing trend in the proportion of diabetic patients and the number of comorbidities for patients who were hospitalized with ACS was also observed (all P<0.001). The proportion of female patients hospitalized with ACS did not change substantially over this time period (Table 1). The length of stay for an ACS hospitalization also declined significantly during the study period from a median length of stay of six days (interquartile range three to 10 days) in 1994 to four days (interquartile range two to seven days) in 2005 (Table 1) (P<0.001).
TABLE 1.
Demographics and baseline characteristics of hospitalized acute coronary syndrome patients*
| 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, years, mean ± SD | 67±13 | 67±13 | 67±13 | 67±13 | 67±13 | 67±13 | 68±13 | 68±13 | 68±13 | 68±14 | 68±14 | 69±14 |
| Patients older than 75 years, % | 30 | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 36 | 37 | 38 | 40 |
| Female patients, % | 39 | 39 | 39 | 39 | 39 | 39 | 39 | 39 | 38 | 38 | 38 | 39 |
| Patients with diabetes, % | 18 | 19 | 19 | 20 | 21 | 22 | 22 | 23 | 23 | 22 | 22 | 20 |
| Charlson comorbidity index†, % | ||||||||||||
| 0 | 58 | 57 | 56 | 56 | 55 | 54 | 54 | 52 | 53 | 55 | 55 | 60 |
| 1 | 26 | 27 | 27 | 27 | 26 | 27 | 27 | 27 | 26 | 25 | 24 | 23 |
| ≥2 | 16 | 16 | 17 | 18 | 18 | 19 | 20 | 21 | 21 | 20 | 20 | 18 |
| Length of stay, days, median (IQR) | 6 (3–10) | 6 (39) | 6 (3–9) | 5 (3–9) | 5(3–8) | 5 (3–8) | 5 (3–9) | 5 (3–9) | 5 (3–8) | 5 (2–8) | 4 (2–8) | 4 (2–7) |
Data were not available for Nova Scotia in fiscal year 1994, Saskatchewan for fiscal years 1994 to 1997, Manitoba for fiscal years 2001 to 2003, or Quebec in fiscal year 2005 because of high rates of missing health card numbers used to determine transferred patients. P values for trends <0.001 for all characteristics;
The Charlson comorbidity index is a composite score based on myocardial infarction, heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatological disease, peptic ulcer disease, mild liver disease, diabetes, diabetes with complications, hemiplegia or paraplegia, renal disease, cancer, moderate or severe liver disease, metastatic cancer and AIDS/HIV infection. IQR Interquartile range
Trends in ACS, myocardial infarction and unstable angina hospitalization
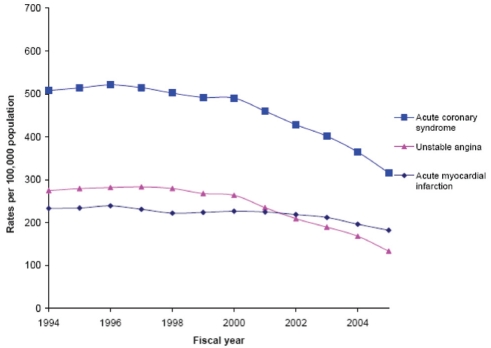
Figure 1 shows age- and sex-standardized hospitalization rates for ACS, acute myocardial infarction and unstable angina from fiscal year 1994 to 2005. In 1994, the age- and sex-standardized hospitalization rate of ACS was 508 per 100,000 persons. In 2005, the age- and sex-standardized hospitalization rate for ACS was substantially reduced to 317 per 100,000 persons. The relative reduction in ACS hospitalization rate was 37.8%, comparing rates from 2005 and 1994, with an average annual relative decline in the rate of ACS hospitalization of 3.9% (Table 2). In addition, a significantly greater decline in ACS hospitalization was observed during the latter part of the study period from 2000 to 2005 compared with 1994 to 1999 (P<0.001).
Figure 1).
Age- and sex-standardized rates for acute coronary syndrome, acute myocardial infarction and unstable angina hospitalization rates in Canada, 1994 to 2005
TABLE 2.
Change in acute coronary syndrome hospitalization rates stratified by age, sex and province*
| Characteristics | Average annual reduction, % (95% CI) | Relative reduction†, % (95% CI) |
|---|---|---|
| Overall | 3.87 (3.86 to 3.88) | 37.8 (37.2 to 38.4) |
| Male patients | ||
| All | 3.90 (3.88 to 3.91) | 39.0 (38.2 to 39.8) |
| 20–49 | 3.38 (3.37 to 3.39) | 35.5 (33.3 to 37.9) |
| 50–64 | 4.66 (4.65 to 4.67) | 44.9 (43.8 to 46.2) |
| 65–74 | 4.23 (4.21 to 4.24) | 40.4 (38.9 to 41.7) |
| ≥75 | 2.17 (2.16 to 2.18) | 25.2 (23.4 to 27.1) |
| Female patients | ||
| All | 3.83 (3.82 to 3.84) | 35.8 (34.8 to 36.9) |
| 20–49 | 2.21 (2.20 to 2.22) | 23.7 (18.0 to 27.9) |
| 50–64 | 5.62 (5.61 to 5.63) | 47.8 (45.9 to 49.4) |
| 65–74 | 5.11 (5.10 to 5.12) | 44.2 (42.5 to 45.8) |
| ≥75 | 2.06 (2.05 to 2.07) | 22.2 (20.4 to 23.9) |
| Province | ||
| NL | 3.43 (3.42 to 3.44) | 30.1 (26.2 to 34.0) |
| PEI | ‡ | ‡ |
| NS | 3.51 (3.50 to 3.53) | 33.2 (29.9 to 36.1) |
| NB | 2.68 (2.67 to 2.69) | 23.3 (19.5 to 26.7) |
| QC | 3.23 (3.22 to 3.24) | 27.8 (26.6 to 28.9) |
| ON | 3.96 (3.94 to 3.97) | 36.8 (35.9 to 37.6) |
| MB | ‡ | 21.6 (17.8 to 25.2) |
| SK | ‡ | ‡ |
| AB | 3.09 (3.08 to 3.09) | 31.4 (28.9 to 33.5) |
| BC | 4.22 (4.21 to 4.23) | 37.0 (35.3 to 38.6) |
Age in years presented for male and female patients.
Overall and provincial hospitalization rates adjusted for age and sex using Canadian 1991 census data;
Relative changes calculated by comparing acute coronary syndrome hospitalization rates in fiscal year 1994 with fiscal year 2005, except for Nova Scotia (relative changes calculated by comparing rates in 1995 with 2005) and Quebec (relative changes calculated by comparing rates in 1994 and 2004);
Calculation was not possible because of incomplete data for the entire study period. AB Alberta; BC British Columbia; MB Manitoba; NB New Brunswick; NL Newfoundland and Labrador; NS Nova Scotia; ON Ontario; PEI Prince Edward Island; QC Quebec; SK Saskatchewan
The decline in ACS was primarily driven by a larger decline in hospitalization rates for unstable angina (relative change 51.3%) compared with a smaller decline in hospitalization rates for patients with myocardial infarction (relative change 21.8%) during the study period (Figure 1).
ACS hospitalization rate trends in different subgroups
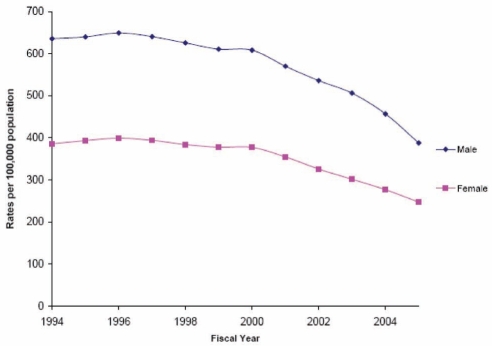
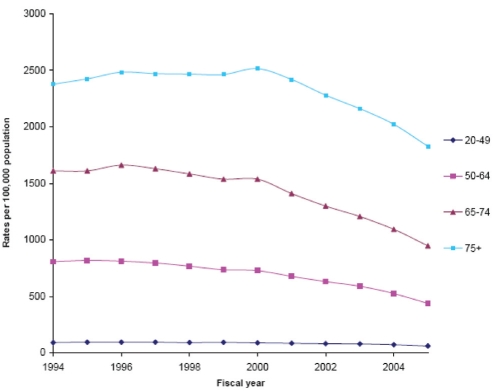
Similar declining trends in ACS hospitalizations were observed among the subgroups of age and sex from 1994 to 2005 (all P<0.05 for trend) (Figures 2 and 3, and Table 2). In 2005, the hospitalization rate for ACS was 391 per 100,000 for men and 249 per 100,000 for women. From 1994 to 2005, the average annual relative reduction in ACS hospitalization was similar for both men (3.9%) and women (3.8%). Similarly, each age group had a significant decline in ACS hospitalizations over the study period and, although older patients have substantially higher hospitalization rates for ACS, each age group had a significant decline in ACS hospitalizations over the study period.
Figure 2).
Age-standardized rates for acute coronary syndrome hospitalizations by sex in Canada, 1994 to 2005
Figure 3).
Sex-standardized rates for acute coronary syndrome hospitalizations by age group in Canada, 1994 to 2005
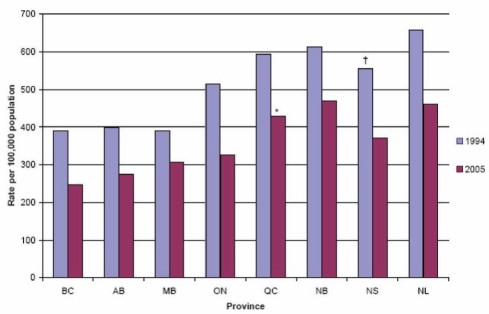
Across Canadian provinces, a reduction in overall hospitalization rates was also observed over time (Figures 3 and 4, and Table 2). Some variations in the magnitude of decline were observed across Canada, ranging from the largest average annual relative reduction of 4.2% in British Columbia to the smallest decline of 2.7% in New Brunswick, but no significant interaction between province and trend of ACS hospitalization was observed (interaction P=0.493). Examination of trends in Prince Edward Island was not possible because of the large year-to-year fluctuation in ACS hospitalizations. The overall annual relative trends for Manitoba and Saskatchewan could also not be calculated because of incomplete data for the entire study period. However, available data also suggested declining trends of ACS hospitalizations in Manitoba (378 per 100,000 in 1994, and 307 per 100,000 in 2005) and in Saskatchewan (448 per 100,000 in 1998, and 387 per 100,000 in 2005).
Figure 4).
Age- and sex-standardized rates for acute coronary syndrome hospitalization by province in Canada in 1994 and 2005. All hospitalization rates are standardized to the 1991 Canadian census. *Fiscal year 2004 data; †Fiscal year 1995 data. AB Alberta; BC British Columbia; MB Manitoba; NB New Brunswick; NL Newfoundland and Labrador; NS Nova Scotia; ON Ontario; QC Quebec
DISCUSSION
The main finding of our study was that hospitalization rates for ACS have decreased substantially over the past decade. We observed a 38% relative decrease and an annual relative decline of 3.9% in ACS hospitalization rates over the past decade. These declines are significant considering that these rates almost doubled the 2.1% annual reduction observed in the WHO MONICA project (6). In addition, the decline in hospitalization rates was observed in all subgroups including those traditionally under-represented in randomized studies such as female patients and older patients.
We also observed a significant ‘east-to-west’ gradient in which eastern Canadian provinces had approximately 1.5-fold to twofold more ACS hospitalizations than western provinces. In previous evaluations (15), we found that regional rates of smoking and obesity were the strongest determinants of geographical variation in cardiovascular death rates in Canada, and that the traditional cardiac risk factors explained 42% of the total variation. We hypothesized that higher rates of these risk factors in eastern Canadian provinces explain much of the east-to-west gradient in cardiovascular disease mortality and hospitalizations. Although the baseline rates of ACS hospitalizations varied substantially across Canada in our study, we observed that all provinces experienced a similar rate of decline in ACS hospitalizations during the study period.
Several epidemiological studies have focused on trends in myocardial infarction and demonstrated small declines in recent years (2,16). In contrast, our study focused on ACS hospitalizations because the definition of acute myocardial infarction has changed drastically over the past decade (8). In 2000, national practice guidelines revised the definition of acute myocardial infarction, emphasizing the use of sensitive cardiac biomarkers such as troponins (8). It has been predicted that this change in how myocardial infarction is defined may result in 40% more myocardial infarction cases (17). As a result, our findings of a relatively small decline in hospitalization rates is probably an underestimation of the overall improvements in acute myocardial infarction incidence rates because it is likely that some patients who were hospitalized for unstable angina before the widespread use of troponin assays would have been diagnosed with a myocardial infarction in the following years. It also implies that epidemiological studies focusing solely on acute myocardial infarction trends may obscure important changes in coronary artery disease trends (18).
Although our study was not intended to address the reasons behind the declining ACS hospitalizations, some hypotheses may be considered. First, there have been substantial reductions in the prevalence of major cardiovascular risk factors such as smoking, elevated total cholesterol and high blood pressure (19–22). For example, a recent Ontario survey suggested that 66% of patients with hypertension in 2006 had received treatment and achieved blood pressure control compared with 21% in 1992 (22). Another study has shown a substantial reduction ranging from 30% to 50% in the number of daily smokers in Canada in 2005 compared with the previous decade (20). These preventive efforts may have delayed the onset of ACS presentation to an older age group and thus explain, in part, our observation that an increasing proportion of patients being hospitalized with ACS are older than 75 years (23).
Second, it is possible that the substantial decline in ACS hospitalizations may be, in part, related to our improved ability to diagnose ACS. The increasing use of cardiac catheterization, serum troponin assays and chest pain observation units might have reduced the misclassification of patients with noncardiac chest pain as having ACS.
Third, there have been significant improvements in the treatment of patients with established coronary artery disease. There has been widespread adoption of evidence-based therapies, including the use of acetylsalicylic acid, beta-blockers, angiotensin-converting enzyme inhibitors and lipid-lowering therapy in patients hospitalized with ACS, which has likely reduced recurrent ACS hospitalization rates (24–27). Cardiac invasive therapies such as percutaneous coronary interventions and coronary artery bypass surgery have also been adopted into routine practice for the treatment of ACS patients; this has likely reduced the frequency of patients experiencing angina post-ACS (28,29). Furthermore, these therapies are also likely responsible for the improved mortality outcomes for patients after an acute myocardial infarction. A recent study (30) by our group found that the in-hospital mortality rate for acute myocardial infarction in Canada declined from 14.5% in 1994, to 9.7% in 2004, which translates to a 33.1% decline over this time period. Because ACS is a major indication for both cardiac catheterization and associated revascularization procedures, a continuous decline in ACS rates may result in a reduction in the need for percutaneous coronary intervention and coronary artery bypass surgery procedures in the future.
Studies from the late 1990s demonstrated an improvement in primary prevention of cardiovascular risk factors and improved treatment of patients after ACS associated with evidence-based therapies (21,22,24,27–29). These treatment advances, in concert with an improvement in ACS diagnosis due to the advent of troponin assays in early 2000, may have resulted in a significantly greater decline in ACS hospitalization occurring in the latter half of our study period.
On the other hand, it has been suggested that the aging of the population, and the rapidly increasing prevalence of obesity and diabetes are beginning to exert a major negative impact on coronary artery disease (31). Therefore, future epidemiological evaluations of ACS trends, and ongoing efforts to promote primary and secondary prevention will be important to ensure continuing declining trends.
Several limitations of our study merit consideration. First, the shift from ICD-9 to ICD-10 occurred during the study period, with Canadian provinces adopting ICD-10 at different points in the study period. However, the conversion between ICD-9 and ICD-10 codes has been validated in the United States, demonstrating that codes for coronary artery disease admission are comparable (2). Furthermore, we also conducted internal data validation using the GRACE registry and found that the administrative data coding accuracy rates of the ICD codes were similar between the two versions. Second, we were unable to study the secular trends of ST segment elevation myocardial infarction and non-ST segment elevation myocardial infarction on a national level because these data are currently not available from administrative sources.
SUMMARY
We observed a substantial decline in the hospitalization rates of ACS over the past decade in Canada. This is likely attributable to improvements in primary and secondary prevention of coronary artery disease. Future epidemiological evaluations of ACS trends are essential to ensure continuing declining trends, given the aging of the population and the emerging obesity and diabetic epidemics.
Footnotes
FUNDING SUPPORT: This work was supported by a Canadian Institutes of Health Research Team Grant in Cardiovascular Outcomes Research to the Canadian Cardiovascular Outcomes Research Team and a Canadian Institutes of Health Research operating grant. Dr Ko is supported by a Clinician Scientist Award by the Heart and Stroke Foundation of Ontario (HSFO). Dr Alter is supported by a Career Investigator Award from the HSFO. Dr Austin is supported by a Career Scientist Award from the HSFO. Dr Tu is supported by a Canada Research Chair in Health Services Research and a Career Investigator Award from the HSFO. The Institute for Clinical Evaluative Sciences is supported by an Ontario Ministry of Health and Long-Term Care grant.
DISCLOSURE: Parts of this material are based on data and information provided by the Canadian Institute for Health Information. The results and conclusions are those of the authors, and should not be attributed to any of the funding or sponsoring agencies.
POTENTIAL CONFLICTS OF INTEREST: Dr Alter is the Chief Scientific Director of INTERxVENT Canada, a therapeutic lifestyle and disease management company. Dr Goodman has received research grant support and speaker/consulting honoraria from sanofi-aventis and Bristol-Myers Squibb.
REFERENCES
- 1.World Health Organization World Health Statistics 2008. <http://www.who.int/whosis/whostat/EN_WHS08_Full.pdf> (Accessed on May 21, 2008).
- 2.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics – 2008 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 3.Manuel DG, Leung M, Nguyen K, Tanuseputro P, Johansen H. Burden of cardiovascular disease in Canada. Can J Cardiol. 2003;19:997–1004. [PubMed] [Google Scholar]
- 4.Heart and Stroke Foundation of Canada. The Growing Burden of Heart Disease and Stroke in Canada 2003. Ottawa: Heart and Stroke Foundation of Canada; 2003. [Google Scholar]
- 5.Hall RE, Tu JV. Hospitalization rates and length of stay for cardiovascular conditions in Canada, 1994 to 1999. Can J Cardiol. 2003;19:1123–31. [PubMed] [Google Scholar]
- 6.Tunstall-Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary artery disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353:1547–57. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 7.Rosamond WD, Chambless LE, Folsom AR, et al. Trends in the incidence of myocardial infarction and in mortality due to coronary artery disease, 1987 to 1994. N Engl J Med. 1998;339:861–7. doi: 10.1056/NEJM199809243391301. [DOI] [PubMed] [Google Scholar]
- 8.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 9.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50:e1–e157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 10.Canadian Institute for Health Information. Canadian Coding Standards for ICD-10-CA and CCI for 2007. <http://www.cihi.ca> (Accessed on June 1, 2008).
- 11.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 12.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 13.Eagle KA, Lim MJ, Dabbous OH, et al. A validated prediction model for all forms of acute coronary syndrome: Estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004;291:2727–33. doi: 10.1001/jama.291.22.2727. [DOI] [PubMed] [Google Scholar]
- 14.Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144:290–6. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- 15.Filate WA, Johansen HL, Kennedy CC, Tu JV. Regional variations in cardiovascular mortality in Canada. Can J Cardiol. 2003;19:1241–8. [PubMed] [Google Scholar]
- 16.Roger VL. Epidemiology of myocardial infarction. Med Clin North Am. 2007;91:537–52. doi: 10.1016/j.mcna.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roger VL, Killian JM, Weston SA, et al. Redefinition of myocardial infarction: Prospective evaluation in the community. Circulation. 2006;114:790–7. doi: 10.1161/CIRCULATIONAHA.106.627505. [DOI] [PubMed] [Google Scholar]
- 18.Salomaa V, Ketonen M, Koukkunen H, et al. The effect of correcting for troponins on trends in coronary artery disease events in Finland during 1993–2002: The FINAMI study. Eur Heart J. 2006;27:2394–9. doi: 10.1093/eurheartj/ehl120. [DOI] [PubMed] [Google Scholar]
- 19.Tanuseputro P, Manuel DG, Leung M, Nguyen K, Johansen H. Risk factors for cardiovascular disease in Canada. Can J Cardiol. 2003;19:1249–59. [PubMed] [Google Scholar]
- 20.Manuel DG, Creatore MI, Rosella LCA, Henry DA. What does it take to make a healthy province? A benchmark study of jurisdictions with the highest levels of health and the best health behaviours. Toronto: ICES; 2008. [Google Scholar]
- 21.Carroll MD, Lacher DA, Sorlie PD, et al. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–81. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 22.Leenen FH, Dumais J, McInnis NH, et al. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ. 2008;178:1441–9. doi: 10.1503/cmaj.071340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldberg RJ, Spencer FA, Yarzebski J, et al. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–8. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 24.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998–1999 to 2000–2001. JAMA. 2003;289:305–12. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 25.Tu JV, Donovan LR, Lee DS, et al. Quality of Cardiac Care in Ontario. Toronto: ICES; 2004. [Google Scholar]
- 26.Fox KA, Steg PG, Eagle KA, et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 27.Austin PC, Tu JV, Ko DT, Alter DA. Use of evidence-based therapies after discharge among elderly patients with acute myocardial infarction. CMAJ. 2008;179:895–900. doi: 10.1503/cmaj.071481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alter DA, Stukel TA, Newman A. Proliferation of cardiac technology in Canada: A challenge to the sustainability of Medicare. Circulation. 2006;113:380–7. doi: 10.1161/CIRCULATIONAHA.105.560466. [DOI] [PubMed] [Google Scholar]
- 29.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–9. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tu JV, Nardi L, Fang J, Liu J, Khalid L, Johansen H. National trends in rates of death and hospital admissions related to acute myocardial infarction, heart failure and stroke, 1994–2004. CMAJ. 2009;180:E118–25. doi: 10.1503/cmaj.081197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]