Abstract
OBJECTIVE:
The impact of admission serum glucose (SG) level on outcomes in coronary artery bypass grafting (CABG) surgery is unknown. The present study sought to determine whether elevated admission SG level is associated with adverse outcomes following CABG surgery.
METHODS:
Patients undergoing CABG surgery between January 2000 and December 2005 at a single centre were identified (n=2856). Admission SG levels of less than 9.2 mmol/L and 9.2 mmol/L or greater were chosen to divide patients into two groups based on the 75th percentile of SG distribution. A logistic regression model was generated to determine the impact of admission SG level on a composite outcome of any one or more of in-hospital mortality, stroke, perioperative myocardial infarction, sepsis, deep sternal wound infection, renal failure, requirement for postoperative inotropes and prolonged ventilation.
RESULTS:
In total, 76.3% of patients had an admission SG level of less than 9.2 mmol/L (group A) and 23.7% had an admission SG level of 9.2 mmol/L or greater (group B). Group B patients were more likely to be female, have diabetes, have preoperative renal failure, have an ejection fraction of less than 40%, experience myocardial infarction within 21 days before surgery, and have triple vessel or left main disease (P<0.05). Univariate analysis revealed no difference in in-hospital mortality between group A (2.2%) and group B (3.2%) (P=0.12); however, the composite outcome was more likely to occur in group B (40.8%) versus group A (27.9%) (P=0.0001). After multivariable adjustment, admission SG level of 9.2 mmol/L or greater remained an independent predictor of composite outcome (OR=1.3, 95% CI 1.0 to 1.7, P=0.02, receiver operating characteristic = 78%).
CONCLUSION:
Admission SG level of 9.2 mmol/L or greater is associated with significant morbidity in patients undergoing CABG surgery.
Keywords: Admission glucose, Bypass surgery, Diabetes, Outcome
Abstract
OBJECTIF :
On ne connaît pas les répercussions du taux de glucose sérique (GS) à l’admission sur les issues du pontage aortocoronarien (PAC). La présente étude visait à déterminer si un taux de GS élevé à l’admission s’associe à des issues négatives après un PAC.
MÉTHODOLOGIE :
Les auteurs ont repéré les patients qui ont subi un PAC entre janvier 2000 et décembre 2005 dans un seul centre (n=2 856). Ils ont sélectionné les valeurs de GS inférieures à 9,2 mmol/L et d’au moins 9,2 mmol/L à l’admission pour séparer les patients en deux groupes d’après le 75e percentile de distribution du GS. Ils ont produit un modèle de régression logistique pour déterminer les répercussions du GS à l’admission sur une issue composite d’au moins l’une des constatations suivantes : décès intra-hospitalier, accident cérébral vasculaire, infarctus du myocarde périopératoire, sepsie, infection profonde de la plaie sternale, insuffisance rénale, besoin d’inotropes postopératoires et ventilation prolongée.
RÉSULTATS :
Au total, 76,3 % des patients présentaient un taux de GS à l’admission inférieur à 9,2 mmol/L (groupe A), et 23,7 %, un taux de GS à l’admission d’au moins 9,2 mmol/L (groupe B). Les patients du groupe B étaient plus susceptibles d’être des femmes, d’être diabétiques, de présenter une insuffisance rénale préopératoire, d’avoir une fraction d’éjection inférieure à 40 %, d’avoir subi un infarctus du myocarde dans les 21 jours précédant l’opération et d’avoir une triple vasculopathie ou une maladie de la souche principale gauche (P<0,05). L’analyse multivariée n’a révélé aucune différence de mortalité intra-hospitalière entre le groupe A (2,2 %) et le groupe B (3,2 %) (P=0,12). Cependant, une issue composite était plus susceptible de s’observer dans le groupe B (40,8 %) que dans le groupe A (27,9 %) (P=0,0001). Après rajustement multivarié, un GS à l’admission d’au moins 9,2 mmol/L demeurait un prédicteur indépendant d’issue composite (RR=1,3, 95 % IC 1,0 à 1,7, P=0,02, fonction d’efficacité du récepteur = 78 %).
CONCLUSION :
Un GS d’au moins 9,2 mmol/L à l’admission s’associe à une morbidité importante chez les patients qui subissent un PAC.
It has been confirmed that serum glucose (SG) levels are independently associated with both short- and long-term outcomes of patients with cardiovascular disease (1). In the setting of an acute myocardial infarction, hyperglycemia enhances the risk of morbidity and mortality independent of the patients’ diabetes status (2). Hyperglycemia is also highly predictive of the occurrence of left ventricular failure and cardiac death in patients with acute coronary syndrome (3,4), and is associated with larger infarct size, worse functional recovery and higher long-term mortality in patients undergoing reperfusion with either thrombolysis or percutaneous coronary intervention (5,6).
In patients undergoing cardiac surgery, there is also evidence that both intraoperative (7,8) and postoperative (9) SG levels predict the occurrence of adverse postoperative events. Tight control of intra- and postoperative SG levels with insulin increases survival and decreases the incidence of ischemic events in diabetic patients undergoing coronary artery bypass grafting (CABG) surgery (10).
In contrast to the known importance of intra- and/or postoperative SG levels on the outcomes of CABG surgery, there exists a paucity of data regarding the potential impact of preoperative or admission SG level on the outcomes of cardiac surgery. We hypothesized that an elevated preoperative or admission SG level would be an independent predictor of adverse outcomes in patients having cardiac surgery. In this regard, we undertook the current study to specifically determine whether an elevated admission SG level is associated with increased in-hospital mortality (IHM) and/or morbidity in patients with or without a known history of diabetes mellitus (DM) undergoing isolated CABG surgery.
METHODS
Patient selection and definition
The computerized database from the Maritime Heart Center, Division of Cardiac Surgery (Dalhousie University, Halifax, Nova Scotia), was used to identify 2856 consecutive patients undergoing isolated CABG surgery between December 2000 and January 2005. This registry captures 100% of cardiac surgeries performed at this institution and is validated annually by random audit of patient charts. Perioperative data were collected by full-time research assistants and maintained in a computer database format. The end points of interest analyzed to determine the association between admission SG level and outcomes included IHM, stroke, perioperative myocardial infarction, sepsis, deep sternal wound infection, renal failure (RF), postoperative ino-trope requirement, prolonged (longer than 24 h) ventilation, and a composite outcome, defined as any one or more of the above. Perioperative myocardial infarction was defined as a rise in creatine kinase MB fraction of greater than 5% and the presence of new Q waves or regional wall motion abnormalities as determined by radio-nuclide imaging or echocardiography. Stroke was defined as a new permanent neurological deficit confirmed by physical examination by a neurological consultant and corroborated by ancillary computed tomography or magnetic resonance imaging. Transient ischemic attacks and reversible ischemic neurological deficits were not included as a stroke end point. RF was defined by a serum creatinine level of 177 μmol/L or greater, a dialysis requirement, or an increase in serum creatinine of 30% or greater of the baseline value. Sepsis was defined as any postoperative positive blood culture (bacteremia) associated with signs and symptoms of a systemic inflammatory response. Deep sternal wound infection was defined by the presence of culture-positive sternal wound drainage associated with sternal instability, and requiring surgical debridement or sternal resuturing. All the end points assessed were captured in the computerized database. Surgical urgency status was determined according to slight modifications of the standard Society of Thoracic Surgeons guidelines (www.sts.org). An elective case was defined as a patient being admitted for surgery on a same-day basis from home. Nonurgent in-hospital patients were those in-hospital patients who were stable for longer than 24 h before the procedure. Urgent operation required surgery to be performed within 24 h to prevent further clinical deterioration. Surgery was deemed emergent in patients who required an immediate operation. Cardiopulmonary bypass was performed in a standardized fashion. Body temperature during the procedure was allowed to drift to approximately 32°C. Standard intermittent antegrade and/or retrograde cold blood cardioplegia was used for myocardial protection.
Admission SG level is not captured as an explicit variable in the database and, hence, chart reviews were performed to extract this variable. In patients classified as elective, admission SG level was defined as the random SG value obtained from routine blood chemistry analyses of blood drawn during the patient’s visit to the preadmission clinic (characteristically one to three days before surgery). In nonurgent in-hospital patients and those who underwent urgent or emergent surgery, admission SG level was defined as the first random SG value obtained on hospital admission.
The study protocol was in compliance with the institutional clinical research ethics board and received full approval.
Data analysis and statistics
Statistical analysis was performed using the SAS software package (Release 9.1, SAS Institute Inc, USA). Categorical variables were analyzed univariately with the χ2 test or Fisher’s exact test where appropriate; continuous variables were examined by t test or Wilcoxon’s rank sum test. A cut point for elevated admission SG level was selected after examining the prevalence of the composite outcome across 1 mmol/L increments of SG values, as well as the distribution of SG values by percentile. When 1 mmol/L increments of admission SG values were examined, the prevalence of the composite outcome increased when the SG level exceeded 9 mmol/L. Furthermore, the 75th percentile of the distribution of SG values was bounded by 9.2 mmol/L. Therefore, a cutoff admission SG level of less than 9.2 mmol/L (group A) or 9.2 mmol/L or greater (group B) was chosen a priori to divide patients into two groups based on the 75th percentile of admission SG distribution in the entire study population. An adjusted logistic regression model was generated to determine the association of admission SG level of 9.2 mmol/L or greater with a composite outcome in the entire population of study patients. In addition, the study population was then divided into two groups based on whether a diagnosis of diabetes was present. Separate logistic regression models were created to analyze the impact of an admission SG level of 9.2 mmol/L or greater on the composite outcome in patients with and without a preceding history of diabetes. Potential covariates included in the models are listed in Table 1 and follow those previously established to be of relevance (11). The discriminatory capacities of the regression models were evaluated using the area under the receiver operating characteristic curve.
Table 1.
Baseline patient characteristics
| Patient characteristic | SG <9.2 mmol/L (n=2180), % | SG ≥9.2 mmol/L (n=676), % | P |
|---|---|---|---|
| Age >70 years | 30.1 | 30.3 | 0.93 |
| Female sex | 23.1 | 26.8 | 0.052 |
| Diabetes | 23.8 | 83.9 | 0.0001 |
| Renal failure | 3.7 | 6.8 | 0.0007 |
| Peripheral vascular disease | 17.4 | 22.8 | 0.0017 |
| Cerebrovascular disease | 14.4 | 17.2 | 0.080 |
| Ejection fraction <40% | 10.4 | 17.7 | 0.0001 |
| Previous CABG | 3.2 | 4.0 | 0.30 |
| Acuity | |||
| Elective | 49.4 | 48.7 | 0.71 |
| Nonurgent in-hospital | 37.2 | 36.7 | |
| Urgent or emergent | 13.4 | 14.6 | |
| COPD | 15.3 | 16.9 | 0.34 |
| MI within 21 days before surgery | 17.7 | 21.2 | 0.04 |
| TVD or LM >50% | 78.9 | 85.1 | 0.0004 |
| ACE inhibitor | 58.3 | 66.7 | 0.0001 |
| Beta-blocker | 88.8 | 87.0 | 0.18 |
| Statin | 80.7 | 78.2 | 0.16 |
| Intravenous nitroglycerin | 17.2 | 17.2 | 0.98 |
| Bilateral mammary artery | 13.2 | 8.6 | 0.0014 |
ACE Angiotensin-converting enzyme; CABG Coronary artery bypass grafting; COPD Chronic obstructive pulmonary disease; LM Left main; MI Myocardial infarction; SG Serum glucose; TVD Triple vessel disease
RESULTS
A total of 2856 consecutive patients undergoing isolated CABG surgery between December 2000 and January 2005 at the Maritime Heart Center were identified. Of these, 2180 (76.3%) had an admission SG level of less than 9.2 mmol/L (group A) and 676 (23.7%) had an admission SG level of 9.2 mmol/L or greater (group B). The baseline characteristics of group A and group B patients are listed in Table 1. Group B patients (SG level of 9.2 mmol/L or greater) were more likely to be female (P=0.05), have diabetes (P=0.0001), manifest RF (P=0.0007), have peripheral vascular disease (P=0.002), have an ejection fraction of less than 40% (P=0.0001), sustain a myocardial infarction less than 21 days before surgery (P=0.04), and present with triple vessel or left main coronary disease (P=0.0004). Importantly, the two groups did not differ in the acuity or urgency of operation, or the proportion of repeat or ‘redo’ revascularization procedures. With regard to preoperative pharmacological therapy, there were no differences in the use of beta-blockers, statins or intravenous nitroglycerin administration between the two groups. However, patients with an admission SG level of 9.2 mmol/L or greater (group B) were more likely to receive angiotensin-converting enzyme inhibitors (P=0.0001).
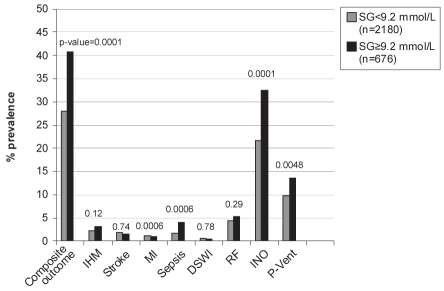
The unadjusted outcomes are illustrated in Figure 1. There was no significant difference in IHM between the two groups (group A, 2.2%; group B, 3.2%; P=0.12). However, sepsis (group A 1.7% versus group B 4.0%; P=0.0006), postoperative inotrope requirement (group A 21.6% versus group B 32.4%; P=0.0001) and prolonged ventilation (group A 9.8% versus group B 13.6%; P=0.0048) were more likely to occur in patients with an admission blood glucose level of 9.2 mmol/L or greater (group B). After multivariable adjustment for comorbidity, which included a history of diabetes, an admission SG level of 9.2 mmol/L or greater remained an independent predictor for the occurrence of a composite outcome with an adjusted OR of 1.3 (95% CI 1.0 to 1.7, P=0.02; Table 2). The receiver operating characteristic for this adjusted model for composite outcome was 78%, indicating a fairly robust discriminatory capacity.
Figure 1).
Percentage prevalence of outcomes in patients with serum glucose (SG) of less than 9.2 mmol/L (group A) versus SG of 9.2 mmol/L or greater (group B). DSWI Deep sternal wound infection; IHM In-hospital mortality; INO Inotropic support; MI Myocardial infarction; P-Vent Prolonged ventilation; RF Renal failure
TABLE 2.
Fully adjusted logistic regression model for composite outcome
| Preoperative characteristic | OR | 95% CI | P |
|---|---|---|---|
| Acuity | |||
| Nonurgent in-hospital | 1.3 | 1.0–1.6 | 0.0293 |
| Urgent or emergent | 3.3 | 2.4–4.7 | 0.0001 |
| Ejection fraction <40% | 4.3 | 3.3–5.6 | 0.0001 |
| Previous CABG | 4.1 | 2.6–6.5 | 0.0001 |
| Renal failure | 3.0 | 1.9–4.6 | 0.0001 |
| TVD or LM >50% | 2.0 | 1.5–2.6 | 0.0001 |
| Cerebrovascular disease | 1.8 | 1.4–2.3 | 0.0001 |
| Age >70 years | 1.6 | 1.3–1.9 | 0.0001 |
| Chronic obstructive pulmonary disease | 1.5 | 1.2–2.0 | 0.0004 |
| Female sex | 1.4 | 1.1–1.7 | 0.0036 |
| Peripheral vascular disease | 1.4 | 1.1–1.8 | 0.0057 |
| Intravenous nitroglycerin | 1.4 | 1.0–1.8 | 0.0292 |
| Serum glucose ≥9.2 mmol/L | 1.3 | 1.0–1.7 | 0.0226 |
| Diabetes | 1.3 | 1.0–1.6 | 0.0268 |
| MI within 21 days before surgery | 1.3 | 1.0–1.7 | 0.0465 |
| ACE inhibitor | 1.1 | 0.9–1.3 | 0.5763 |
| Statin | 0.9 | 0.7–1.1 | 0.2849 |
| Beta-blocker | 0.8 | 0.6–1.1 | 0.1770 |
| Bilateral mammary artery | 0.8 | 0.6–1.1 | 0.1384 |
Model receiver operating characteristic = 78%. ACE Angiotensin-converting enzyme; CABG Coronary artery bypass grafting; LM Left main; MI Myocardial infarction; TVD Triple vessel disease
As expected, colinearity existed between an admission SG level of 9.2 mmol/L or greater and a history of diabetes, with a correlation coefficient of 0.5144. As such, separate logistic regression analyses were performed to assess the association of an admission SG level of 9.2 mmol/L or greater with the composite outcome in patients with (n=1086) and without (n=1770) a preceding history of diabetes. An admission SG level of 9.2 mmol/L or greater emerged as an independent predictor of the composite outcome in patients with diabetes (OR=1.4, 95% CI 1.1 to 1.9, P=0.02; Table 3) but was not an independent predictor of the composite outcome in nondiabetic patients (OR=1.1, 95% CI 0.7 to 1.8, P=0.7).
TABLE 3.
Fully adjusted logistic regression model for composite outcome in diabetic patients
| Preoperative characteristic | OR | 95% CI | P |
|---|---|---|---|
| Acuity | |||
| Nonurgent in-hospital | 1.1 | 0.8–1.6 | 0.4410 |
| Urgent or emergent | 2.3 | 1.4–3.9 | 0.0017 |
| Ejection fraction <40% | 4.8 | 3.2–7.2 | 0.0001 |
| Previous CABG | 4.3 | 2.0–9.6 | 0.0003 |
| Renal failure | 2.6 | 1.4–4.8 | 0.0019 |
| TVD or LM >50% | 1.5 | 1.0–2.2 | 0.0751 |
| Cerebrovascular disease | 1.5 | 1.1–2.2 | 0.0233 |
| Age >70 years | 1.6 | 1.2–2.2 | 0.0030 |
| Chronic obstructive pulmonary disease | 1.9 | 1.3–2.8 | 0.0006 |
| Female sex | 1.3 | 1.0–1.8 | 0.0791 |
| Peripheral vascular disease | 1.5 | 1.1–2.1 | 0.0144 |
| Intravenous nitroglycerin | 1.7 | 1.1–2.6 | 0.0147 |
| Serum glucose ≥9.2 mmol/L | 1.4 | 1.1–1.9 | 0.0150 |
| MI within 21 days before surgery | 1.8 | 1.3–2.4 | 0.0002 |
| ACE inhibitor | 1.1 | 0.8–1.5 | 0.5982 |
| Statin | 0.8 | 0.6–1.2 | 0.2425 |
| Beta-blocker | 0.7 | 0.4–1.1 | 0.1305 |
| Bilateral mammary artery | 0.7 | 0.4–1.3 | 0.2655 |
Model receiver operating characteristic = 78%. ACE Angiotensin-converting enzyme; CABG Coronary artery bypass grafting; LM Left main; MI Myocardial infarction; TVD Triple vessel disease
DISCUSSION
The present retrospective analysis of a prospectively assembled cohort study, which included 2856 patients, was designed to evaluate whether admission SG levels are of prognostic value in determining the occurrence of major morbidity following isolated CABG. To our knowledge, the present study is the first to report such an association. We found that patients admitted with an SG level of 9.2 mmol/L or greater were more likely to suffer major morbidity postoperatively than patients with an admission SG level of less than 9.2 mmol/L. It is worth noting that, in our cohort, most patients (83.9%) with an admission SG level of 9.2 mmol/L or greater were previously known to have DM, whereas in patients with an admission SG level of less than 9.2 mmol/L, 23.8% had previously diagnosed DM. However, in those patients who did not have a previously documented history of diabetes, an admission SG level of 9.2 mmol/L or greater was not associated with poor outcome. However, our study is the first to show that, along with the diagnosis of DM, an admission SG level of 9.2 mmol/L or greater is an independent risk factor for poor outcome, as evidenced by our composite measure. Although statistical significance does not apply to each of the individual components of the composite outcome, together they are clinically important.
Much attention has been given to the prognostic value of both intraoperative and postoperative glycemic control, and subsequent studies have looked at the potential impact of modifying perioperative glycemic control on morbidity. Doenst et al (8) measured the SG level approximately every 15 min in 1579 diabetic and 4701 nondiabetic patients undergoing cardiac surgery, and found that a high peak SG level during cardiopulmonary bypass was an independent risk factor for morbidity and mortality. Postoperative SG level also impacts the outcome in patients undergoing CABG surgery. In a retrospective study of 200 patients who underwent CABG surgery, Fish et al (9), using a postoperative blood glucose cut-off level of 11.1 mmol/L to identify diabetes, reported a threefold increase in complications associated with hyperglycemia. In another study of 878 previously nondiabetic patients undergoing CABG surgery, Zindrou et al (12) reported that in women, an admission SG level of greater than 6 mmol/L was predictive of increased 30-day mortality. This study did not assess the long-term outcomes of these patients.
There is also evidence suggesting that treating CABG surgery patients with insulin in an effort to lower SG level improves outcomes. In an intervention study of DM patients undergoing CABG surgery aimed at lowering perioperative hyperglycemia, Lazar et al (10) compared tight glycemic control (6.9 mmol/L to 11.1 mmol/L) using a glucose/insulin/potassium infusion versus standard care (SG level less than 13.9 mmol/L) using intermittent subcutaneous insulin starting preoperatively and continuing for 12 h postoperatively. They found that tight glycemic control using glucose/insulin/potassium was associated with less postoperative atrial fibrillation, a shorter length of stay in hospital, fewer recurrent wound infections, fewer episodes of ischemia and a survival advantage at two years. In another retrospective study (13) assessing the impact of intravenous and subcutaneous insulin in patients with DM and stress-induced hyperglycemia undergoing cardiothoracic surgery, a subgroup analysis of the CABG surgery patients showed that insulin treatment resulted in reduction of adverse outcomes to that of the range of non-DM patients.
In the present study, we cannot conclude whether the observed increase in morbidity associated with admission SG level was due solely to acute hyperglycemia or whether the observed hyperglycemia is merely a marker of those who were more likely to have had longstanding poor glycemic control. Without glycosylated hemoglobin values, we are unable to support either hypothesis.
The interplay between SG toxicity and insulin resistance, and their contribution to the observed increase in morbidity associated with hyperglycemia in patients undergoing CABG surgery, is not well understood. Furthermore, it is currently debatable whether it is, in fact, the lowering of SG level alone or insulin treatment, or the combination of the two that is responsible for the improvement in outcome.
Further trials are required to clarify the individual roles of insulin versus glucose lowering in these patients.
The strength of the present study includes a large population with well-defined prospectively collected end point data and the availability of admission SG levels in virtually all patients. However, as pointed out earlier, the primary limitation of our study is that some of the patients designated as nondiabetic individuals with admission hyperglycemia may have been previously undiagnosed diabetic individuals. Furthermore, because the present study was a retrospective analysis of an existing database that recorded all studied variables except admission SG level, thus necessitating a chart review and data extraction, the possibility of selection bias cannot be eliminated. Furthermore, capturing the time interval from admission SG level measurement to surgery may provide additional insight in future studies.
As far as we are aware, the present study is the first to show that, in a large cohort of patients undergoing CABG surgery, an admission hyperglycemia level of 9.2 mmol/L or greater is an independent risk factor for adverse outcomes. Further studies assessing the relationship between degree of hyperglycemia (both acute and chronic) on admission and outcome are warranted. This paves the way for interventional studies aimed at lowering admission SG level to assess the impact on postoperative outcomes.
Acknowledgments
Portions of the present work have been presented in scientific poster format at the American College of Cardiology 2006 Annual Scientific Session, as well as the Canadian Diabetes Association/Canadian Society of Endocrinology and Metabolism 2007 Professional Conference and Annual Meeting.
REFERENCES
- 1.Port SC, Boyle NG, Hsueh WA, Quinones MJ, Jenrich RI, Goodarzi MO. The predictive role of blood glucose for mortality in subjects with cardiovascular disease. Am J Epidemiol. 2006;163:342–51. doi: 10.1093/aje/kwj027. [DOI] [PubMed] [Google Scholar]
- 2.Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: A systematic overview. Lancet. 2000;355:773–8. doi: 10.1016/S0140-6736(99)08415-9. [DOI] [PubMed] [Google Scholar]
- 3.Foo K, Cooper J, Deaner A, et al. A single serum glucose measurement predicts adverse outcomes across the whole range of acute coronary syndromes. Heart. 2003;89:512–6. doi: 10.1136/heart.89.5.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhadriraju S, Ray K, DeFranco A, et al. Association between blood glucose and long-term mortality in patients with acute coronary syndromes in the OPUS-TIMI 16 Trial. Am J Cardiol. 2006;97:1573–7. doi: 10.1016/j.amjcard.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 5.Timmer JR, van der Horst IC, Ottervanger JP, et al. Zwolle Myocardial Infarction Study Group Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399–404. doi: 10.1016/j.ahj.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 6.Iwakura K, Ito H, Ikushima M, et al. Association between hyperglycemia and the no-reflow phenomenon in patients with acute myocardial infarction. J Am Coll Cardiol. 2003;41:1–7. doi: 10.1016/s0735-1097(02)02626-8. [DOI] [PubMed] [Google Scholar]
- 7.Gandhi G, Nuttall G, Abel M, et al. Intraoperative hyperglycemia and perioperative outcomes in cardiac surgery patients. Mayo Clin Proc. 2005;80:862–6. doi: 10.4065/80.7.862. [DOI] [PubMed] [Google Scholar]
- 8.Doenst T, Wijeysundera D, Karkouti K, et al. Hyperglycemia during cardiopulmonary bypass is an independent risk factor for mortality in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2005;130:1144.e1–8. doi: 10.1016/j.jtcvs.2005.05.049. [DOI] [PubMed] [Google Scholar]
- 9.Fish LH, Weaver TW, Moore Al, Steel LG. Value of postoperative blood glucose in predicting complications and length of stay after coronary artery bypass grafting. Am J Cardiol. 2003;92:74–6. doi: 10.1016/s0002-9149(03)00472-7. [DOI] [PubMed] [Google Scholar]
- 10.Lazar HL, Chipkin SR, Fitzgerald CA, Bao Y, Cabral H, Apstein CS. Tight glycemic control in diabetic coronary artery bypass graft patients improves perioperative outcomes and decreases recurrent ischemic events. Circulation. 2004;109:1497–502. doi: 10.1161/01.CIR.0000121747.71054.79. [DOI] [PubMed] [Google Scholar]
- 11.Fortescue E, Kahn K, Bates D. Development and validation of a clinical prediction rule for major adverse outcomes in coronary bypass grafting. Am J Cardiol. 2001;88:1251–8. doi: 10.1016/s0002-9149(01)02086-0. [DOI] [PubMed] [Google Scholar]
- 12.Zindrou D, Taylor KM, Bagger JP. Admission plasma glucose: An independent risk factor in nondiabetic women after coronary artery bypass grafting. Diabetes Care. 2001;24:1634–9. doi: 10.2337/diacare.24.9.1634. [DOI] [PubMed] [Google Scholar]
- 13.Schmeltz LR, Desantis AJ, Thiyagarajan V, et al. Reduction of surgical mortality and morbidity in diabetic patients undergoing cardiac surgery with combined intravenous and subcutaneous insulin glucose management strategy. Diabetes Care. 2007;30:823–8. doi: 10.2337/dc06-2184. [DOI] [PubMed] [Google Scholar]