Abstract
Background:
Transfusion-related acute lung injury (TRALI) and transfusion-associated circulatory overload (TACO) commonly complicate transfusion in critically ill patients. Prior outcome studies of TACO and TRALI have focused on short-term morbidity and mortality, but the long-term survival and quality of life (QOL) of these patients remain unknown.
Methods:
In a nested case-control study, we compared survival and QOL between critically ill medical patients who developed pulmonary edema after transfusion (TRALI or TACO) and medical critically ill transfused controls, matched by age, gender, and admission diagnostic group. QOL in survivors was assessed with a 36-item short form health survey 1 year after initial hospitalization.
Results:
Hospital, 1-year, and 2-year mortality among the 74 TRALI cases and 74 matched controls were 43.2% vs 24.3% (P = .020), 63.8% vs 46.4% (P = .037) and 74.3% vs 54.3% (P = .031), whereas among the 51 TACO cases and 51 matched controls these values were 7.8% vs 11.8% (P = .727), 38.0% vs 28.0% (P = .371), and 44.9% vs 38.8% (P = .512). When adjusted for age and baseline severity of illness in a Cox proportional hazard analysis, the development of TRALI remained associated with decreased survival (hazard ratio 1.86; 95% CI, 1.19-2.93; P = .006). Both TRALI (P = .006, P = .03) and TACO (P = .03, P = .049) were associated with prolonged ICU and hospital lengths of stay.
Conclusions:
In critically ill medical patients, development of TRALI, but not TACO, is independently associated with decreased long-term survival.
A hydrostatic edema (transfusion-associated circulatory overload [TACO]) and a permeability edema (transfusion-related acute lung injury [TRALI]) are common pulmonary complications of blood transfusion. With advances in transfusion safety, in particular regarding the transmission of infectious agents, TRALI and TACO emerged as the most important transfusion complications. According to a US Food and Drug Administration report, TRALI was the most frequent cause of transfusion-related fatalities (65%) reported to the Food and Drug Administration during the years 2005 to 2007, with TACO (10%) and microbial contamination (12%) being the second most important reported causes of death.1 Our previous study2 confirmed the high frequency of TRALI (75 out of 903) and TACO (52 out of 903) in critically ill medical patients, which is previously largely underdiagnosed and underreported.3-6
TRALI is generally thought to be transient, reverses spontaneously, and carries a better prognosis compared with many other forms of acute lung injury (ALI), including ARDS.7,8 The mortality of TRALI reported to the transfusion services is estimated at 5%.3,9 There are no clear prognostic factors that influence mortality.10 Survivors had been reported to recover to their baseline oxygen saturation and pulmonary function without apparent sequelae.9 TACO may be the most underrecognized and serious transfusion complication.11 A study of orthopedic surgery12 patients reported that incidence of TACO was between 1% to 8%. Patients < 3 years of age or older than 60 years of age were at greatest risk.
Prior studies of TRALI and TACO have focused predominantly on short-term morbidity and mortality, but the long-term survival and quality of life (QOL) of these patients have not been systematically studied. This study was performed to identify the long-term survival and QOL of medical critically ill patients identified with TRALI and TACO in the prior prospective study.2
Materials and Methods
Consecutive patients transfused in a medical ICU of a tertiary care medical center were closely observed for 24 h after transfusion.2 Expert intensivists, blinded to specific transfusion factors, subsequently reviewed all clinical data and assigned the diagnosis of TRALI (suspected or possible TRALI) and TACO within 6 h of transfusion. TRALI was defined according to a recent Canadian Consensus Conference definition as a syndrome of inflammation and increased pulmonary capillary permeability that is associated with a constellation of clinical, radiologic, and physiologic abnormalities of acute pulmonary edema that cannot be explained by left atrial hypertension, that is, ALI developing within 6 h of transfusion.9,13 The term “possible TRALI” was used in the presence of other known risk factorsof ALI, including sepsis, pneumonia, trauma, and aspiration, although the transfusion itself may have had a contributory or even primary role in the development of the ALI.9,14,15 TACO was defined by a combination of clinical signs (gallop, jugular venous distension, systolic hypertension), radiographic (cardiothoracic ratio > 0.53 and vascular pedicle width > 65 mm), electrocardiographic (new ST segment and T wave changes), laboratory (elevated troponin T > 0.1 ng/mL), hemodynamic (pulmonary artery occlusion pressure > 18 mm Hg, central venous pressure > 12), echocardiographic findings (the ratio of mitral peak velocity of early filling to early diastolic mitral annular velocity [E/E′ ratio] > 15 and/or ejection fraction of < 45%], presence of severe left-sided valvular heart disease (aortic or mitral stenosis or regurgitation), and the prompt response to appropriate therapy: preload/afterload reduction, treatment of ischemia, or inotropic agents.5,11 The institutional review board approved the study protocol and patients who refused research authorization were excluded.
In the nested case-control study, long-term survival and QOL were compared between patients who developed TACO or TRALI/possible TRALI after transfusion with transfused control patients matched by age ± 10 years, sex, and admission diagnostic group.2 Prognostic and QOL variables were grouped as follows:
Patient factors before transfusion: Severity of illness was determined by calculating Acute Physiology and Chronic Health Evaluation (APACHE) III scores16 before transfusion. Sepsis, pneumonia, and chronic liver disease were defined according to standard clinical criteria.17,18
Transfusion factors: Units given 0 to 6 h before the development of ALI/ARDS (in cases)9,14,15 or 0 to 6 h after the beginning of the first transfusion (control subjects) were considered associated units. The exposure time for each control subject was matched to the exposure time of the corresponding case subject.2
Long-term QOL.
The QOL was assessed with the 36-item short form health survey (SF-36)19,20 at 1 year after hospital discharge. The eight domains of the SF-36 (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health) are clustered to form two higher order domains—the physical and mental health scores. Each domain is scored from 0 to 100, with 100 representing the best possible health state.
Statistical Analysis
Baseline characteristics and outcomes were compared among patients who developed TACO, TRALI/possible TRALI, and corresponding matched control groups. Data were expressed as mean values ± SD, median, or proportions. Paired parametric and nonparametric testing was used in univariate analyses as appropriate. The Kaplan-Meier survival curves were compared with the log-rank test. If a significant difference existed in Kaplan-Meier survival analyses between the matched groups, the impact of transfusion complications on long-term survival was analyzed by Cox regression analysis. Cox proportional hazard model selection was done with a backward stepwise method starting from all of the variables with P < .05 in univariate analyses, taking into account colinearity and clinical plausibility. SAS, version 9, statistical software was used for all analyses (SAS Institute, Inc.; Cary, NC).
Results
The study subjects were followed for median 825 days (interquartile range, 214-1,265 days). The 1- and 2-year follow-up rates were 98.4% and 97.6%. Baseline characteristics, short-term outcomes, and long-term outcomes of patients who developed TRALI/possible TRALI or TACO, and corresponding matched controls are presented in Table 1. Baseline severity of illness was similar between cases and controls. Patients who developed TRALI/possible TRALI had longer ICU and hospital lengths of stay (LOS) and higher hospital, 1-year, and 2-year mortality. Patients who developed TACO also had longer ICU and hospital LOS, but mortality was not significantly different.
Table 1.
—Baseline Characteristics and Outcome of Transfusion-Associated Circulatory Overload, Transfusion-Related Acute Lung Injury, and Matched Controls
| Medical Variables | TRALI/Possible TRALI(n = 74) | TRALI Controls(n = 74) | TACO(n = 51) | TACO Controls(n = 51) |
| Age (SD), y | 61.2 (17.8) | 62.5 (17.6) | 69.8 (14.9) | 71.5 (14.2) |
| Female gender, No. (%) | 37 (50) | 37 (50) | 24 (47.1) | 24 (47.1) |
| APACHE III scores | 61 (44-75) | 57 (45-81) | 24 (17-41) | 24 (16-42) |
| Chronic liver disease, No. (%) | 20 (27.4)a | 11 (15.1) | 10 (19.6) | 6 (11.8) |
| Sepsis, No. (%) | 27 (36.5)a | 16 (21.6) | 10 (19.6) | 9 (17.7) |
| Number of associated transfusions, median (IQR) | 3 (1-5) | 2 (1-3) | 3 (2-6)a | 2 (2-3) |
| ICU LOS, days | 4.7 (2.4-7.8)a | 2.1 (1.1-5.3) | 3.0 (1.9-4.2)a | 1.7 (1.0-3.1) |
| Hospital LOS, days | 11.5 (7.0-19.3)a | 7.8 (3.6-14.0) | 9.4 (5.7-13.8)a | 6.1 (3.9-10.0) |
| Hospital mortality, No. (%) | 32 (43.2)a | 18 (24.3) | 4 (7.8) | 6 (11.8) |
| 1-y mortality, No. (%)b | 46 (63.8)a | 33 (46.4)a | 19 (38.0) | 14 (28.0) |
| 2-y mortality, No. (%)c | 52 (74.3)a | 38 (54.3)a | 22 (44.9) | 19 (38.8) |
APACHE = Acute Physiology and Chronic Health Evaluation; IQR = interquartile range; LOS = length of stay; TACO = transfusion-associated circulatory overload; TRALI = transfusion-associated acute lung injury.
Significant difference between cases and controls (P < .05).
71 pairs of TRALI and controls, 50 pairs of TACO and controls.
70 pairs of TACO and controls; 49 pairs of TACO and controls.
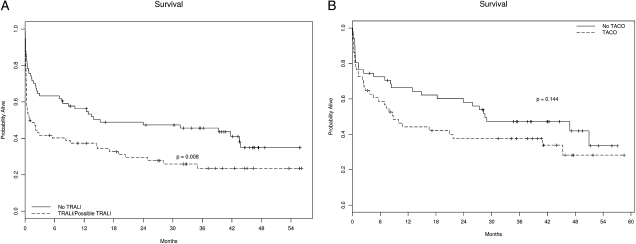
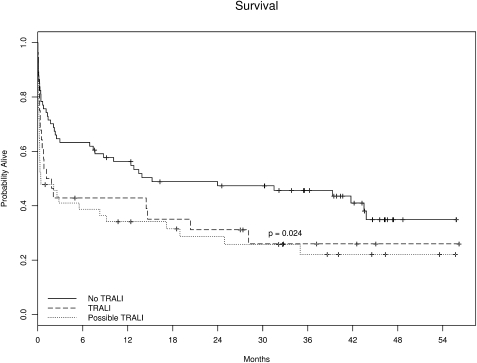
Survival curves of TRALI/possible TRALI and TACO vs controls are presented in Figure 1. Long-term survival was reduced in TRALI/possible TRALI cases compared with matched controls (P = .008). When the analysis was restricted to TRALI cases (excluding possible TRALI), the median survival remained significantly lower than in matched controls (35 vs 410 days, P = .024) (Fig 2). Compared with matched controls, TACO cases also had a reduced survival, but this difference did not reach statistical significance (P = .144). There was no significant difference in survival between TRALI and possible TRALI (1-year survival: 40% vs 31%, P = .752; 2-year survival: 29% vs 23%, P = .930). In a post hoc analysis, patients treated for non-transfusion-related ALI had similar hospital mortality to patients with transfusion-related ALI (40% vs 43.2%, P = .743, χ2 test).
Figure 1.
Survival curve of TRALI/possible TRALI vs matched control group (A). Survival curve of TACO vs matched control group (B). TACO = transfusion-associated circulatory overload; TRALI = transfusion-associated acute lung injury.
Figure 2.
Survival curve of no TRALI, TRALI, and possible TRALI. See Figure 1 legend for expansion of abbreviation.
When adjusted for baseline characteristics in a multivariate Cox proportional hazards model, the development of TRALI/possible TRALI remained significantly associated with decreased survival (hazard ratio [HR], 1.86; 95% CI, 1.19-2.93; P = .006]. Other important prognostic factors included pre-transfusion APACHE III scores (HR, 1.19; 95% CI, 1.09-1.29; P < .001), age (HR, 1.02; 95% CI, 1-1.03; P = .009) and chronic liver disease (HR, 2.12; P = .005).
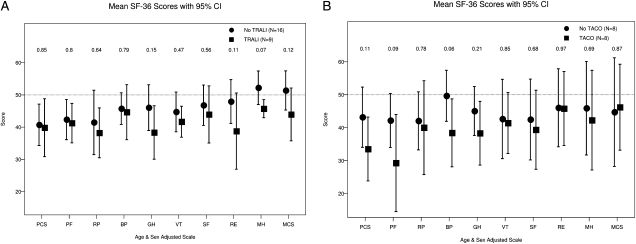
Half (50%) of 1-year survivors returned QOL surveys. Composite and individual components of QOL survey were similar between surviving cases of TACO and TRALI and corresponding matched controls (Fig 3).
Figure 3.
Mean SF-36 scores 1 year later. TRALI vs matched controls (A). TACO vs matched controls (B). SF-36 = 36-item short form health survey. See Figure 1 legend for expansion of other abbreviations.
Discussion
In this single-center prospective observational cohort of critically ill medical patients, the development of TRALI was associated with decreased long-term survival. Additional poor prognostic features included older age, history of liver disease, and higher severity of illness. Compared with matched controls, TACO cases also had a reduced survival, but this difference did not reach statistical significance. Both TRALI and TACO were associated with prolonged ICU and hospital LOS. QOL scores were lower than the age-adjusted population predictions, but were not significantly different between responding survivors who did and did not develop transfusion-associated pulmonary complications.
To our knowledge, this is the first long-term follow-up study of critically ill medical patients who experienced transfusion-associated pulmonary complications—TRALI and TACO. With better control of the transfusion products, the risk of transmission of infectious agents decreased.21-23 Serious noninfectious hazards have emerged as the most common adverse reactions related to transfusion. In addition to TRALI and TACO, less common complications include posttransfusion purpura, transfusion-associated graft vs host disease, microchimerism, transfusion-related immunomodulation, alloimmunization, metabolic derangements, coagulopathic complications of massive transfusion, complications from red cell storage lesions, complications from overtransfusion or undertransfusion, and iron overload.24 TRALI and TACO are frequently confused with one another and account for most of the morbidity and mortality from acute transfusion reactions in the United States.8,25,26
Although TACO had been recognized as a complication of transfusion for decades, it received relatively little attention in the scientific literature.27 The prolonged hospital LOS observed in our study is similar to the results of a previous study in orthopedic surgical patients who developed TACO postoperatively.12 TACO is similar to other causes of acute hydrostatic pulmonary edema and the outcome varies with the overall clinical status of the patient. Clinical consequences include prolonged hospitalization, greater intensity of care, and death.11
TRALI is generally thought to have a better prognosis compared with other causes of ALI and ARDS.3,28,29 Most patients recover rapidly, and there are no long-term sequelae.3 Relatively high mortality of our suspected or possible TRALI cases is similar to some30-32 but higher than in other epidemiologic studies.5,28,33 The following reasons are likely to explain a significantly higher observed mortality in our study: The population of our study was from a medical ICU in a tertiary care medical center, a group with an inherently high mortality rate, even in the absence of transfusion complications. More importantly, our definition included cases of possible TRALI9,14,15 in whom transfusion was not the only factor contributing to ALI. Compared with TRALI control group, the result is similar even excluding possible TRALI cases, which could be explained by a “two-hit” model of TRALI: underlying patient characteristics (first hit) and specific transfusion factors (second hit) were associated with the development of ALI after blood transfusion.34,35
It is important to emphasize that the transfusion is one of multiple hits in the development of ALI, analogous to the interplay between high BP, smoking, and high cholesterol in the pathogenesis of coronary disease. It is postulated that neutrophil priming factors (antibodies and biologic response modifiers) in the transfused component can mediate TRALI in a patient with preexisting (first hit) pulmonary endothelial activation.26 Such a two-hit (or multiple-hit) hypothesis has been used to explain the occurrence of both TRALI 27,28,36,37 and ALI in general.38-40 The advances in understanding the mechanisms of TRALI have led to new emphasis on its prevention.23,41-45
A small number of responders limit the interpretation of the 1-year QOL surveys in our study. Recent systematic review of QOL after ARDS evaluated by SF-36 suggests that despite early improvement in some domains, QOL in ARDS survivors remains persistently lower than in the healthy population.46 Other studies have shown similar long-term QOL outcome between ALI/ARDS and matched controls. Cooper et al47 found that impairments in QOL among ARDS survivors may not be distinguishable from those among other ICU survivors. No significant difference was found by Granja et al48 in QOL between ARDS and other ICU survivors matched by age, previous health state, and severity of disease. Our study was consistent with findings by Granja and Cooper and showed no significant difference in SF-36 scores of TRALI and TACO cases vs matched controls 1 year after discharge from the hospital.
Our study has significant limitations. The prognosis of critically ill medical patients treated in a tertiary care institution can hardly be extrapolated to other settings. Definitions of TRALI and TACO are prone to subjective interpretation and it is possible that some patients have been misclassified. We restricted our study to pulmonary complications occurring within 6 h of transfusion (according to consensus conference criteria) and did not take into account the potential for delayed reactions, including ALI49 and pulmonary infections and other reactions resulting from transfusion-related immunomodulation.50-52 Only 50% of 1-year survivors completed SF-36 questionnaires. Our follow-up did not include important events that occurred after initial hospitalization (including possible recurrent episodes of TRALI or TACO).
In conclusion, in the long-term follow-up study of transfused critically ill medical patients in a tertiary care center, the development of TRALI was associated with decreased survival, with most deaths occurring during initial hospitalization. Poor prognostic features included the occurrence of TRALI, older age, history of liver disease, and higher severity of illness (APACHE III scores). Both TACO and TRALI were associated with longer ICU and hospital LOS.
Acknowledgments
Author contributions: Dr Li: contributed to drafting the manuscript.
Dr Kojicic: contributed to data collection and management.
Dr Reriani: contributed to drafting the manuscript.
Dr Fernández Pérez: contributed to drafting the manuscript.
Dr Thakur: contributed to data collection and management.
Dr Kashyap: contributed to data collection and management.
Dr Van Buskirk: contributed to designing the research and revising the article.
Dr Gajic: contributed to designing the research and revising the article.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Other contributions: This study was performed at the Mayo Clinic, Rochester, MN.
Abbreviations
- ALI
acute lung injury
- APACHE
Acute Physiology and Chronic Health Evaluation
- HR
hazard ratio
- LOS
length of stay
- QOL
quality of life
- SF-36
36-item short form health survey
- TACO
transfusion-associated circulatory overload
- TRALI
transfusion-related acute lung injury
Footnotes
Funding/Support: This work was supported by grants from the National Heart Lung and Blood Institute, Special Center of Research in Transfusion Medicine [Grant HL81027] and the National Institutes of Health [Grant HL78743].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestpubs.org/site/misc/reprints.xhtml).
References
- 1.US Food and Drug Administration Fatalities reported to FDA following blood collection and transfusion: annual summary for fiscal year 2007. http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ReportaProblem/TransfusionDonationFatalities/ucm118316.htm.
- 2.Gajic O, Rana R, Winters JL, et al. Transfusion-related acute lung injury in the critically ill: prospective nested case-control study. Am J Respir Crit Care Med. 2007;176(9):886–891. doi: 10.1164/rccm.200702-271OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Popovsky MA, Chaplin HC, Jr, Moore SB. Transfusion-related acute lung injury: a neglected, serious complication of hemotherapy. Transfusion. 1992;32(6):589–592. doi: 10.1046/j.1537-2995.1992.32692367207.x. [DOI] [PubMed] [Google Scholar]
- 4.Kopko PM, Marshall CS, MacKenzie MR, Holland PV, Popovsky MA. Transfusion-related acute lung injury: report of a clinical look-back investigation. JAMA. 2002;287(15):1968–1971. doi: 10.1001/jama.287.15.1968. [DOI] [PubMed] [Google Scholar]
- 5.Popovsky MA. Transfusion and the lung: circulatory overload and acute lung injury. Vox Sang. 2004;87(suppl 2):62–65. doi: 10.1111/j.1741-6892.2004.00453.x. [DOI] [PubMed] [Google Scholar]
- 6.Rana R, Mendez JL, Rickman OB, et al. Transfusion related acute lung injury in medical intensive care unit: a four months pilot prospective study [abstract] Proc Am Thorac Soc. 2005;2:B51S. [Google Scholar]
- 7.Kopko PM, Holland PV. Transfusion-related acute lung injury. Br J Haematol. 1999;105(2):322–329. doi: 10.1111/j.1365-2141.1999.01357.x. [DOI] [PubMed] [Google Scholar]
- 8.Davis A, Mandal R, Johnson M, Makar R, Stowell C, Dzik S. A touch of TRALI. Transfusion. 2008;48(3):541–545. doi: 10.1111/j.1537-2995.2007.01567.x. [DOI] [PubMed] [Google Scholar]
- 9.Kleinman S, Caulfield T, Chan P, et al. Toward an understanding of transfusion-related acute lung injury: statement of a consensus panel. Transfusion. 2004;44(12):1774–1789. doi: 10.1111/j.0041-1132.2004.04347.x. [DOI] [PubMed] [Google Scholar]
- 10.Holness L, Knippen MA, Simmons L, Lachenbruch PA. Fatalities caused by TRALI. Transfus Med Rev. 2004;18(3):184–188. doi: 10.1016/j.tmrv.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Popovsky MA. Pulmonary consequences of transfusion: TRALI and TACO. Transfus Apher Sci. 2006;34(3):243–244. doi: 10.1016/j.transci.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Popovsky MA, Audet AM, Andrzejewski C., Jr Transfusion-associated circulatory overload in orthopedic surgery patients: a multi-institutional study. Immunohematology. 1996;12(2):87–89. [PubMed] [Google Scholar]
- 13.Toy P, Lowell C. TRALI—definition, mechanisms, incidence and clinical relevance. Best Pract Res Clin Anaesthesiol. 2007;21(2):183–193. doi: 10.1016/j.bpa.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 pt 1):818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 15.Gajic O, Gropper MA, Hubmayr RD. Pulmonary edema after transfusion: how to differentiate transfusion-associated circulatory overload from transfusion-related acute lung injury. Crit Care Med. 2006;34(5) Suppl:S109–S113. doi: 10.1097/01.CCM.0000214311.56231.23. [DOI] [PubMed] [Google Scholar]
- 16.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 17.American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20(6):864–874. [PubMed] [Google Scholar]
- 18.Bartlett JG, Dowell SF, Mandell LA, File TM, Jr, Musher DM, Fine MJ. Infectious Diseases Society of America Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis. 2000;31(2):347–382. doi: 10.1086/313954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ware JEKM, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston, MA: New England Medical Center; 1994. [Google Scholar]
- 20.Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26(7):724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Satake M, Mitani T, Oikawa S, et al. Frequency of bacterial contamination of platelet concentrates before and after introduction of diversion method in Japan. Transfusion. 2009;49(10):2152–2157. doi: 10.1111/j.1537-2995.2009.02243.x. [DOI] [PubMed] [Google Scholar]
- 22.Walther-Wenke G. Incidence of bacterial transmission and transfusion reactions by blood components. Clin Chem Lab Med. 2008;46(7):919–925. doi: 10.1515/CCLM.2008.151. [DOI] [PubMed] [Google Scholar]
- 23.Spahn DR, Moch H, Hofmann A, Isbister JP. Patient blood management: the pragmatic solution for the problems with blood transfusions. Anesthesiology. 2008;109(6):951–953. doi: 10.1097/ALN.0b013e31818e3d75. [DOI] [PubMed] [Google Scholar]
- 24.Hendrickson JE, Hillyer CD. Noninfectious serious hazards of transfusion. Anesth Analg. 2009;108(3):759–769. doi: 10.1213/ane.0b013e3181930a6e. [DOI] [PubMed] [Google Scholar]
- 25.Skeate RC, Eastlund T. Distinguishing between transfusion related acute lung injury and transfusion associated circulatory overload. Curr Opin Hematol. 2007;14(6):682–687. doi: 10.1097/MOH.0b013e3282ef195a. [DOI] [PubMed] [Google Scholar]
- 26.Triulzi DJ. Transfusion-related acute lung injury: current concepts for the clinician. Anesth Analg. 2009;108(3):770–776. doi: 10.1213/ane.0b013e31819029b2. [DOI] [PubMed] [Google Scholar]
- 27.Popovsky MA. Transfusion and lung injury. Transfus Clin Biol. 2001;8(3):272–277. doi: 10.1016/s1246-7820(01)00111-2. [DOI] [PubMed] [Google Scholar]
- 28.Popovsky MA, Moore SB. Diagnostic and pathogenetic considerations in transfusion-related acute lung injury. Transfusion. 1985;25(6):573–577. doi: 10.1046/j.1537-2995.1985.25686071434.x. [DOI] [PubMed] [Google Scholar]
- 29.Webert KE, Blajchman MA. Transfusion-related acute lung injury. Transfus Med Rev. 2003;17(4):252–262. doi: 10.1016/s0887-7963(03)00039-7. [DOI] [PubMed] [Google Scholar]
- 30.Rana R, Fernández-Pérez ER, Khan SA, et al. Transfusion-related acute lung injury and pulmonary edema in critically ill patients: a retrospective study. Transfusion. 2006;46(9):1478–1483. doi: 10.1111/j.1537-2995.2006.00930.x. [DOI] [PubMed] [Google Scholar]
- 31.Wallis JP, Lubenko A, Wells AW, Chapman CE. Single hospital experience of TRALI. Transfusion. 2003;43(8):1053–1059. doi: 10.1046/j.1537-2995.2003.00466.x. [DOI] [PubMed] [Google Scholar]
- 32.Li GS, Ye QF, Xia SS, et al. Acute respiratory distress syndrome after liver transplantation: etiology, prevention and management. Hepatobiliary Pancreat Dis Int. 2002;1(3):330–334. [PubMed] [Google Scholar]
- 33.Moore SB. Transfusion-related acute lung injury (TRALI): clinical presentation, treatment, and prognosis. Crit Care Med. 2006;34(5) suppl:S114–S117. doi: 10.1097/01.CCM.0000214312.20718.3E. [DOI] [PubMed] [Google Scholar]
- 34.Silliman CC, Ambruso DR, Boshkov LK. Transfusion-related acute lung injury. Blood. 2005;105(6):2266–2273. doi: 10.1182/blood-2004-07-2929. [DOI] [PubMed] [Google Scholar]
- 35.Silliman CC. The two-event model of transfusion-related acute lung injury. Crit Care Med. 2006;34(5) suppl:S124–S131. doi: 10.1097/01.CCM.0000214292.62276.8E. [DOI] [PubMed] [Google Scholar]
- 36.Popovsky MA, Haley NR. Further characterization of transfusion-related acute lung injury: demographics, clinical and laboratory features, and morbidity. Immunohematology. 2000;16(4):157–159. [PubMed] [Google Scholar]
- 37.Popovsky MA. Breathlessness and blood: a combustible combination. Vox Sang. 2002;83(suppl 1):147–150. doi: 10.1111/j.1423-0410.2002.tb05290.x. [DOI] [PubMed] [Google Scholar]
- 38.Hudson LD, Milberg JA, Anardi D, Maunder RJ. Clinical risks for development of the acute respiratory distress syndrome. Am J Respir Crit Care Med. 1995;151(2 pt 1):293–301. doi: 10.1164/ajrccm.151.2.7842182. [DOI] [PubMed] [Google Scholar]
- 39.Matthay MA, Zimmerman GA, Esmon C, et al. Future research directions in acute lung injury: summary of a National Heart, Lung, and Blood Institute working group. Am J Respir Crit Care Med. 2003;167(7):1027–1035. doi: 10.1164/rccm.200208-966WS. [DOI] [PubMed] [Google Scholar]
- 40.Repine JE. Scientific perspectives on adult respiratory distress syndrome. Lancet. 1992;339(8791):466–469. doi: 10.1016/0140-6736(92)91067-i. [DOI] [PubMed] [Google Scholar]
- 41.Hume HA. TRALI: moving toward prevention. Transfusion. 2009;49(3):402–405. doi: 10.1111/j.1537-2995.2008.02090.x. [DOI] [PubMed] [Google Scholar]
- 42.Vlaar AP, Binnekade JM, Schultz MJ, Juffermans NP, Koopman MM. Preventing TRALI: ladies first, what follows? Crit Care Med. 2008;36(12):3283–3284. doi: 10.1097/CCM.0b013e31818f2f37. [DOI] [PubMed] [Google Scholar]
- 43.Valeri CR, Ragno G. Prevention of TRALI. Vox Sang. 2008;94(1):81. doi: 10.1111/j.1423-0410.2007.00996.x. [DOI] [PubMed] [Google Scholar]
- 44.Powers A, Stowell CP, Dzik WH, et al. Testing only donors with a prior history of pregnancy or transfusion is a logical and cost-effective transfusion-related acute lung injury prevention strategy. Transfusion. 2008;48(12):2549–2558. doi: 10.1111/j.1537-2995.2008.01902.x. [DOI] [PubMed] [Google Scholar]
- 45.Wright SE, Snowden CP, Athey SC, et al. Acute lung injury after ruptured abdominal aortic aneurysm repair: the effect of excluding donations from females from the production of fresh frozen plasma. Crit Care Med. 2008;36(6):1796–1802. doi: 10.1097/CCM.0b013e3181743c6e. [DOI] [PubMed] [Google Scholar]
- 46.Dowdy DW, Eid MP, Dennison CR, et al. Quality of life after acute respiratory distress syndrome: a meta-analysis. Intensive Care Med. 2006;32(8):1115–1124. doi: 10.1007/s00134-006-0217-3. [DOI] [PubMed] [Google Scholar]
- 47.Cooper AB, Ferguson ND, Hanly PJ, et al. Long-term follow-up of survivors of acute lung injury: lack of effect of a ventilation strategy to prevent barotrauma. Crit Care Med. 1999;27(12):2616–2621. doi: 10.1097/00003246-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Granja C, Morujão E, Costa-Pereira A. Quality of life in acute respiratory distress syndrome survivors may be no worse than in other ICU survivors. Intensive Care Med. 2003;29(10):1744–1750. doi: 10.1007/s00134-003-1808-x. [DOI] [PubMed] [Google Scholar]
- 49.Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008;36(9):2667–2674. doi: 10.1097/CCM.0b013e3181844677. [DOI] [PubMed] [Google Scholar]
- 50.Atzil S, Arad M, Glasner A, et al. Blood transfusion promotes cancer progression: a critical role for aged erythrocytes. Anesthesiology. 2008;109(6):989–997. doi: 10.1097/ALN.0b013e31818ddb72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bucová M, Mistrík M. Transfusion-induced immunomodulation and infectious complications [in Czech] Vnitr Lek. 2006;52(11):1085–1092. [PubMed] [Google Scholar]
- 52.Nishimura M, Mitsunaga S, Ishikawa Y, Satake M. Possible mechanisms underlying development of transfusion-related acute lung injury: roles of anti-major histocompatibility complex class II DR antibody. Transfus Med. 2003;13(3):141–147. doi: 10.1046/j.1365-3148.2003.00434.x. [DOI] [PubMed] [Google Scholar]