Abstract
Study Design
Prospective controlled study.
Purpose
The results of conventional open surgery was compared with those from minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for lumbar fusion to determine which approach resulted in less postoperative paraspinal muscle degeneration.
Overview of Literature
MI TLIF is new surgical technique that appears to minimize iatrogenic injury. However, there aren't any reports yet that have quantitatively analyzed and proved whether there's difference in back muscle injury and degeneration between the minimally invasive surgery and conventional open surgery in more than 1 year follow-up after surgery.
Methods
This study examined a consecutive series of 48 patients who underwent lumbar fusion in our hospital during the period, March 2006 to March 2008, with a 1-year follow-up evaluation using MRI. There were 17 cases of conventional open surgery and 31 cases of MI-TLIF (31 cases of single segment fusion and 17 cases of multi-segment fusion). The digital images of the paravertebral back muscles were analyzed and compared using the T2-weighted axial images. The point of interest was the paraspinal muscle of the intervertebral disc level from L1 to L5. Picture archiving and communication system viewing software was used for quantitative analysis of the change in fat infiltration percentage and the change in cross-sectional area of the paraspinal muscle, before and after surgery.
Results
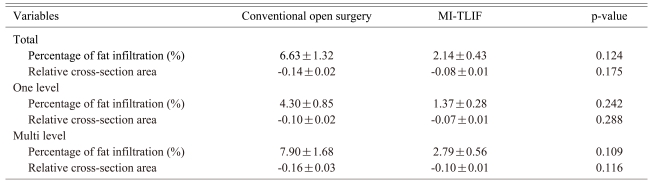
A comparison of the traditional posterior fusion method with MI-TLIF revealed single segment fusion to result in an average increase in fat infiltration in the paraspinal muscle of 4.30% and 1.37% and a decrease in cross-sectional area of 0.10 and 0.07 before and after surgery, respectively. Multi-segment fusion showed an average 7.90% and 2.79% increase in fat infiltration and a 0.16 and 0.10 decrease in cross-sectional area, respectively. Both single and multi segment fusion showed less change in the fat infiltration percentage and cross-sectional area, particularly in multi segment fusion. There was no significant difference between the two groups in terms of the radiologic results.
Conclusions
A comparison of conventional open surgery with MI-TLIF upon degeneration of the paraspinal muscle with a 1 year follow-up evaluation revealed that both single and multi segment fusion showed less change in fat infiltration percentage and cross-sectional area in the MI-TLIF but there was no significant difference between the two groups. This suggests that as time passes after surgery, there is no significant difference in the level of degeneration of the paraspinal muscle between surgical techniques.
Keywords: Paraspainal muscle, Fat degeneration, MRI, Posterior fusion
Introduction
One of the most important functions of the trunk muscle is to support the vertebral body. In particular, the back muscle, which is the extensor muscle of the lower lumber part, plays a pivotal role in the stability of the lumbar segment, and is essential in the dynamic control of segmentation movement. A direct injury to the back muscle during surgery for posterior fusion or an indirect injury from ischemia and denervation during the process of retracting the back muscle with long hours of excessive pressure are inevitable and might cause muscular atrophy and pain. This has become a major issue in failed back surgery syndrome1. Recently, with posterior vertebral surgery, there have been reports of a relationship between back muscle injury with an excessive muscle dissection2 and the retraction time and pressure of the back muscle3-5 from a spinous process and lamina through the histological, enzymological, radiological quantification of a back muscle injury and degeneration. As a solution for these issues, there has been increasing interest in neural decompression and interbody fusion that employ minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) minimizing soft tissue injury, peripheral tissue injury and loss of blood6,7.
There are reports showing that the minimally invasive approach can reduce muscular injury and systemic inflammatory response compared to the temporal approach by serologically analyzing the degree of back muscle injury immediately after surgery8. However, there are no reports that have quantitatively analyzed and demonstrated a difference in back muscle injury and degeneration between minimally invasive surgery and conventional open surgery after a follow-up of more than 1 year after surgery.
Therefore, as the degree of comparison between tissues is excellent, the authors compared the results by quantitatively analyzing the degree of back muscle degeneration after posterior fusion according to the surgical approach by MRI, where measurements of the percentage fat infiltration of the skeletal muscles9,10 and muscle mass11 is possible through linkage with a range of software.
Materials and Methods
1. Research design and materials
For this study, the preoperative selection of subjects and those to be observed for postoperative back muscle degeneration was performed in a prospective manner. Forty eight patients had received posterior fusion of either a single or multi-segment with spinal stenosis at our hospital from March 2006 to March 2008 and were available for a 1 year MRI follow-up (Average of 12.7 months, 11 to 29 months). Among the patients, those with a history of spinal surgery, possible atrophy in the back muscle according to a preoperative MRI inspection or possible malignant tumor or infections in the spine were excluded.
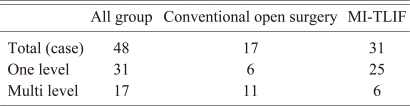
There were 17 cases of conventional open surgery (10 cases of posterior lumbar interbody fusion, 7 cases of posterolateral fusion) and 31 cases of MI-TLIF. There were 31 cases of single segment fusion and 17 cases of multi-segment fusion (Table 1). In this study, there were many cases of multi-segment fusion in the group that underwent conventional open surgery and in cases of single segment fusion in the group that had undergone MI-TLIF. As the quantification analysis of back muscle degeneration can differ according to the approaches, the analysis was made by classifying the subjects into single segment and multi-segment fusions according to the number of fusion segments.
Table 1.
Case analysis
MI-TLIF: minimally invasive transforaminal lumbar interbody fusion.
There were 17 men and 31 women with an average age at the time of surgery of 57 years (range, 30 to 77 years). The mean follow-up period was 18 months(range,12 to 29 months). All procedures were performed by a single surgeon at the same institution.
2. Surgical methods
For conventional open surgery, a horizontal skin incision was performed along the center line around the lesion, and a muscular dissection and detachment were performed from the spinous process and lamina using bipolar electrocautery so that the lower lamina and outer border of the facet joint could be seen. Posterior decompression, disectomy, interbody fusion and fixation of a vertebral body screw were then performed with the muscle being pulled using a Codman spinal retractor.
For MI-TLIF, two paramedian skin incisions, 2.5 cm in length, were made on the site approximately 2.5 cm apart from the midline, and the approach was made between the muscles reaching up to the lamina and facet joint through a blunt dissection of the multifidus and longissimus muscle. When the facet joint was exposed, facet joint removal, posterior soft tissue decompression, disc removal and interbody fusion were performed with the muscle being pulled using the tubular retractor system. When the vertebral body screw was fixed, fixation of percutaneous vertebral body screw was performed by C-arm fluoroscopy through the multifidus and longissimus muscle.
Walking began by applying a lumbosacral orthoses from 1 day after surgery, and was worn for 3 months by observing the fusion state by X-rays in the outpatient follow-up.
3. Image acquisition and analysis
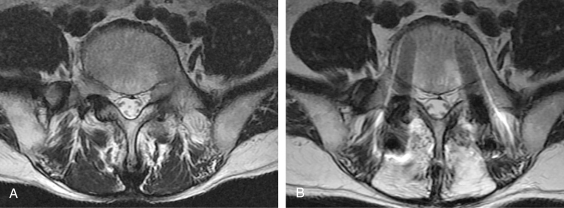
MRI was performed using a 1.5-Tesla model (Signa; General Electric Medical Systems, Milwaukee, WI, USA) in the supine position with the legs spread and the lumbar area in the neutral position. An axial plane image was acquired with 3 sections per disc range in the T2 enhanced image (TE/TR 122/4000, DFOV 280.0 mm, NEX 4, slice thickness/gap 4 mm/1 mm) so that each disc become horizontal by setting the position of the lumbar disc in the sagittal plane. Among these, images of the center site on the disc in the sagittal plane were taken. Postoperative MRI was performed approximately 1 year after surgery when postoperative edema and swelling of the muscles had disappeared. To minimize the intervention of the vertebral pedicle screw and metal rods artifact of the fusion site, the uppermost axial plane image were selected instead of the middle part of the disc (Fig. 1).
Fig. 1.
Magnetic resonance imaging of the preoperative shows healthy back muscle (A), whereas that of the postoperative shows muscular atrophy and fat infiltration (B).
After scanning, the images were stored in the form of a DICOM file using image storage and transmission system software. The images were analyzed using MultiVox (Tech-Heim, Seoul, Korea) and PiView (Infinitt, Seoul, Korea) digital image software.
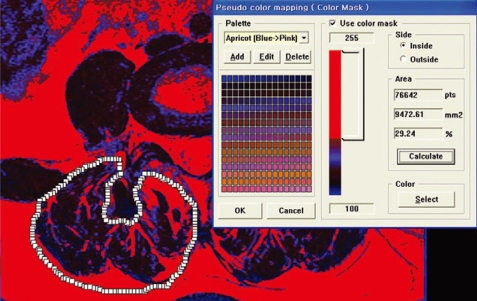
The areas of interest of the back muscle were established on the lumbar's T2 enhanced axial image at the L1-L2, L2-L3, L3-L4 and L4-L5 disc level, and the proportion for each cross-sectional area and fat infiltration were measured and analyzed. The L5-S1 level was not included because the axial cutting gantry was obstructed by the iliac crest and the muscular anatomy was quite different from the upper levels. The regions of interest were outlined with a graphic cursor around the back muscle on the right side, as well as on the intervertebral disc at each level. The fascia thoracolumbalis was traced down laterally and anteriorly to the dorsal side of the quadratus lumborum, followed by the posterior surface of the facet and lamina, and lateral margin of the spinous process. In the areas of interest, the cross-sectional area of the back muscle before and after surgery at each disc level was measured. Their average values were obtained and the degree of preoperative and postoperative back muscle cross-sectional area was calculated to determine if there was a difference between the groups (Fig. 2). The percentage muscle fat infiltration was measured using the pseudo coloring technique12, and was also compared to determine if there was a difference in the change from before and after surgery between the groups (Fig. 3).
Fig. 2.
Bright pixels of fat tissue in the MR images were colored in red (darker color in the black and white version) using a pseudocoloring technique. The percentage of red pixel area(fat components) in the muscle compartment was calculated and read in the signal intensity histogram.
Fig. 3.
Areas of the right-sided back muscle were measured using the picture archiving and communication system viewing software tools.
One radiological specialist and two orthopedic specialists analyzed the images. Each value was measured 3 times by each specialist with an at least 2 week interval between measurements.
4. Statistical analysis
An independent specimen t-test was used to make a comparison between each group and determine the statistical significance using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A p-value <0.05 level was considered significant. The degree of agreement between the measurers was evaluated using the intraclasscorrelation coefficients (ICCs) introduced by Shrout and Fleiss13.
Results
The degree of postoperative back muscle fat degeneration in the conventional open surgery and MI-TLIF group increased 6.63% and 2.14%, respectively, compared to the preoperative figures, whereas the cross-sectional area decreased 0.14 and 0.08, respectively. For single segment fusion, the degree of postoperative back muscle fat degeneration increased 4.30% and 1.37%, respectively, compared to the preoperative figures, whereas the cross-sectional area decreased 0.10 and 0.07, respectively. For multi-segment fusion, the degree of postoperative back muscle fat degeneration increased 7.90% and 2.79%, respectively, compared to the preoperative figures, whereas the cross-sectional area decreased 0.16 and 0.10, respectively (Table 2). Although the difference in degeneration measurements between the approaches were larger in the group that had undergone multi-segment fusion compared to the group that had undergone single segment fusion, the difference was not significant (p>0.05).
Table 2.
The postoperative changes of back muscle on the conventional open surgery and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF)
*It were compared and analyzed by obtaining the total average value.
Discussion
In performing spinal fusion, there are many factors that might cause iatrogenic and degenerative changes to the back muscle. In particular, conventional open surgery can cause ischemia and denervation of the back muscle due to the need to make a long skin incision and also from the long hours of excessive pressure during the process of retracting the back muscle from the spinous process1,2. According to Kawaguchi et al.3-5, back muscle injury at the time of posterior lumbar surgery is related to the operation time and retraction pressure. Therefore, it is recommended that the retraction be released for 5 minutes after 1 hour of retraction to prevent serious back muscle injury. Gejo et al.14 also reported that the muscle retraction time influences the osteoperative back muscle function, and more than 2 hours pressure after retraction is believed to reduce the flow of capillary vessels, causing ischemic intramuscular changes15-17. Recently, as a solution for these issues, MI-TLIF has attracted considerable attention because it minimizes the level of soft tissue injury during surgery, surrounding muscle injury and blood loss during surgery6,7. Stevens et al.18 compared the pressure applied to the muscles between the two approaches using a cadaver with a minimally invasive approach and reported a lower value with MI-TLIF.
In this study, a relatively long skin incision was applied to detach the back muscle from the bones, which is known as conventional open surgery, and considerable pressure was applied for many hours when all surgical methods were performed to retract both sides of the back muscle, which may cause injury or degeneration. On the other hand, a relatively short skin incision was made in MI-TLIF with a blunt dissection of the space between the muscles, which reduces the direct muscle injury, and the time for back muscle retraction is relatively short and there is a lower degree of pressure because the surgery is performed through 2 incisions on the site. Therefore, methods to quantify them have been examined with the aim of reducing the level of back muscle degeneration.
Hyun et al.19 reported that the paramedian interfascial approach may preserve the back muscle even more by comparing the degree of back muscle injury according to the midline and paramedian approaches in lumbar fusion through postoperative quantification of back muscle mass using Computed tomography in 26 patients. However, computed tomography has difficulty in observing fat infiltrations, degenerative changes, and internal structures in patients who have undergone fixation by inserting metallic objects due to the artifacts20. Therefore, many attempts have been made to evaluate the degree of muscle injury by measuring the degree of back muscle injury with a serological evaluation after diverse lumbar surgeries1,21. Kim et al.8 reported that in lumbar fusion, the minimally invasive approach contributes considerably to reducing the level of postoperative muscular injury and systemic inflammatory response compared to the temporary approach through quantitative analysis that employs serum enzymes, such as creatine phosphokinase, inflammatory cytokine etc. After operating on 17 cases of MI-TLIF and 18 cases of posterior lumber fusion (PLF), Starkweather et al.22 reported that after a 6-week follow-up visit, the Interleukin-6 levels were also significantly higher in the MI-TLIF group than in those patients who had undergone PLF, which may be an indicator of ongoing nerve regeneration and healing. Serological analysis may be used to evaluate an immediate postoperative muscular injury21. However, as time passes after the injury, metabolic equilibrium is formed where the figures are normalized making a long term observation difficult. Another study measured the degree of back muscle degeneration using MRI12,23,24. MRI is not only capable of measuring the muscle mass9 but can also calculate the fat content of the skeletal muscles10,11 thus enabling measurements of the degree of fat infiltration before and after surgery. After surgery using the traditional and minimally invasive approaches in 4 cases each, and carrying out a follow up evaluation of the extent of damage and edema in the multifidus muscle using MRI, Stevens et al.18 reported a remarkable decrease in edema of the multifidus muscle but no significant difference in muscle contraction.
In this experiment study, in 48 cases in whom conventional open surgery and MI-TLIF had been performed, a quantitative analysis of the degenerative changes in the back muscle after 1 year revealed that MI-TLIF is effective in diminishing the changes in the percentile value of fat infiltration of the back muscle and the proportion of crosssectional area compared to the conventional open surgery. In particular, in a group where a multi-segment fusion had been performed, the difference in the surgical approach was clear as compared to the group where a single segment fusion had been performed. However, the difference was not significant. In addition to the direct intraoperative injury to the back muscle, factors, such as the postoperative bed rest, period of brace use and degree of activity, should also affect the degenerative changes in the back muscle25,26. In addition, from a long-term perspective, postoperative management might play a role as the key parameter for the degeneration of the back muscle.
A radiologic evaluation has limitations in accurately reflecting the actual clinical status. Therefore, further study will be needed to analyze the clinical assessment specifications and muscle activity. In this study, it could not be demonstrated whether the degree of back muscle degeneration reached statistical significance in both groups. Follow-up studies are warranted because of the possibility that this might have originated from a type II error (βerror)27 due to the small sample size.
Conclusions
The MI-TLIF is a method that minimizes damage to the soft tissue, regional muscles and blood loss immediately after surgery. However, after a period of more than 1 year, there was no significant difference in the paraspinal degenerative changes between the two techniques.
References
- 1.Suwa H, Hanakita J, Ohshita N, et al. Postoperative changes in paraspinal muscle thickness after various lumbar back surgery procedures. Neurol Med Chir (Tokyo) 2000;40:151–154. doi: 10.2176/nmc.40.151. [DOI] [PubMed] [Google Scholar]
- 2.Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical technique. A prospective multicenter randomized study from the Swedish lumbar spine study group. Spine (Phila Pa 1976) 2002;27:1131–1141. doi: 10.1097/00007632-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 3.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 1. Histologic and histochemical analyses in rats. Spine (Phila Pa 1976) 1994;19:2590–2597. doi: 10.1097/00007632-199411001-00017. [DOI] [PubMed] [Google Scholar]
- 4.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 2. Histologic and histochemical analyses in humans. Spine (Phila Pa 1976) 1994;19:2598–2602. doi: 10.1097/00007632-199411001-00018. [DOI] [PubMed] [Google Scholar]
- 5.Kawaguchi Y, Yabuki S, Styf J, et al. Back muscle injury after posterior lumbar spine surgery. Topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine (Phila Pa 1976) 1996;21:2683–2688. doi: 10.1097/00007632-199611150-00019. [DOI] [PubMed] [Google Scholar]
- 6.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28:S26–S35. doi: 10.1097/01.BRS.0000076895.52418.5E. [DOI] [PubMed] [Google Scholar]
- 7.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 8.Kim KT, Lee SH, Suk KS, Bae SC. The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine (Phila Pa 1976) 2006;31:712–716. doi: 10.1097/01.brs.0000202533.05906.ea. [DOI] [PubMed] [Google Scholar]
- 9.Lonn L, Starck G, Alpsten M, Ekholm S, Sjostrom L. Determination of tissue volumes: a comparison between CT and MR imaging. Acta Radiol. 1999;40:314–321. doi: 10.3109/02841859909175560. [DOI] [PubMed] [Google Scholar]
- 10.Mitsiopoulos N, Baumgartner RN, Heymsfield SB, et al. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol. 1998;85:115–122. doi: 10.1152/jappl.1998.85.1.115. [DOI] [PubMed] [Google Scholar]
- 11.Phoenix J, Betal D, Roberts N, Helliwell TR, Edwards RH. Objective quantification of muscle and fat in human dystrophic muscle by magnetic resonance image analysis. Muscle Nerve. 1996;19:302–310. doi: 10.1002/(SICI)1097-4598(199603)19:3<302::AID-MUS4>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 12.Lee JC, Cha JG, Kim Y, Kim YI, Shin BJ. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: comparison with the normal controls. Spine (Phila Pa 1976) 2008;33:318–325. doi: 10.1097/BRS.0b013e318162458f. [DOI] [PubMed] [Google Scholar]
- 13.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 14.Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine (Phila Pa 1976) 1999;24:1023–1028. doi: 10.1097/00007632-199905150-00017. [DOI] [PubMed] [Google Scholar]
- 15.Styf JR, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine (Phila Pa 1976) 1998;23:354–358. doi: 10.1097/00007632-199802010-00014. [DOI] [PubMed] [Google Scholar]
- 16.Datta G, Gnanalingham KK, Peterson D, et al. Back pain and disability after lumbar laminectomy: Is there a relationship to muscle retraction? Neurosurgery. 2004;54:1413–1420. doi: 10.1227/01.neu.0000124751.57121.a6. [DOI] [PubMed] [Google Scholar]
- 17.Taylor H, McGregor AH, Medhi-Zadeh S, et al. The impact of self-retaining retractors on the paraspinal muscles during posterior spinal surgery. Spine (Phila Pa 1976) 2002;27:2758–2762. doi: 10.1097/00007632-200212150-00004. [DOI] [PubMed] [Google Scholar]
- 18.Stevens KJ, Spenciner DB, Griffiths KL, et al. Comparison of minimally invasive and conventional open posterolateral lumbar fusion using magnetic resonance imaging and retraction pressure studies. J Spinal Disord Tech. 2006;19:77–86. doi: 10.1097/01.bsd.0000193820.42522.d9. [DOI] [PubMed] [Google Scholar]
- 19.Hyun SJ, Kim YB, Kim YS, et al. Postoperative changes in paraspinal muscle volume: comparison between paramedian interfascial and midline approaches for lumbar fusion. J Korean Med Sci. 2007;22:646–651. doi: 10.3346/jkms.2007.22.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bates D, Ruggieri P. Imaging modalities for evaluation of the spine. Radiol Clin North Am. 1991;29:675–690. [PubMed] [Google Scholar]
- 21.Kim K, Isu T, Sugawara A, Matsumoto R, Isobe M. Comparison of the effect of 3 different approaches to the lumbar spinal canal on postoperative paraspinal muscle damage. Surg Neurol. 2008;69:109–113. doi: 10.1016/j.surneu.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 22.Starkweather AR, Witek-Janusek L, Nockels RP, Peterson J, Mathews HL. The multiple benefits of minimally invasive spinal surgery: results comparing transforaminal lumbar interbody fusion and posterior lumbar fusion. J Neurosci Nurs. 2008;40:32–39. [PMC free article] [PubMed] [Google Scholar]
- 23.Kjaer P, Bendix T, Sorensen JS, Korsholm L, Leboeuf-Yde C. Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med. 2007;5:2. doi: 10.1186/1741-7015-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ranson CA, Burnett AF, Kerslake R, Batt ME, O'Sullivan PB. An investigation into the use of MR imaging to determine the functional cross sectional area of lumbar paraspinal muscles. Eur Spine J. 2006;15:764–773. doi: 10.1007/s00586-005-0909-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Motosuneya T, Asazuma T, Tsuji T, et al. Postoperative change of the cross-sectional area of back musculature after 5 surgical procedures as assessed by magnetic resonance imaging. J Spinal Disord Tech. 2006;19:318–322. doi: 10.1097/01.bsd.0000211205.15997.06. [DOI] [PubMed] [Google Scholar]
- 26.Hides JA, Belavy DL, Stanton W, et al. Magnetic resonance imaging assessment of trunk muscles during prolonged bed rest. Spine (Phila Pa 1976) 2007;32:1687–1692. doi: 10.1097/BRS.0b013e318074c386. [DOI] [PubMed] [Google Scholar]
- 27.Lochner HV, Bhandari M, Tornetta P., 3rd Type-II error rates (beta errors) of randomized trials in orthopaedic trauma. J Bone Joint Surg Am. 2001;83:1650–1655. doi: 10.2106/00004623-200111000-00005. [DOI] [PubMed] [Google Scholar]