Abstract
Background and purpose The optimal treatment for isolated patellofemoral osteoarthritis is unclear at present. We systematically reviewed the highest level of available evidence on the nonoperative and operative treatment of isolated patellofemoral osteoarthritis to develop an evidenced-based discussion of treatment options.
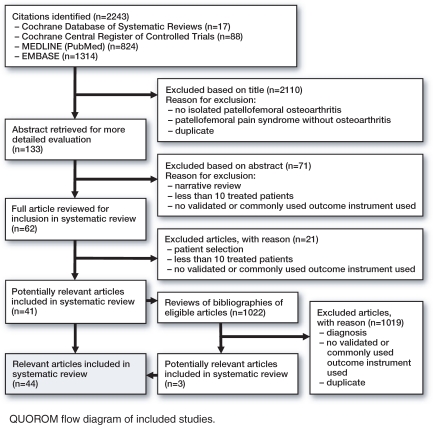
Methods A systematic computerized database search (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, MEDLINE (PubMed), and EMBASE) was performed in March 2009. The quality of the studies was assessed independently by two authors using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.
Results We extracted data from 44 articles. The best available evidence for treatment of isolated patellofemoral osteoarthritis is sparse and of generally low methodological quality. Nonoperative treatment using physiotherapy (GRADE: high quality, weak recommendation for use), taping (GRADE: moderate quality, weak recommendation for use), or injection therapy (GRADE: very low quality, weak recommendation for use) may result in short-term relief. Joint-preserving surgical treatment may result in insufficient, unpredictable, or only short-term improvement (GRADE: low quality, weak recommendation against use). Total knee replacement with patellar resurfacing results in predictable and good, durable results (GRADE: low quality, weak recommendation for use). Outcome after patellofemoral arthroplasty in selected patients is good to excellent (GRADE: low quality, weak recommendation for use).
Interpretation Methodologically good quality comparative studies, preferably using a patient-relevant outcome instrument, are needed to establish the optimal treatment strategy for patients with isolated patellofemoral osteoarthritis.
Introduction
A multitude of nonoperative and operative treatment options have been described for isolated patellofemoral osteoarthritis in the literature, but the optimal treatment is unclear at present. To develop an evidenced-based discussion of treatment options in isolated patellofemoral osteoarthritis, we reviewed the highest level of available evidence on the nonoperative and operative treatment of isolated patellofemoral osteoarthritis.
Materials and methods
With use of the evidence-based cycle, we formulated 3 focused clinical questions with well-articulated Patient/Population (P), Intervention (I), Comparison (C), and Outcome (O) (PICO) elements (Poolman et al. 2007a). The questions were as follows. (1) In patients with isolated patellofemoral osteoarthritis (P), is physical therapy (I) better than no physical therapy (C) when assessed with a validated outcome measure (O)? (2) In patients with isolated patellofemoral osteoarthritis (P), is operative treatment (I) better than nonoperative treatment (C) when assessed with a validated outcome measure (O)? (3) In patients with isolated patellofemoral osteoarthritis (P), is patellofemoral arthroplasty (I) better than other operative treatment options (C) when assessed with a validated outcome measure (O)?
Criteria for eligibility
We searched for studies that fulfilled certain inclusion criteria. Publications in the English, French, Dutch, or German language that describe the clinical outcome of nonoperative or operative treatments for isolated patellofemoral osteoarthritis in 10 or more patients were included. Publications reporting the results of treatment of patellofemoral pain syndrome without osteoarthritis were excluded, as were studies with incompletely described patient populations, insufficient descriptions of treatment, and studies lacking the use of validated or commonly used outcome measures.
Study identification
Using the following search terms with Boolean operators ([femoropatell* OR femoro-patell* OR patell*] AND [osteoarthritis OR arthritis OR arthrosis]), we conducted the following searches:
Computerized database searches of: (a) the Cochrane Database of Systematic Reviews (2009, Issue 1); (b) the Cochrane Central Register of Controlled Trials (2009, Issue 1); (c) MEDLINE (PubMed) (1966 to 6 March 2009) using the “clinical queries” feature with a “broad search” for “therapy”; (d) EMBASE (1966 to 7 March 2009) using a search strategy with “Include sub-terms/derivatives” and “Record limits: Humans”.
Reviews of the bibliographies of eligible articles.
The systematic search was performed in March 2009 with adherence to the QUOROM statement and the MOOSE guidelines (Moher et al. 1999, Stroup et al. 2000). The search was performed in duplicate by one of the authors (HPWvJ) and a librarian. Authors of eligible studies were not contacted with regard to possible unpublished results.
Evaluation of methodological quality
The quality of the studies included was assessed independently by two authors (HPWvJ, RWP) using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (www.gradeworkinggroup.org) (Atkins et al. 2004, Petrisor et al. 2006, Guyatt et al. 2008). Apart from describing the methodological quality of the studies (high, moderate, low, and very low), a strong or weak recommendation was given for or against the use of an intervention. A strong recommendation for using an intervention was given when the benefits clearly outweighed the risks for most if not all patients, with high-quality evidence supporting that recommendation. However, a strong recommendation against use may also be supported by studies of low-grade quality, such as case series that show serious adverse effects of the intervention (Poolman et al. 2007b). A weak recommendation for or against use of an intervention was given where the risks and benefits were more closely balanced or were more uncertain because of the low methodological quality of the supporting studies.
Data abstraction
Relevant data regarding study design, study population, intervention, and outcome measures were extracted from the text, figures, and tables of the articles included.
Results
44 studies, all of which were published as full journal articles, met the eligibility criteria and were included in this review (Figure and Table).
QUOROM flow diagram of included studies.
GRADE evidence profile: nonoperative and operative treatment for isolated patellofemoral osteoarthritis
| Quality assessment |
Summary of findings |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | K | L |
| A. Number of studies | |||||||||||
| B. Design | |||||||||||
| RT: Randomized trial | |||||||||||
| RC: Randomized crossover trial | |||||||||||
| O: Observational | |||||||||||
| MO: Matched case control, observational | |||||||||||
| SO: Systematic review, observational | |||||||||||
| C. Limitations | |||||||||||
| No: No serious limitations | |||||||||||
| Yes: Serious | |||||||||||
| b patients not blinded, short follow-up. | |||||||||||
| c pilot study, important heterogeneity in diagnosis. | |||||||||||
| D. Inconsistency | |||||||||||
| No: No serious inconsistency | |||||||||||
| Yes: Only one study | |||||||||||
| E. Indirectness | |||||||||||
| No: No serious indirectness | |||||||||||
| S: Some uncertainty about directness (-1), not specifically limited to isolated patellofemoral osteoarthritis. | |||||||||||
| F. Imprecision | |||||||||||
| No: No serious imprecision | |||||||||||
| G. Publication bias | |||||||||||
| U: Undetected | |||||||||||
| H. Number of treated patients | |||||||||||
| I. Number of controls | |||||||||||
| J. Absolute effect and 95% confidence interval. KSPS: Knee Specific Pain Score. | |||||||||||
| K. Quality | |||||||||||
| H: High | |||||||||||
| M: Moderate | |||||||||||
| L: Low | |||||||||||
| VL: Very low | |||||||||||
| L. Recommendation | |||||||||||
| (+): Weak for | |||||||||||
| (–): Weak against | |||||||||||
| –: Strong against | |||||||||||
| Nonoperative treatment: Physiotherapy versus no physiotherapy | |||||||||||
| 1 | RT | No | Yes | No | No | U | 40 | 43 | Knee pain at 5 months (–6.4 mm; 95% CI –15.3 to 2.4; p = 0.16) Increased quadriceps strength at 5 months (+11.7 Nm; 95% CI 4.5 to 19.0; p = 0.002) WOMAC at 5 months (-0.6; 95% CI -3.7 to 2.4; p = 0.68) |
H | (+) |
| Nonoperative treatment: Taping | |||||||||||
| 1 | RC | Yes (-1) b | Yes | No | No | U | 14 | (14) | Neutral vs. medial taping: knee pain at 4 days (15.5 mm; 95% CI 2.4 to 28.6; p = 0.023) Neutral vs. lateral taping: knee pain at 4 days (-8.0 mm; 95%CI -22.5 to 6.5, p = 0.26) |
M | (+) |
| Nonoperative treatment: Intra-articular injection | |||||||||||
| 1 | O | Yes (-1) c | Yes | No | No | U | 25 | – | VL | (+) | |
| Operative treatment: Arthroscopy | |||||||||||
| 2 | RT | No | No | S (-1) | No | U | 196 | 135 | KSPS at 24 months (placebo 51.6±23.7; lavage 53.7±23,7; debridement 51.4±23.2; p = 0.64 and p = 0.96) WOMAC at 24 months (-23±605; 95% CI -208 to 161; p = 0.22) |
M | – |
| Operative treatment: Chondroplasty, resection arthroplasty, and lateral facetectomy | |||||||||||
| 5 | O | No | No | No | No | U | 155 | – | L | (+) | |
| Operative treatment: Extensor mechanism alignment and lateral release | |||||||||||
| 7 | O | No | No | No | No | U | 224 | – | L | (–) | |
| Operative treatment: Patellectomy | |||||||||||
| 0 | |||||||||||
| Operative treatment: Total knee arthroplasty | |||||||||||
| 6 | MO | No | No | No | No | U | 271 | – | L | (+) | |
| Operative treatment: Patellofemoral arthroplasty | |||||||||||
| 24 | SO | No | No | No | No | U | 2,938 | – | L | (+) | |
Results relating to the 3 focused, patient-oriented clinical questions developed using PICO were as follows. 1 randomized controlled trial described the short-term outcome of physical therapy compared with no physical therapy (Quilty et al. 2003). We were unable to identify studies that directly compared the results of operative and nonoperative treatments. Also, no comparative studies were retrieved that directly compared the results of patellofemoral arthroplasty with the results of other operative treatment options.
Due to the heterogeneity of the study designs and outcome measures, a meta-analysis was not performed. The following review of the literature is therefore descriptive.
Highest available evidence
- Nonoperative treatment:
- Physical therapy vs. no physical therapy: 1 randomized controlled trial (83 patients) (Quilty et al. 2003)
- Taping: 1 randomized crossover trial (14 patients) (Cushnaghan et al. 1994)
- Intra-articular injection: 1 prospective case series (25 patients) (Clarke et al. 2005)
- Nonoperative vs. operative treatment:
- No comparative studies identified.
- Operative treatment:
- Arthroscopy: 2 randomized controlled trials (165 and 168 patients) were included based on indirect evidence (Moseley et al. 2002, Kirkley et al. 2008)
- Chondroplasty, resection-arthroplasty, and lateral facetectomy: 1 prospective case series (50 patients) (Becker et al. 2008) and 4 retrospective case series (11–63 patients) (Beltran 1987, Yercan et al. 2005, Spak and Teitge 2006, Paulos et al. 2008)
- Extensor mechanism alignment and lateral release: 2 prospective case series (35 and 50 patients) (Alemdaroglu et al. 2008, Becker et al. 2008), 2 retrospective comparative studies (12 and 48 patients) (Weaver et al. 1991, Jacquot et al. 2004), and 3 retrospective case series (14–50 patients) (Aderinto and Cobb 2002, Kohn et al. 2004, Carofino and Fulkerson 2008)
- Patellectomy: no studies met the inclusion criteria
- Total knee arthroplasty: 2 matched case-control studies (94 and 54 patients) of total knee arthroplasty for isolated patellofemoral osteoarthritis compared with total knee arthroplasty for tri-compartmental osteoarthritis (Laskin and Van Steijn 1999, Meding et al. 2007), 1 prospective case series (24 patients) (Parvizi et al. 2001), and 3 retrospective case series (25–47 patients) (Mont et al. 2002, Dejour et al. 2004, Dalury 2005)
- Patellofemoral arthroplasty: 3 systematic reviews of case series (538–812 patients) (Leadbetter et al. 2005, 2006, Becher et al. 2008), 5 prospective case series (15–240 patients) (Arnbjornsson and Ryd 1998, Tauro et al. 2001, Merchant 2004, Ackroyd and Chir 2005, Ackroyd et al. 2007), and 16 retrospective case series (12–65 patients) (Arciero and Toomey 1988, Cartier et al. 1990, Argenson et al. 1995, Krajca-Radcliffe and Coker 1996, Mertl et al. 1997, De Cloedt et al. 1999, Fink et al. 1999, de Winter et al. 2001, Smith et al. 2002, Kooijman et al. 2003, Board et al. 2004, Argenson et al. 2005, Cartier et al. 2005, Merchant 2005, Sisto and Sarin 2006, Gadeyne et al. 2008).
The available evidence together with background information from systematic reviews and other relevant sources was used for the following discussion of treatment options.
Nonoperative treatment options
Physiotherapy.
Initially, patients with isolated patellofemoral osteoarthritis can be treated using a nonoperative approach such as activity modification, weight loss, and physiotherapy. 1 randomized controlled trial described the short-term outcome of a commonly used physiotherapy package (patellar taping, functional exercises, education, quadriceps strengthening exercises, postural advice, and education) compared with no physical therapy (Quilty et al. 2003). The physiotherapy intervention was delivered by a single physiotherapist in nine 30-minute sessions over 10 weeks, with advice to continue thereafter. The treatment group had a small reduction in pain and a substantial increase in the quadriceps strength of the index knee 10 weeks after treatment compared with the no-treatment group. After 12 months, no differences in patient-relevant outcome measures were noted between groups (Quilty et al. 2003). According to GRADE, the quality of this evidence is high, with a weak recommendation for use of the intervention.
Taping.
A randomized crossover trial using visual analog scale ratings for pain demonstrated a 25% reduction in knee pain when the patella was taped medially. However, each tape (medial, lateral, or neutral) was applied for only 4 days, with 3 days of no treatment between tape positions (Cushnaghan et al. 1994). According to GRADE, the quality of the evidence is moderate, with a weak recommendation for use of this intervention.
Intra-articular injections/visco-supplementation
The clinical effect of intra-articular visco-supplementation with hylan G-F 20 (Synvisc; Genzyme Corporation, Cambridge, MA) was assessed in a non-randomized clinical trial with use of a patient-relevant outcome instrument. Pain upon stair climbing improved 4 weeks after the initial injection and the improvement was maintained to 26 and 52 weeks (Clarke et al. 2005). According to GRADE, the evidence is of very low quality, with a weak recommendation for use of this intervention.
Operative treatment options
Arthroscopy.
We did not identify any studies describing the results of arthroscopic debridement of articular cartilage for patients with isolated patellofemoral osteoarthritis. However, we did include 2 methodologically sound randomized controlled trials, although they describe the results of arthroscopy in osteoarthritis of the knee, and were not specifically limited to isolated patellofemoral osteoarthritis (Moseley et al. 2002, Kirkley et al. 2008). No differences in outcome were found between surgical placebo treatment and arthroscopy, and between arthroscopy combined with physiotherapy as opposed to nonoperative treatment with physiotherapy only. Although these papers do not strictly describe the results of arthroscopic treatment for isolated patellofemoral osteoarthritis, indirect evidence is given. Based on these high-quality studies, arthroscopy is not recommended for osteoarthritis of the knee. In the case of indirect evidence, the GRADE group advises reducing the level of quality from high to moderate (Guyatt et al. 2008), with a strong recommendation against the use of this intervention.
Chondroplasty, resection-arthroplasty, and lateral facetectomy.
A retrospective case series in patients younger than 55 years of age showed that the use of fresh osteochondral allografts for patellofemoral arthritis resulted in relief of the arthritic condition, improved knee function, and delayed prosthetic knee replacement (Spak and Teitge 2006). A retrospective case series describing the results of en bloc removal of articular cartilage and subchondral bone showed that 20 of the 33 operated knees were pain-free after an average of 31-months of follow-up (Beltran 1987). Partial lateral facetectomy results in short-term improvement in pain scores with no or moderate improvement in function, as assessed with a patient-relevant outcome instrument (Yercan et al. 2005, Becker et al. 2008, Paulos et al. 2008). According to GRADE, the evidence is of low quality, with a weak recommendation for use of these interventions.
Extensor mechanism alignment and lateral release.
Anterior displacement of the tibial tuberosity reduces the contact forces, but not necessarily the stress on the patellofemoral joint (Lewallen et al. 1990). Anteromedialization, which translates the contact area medially, results in relief of the lateral facet which could theoretically reduce pain. Retrospective case series evaluating the 2- to 6-year results of anteromedial transfer of the tibial tuberosity combined with lateral retinacular release have demonstrated an improvement in outcome measures with reduced pain (Weaver et al. 1991, Kohn et al. 2004, Carofino and Fulkerson 2008). Total loss of cartilage or absence of lateralization are contraindications to the Fulkerson procedure (Steimer and Kohn 2007). Compared with medialization with vastus medialis obliquus shortening, anterior displacement and lateral facetectomy both result in improved knee function (Jacquot et al. 2004). However, the number of complications associated with the Maquet anterior displacement is high (Kadambande et al. 2004). Combined partial lateral facetectomy, lateral release, and medialization of the tibial tubercle result in incomplete improvement of symptoms as assessed with a patient-relevant outcome instrument (Becker et al. 2008). In a large number of patients, isolated arthroscopic lateral retinacular release results in reduction of pain rather than resolution (Aderinto and Cobb 2002, Alemdaroglu et al. 2008). In evaluating the results, a patient-relevant outcome instrument was used. According to GRADE, the evidence is of low quality, with a weak recommendation against use of these interventions.
Total knee arthroplasty.
Total knee replacement with patellar resurfacing gives satisfactory 5- to 7-year results in patients with isolated patellofemoral osteoarthritis (Laskin and Van Steijn 1999, Parvizi et al. 2001, Mont et al. 2002, Dejour et al. 2004, Dalury 2005, Meding et al. 2007). These results are similar to those achieved after total knee arthroplasty with patellar resurfacing for femorotibial osteoarthritis (Laskin and Van Steijn 1999, Meding et al. 2007). However, up to one-fifth of patients have reported anterior knee pain after total knee replacement (Laskin and Van Steijn 1999, Parvizi et al. 2001, Mont et al. 2002, Meding et al. 2007). As with total knee arthroplasty for tricompartmental osteoarthritis, it remains unclear whether patellar resurfacing results in better outcomes in isolated patellofemoral osteoarthritis (Thompson et al. 2001). Because of its relationship with patellofemoral instability, total knee arthroplasty in patients with isolated patellofemoral osteoarthritis is a technically more demanding procedure (Laskin and Van Steijn 1999, Parvizi et al. 2001, Mont et al. 2002, Saleh et al. 2005). According to GRADE, the evidence is of low quality, with a weak recommendation for use of this intervention.
Patellofemoral arthroplasty.
In patellofemoral arthroplasty, the femorotibial compartments with cruciate ligaments and menisci are spared, which probably allows preservation of physiological femorotibial joint mechanics. The clinical results reported are related to prosthetic design, surgical technique, patient selection and indication, and length of follow-up, and have shown good to excellent 3- to 17-year results in two-thirds of patients to all of them (Arciero and Toomey 1988, Cartier et al. 1990, Argenson et al. 1995, Krajca-Radcliffe and Coker 1996, Mertl et al. 1997, Arnbjornsson and Ryd 1998, de Winter et al. 2001, Smith et al. 2002, Kooijman et al. 2003, Merchant 2004, 2005, Ackroyd and Chir 2005, Cartier et al. 2005, Sisto and Sarin 2006, Ackroyd et al. 2007, Gadeyne et al. 2008). Progression of femorotibial osteoarthritis, malposition of the prosthesis, and wear or loosening may result in failure of the patellofemoral arthroplasty (Leadbetter et al. 2005). Development of painful femorotibial osteoarthritis is the most important non-prosthetic-related reason for conversion to total knee arthroplasty. Conversion rates of 1 in 5 have been reported after an average of 7 to 16 years (Kooijman et al. 2003, Argenson et al. 2005). It remains unclear which patients are at risk of developing femorotibial osteoarthritis (Leadbetter et al. 2005). Recently, the results of revision to total knee arthroplasty for progression of femorotibial osteoarthritis or malposition was described (Lonner et al. 2006). Clinical outcome as assessed by the Knee Society score (KSS) improved after revision. Patellofemoral arthroplasty does not have a negative effect on the outcome of later total knee arthroplasty (van Jonbergen et al. 2009). According to GRADE, the evidence is of low quality, with a weak recommendation for use of this intervention.
Discussion
Several nonoperative and operative treatment options for isolated patellofemoral osteoarthritis have been described. At present, there are no publications describing the outcome of nonoperative treatment after 1 year. A multitude of studies of generally low methodological quality have reported the short- and long-term results of surgical management. Despite these limitations, we present the following treatment recommendations based on the best available evidence.
Nonoperative treatment using physical therapy (GRADE: high quality, weak recommendation for use), taping (GRADE: moderate quality, weak recommendation for use), or injection therapy (GRADE: very low quality, weak recommendation for use) may result in short-term relief. Joint-preserving surgical treatment may result in insufficient, unpredictable, or only short-term improvement (GRADE: low quality, weak recommendation against use). Total knee replacement with patellar resurfacing results in predictable and durable good results (GRADE: low quality, weak recommendation for use). However, for a degenerative disease involving only one compartment, it is probably too aggressive. Outcome after patellofemoral arthroplasty in selected patients is good to excellent (GRADE: low quality, weak recommendation for use). Total knee replacement can be performed later if painful femorotibial osteoarthritis develops.
Strengths and limitations of this review
Our study is the first systematic review to use both well-articulated patient-oriented clinical questions (PICO) and an evaluation using the GRADE approach in order to obtain an evidenced-based discussion of nonoperative and operative treatment options in isolated patellofemoral osteoarthritis. However, our study has some limitations that should be considered. First, there is always the possibility that we failed to identify some studies, although a comprehensive search strategy was used including visually searching the reference lists of all eligible articles. Secondly, our aim was to evaluate the best evidence on the treatment of patellofemoral osteoarthritis, and therefore we did not include chondromalacia in our search strategy. Because there is currently no consensus on the diagnostic criteria of patellofemoral osteoarthritis, it is possible that we included studies with important heterogeneity among the degree of osteoarthritis and clinical complaints.
Limitations of primary research
This systematic review shows that the current best available evidence for treatment of isolated patellofemoral osteoarthritis is sparse and generally of low methodological quality. The lack of randomized, controlled studies may result in substantial selection bias. Also, comparison of the results of different treatments is hampered by the extensive heterogeneity among the outcome instruments used. Only 4 of the 44 studies included employed a patient-relevant outcome instrument such as the WOMAC osteoarthritis index in evaluating the results of treatment (Quilty et al. 2003, Clarke et al. 2005, Alemdaroglu et al. 2008, Becker et al. 2008).
Implications for future research
Methodologically good-quality studies, preferably evaluating results with a validated patient-relevant outcome measure such as the KOOS or WOMAC (Paxton and Fithian 2005), are needed to establish the optimal treatment strategy for patients with isolated patellofemoral osteoarthritis. Ideally, such studies should compare the results of commonly advocated methods of nonoperative and operative treatments.
Conclusion
The results of this systematic review show that the best available evidence for nonoperative and operative treatment options for patients with isolated patellofemoral osteoarthritis is sparse and of low methodological quality. Presently, there is no convincing evidence that one specific treatment modality is superior to another in terms of better outcomes.
Acknowledgments
HPvJ and AvK initiated the study. HPvJ and RWP collected and analyzed the data. HPvJ wrote the manuscript under the supervision of RWP and AvK.
No competing interests declared.
References
- 1.Ackroyd CE, Chir B. Development and early results of a new patellofemoral arthroplasty. Clin Orthop. 2005;((436)):7–13. doi: 10.1097/01.blo.0000171914.94503.d1. [DOI] [PubMed] [Google Scholar]
- 2.Ackroyd CE, Newman JH, Evans R, Eldridge JD, Joslin CC. The Avon patellofemoral arthroplasty: Five-year survivorship and functional results. J Bone Joint Surg (Br) 2007;89((3)):310–5. doi: 10.1302/0301-620X.89B3.18062. [DOI] [PubMed] [Google Scholar]
- 3.Aderinto J, Cobb AG. Lateral release for patellofemoral arthritis. Arthroscopy. 2002;18((4)):399–403. doi: 10.1053/jars.2002.32306. [DOI] [PubMed] [Google Scholar]
- 4.Alemdaroglu KB, Cimen O, Aydogan NH, Atlihan D, Iltar S. Early results of arthroscopic lateral retinacular release in patellofemoral osteoarthritis. Knee. 2008;15((6)):451–5. doi: 10.1016/j.knee.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Arciero RA, Toomey HE. Patellofemoral arthroplasty. A three- to nine-year follow-up study. Clin Orthop. 1988;((236)):60–71. [PubMed] [Google Scholar]
- 6.Argenson JN, Guillaume JM, Aubaniac JM. Is there a place for patellofemoral arthroplasty? Clin Orthop. 1995;((321)):162–7. [PubMed] [Google Scholar]
- 7.Argenson JN, Flecher X, Parratte S, Aubaniac JM. Patellofemoral arthroplasty: an update. Clin Orthop. 2005;((440)):50–3. doi: 10.1097/01.blo.0000187061.27573.70. [DOI] [PubMed] [Google Scholar]
- 8.Arnbjornsson AH, Ryd L. The use of isolated patellar prostheses in Sweden 1977-1986. Int Orthop. 1998;22((3)):141–4. doi: 10.1007/s002640050227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O'Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer TT, Varonen H, Vist GE, Williams JW, Jr., Zaza S. Grading quality of evidence and strength of recommendations. BMJ. 2004;328((7454)):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becher C, Renke A, Heyse TJ, Schofer M, Tibesku CO, Fuchs-Winkelmann S. Patellofemorale Endoprothetik in Deutschland - eine Standortbestimmung und Überblick Über die Literatur. Z Orthop Unfall. 2008;146((6)):773–81. doi: 10.1055/s-2008-1039000. [DOI] [PubMed] [Google Scholar]
- 11.Becker R, Ropke M, Krull A, Musahl V, Nebelung W. Surgical treatment of isolated patellofemoral osteoarthritis. Clin Orthop. 2008;((466)):443–9. doi: 10.1007/s11999-007-0071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beltran JE. Resection arthroplasty of the patella. J Bone Joint Surg (Br) 1987;69((4)):604–7. doi: 10.1302/0301-620X.69B4.3611166. [DOI] [PubMed] [Google Scholar]
- 13.Board TN, Mahmood A, Ryan WG, Banks AJ. The Lubinus patellofemoral arthroplasty: a series of 17 cases. Arch Orthop Trauma Surg. 2004;124((5)):285–7. doi: 10.1007/s00402-004-0645-x. [DOI] [PubMed] [Google Scholar]
- 14.Carofino BC, Fulkerson JP. Anteromedialization of the tibial tubercle for patellofemoral arthritis in patients > 50 years. J Knee Surg. 2008;21((2)):101–5. doi: 10.1055/s-0030-1247803. [DOI] [PubMed] [Google Scholar]
- 15.Cartier P, Sanouiller JL, Grelsamer R. Patellofemoral arthroplasty. 2-12-year follow-up study. J Arthroplasty. 1990;5((1)):49–55. doi: 10.1016/s0883-5403(06)80009-4. [DOI] [PubMed] [Google Scholar]
- 16.Cartier P, Sanouiller JL, Khefacha A. Long-term results with the first patellofemoral prosthesis. Clin Orthop. 2005;((436)):47–54. doi: 10.1097/01.blo.0000171918.24998.d1. [DOI] [PubMed] [Google Scholar]
- 17.Clarke S, Lock V, Duddy J, Sharif M, Newman JH, Kirwan JR. Intra-articular hylan G-F 20 (Synvisc) in the management of patellofemoral osteoarthritis of the knee (POAK) Knee. 2005;12((1)):57–62. doi: 10.1016/j.knee.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Cushnaghan J, McCarthy C, Dieppe P. Taping the patella medially: a new treatment for osteoarthritis of the knee joint? BMJ. 1994;308((6931)):753–5. doi: 10.1136/bmj.308.6931.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalury DF. Total knee replacement for patellofemoral disease. J Knee Surg. 2005;18((4)):274–7. doi: 10.1055/s-0030-1248191. [DOI] [PubMed] [Google Scholar]
- 20.De Cloedt P, Legaye J, Lokietek W. Les prothèses fémoro-patellaires: étude rétrospective de 45 cas successifs avec un recul de 3 à 12 ans. Acta Orthopaedica Belgica. 1999;65((2)):170–5. [PubMed] [Google Scholar]
- 21.Dejour D, Barbosa J, Jacquot N, Neyret P. Résultats des prothèses totales du genou dans l´arthrose fémoro-patellaire isolée. Rev Chir Orthop (Suppl. 5) 2004;90:1S111–3. [Google Scholar]
- 22.de Winter WE, Feith R, van Loon CJ. The Richards type II patellofemoral arthroplasty: 26 cases followed for 1-20 years. Acta Orthop Scand. 2001;72((5)):487–90. doi: 10.1080/000164701753532826. [DOI] [PubMed] [Google Scholar]
- 23.Fink B, Schneider T, Tillmann K, Ruther W. Die Femoropatellarendoprothese—in der heutigen Zeit sinnvoll? Z Orthop. 1999;137((3)):247–52. doi: 10.1055/s-2008-1037402. [DOI] [PubMed] [Google Scholar]
- 24.Gadeyne S, Besse JL, Galand-Desme S, Lerat JL, Moyen B. Résultats de la prothèse fémoropatellaire autocentrique: à propos d'une série continue de 57 prothèses. Rev Chir Orthop. 2008;94((3)):228–40. doi: 10.1016/j.rco.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 25.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336((7651)):995–8. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacquot N, Barbosa J, Dejour D, Neyret P. Résultats du traitement conservateur chirurgical dans l'arthrose fémoro- patellaire isolée. Rev Chir Orthop (Suppl. 5) 2004;90:1S97–9. [Google Scholar]
- 27.Kadambande SS, Auyeung J, Ghandour A, Mintowt-Czyz W. A review of wound healing following Maquet osteotomy. Knee. 2004;11((6)):463–7. doi: 10.1016/j.knee.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 28.Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, Feagan BG, Donner A, Griffin SH, D'Ascanio LM, Pope JE, Fowler PJ. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359((11)):1097–107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 29.Kohn D, Steimer O, Seil R. Der Anteromedialisierung der Tuberositas tibiae. Orthopäde. 2004;33((2)):218–23. doi: 10.1007/s00132-003-0592-1. [DOI] [PubMed] [Google Scholar]
- 30.Kooijman HJ, Driessen AP, van Horn JR. Long-term results of patellofemoral arthroplasty. A report of 56 arthroplasties with 17 years of follow-up. J Bone Joint Surg (Br) 2003;85((6)):836–40. [PubMed] [Google Scholar]
- 31.Krajca-Radcliffe JB, Coker TP. Patellofemoral arthroplasty. A 2- to 18-year followup study. Clin Orthop. 1996;((330)):143–51. [PubMed] [Google Scholar]
- 32.Laskin RS, Van Steijn M. Total knee replacement for patients with patellofemoral arthritis. Clin Orthop. 1999;((367)):89–95. [PubMed] [Google Scholar]
- 33.Leadbetter WB, Ragland PS, Mont MA. The appropriate use of patellofemoral arthroplasty: an analysis of reported indications, contraindications, and failures. Clin Orthop. 2005;((436)):91–9. [PubMed] [Google Scholar]
- 34.Leadbetter WB, Seyler TM, Ragland PS, Mont MA. Indications, contraindications, and pitfalls of patellofemoral arthroplasty. J Bone Joint Surg (Am) (Suppl 4) 2006;88:122–37. doi: 10.2106/JBJS.F.00856. [DOI] [PubMed] [Google Scholar]
- 35.Lewallen DG, Riegger CL, Myers ER, Hayes WC. Effects of retinacular release and tibial tubercle elevation in patellofemoral degenerative joint disease. J Orthop Res. 1990;8((6)):856–62. doi: 10.1002/jor.1100080611. [DOI] [PubMed] [Google Scholar]
- 36.Lonner JH, Jasko JG, Booth RE., Jr Revision of a failed patellofemoral arthroplasty to a total knee arthroplasty. J Bone Joint Surg (Am) 2006;88((11)):2337–42. doi: 10.2106/JBJS.F.00282. [DOI] [PubMed] [Google Scholar]
- 37.Meding JB, Wing JT, Keating EM, Ritter MA. Total knee arthroplasty for isolated patellofemoral arthritis in younger patients. Clin Orthop. 2007;((464)):78–82. doi: 10.1097/BLO.0b013e3181576069. [DOI] [PubMed] [Google Scholar]
- 38.Merchant AC. Early results with a total patellofemoral joint replacement arthroplasty prosthesis. J Arthroplasty. 2004;19((7)):829–36. doi: 10.1016/j.arth.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 39.Merchant AC. A modular prosthesis for patellofemoral arthroplasty: design and initial results. Clin Orthop. 2005;((436)):40–6. doi: 10.1097/01.blo.0000171917.47869.6c. [DOI] [PubMed] [Google Scholar]
- 40.Mertl P, Tran Van F, Bonhomme P, Vives P. Traitement de l'arthrose fémoro-patellaire par prothèse sphéro-centrique: Etude rétrospective de 50 implants. Rev Chir Orthop. 1997;83((8)):712–8. [PubMed] [Google Scholar]
- 41.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354((9193)):1896–900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 42.Mont MA, Haas S, Mullick T, Hungerford DS. Total knee arthroplasty for patellofemoral arthritis. J Bone Joint Surg (Am) 2002;84((11)):1977–81. doi: 10.2106/00004623-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 43.Moseley JB, O'Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347((2)):81–8. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 44.Parvizi J, Stuart MJ, Pagnano MW, Hanssen AD. Total knee arthroplasty in patients with isolated patellofemoral arthritis. Clin Orthop. 2001;((392)):147–52. doi: 10.1097/00003086-200111000-00018. [DOI] [PubMed] [Google Scholar]
- 45.Paulos LE, O'Connor DL, Karistinos A. Partial lateral patellar facetectomy for treatment of arthritis due to lateral patellar compression syndrome. Arthroscopy. 2008;24((5)):547–53. doi: 10.1016/j.arthro.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 46.Paxton EW, Fithian DC. Outcome instruments for patellofemoral arthroplasty. Clin Orthop. 2005;((436)):66–70. doi: 10.1097/01.blo.0000171544.38095.77. [DOI] [PubMed] [Google Scholar]
- 47.Petrisor BA, Keating J, Schemitsch E. Grading the evidence: levels of evidence and grades of recommendation. Injury. 2006;37((4)):321–7. doi: 10.1016/j.injury.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 48.Poolman RW, Kerkhoffs GM, Struijs PA, Bhandari M, International Evidence-Based Orthopedic Surgery Working Group Don't be misled by the orthopedic literature: tips for critical appraisal. Acta Orthop. 2007a;78((2)):162–71. doi: 10.1080/17453670710013636. [DOI] [PubMed] [Google Scholar]
- 49.Poolman RW, Petrisor BA, Marti RK, Kerkhoffs GM, Zlowodzki M, Bhandari M. Misconceptions about practicing evidence-based orthopedic surgery. Acta Orthop. 2007b;78((1)):2–11. doi: 10.1080/17453670610013358. [DOI] [PubMed] [Google Scholar]
- 50.Quilty B, Tucker M, Campbell R, Dieppe P. Physiotherapy, including quadriceps exercises and patellar taping, for knee osteoarthritis with predominant patello-femoral joint involvement: randomized controlled trial. J Rheumatol. 2003;30((6)):1311–7. [PubMed] [Google Scholar]
- 51.Saleh KJ, Arendt EA, Eldridge J, Fulkerson JP, Minas T, Mulhall KJ. Symposium. Operative treatment of patellofemoral arthritis. J Bone Joint Surg (Am) 2005;87((3)):659–71. doi: 10.2106/JBJS.D.03035. [DOI] [PubMed] [Google Scholar]
- 52.Sisto DJ, Sarin VK. Custom patellofemoral arthroplasty of the knee. J Bone Joint Surg (Am) 2006;88((7)):1475–80. doi: 10.2106/JBJS.E.00382. [DOI] [PubMed] [Google Scholar]
- 53.Smith AM, Peckett WR, Butler-Manuel PA, Venu KM, d'Arcy JC. Treatment of patello-femoral arthritis using the Lubinus patello-femoral arthroplasty: a retrospective review. Knee. 2002;9((1)):27–30. doi: 10.1016/s0968-0160(01)00127-2. [DOI] [PubMed] [Google Scholar]
- 54.Spak RT, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis: Long-term followup. Clin Orthop. 2006;((444)):193–200. doi: 10.1097/01.blo.0000201152.98830.ed. [DOI] [PubMed] [Google Scholar]
- 55.Steimer O, Kohn D. Anteromedialization of the Tibial Tubercle. Operative Techniques in Orthopaedics. 2007;17((1)):66–71. [Google Scholar]
- 56.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283((15)):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 57.Tauro B, Ackroyd CE, Newman JH, Shah NA. The Lubinus patellofemoral arthroplasty. A five- to ten-year prospective study. J Bone Joint Surg (Br) 2001;83((5)):696–701. doi: 10.1302/0301-620x.83b5.11577. [DOI] [PubMed] [Google Scholar]
- 58.Thompson NW, Ruiz AL, Breslin E, Beverland DE. Total knee arthroplasty without patellar resurfacing in isolated patellofemoral osteoarthritis. J Arthroplasty. 2001;16((5)):607–12. doi: 10.1054/arth.2001.23570. [DOI] [PubMed] [Google Scholar]
- 59.van Jonbergen HPW, Werkman DM, van Kampen A. Conversion of patellofemoral arthroplasty to total knee arthroplasty. A matched case-control study of 13 patients. Acta Orthop. 2009;80((1)):62–6. doi: 10.1080/17453670902805031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weaver JK, Wieder D, Derkash RS. Patellofemoral arthritis resulting from malalignment. A long-term evaluation of treatment options. Orthop Rev. 1991;20((12)):1075–81. [PubMed] [Google Scholar]
- 61.Yercan HS, Ait Si Selmi T, Neyret P. The treatment of patellofemoral osteoarthritis with partial lateral facetectomy. Clin Orthop. 2005;((436)):14–9. doi: 10.1097/00003086-200507000-00004. [DOI] [PubMed] [Google Scholar]