Abstract
Objectives: To estimate the efficacy of dietary advice to lower blood total cholesterol concentration in free-living subjects and to investigate the efficacy of different dietary recommendations.
Design: Systematic overview of 19 randomised controlled trials including 28 comparisons.
Subjects: Free-living subjects.
Interventions: Individualised dietary advice to modify fat intake.
Main outcome measure: Percentage difference in blood total cholesterol concentration between the intervention and control groups.
Results: The percentage reduction in blood total cholesterol attributable to dietary advice after at least six months of intervention was 5.3% (95% confidence interval 4.7% to 5.9%). Including both short and long duration studies, the effect was 8.5% at 3 months and 5.5% at 12 months. Diets equivalent to the step 2 diet of the American Heart Association were of similar efficacy to diets that aimed to lower total fat intake or to raise the polyunsaturated to saturated fatty acid ratio. These diets were moderately more effective than the step 1 diet of the American Heart Association (6.1% v 3.0% reduction in blood total cholesterol concentration; P<0.0001). On the basis of reported food intake, the targets for dietary change were seldom achieved. The observed reductions in blood total cholesterol concentrations in the individual trials were consistent with those predicted from dietary intake on the basis of the Keys equation.
Conclusions: Individualised dietary advice for reducing cholesterol concentration is modestly effective in free-living subjects. More intensive diets achieve a greater reduction in serum cholesterol concentration. Failure to comply fully with dietary recommendations is the likely explanation for this limited efficacy.
Key messages
Results from metabolic ward studies suggest that dietary change can reduce blood cholesterol concentrations by up to 15%
In free-living subjects the standard step 1 diet of the American Heart Association lowers cholesterol concentration by about 3%, and about another 3% can be achieved with more intensive diets
Difficulties in complying with the prescribed dietary change explain the failure to achieve the expected reductions in cholesterol concentrations
It is important to be realistic about the reductions in cardiovascular risk that can be achieved by individual dietary counselling
Introduction
Blood cholesterol concentration is an important and modifiable risk factor for coronary heart disease.1 A sustained reduction in blood total cholesterol concentration of 1% is associated with a 2-3% reduction in incidence of coronary heart disease.2 Even small reductions in population cholesterol concentrations could therefore be worth while.
Dietary changes can reduce blood total cholesterol concentrations. Results from metabolic ward studies have shown that feasible changes in diet can reduce blood total cholesterol concentration by 10-15%.3 The chief determinants of blood total cholesterol concentrations are dietary intake of saturated fat, polyunsaturated fat, and cholesterol.3–6 Cholesterol concentrations are also affected by reduced energy intakes resulting in weight loss7 and possibly by specific dietary supplements such as fibre,8 garlic,9 and fish oils.10 Diets that lower cholesterol concentrations may modify some or all of these factors.
Individualised dietary counselling, usually delivered through primary care, has been proposed as a method of achieving population goals for reducing coronary artery disease by the British government in its Health of the Nation targets.11 But, the extent to which individualised cholesterol lowering diets are effective in free-living populations is controversial. One review claimed that the effect of the usual diet advised (step 1 of the American Heart Association dietary guidelines12) produced too small a reduction in blood total cholesterol concentration (less than 4%) to have much value in clinical management and that the feasibility of implementing more intensive diets was unknown.13 Another more selective review claimed, however, that dietary counselling could achieve reductions in blood total cholesterol concentration of 10% or more in free-living subjects and, hence, could play an important part in reducing rates of coronary heart disease.14
In view of the public health importance of the issue, the resource implications, and the disagreements in the literature, we reviewed systematically and quantitatively the evidence from randomised trials for the efficacy of individualised counselling for lowering cholesterol concentration.
Methods
Identification of trials and extraction of data
We aimed to identify all unconfounded randomised trials of dietary advice to lower cholesterol concentration in free-living subjects published before 1996. Trials were eligible for inclusion if there were at least two groups, of which one could be considered a control group; treatment assignment was by random allocation; the intervention was a global dietary modification (changes to various food components of the diet to achieve the desired targets); and lipid concentrations were measured before and after the intervention.
Trials of diets to reduce fat intake in women considered to be at risk of breast cancer were included because the diets were similar to those aimed at lowering cholesterol concentration. We excluded trials of specific supplementation diets (such as with particular oils or margarine, garlic, plant sterol, or fibre supplements, etc), multifactorial intervention trials, trials aimed primarily at lowering body weight or blood pressure, and trials whose interventions lasted less than 4 weeks. Trials based on randomisation of workplace or general practice were also excluded.
To identify these trials we searched four electronic databases (Medline, Human Nutrition, EMBASE, and Allied and Alternative Medicine). These databases included trials published after 1966. We also identified trials by hand searching the American Journal of Clinical Nutrition, by scrutinising the references of review articles and of each relevant randomised trial, and by consulting experts on the subject.
Two of us (JLT and JMA) independently extracted data from each identified trial on to a standard form, disagreements being resolved by another of us (TL). Reports that appeared only in non-English language journals were examined with the help of translators. Trials were categorised according to their approximate target diet into four groups.12
Step 1 diet of the American Heart Association or its equivalent (<30% of total energy intake as fat, with 8-10% as saturated fat; ratio of polyunsaturated to saturated fatty acid >1.0; cholesterol intake <300 mg/day; and energy intake to achieve desirable body weight).
Step 2 diet of the American Heart Association or its equivalent (<30% of total energy intake as fat, with 7% or less as saturated fat; ratio of polyunsaturated to saturated fatty acid >1.4; cholesterol intake <200 mg/day; and energy intake to achieve desirable body weight).
Diet to increase the ratio of polyunsaturated to saturated fatty acid with little or no change in total fat content.
Low total fat diets, without changing the proportions of the different fats consumed.
The amount of advice given to achieve dietary change was categorised as intensive (3), moderate (2), or brief (1). The criteria for this categorisation were the total number of hours of counselling, the number of adviser-subject contacts, the duration of counselling, and whether special efforts had been made to achieve change (such as home visits, spouse support, food selection skills, and providing relevant foods in local shops). In general, trials rated 3 had more than two sessions or contacts between adviser and patient per month, those rated 2 had between one and two contacts per month, and those rated 1 had on average less than one contact per month.
Compliance was estimated by comparing self reported dietary consumption during the intervention with the targets for each diet and by comparing the fall in blood total cholesterol concentration predicted by the Keys equation,6 using information from the self reported dietary data, with the observed fall in blood total cholesterol concentration.
Statistical analysis
For each comparison within each trial we computed the absolute difference (in mmol/l) in the mean change in blood total cholesterol values (baseline minus final value) between the intervention and control group. (No distinction was made between serum or plasma cholesterol values.) We expressed this difference as a percentage change in blood total cholesterol concentration using a mean of the baseline values as the denominator. The principal end point for each comparison was the percentage reduction in cholesterol concentration at the end of the intervention or at 12 months, whichever was the sooner (although we also considered reductions in cholesterol concentration at different time points). The standard error (SE) of the difference (x1−x0) for each comparison within each trial was calculated using the formula SE(x1−x0)=√(SD12/n1+SD02/n0), where x1 and x0 are the mean changes over time in the intervention and control groups respectively, SD1 and SD0 are the standard deviations of these mean changes, and n1 and n0 are the number of subjects in each group.15 When the values for SD were not given we imputed values16 using as much information as was available from that trial. The summary effect for each grouping of different trials was derived from the average of the means of each separate trial weighted by 1/SE2 for each trial.15 For studies with more than one intervention group the standard errors were adjusted to take account of the control group having been used more than once. Results are presented as mean percentage changes in blood total cholesterol concentration with 95% confidence intervals.
Similar methods were used to assess changes in reported dietary intake. To compute each change in a dietary factor requires up to four dietary measurements, each with their own measurement error and with additional correlated changes in saturated and polyunsaturated fatty acid intakes. The estimates of achieved dietary intake are therefore imprecise. For this reason, the confidence limits around the predicted values are likely to be much wider than those around the achieved reductions in cholesterol concentration. Some trials reported insufficient information to allow calculations of predicted cholesterol reductions based on the Keys equation.
We performed all analyses (including weighted means, tests for heterogeneity, significance tests, and between group comparisons) using regression techniques in sas 6.07. We explored statistical heterogeneity17 by comparing the observed results in different categories of trials grouped according to type of diet, intensity of advice, and type of patients.
Results
Description of trials
We identified published reports of 133 randomised trials of some type of dietary advice to lower blood cholesterol concentration in free-living subjects; we did not find any unpublished trials. Sixty five trials were excluded because the intervention entailed supplementation with a specific dietary factor such as fish oil, cooking oil, or a modified fat product, and a further 34 were excluded because dietary advice was part of a multifactorial intervention. Five trials were excluded because they did not have an appropriate untreated control group,18–22 three trials because they reported insufficient data for analysis,23–25 three trials because lowering body weight was their primary aim,26–28 two trials because reducing other coronary risk factors and not cholesterol concentration was their primary aim,29,30 and one trial because a large proportion of subjects were taking tamoxifen, which alters blood cholesterol concentration.31 This left 19 trials,32–52 yielding 28 comparisons eligible for inclusion in this report. Information about the trial reported by Leren is included in three publications,44–46 and the American diet-heart study includes seven different dietary comparisons.37
The table summarises the 19 trials. All stated that they were randomised, although the method of randomisation was rarely reported, and efforts had been made in most to blind those assessing results. In most of these trials the numbers of patients included in the laboratory analyses were given (the percentage analysed in the table). Five trials were in patients with coronary heart disease and the aim of the study was secondary prevention of coronary heart disease, four in subjects with raised cholesterol concentration, three in patients with raised blood pressure, four (yielding nine comparisons) in healthy adult volunteers, two in women at increased risk of breast cancer, and one in children. Most trials were in parallel groups but two were crossover in design. In the main analyses the authors assumed that the people who were not included in the reported analyses of the trial would have behaved in a way similar to those in the group to which they were allocated. An alternative assumption is that these people did not achieve any dietary change or change in their blood cholesterol concentration, and we also calculated estimates under this assumption.
Grouping of trials
The table groups trial comparisons according to their target diet. Dietary interventions that entailed both a decrease in total fat intake and an increase in the ratio of polyunsaturated to saturated fatty acid but without stated targets and those that differed from the standard diets of the American Heart Association were grouped with the diet they most closely resembled. In eight comparisons the intervention was roughly equivalent to the association’s step 1 diet and in nine to the step 2 diet. In seven comparisons the intervention diet was primarily an increase in ratio of polyunsaturated to saturated fatty acid without a change in the total fat intake. The target diet in the early trial by Leren was not clearly described but we judged it to be an increase in ratio of polyunsaturated to saturated fatty acid concentration on the basis of information given on fat intake in the Norwegian population at that time.44–46 In four trials the target diet was primarily reduced or low total fat intake. In almost all trials which provided information on the methods of dietary intervention, the methods were categorised as moderate or intensive (table), thereby not allowing any discrimination by intensity of advice.
The duration of follow up varied from six weeks to five years. The longer trials had coronary heart disease events as the primary outcome, and, in general, the shorter trials specifically measured lipid concentrations. Thirteen trials had a follow up of at least six months and provided 22 comparisons. The average baseline blood total cholesterol concentration was 6.3 mmol/l.
Overall effect of dietary advice on blood total cholesterol
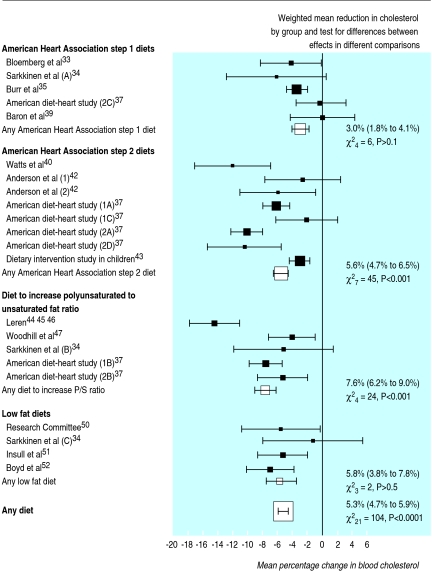
The overall weighted mean reduction in blood total cholesterol concentration across all dietary comparisons was 5.7% (95% confidence interval 5.2% to 6.3%) using either the final reduction in cholesterol concentration at the end of the intervention or at 12 months (whichever was the sooner). For the 22 comparisons available from trials of at least six months duration, the weighted mean reduction in blood cholesterol concentration was 5.3% (4.7% to 5.9%) (figure) or, if it was assumed that subjects lost to follow up experienced no change, the mean reduction in cholesterol concentration in the longer trials was 4.5% (3.9% to 5.1%). There was obvious statistical heterogeneity between the percentage reductions in blood cholesterol concentration observed in the individual comparisons of more than six months (χ221=104, P<0.001), and this was not explained by grouping the trials by category of diet (see below). Trials published before 1981 (about halfway between the first and most recently published studies) achieved greater mean reductions in blood total cholesterol concentration (7.0% ( 6.1% to 7.9%)) than those published later (3.9% (3.1% to 4.7%)) (χ21=26, P<0.001). But all except one of the earlier studies were of diets that were more intensive than the step 1 diet of the American Heart Association.
Reductions in blood cholesterol by category of diet
There were significant differences between the reductions in blood cholesterol concentration observed with the four different categories of diet (χ23=17, P<0.001). The estimated reduction in blood total cholesterol concentration with American Heart Association step 1 or equivalent diets, which lasted at least six months, was 3.0% (1.8% to 4.1%). That estimate depends heavily on one large study,35 but there was no significant heterogeneity between these different comparisons (χ24=6, P>0.1). The reduction in blood total cholesterol concentration with American Heart Association step 2 or equivalent diets was 5.6% (4.7% to 6.5%), but there was significant heterogeneity between the effects of different step 2 diets (χ27=45, P<0.001). Among the step 2 diets the dietary intervention study in children was the only trial in children (aged 8-10) and it achieved a smaller effect (3.1% (1.7% to 4.5%))43 than most of the other trials in this group. There was a significant difference between the effect observed in this trial and that observed in the other comparisons of step 2 diets (χ21=23, P<0.001) (7.4% (6.2% to 8.6%)). Diets that increased the ratio of polyunsaturated to saturated fat reduced blood cholesterol concentration by 7.6% (6.2% to 9.0%), but there was significant heterogeneity between their effects (χ24=24, P<0.001). Among the diets that increased the ratio of polyunsaturated to saturated fatty acid concentration the estimate from the trial by Leren was extreme,45 with significant heterogeneity between the estimated reduction in blood total cholesterol concentration in that trial (14.5% (11.2% to 17.8%)) and the other comparisons of diets increasing the ratio of polyunsaturated to saturated fat (6.2% (4.7% to 7.7%)) (χ21=20, P<0.001). The four comparisons of low fat diets seemed overall to reduce blood total cholesterol concentration by 5.8% (3.8% to 7.8%) without significant heterogeneity between their separate effects.
Reduction in cholesterol concentration by duration of intervention
Changes in blood total cholesterol concentration around 6 weeks and around 3, 6, 12, and 24 months were estimable in 11, 18, 14, 14, and 4 comparisons respectively, based on 2546, 3686, 4768, 6438, and 1688 subjects. The overall reduction in blood total cholesterol concentration attributable to dietary advice was 6.6% at about 6 weeks (including some values at 1 month and 2 months), 8.5% at about 3 months, 6.8% at 6 months, 5.5% at 12 months, and 4.4% at 24 months.
Compliance with dietary advice
Sixteen comparisons provided some information on reported dietary intake before and during the intervention. The table shows by category of diet reported dietary consumption of type and amount of fat and the reductions in blood total cholesterol predicted by the Keys equation. Fat intakes in the control groups were variable (ranging from 29% to 42% of total energy intake) and, in general, the dietary targets were not achieved. Among the comparisons of step 1 diets only two trials36,38 met the targets for both saturated fat and the ratio of polyunsaturated to saturated fat (10% of total fat as saturated fat and a ratio of at least 1.0); both trials also achieved the largest reductions in blood total cholesterol concentration (table). Among the comparisons of step 2 diets only the comparison of the first and second American diet heart study reached the target of 7% of energy intake as saturated fat and a ratio of polyunsaturated to saturated fatty acid concentration greater than 1.4.37 All of the interventions to increase the ratio of polyunsaturated to saturated fat achieved an increase in the ratio but the targets varied. Similarly, all the low fat diets reduced total and saturated fat intake but the targets differed. Dietary compliance might be expected to be better in patients at higher risk of cardiovascular disease, but the reduction in blood cholesterol concentration was similar in the five comparisons among patients with coronary heart disease (5.3% (4.2% to 6.4%)) and in the 17 other comparisons of at least 6 months duration (5.3% (4.9% to 5.7%)).
Discussion
The results of metabolic ward studies of dietary lipid and cholesterol concentrations suggest that switching from the typical British diet53 to at least the step 1 diet of the American Heart Association could reduce blood total cholesterol concentrations by an average of about 9% and that a step 2 diet might yield a further reduction of about 4%.3 Most of the reduction in blood total cholesterol concentration is due to reductions in low density lipoprotein cholesterol concentration. Our review shows that prescribed dietary advice about as intensive as the step 1 diet would typically achieve a reduction in blood cholesterol concentration of only about 3% in free-living subjects. The more intensive diets studied typically achieved a reduction of about 6% in blood cholesterol concentration.
The most plausible explanation for the modest effects of these diets in our overview is incomplete compliance with dietary advice. In this analysis the achieved reduction in cholesterol concentration was consistent with that predicted by the Keys equation from the estimated changes in intake of saturated and polyunsaturated fatty acid. But among the comparisons of step 1 diets, only two comparisons reported reaching the target ratio of about 1.0 for polyunsaturated to saturated fat, although the target for saturated fat intake of 10% or less was reached in five of the six comparisons which provided this information. Similarly, in the step 2 diets the target ratio of polyunsaturated to saturated fat was achieved in only one out of eight comparisons and the target of 7% of energy intake as saturated fat in only three.
Heterogeneity between study effects
The design and results of these dietary studies differed greatly. They were conducted over 30 years and varied in their aims, in the intensity and type of intervention, and in the different baseline characteristics of the subjects included. Completeness and duration of follow up also differed. Unsurprisingly, the heterogeneity between their effects on blood cholesterol concentration was also significant.17 Among the longer trials some, but not all, of the heterogeneity between the effects on blood cholesterol concentration seemed to be due to the type of diet recommended. Deciding which trials should be included in which groups is open to different interpretation and, although we tried to be consistent, for some trials the target diets either were not clearly stated or did not fit neatly into recognised categories such as the step 1 and 2 diets. It is important to be cautious in interpreting meta-analysis when there is evidence of significant heterogeneity, although there was no evidence that the overall results were influenced by trials with outlying values.
We used percentage rather than absolute changes in blood total cholesterol concentration because of the substantial differences in baseline diets and cholesterol values between these studies. This may reflect the period of several decades and the diverse populations in which the studies were carried out. In trials published before 1981, the mean reductions in blood total cholesterol concentration were greater than in later trials (7.0% v 4.0%), which may partly reflect the early predominance of more intensive diets. But we found no significant difference between the percentage reduction in blood total cholesterol concentration observed in trials with above or below average mean baseline cholesterol values (5.2% v 5.4% respectively).
Methodological issues
We included only comparisons in which the dietary advice was a single intervention. Excluding trials in which dietary advice was given together with other interventions reduced the number of subjects available for analysis. However, limiting the overview to single interventions may provide a better estimate of the effect of dietary advice by increasing the likelihood that dietary messages were delivered without dilution by other forms of health advice. In addition, this approach had the advantage that the estimate of the effect of dietary advice was largely unconfounded by other interventions which might affect cholesterol values such as exercise and substantial weight loss. The low fat diets were associated with significant weight loss (2-3 kg), and this may contribute to some of the cholesterol lowering—for example, a weight loss of 1 kg is associated with a reduction in cholesterol concentration of 0.05 mmol/l.7 However, weight loss was minimal in most of the other trials included in this overview and so is unlikely to account for much of the reduction in cholesterol concentration.
Our inclusion of only randomised and unconfounded comparisons may partly explain the smaller reductions in cholesterol concentration in comparison with some previous reviews.14
Two other methodological limitations of the present overview need to be borne in mind: the possibility of publication bias54 and the use of tabulated data derived from published reports.55 Although we tried to minimise publication bias, we were not able to identify any unpublished trials. In addition, unpublished trials might exist that would have been eligible for this review and, with only one person reviewing all the published reports of potential trials, some published trials may also have been missed. As studies with negative results are less likely to be published, the probable effect would be to further reduce our summary estimates of effectiveness. We tried to address some of the shortcomings of limiting our analysis to published tabulated data by approaching investigators and experts in the subject to obtain additional unpublished data for their studies or to clarify areas of uncertainty, but this was largely unsuccessful.
Conclusions
This systematic review suggests that dietary advice to free-living subjects can be expected to reduce blood total cholesterol by only 3-6%, depending on the type and intensity of the diet advocated. In particular, the step 1 diet of the American Heart Association has only a small cholesterol lowering effect even among those with evidence of coronary disease. Our analyses relate to effects on blood total cholesterol concentration, and diets that simply lower total fat intake may lower high density lipoprotein cholesterol concentration and offset beneficial effects on coronary heart disease from lowering low density lipoprotein cholesterol.3 This is less likely to be the case with diets in which reduction in saturated fat is replaced by polyunsaturated and monounsaturated fats rather than by complex carbohydrates. The limited efficacy of dietary advice alone should be taken into account in routine clinical practice and when assessing the cost effectiveness of different preventive strategies. More research is required to develop better methods of communicating dietary advice and maintaining compliance with such advice. Small changes in population blood total cholesterol concentrations may be worth while, but this may be better achieved by interventions aimed at populations than by advising individual people about diet.
Table.
Summary information about included trials. Studies cited more than once have several dietary comparisons within the study. Numbers in parentheses permit cross referencing to figure
| Study* | Sex | Primary end point | Baseline cholesterol (mmol/l) | Percentage of energy intake as fat (saturated, poly- unsaturated) in control group | Saturated fatty acid intake achieved as % of total energy intake | P/S (control, intervention) | Change in polyunsaturated fat as % of energy intake | Predicted% reduction in cholesterol† | Intensity rating‡ | Maximim follow up (months) | No randomised (intervention/ control group) | Percentage analysed§ | Reduction in cholesterol at end or at 12 months (%) (SE) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| American Heart Association step 1 diets | |||||||||||||
| Demark-Wahrenfreid et al 199032 | M, F | Lipids | 7.2 | 37 (11, 6) | 8 | 0.5, 0.6 | 0 | 5 | 2 | 3 | 20/20 | 83 | 2.3 (4.0) |
| Bloemberg et al 199133 | M | Lipids | 7.0 | 38 (16, 7) | 12 | 0.4, 0.8 | 3 | 5 | 2 | 6 | 39/41 | 100 | 4.3 (2.1) |
| Sarkkinen et al 1994 (A)34 | M, F | Lipids | 6.6 | 35 (14, 4) | 10 | 0.3, 0.8 | 4 | 6 | 2 | 6 | 41/39 | 99 | 6.3 (3.4) |
| Burr et al 198935 | M | CHD events | 6.5 | 36 (NR) | NR | 0.4, 0.7 | NR | NC | 1 | 24 | 1018/1015 | 84 | 3.5 (0.7) |
| Sciarrone et al 199236 | M, F | Lipids, blood pressure | 6.2 | 37 (18, 3) | 9 | 1.1, 1.4 | 7 | 14 | 2 | 2 | 48/47 | 96 | 12.2 (2.3) |
| American diet-heart study 1968 (2C)37 | M | Lipids | 6.0 | 36 (12, 5) | 10 | 0.5, 0.7 | 2 | 3 | 2 | 6.5 | 120/110 | 88 | 0.2 (1.7) |
| Ehnholm et al 198238 | M, F | Lipids | 5.7 | 39 (20, 5) | 7 | 0.3, 1.0 | 2 | 17 | 3 | 1.5 | 36/38 | 100 | 22.6 (1.8) |
| Baron et al 199039 | M, F | Lipids | 4.9 | 35 (NR) | NR | NR | NR | NC | 1 | 12 | 219/218 | 76 | 0.0 (2.2) |
| American Heart Association step 2 diets | |||||||||||||
| Watts et al 199240 | M | MAWS | 7.1 | NR | NR | NR | NR | NC | 1 | 39 | 30/30 | 83 | 12.2 (2.6) |
| Hunninghake et al 199341¶ | M, F | Lipids | 7.0 | 41 (15, 8) | 7 | 0.5, 1.05 | 0 | 8 | 2 | 2 | 111/111 | 90 | 5.0 (0.8) |
| Anderson et al 1992 (1)42 | M, F | Lipids | 6.0 | 31 (10, 7) | 9 | 0.7, 0.9 | 1 | 2 | 2 | 12 | 59/62 | 83 | 2.8 (2.6) |
| Anderson et al 1992 (2)42 | M, F | Lipids | 6.0 | 31 (10, 7) | 8 | 0.7, 0.9 | 0 | 2 | 2 | 12 | 59/62 | 82 | 6.1 (2.6) |
| American diet-heart study 1968 (1A)37 | M | Lipids | 5.9 | 35 (12, 5) | 7 | 0.4, 1.4 | 5 | 8 | 2 | 12 | 385/382 | 80 | 6.3 (0.9) |
| American diet-heart study 1968 (1C)37 | M | Lipids | 5.9 | 35 (12, 5) | 9 | 0.4, 0.8 | 2 | 4 | 2 | 12 | 54/73 | 80 | 2.2 (2.1) |
| American diet-heart study 1968 (2A)37 | M | Lipids | 5.9 | 36 (12, 5) | 7 | 0.5, 1.6 | 6 | 9 | 2 | 6.5 | 194/110 | 91 | 10.2 (1.1) |
| American diet-heart study 1968 (2D)37 | M | Lipids | 5.9 | 40 (16, 4) | 8 | 0.2, 1.1 | 5 | 12 | 2 | 6.5 | 36/36 | 95 | 10.5 (2.5) |
| Dietary intervention study in children 199543 | M, F | CHD risk | 5.2 | 33 (12, 6) | 9 | 0.5, 0.6 | 0 | 3 | 2 | 12 | 334/329 | 94 | 3.1 (0.7) |
| Diets increasing P/S | |||||||||||||
| Leren 1966, 1968, 197044 45 46 | M | CHD events | 7.6 | 40 (NR) | NR | NR | NR | NC | 2 | 60 | 229/229 | 66 | 14.5 (1.7) |
| Woodhill et al 197847 | M | CHD events | 7.2 | 38 (14, 9) | 10 | 0.8, 1.7 | 6 | 7 | 1 | 84 | 221/237 | 87 | 4.1 (1.6) |
| Sarkkinen 1994 (C)34 | M, F | Lipids | 6.5 | 35 (14, 4) | 11 | 0.3, 0.5 | 1 | 3 | 2 | 6 | 41/39 | 99 | 5.2 (3.4) |
| Kuusi 198548 | M, F | Lipids | 6.2 | 23 (10, 4) | 8 | 0.4, 0.9 | 3 | 4 | 3 | 3 | 40/40 | 98 | 4.0 (3.5) |
| American diet-heart study 1968 (1B)37 | M | Lipids | 5.9 | 36 (12, 5) | 8 | 0.5, 1.8 | 8 | 9 | 2 | 12 | 390/382 | 80 | 7.6 (1.1) |
| American diet-heart study 1968 (2B)37 | M | Lipids | 6.1 | 35 (12, 5) | 8 | 0.4, 1.8 | 8 | 10 | 2 | 6.5 | 127/110 | 89 | 5.3 (1.7) |
| Dreon et al 199049¶ | M, F | Lipids | 5.0 | 29 (8, 5) | 8 | 0.7, 1.7 | 4 | 3 | 2 | 3 | 39/39 | 90 | 0.6 (2.3) |
| Low fat diets | |||||||||||||
| Research Committee 196550 | M | CHD | 6.8 | 42 (NR) | NR | NR | NR | NC | 2 | 48 | 132/132 | 69 | 5.7 (2.7) |
| Sarkkinen et al 199434 | M, F | Lipids | 6.3 | 35 (14, 4) | 12 | 0.3, 0.3 | −1 | 2 | 2 | 6 | 40/39 | 99 | 1.4 (3.4) |
| Insull et al 199051 | F | Fat intake | 5.7 | 37 (13, 7) | 7 | 0.5, 0.6 | 3 | 9 | 2 | 24 | 184/119 | 89 | 5.4 (1.7) |
| Boyd et al 198852 | F | Fat intake | 4.8 | 36 (14, 6) | 8 | 0.5, 0.6 | −2 | 7 | 2 | 12 | 148/147 | 72 | 7.1 (1.6) |
CHD=coronary heart disease. MAWS=mean absolute width of coronary segments on angiography. P/S=polyunsaturated to saturated fatty acid ratio. NR=not reported. NC=not calculable because the necessary information was not reported.
Diets are listed in order of decreasing baseline cholesterol concentration within each group.
Predicted on the basis of the Keys equation for change in saturated and polyunsaturated fatty acid intake.
Intensity rating (1=least intensive, 3=most intensive).
Overall percentage in both intervention and control groups.
Crossover design.
Figure.
Mean percentage changes (with 95% confidence intervals) in blood total cholesterol concentration for each study with at least six months of follow up according to type of diet. Studies cited more than once have several dietary comparisons within the study. Numbers in parentheses permit cross referencing to table
Acknowledgments
We acknowledge the help of Simon Wilson and Paul Sherliker in preparing the original figure, and we thank Robert Clarke for his helpful comments about the manuscript.
Footnotes
Funding: The study was funded by a project grant from the nutrition programme phase 1 of the Department of Health and Medical Research Council. JMA is supported by the British Heart Foundation. TL is supported by the Imperial Cancer Research Fund. The Clinical Trial Service Unit and Epidemiological Studies Unit receives funding from the Medical Research Council, British Heart Foundation, and Imperial Cancer Research Fund.
Conflict of interest: None.
References
- 1.Martin MJ, Hulley SB, Browner WS, Kuller LH, Wentworth D. Serum cholesterol, blood pressure, and mortality: implications from a cohort of 361,662 men. Lancet. 1986;2:933–936. doi: 10.1016/s0140-6736(86)90597-0. [DOI] [PubMed] [Google Scholar]
- 2.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308:367–372. doi: 10.1136/bmj.308.6925.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clarke R, Frost C, Collins R, Appleby P, Peto R. Dietary lipids and blood cholesterol: a quantitative meta-analysis of metabolic ward studies. BMJ. 1997;314:112–117. doi: 10.1136/bmj.314.7074.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hegsted DM, Ausman LM, Johnson JA, Dallal GE. Dietary fat and serum lipids: an evaluation of the experimental data. Am J Clin Nutr. 1993;57:875–883. doi: 10.1093/ajcn/57.6.875. [DOI] [PubMed] [Google Scholar]
- 5.Hegsted DM, McGandy RB, Myers ML, Stare FJ. Quantitative effects of dietary fat on serum cholesterol in man. Am J Clin Nutr. 1965;17:281–295. doi: 10.1093/ajcn/17.5.281. [DOI] [PubMed] [Google Scholar]
- 6.Keys A, Anderson JT, Grande F. Prediction of serum cholesterol responses of man to changes in fat in the diet. Lancet. 1957;ii:959–966. doi: 10.1016/s0140-6736(57)91998-0. [DOI] [PubMed] [Google Scholar]
- 7.Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56:320–328. doi: 10.1093/ajcn/56.2.320. [DOI] [PubMed] [Google Scholar]
- 8.Ripsin CM, Keenan JM, Jacobs DR, Jr, Elmer PJ, Welch RR, Van Horn L, et al. Oat products and lipid lowering: A meta-analysis. JAMA. 1992;267:3317–3325. [PubMed] [Google Scholar]
- 9.Silagy C, Neil A. Garlic as a lipid lowering agent—a meta-analysis. J R Coll Phys Lond. 1994;28:39–45. [PMC free article] [PubMed] [Google Scholar]
- 10.Harris WS. Fish oils and plasma lipid and lipoprotein metabolism in humans: a critical review. J Lipid Res. 1989;30:785–807. [PubMed] [Google Scholar]
- 11.Secretary of State for Health. The health of the nation: a strategy for health in England. London: HMSO; 1992. (Cm 1986.) [Google Scholar]
- 12.Expert Panel. Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Arch Intern Med. 1988;148:36–69. [PubMed] [Google Scholar]
- 13.Ramsay LE, Yeo WW, Jackson PR. Dietary reduction of serum cholesterol concentration: time to think again. BMJ. 1991;303:953–957. doi: 10.1136/bmj.303.6808.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Denke MA. Cholesterol-lowering diets. A review of the evidence. Arch Intern Med. 1995;155:17–26. [PubMed] [Google Scholar]
- 15.Bracken MB. Statistical methods for analysis of effects of treatment in overviews of randomised trials. In: Sinclair JC, Bracken MB, editors. Effective care of the new-born infant. Oxford: Oxford University Press; 1992. pp. 13–18. [Google Scholar]
- 16.Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45:769–773. doi: 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- 17.Thompson SG. Why sources of heterogeneity in meta-analysis should be investigated. BMJ. 1994;309:1351–1355. doi: 10.1136/bmj.309.6965.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neil HA, Roe L, Godlee RJP, Moore JW, Clark GMG, Brown J, et al. Randomised trial of lipid lowering dietary advice in general practice: the effects on serum lipids, lipoproteins, and antioxidants. BMJ. 1995;310:569–573. doi: 10.1136/bmj.310.6979.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rivellese AA, Auletta P, Marotta G, Saldalamacchia G, Giacco A, Mastrilli V, et al. Long term metabolic effects of two dietary methods of treating hyperlipidaemia. BMJ. 1994;308:227–231. doi: 10.1136/bmj.308.6923.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duffield RG, Lewis B, Miller NE, Jamieson CW, Brunt JN, Colchester AC. Treatment of hyperlipidaemia retards progression of symptomatic femoral atherosclerosis. A randomised controlled trial. Lancet. 1983;2:639–642. doi: 10.1016/s0140-6736(83)92527-8. [DOI] [PubMed] [Google Scholar]
- 21.Johnston HJ, Jones M, Ridler Dutton G, Spechler F, Stokes GS, Wyndham LE. Diet modification in lowering plasma cholesterol levels. A randomised trial of three types of intervention. Med J Aust. 1995;162:524–526. [PubMed] [Google Scholar]
- 22.Kromhout D, Arntzenius AC, van der Velde EA. Diet and coronary heart disease: the Leiden intervention trial. Bibl Nutr Dieta. 1986;37:119–120. doi: 10.1159/000412179. [DOI] [PubMed] [Google Scholar]
- 23.Reid CM, Dart AM, Dewar EM, Jennings GL. Interactions between the effects of exercise and weight loss on risk factors, cardiovascular haemodynamics and left ventricular structure in overweight subjects. J Hypertens. 1994;12:291–301. [PubMed] [Google Scholar]
- 24.Curzio JL, Kennedy SS, Elliott HL, Farish E, Barnes JF, Howie CA, et al. Hypercholesterolaemia in treated hypertensives: A controlled trial of intensive dietary advice. J Hypertens. 1989;7:S254–S255. doi: 10.1097/00004872-198900076-00123. [DOI] [PubMed] [Google Scholar]
- 25.Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary treatment of patients with mild to moderate hypertension in a general practice: a pilot intervention study. I. The first three months. J Hum Hypertens. 1990;4:368–371. [PubMed] [Google Scholar]
- 26.Jalkanen L. The effect of a weight reduction program on cardiovascular risk factors among overweight hypertensives in primary health care. Scand J Soc Med. 1991;19:66–71. doi: 10.1177/140349489101900112. [DOI] [PubMed] [Google Scholar]
- 27.MacMahon S, Macdonald G. Treatment of high blood pressure in overweight patients. Nephron 1987;47 (suppl 1):8-12. [DOI] [PubMed]
- 28.Marniemi J, Seppanen A, Hakala P. Long-term effects on lipid metabolism of weight reduction on lactovegetarian and mixed diet. Int J Obes. 1990;14:113–125. [PubMed] [Google Scholar]
- 29.De Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaund I, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454–1459. doi: 10.1016/s0140-6736(94)92580-1. 1995;345:738.] [DOI] [PubMed] [Google Scholar]
- 30.Singh RB, Rastogi SS, Sircar AR, Mehta PJ, Sharma KK. Dietary strategies for risk-factor modification to prevent cardiovascular diseases. Nutrition. 1991;7:210–214. [PubMed] [Google Scholar]
- 31.Buzzard IM, Asp EH, Chlebowski RT, Boyar AP, Jeffrey RW, Nixon DW, et al. Diet intervention methods to reduce fat intake: nutrient and food group composition of self-selected low-fat diets. J Am Diet Assoc. 1990;90:42–50. , 53. [PubMed] [Google Scholar]
- 32.Demark-Wahnefried W, Bowering J, Cohen PS. Reduced serum cholesterol with dietary change using fat-modified and oat bran supplemented diets. J Am Diet Assoc. 1990;90:223–229. [PubMed] [Google Scholar]
- 33.Bloemberg BPM, Kromhout D, Goddijn HE, Jansen A, Obermann de Boer GL. The impact of the guidelines for a healthy diet of the Netherlands Nutrition Council on total and high density lipoprotein cholesterol in hypercholesterolemic free-living men. Am J Epidemiol. 1991;134:39–48. doi: 10.1093/oxfordjournals.aje.a115991. [DOI] [PubMed] [Google Scholar]
- 34.Sarkkinen ES, Uusitupa MI, Pietinen P, Aro A, Ahola I, Penttila I, et al. Long-term effects of three fat-modified diets in hypercholesterolemic subjects. Atherosclerosis. 1994;105:9–23. doi: 10.1016/0021-9150(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 35.Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART) Lancet. 1989;2:757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 36.Sciarrone SEG, Beilin LJ, Rouse IL, Rogers PB. A factorial study of salt restriction and a low-fat/high-fibre diet in hypertensive subjects. J Hypertens. 1992;10:287–298. doi: 10.1097/00004872-199203000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Anonymous. The national diet-heart study final report. Circulation. 1968;37:I1–428. [PubMed] [Google Scholar]
- 38.Ehnholm C, Huttunen JK, Pietinen P, Leino U, Mutanen M, Kostiainen E, et al. Effect of diet on serum lipoproteins in a population with a high risk of coronary heart disease. N Engl J Med. 1982;307:850–855. doi: 10.1056/NEJM198209303071403. [DOI] [PubMed] [Google Scholar]
- 39.Baron JA, Gleason R, Crowe B, Mann JI. Preliminary trial of the effect of general practice based nutritional advice. Br J Gen Pract. 1990;40:137–141. [PMC free article] [PubMed] [Google Scholar]
- 40.Watts GF, Lewis B, Brunt JNH, Lewis ES, Coltart DJ, Smith LDR, et al. Effects on coronary artery disease of lipid-lowering diet, or diet plus cholestyramine, in the St Thomas’ atherosclerosis regression study (STARS) Lancet. 1992;339:563–569. doi: 10.1016/0140-6736(92)90863-x. [DOI] [PubMed] [Google Scholar]
- 41.Hunninghake DB, Stein EA, Dujovne CA, Harris WS, Feldman EB, Miller VT, et al. The efficacy of intensive dietary therapy alone or combined with lovastatin in outpatients with hypercholesterolemia. N Engl J Med. 1993;328:1213–1219. doi: 10.1056/NEJM199304293281701. [DOI] [PubMed] [Google Scholar]
- 42.Anderson JW, Garrity TF, Wood CL, Whitis SE, Smith BM, Oeltgen PR. Prospective, randomised, controlled comparison of the effects of low- fat and low-fat plus high-fiber diets on serum lipid concentrations. Am J Clin Nutr. 1992;56:887–894. doi: 10.1093/ajcn/56.5.887. [DOI] [PubMed] [Google Scholar]
- 43.Writing Group for the DISC Collaborative Research Group. Efficacy and safety of lowering dietary intake of fat and cholesterol in children with elevated low-density lipoprotein cholesterol. The dietary intervention study in children (DISC) JAMA. 1995;273:1429–1435. doi: 10.1001/jama.1995.03520420045036. [DOI] [PubMed] [Google Scholar]
- 44.Leren P. The Oslo diet-heart study. Eleven-year report. Circulation. 1970;42:935–942. doi: 10.1161/01.cir.42.5.935. [DOI] [PubMed] [Google Scholar]
- 45.Leren P. The effect of plasma-cholesterol-lowering diet in male survivors of myocardial infarction. A controlled clinical trial. Bull N Y Acad Med. 1968;44:1012–1020. [PMC free article] [PubMed] [Google Scholar]
- 46.Leren P. The effect of plasma cholesterol lowering diet in male survivors of myocardial infarction. A controlled clinical trial. Acta Med Scand Suppl. 1966;466:1–92. [PubMed] [Google Scholar]
- 47.Woodhill JM, Palmer AJ, Leelarthaepin B, McGilchrist C, Blacket RB. Low fat, low cholesterol diet in secondary prevention of coronary heart disease. Adv Exp Med Biol. 1978;109:317–330. doi: 10.1007/978-1-4684-0967-3_18. [DOI] [PubMed] [Google Scholar]
- 48.Kuusi T, Ehnholm C, Huttunen JK, Kostiainen E, Pietinen P, Leino U, et al. Concentration and composition of serum lipoproteins during a low-fat diet at two levels of polyunsaturated fat. J Lipid Res. 1985;26:360–367. [PubMed] [Google Scholar]
- 49.Dreon DM, Vranizan KM, Krauss RM, Austin MA, Wood PD. The effects of polyunsaturated fat vs monounsaturated fat on plasma lipoproteins. JAMA. 1990;263:2462–2466. [PubMed] [Google Scholar]
- 50.Research Committee. Low-fat diet in myocardial infarction: A controlled trial. Lancet. 1965;2:501–504. [PubMed] [Google Scholar]
- 51.Insull W, Jr, Henderson MM, Prentice RL, Thompson DJ, Clifford C, Goldman S, et al. Results of a randomised feasibility study of a low-fat diet. Arch Intern Med. 1990;150:421–427. [PubMed] [Google Scholar]
- 52.Boyd NF, Cousins M, Beaton M, Fishell E, Wright B, Fish E, et al. Clinical trial of low-fat, high-carbohydrate diet in subjects with mammographic dysplasia: report of early outcomes. J Natl Cancer Inst. 1988;80:1244–1248. doi: 10.1093/jnci/80.15.1244. [DOI] [PubMed] [Google Scholar]
- 53.Gregory J, Foster K, Tyler H, Wiseman M. The dietary and nutritional survey of British adults. London: HMSO; 1990. [Google Scholar]
- 54.Simes RJ. Publication bias: the case for an international registry of clinical trials. J Clin Oncol. 1986;4:1529–1541. doi: 10.1200/JCO.1986.4.10.1529. [DOI] [PubMed] [Google Scholar]
- 55.Stewart LA, Parmar MK. Meta-analysis of the literature or of individual patient data: is there a difference? Lancet. 1993;341:418–422. doi: 10.1016/0140-6736(93)93004-k. [DOI] [PubMed] [Google Scholar]