Abstract
Depression is less prevalent among older adults than among younger adults but can have serious consequences. Over half of cases represent a first onset in later life. Although suicide rates in the elderly are declining, they are still higher than in younger adults and more closely associated with depression. Depressed older adults are less likely to endorse affective symptoms and more likely to display cognitive changes, somatic symptoms, and loss of interest than are younger adults. Risk factors leading to the development of late life depression likely comprise complex interactions among genetic vulnerabilities, cognitive diathesis, age-associated neurobiological changes, and stressful events. Insomnia is an often overlooked risk factor for late life depression. We suggest that a common pathway to depression in older adults, regardless of which predisposing risks are most prominent, may be curtailment of daily activities. Accompanying self-critical thinking may exacerbate and maintain a depressed state. Offsetting the increasing prevalence of certain risk factors in late life are age-related increases in psychological resilience. Other protective factors include higher education and socioeconomic status, engagement in valued activities, and religious or spiritual involvement. Treatments including behavioral therapy, cognitive behavioral therapy, cognitive bibliotherapy, problem-solving therapy, brief psychodynamic therapy, and life review/reminiscence therapy are effective but too infrequently used with older adults. Preventive interventions including education for individuals with chronic illness, behavioral activation, cognitive restructuring, problem-solving skills training, group support, and life review have also received support.
Keywords: Epidemiology, Etiology, Treatment, Prevention, Elderly
INTRODUCTION
Because of its devastating consequences, late life depression is an important public health problem. It is associated with increased risk of morbidity, increased risk of suicide, decreased physical, cognitive and social functioning, and greater self-neglect, all of which are in turn associated with increased mortality (Blazer, 2003). At the same time, contrary to common perception, major depression appears to be less frequent among older adults than at earlier ages (Hasin, Goodwin, Stinson, & Grant, 2005).
Depression in older adults differs in both subtle and obvious ways from depression earlier in the lifespan. Presentation, etiology, risk and protective factors, and potential outcomes all reflect aspects of the older adult's position in the lifespan. Knowledge of the ways in which age may alter factors associated with the onset and maintenance of depression is essential for effective treatment of depressed older adults.
Following this introduction, we provide an overview of current research on the epidemiology, risk and protective factors, sequelae and treatment of late life depression. Wherever possible, we include information about factors that moderate risks or treatment efficacy.
Life course perspective
AGE OF ONSET OF DISORDER
A key distinction in discussions of mental disorder in older adults is between those individuals who have already experienced mental illness earlier in life and those whose first encounter with mental illness occurs in old age. The distinction portends differences in etiology and prognosis, but also differences in the lived experience of having a mental illness.
It appears that half or more of geriatric major depression represents a new condition arising in old age (called late onset depression), whereas half or less experienced their first episode of depression considerably before old age (called early onset depression). For example, among inpatients and outpatients in a geriatric mood disorders unit, Brodaty et al. (2001) found 52% with first onset at age 60 or older, whereas 71% of depressed older home care patients in another study were experiencing their first episode of depression (Bruce et al., 2002). However, studies of late life depression do not systematically report proportions of cases that are early versus late onset, and the age after which onset is called “late” varies considerably. Also unknown is what proportion of those who have experienced depression earlier in life have a recurrence or continuation in later life, and what proportion never again suffer a depressive episode.
There is substantial consensus that older adults with late onset depression have distinctive risk factors and presentation. Those with early onset depression are more likely than those with late onset depression to have a family history of depression (e.g., Heun, Papassotiropoulos, Jessen, Maier, & Breitner, 2001), possibly implying that occurrence of disorder was genetically influenced. Those with early onset depression may also have a higher prevalence of personality disorder or elevated scores on personality traits such as neuroticism (e.g., Brodaty et al., 2001).
The question of what leads an older adult to become depressed is most sharply raised by late onset depression. Most scholars are now focusing on structural changes in the brain. Some have found that older adults with late onset depression are more likely to have vascular risk factors (e.g., Hickie et al., 2001) including history of cerebrovascular disease, although this conclusion is not always supported (e.g., Brodaty et al., 2001). Many studies—but not all—have reported that older adults with late onset depression are more likely to have concomitant cognitive deficits, especially executive cognitive functioning, or are more likely subsequently to develop dementia (see review by Schweitzer, Tuckwell, O'Brein, & Ames, 2002). Neurological findings, including white matter hyperintensities or leukoencephalopathy, are reported as common among late onset but not among early onset depression patients (Krishnan, 2002). The particular frontal-striatal and frontal-limbic brain pathways that are disrupted by these neurological changes are involved in regulating mood. The term “vascular depression” was offered as a hypothesis to explain these findings, later supplanted by the term “depression-executive dysfunction syndrome of late life” in order to encompass dysfunction that may not be exclusively caused by vascular disease (Alexopoulos, 2005). As discussed at greater length later in this article, it seems likely that some proportion of late onset depression—particularly when there is accompanying cognitive impairment or evidence of structural brain changes—represents a prodromal phase of dementia or other acquired cognitive dysfunction. As we also will discuss, while far less studied, the other possible explanation for late onset depression is a response by individuals with certain longstanding vulnerabilities to the occurrence of a unique configuration of stressful life events and losses.
Of course, as pointed out by Alexopoulos (2005), even if there is a special late onset form of depression, it may also arise in an older patient who had depression earlier in life. Thus, characteristics that define late onset depression might be found as well in some older patients who report a previous episode of depression. For this reason, in this article we use the term “late life depression” to encompass both early and late onset cases, and we only refer to age of onset where this distinction was made in the cited study.
LIFE SPAN DEVELOPMENTAL DIATHESIS-STRESS MODEL
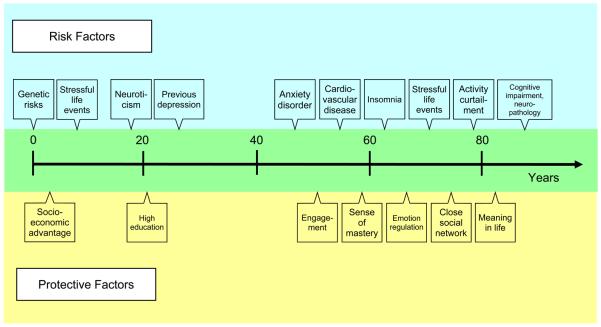
Beyond placing the onset of disorder in the life course, a life span perspective situates risk and protective factors developmentally, as illustrated in Figure 1. We discuss these factors in respective sections below. Inclusion of protective factors as well as risk factors in a developmental model is crucial to crafting an explanation for decreasing rates of depression in old age.
Figure 1.
Life span perspective on risk and protective factors for late life major depression. Schematic illustrating risk and protective factors corresponding to when they emerge over the life span.
EPIDEMIOLOGY
Several depressive disorders are described in the Diagnostic and Statistical Manual for Mental Disorders (4th Edition; DSM-IV; American Psychiatric Association, 1994), including major depressive disorder, dysthymic disorder, bipolar disorder and mood disorder due to a general medical condition. Adjustment disorder with depressed mood may also be considered a form of depression.
Much attention has recently been given to the experience of depressive symptoms that do not fulfill the criteria for a diagnosis of major depressive disorder. Some research has investigated this phenomenon using more or less well-defined categories, e.g., minor depression, subsyndromal depression, etc., whereas other investigators have defined clinically significant depressive symptoms as a score above a threshold on a depressive symptom checklist. Some (Judd, Schettler, & Akiskal, 2002) but not all (Ruscio, Zimmerman, McGlinchey, Chelminski, & Young, 2007) evidence suggests that depression may occur on a spectrum, with symptoms that do not meet syndromal criteria for major depressive disorder representing a less severe manifestation of the same disorder. In older adulthood, the prevalence of major depressive disorder differs from that of clinically significant depressive symptoms, as we discuss below. Nonetheless, in most cases the same risk and protective factors are associated with both. Where differences have been documented, we so indicate. In the present review, we focus primarily on major depressive disorder.
The prevalence of major depressive disorder at any given time in community samples of adults aged 65 and older ranges from 1-5% in most large-scale epidemiological investigations in the United States and internationally, with the majority of studies reporting prevalence in the lower end of the range (e.g., Hasin et al., 2005). Clinically significant depressive symptoms are present in approximately 15% of community-dwelling older adults (Blazer, 2003). Rates of depression appear to be higher in older women than in older men, but with the gender gap somewhat narrower in this age group, particularly among the oldest old, than the two-fold difference seen across the rest of the adult lifespan (Djernes, 2006). There are few differences in depression prevalence by race or ethnicity, although depressive symptoms may be more common among Hispanic older women than non-Hispanic whites (Swenson, Baxter, Shetterly, Scarbro, & Hamman, 2000).
Rates of major depression among older adults are substantially higher in particular subsets of the older adult population, including medical outpatients (5-10%, though estimates vary widely), medical inpatients (10-12%), and residents of long term care facilities (14 to 42%; Blazer, 2003; Djernes, 2006). Congregate living arrangements are not depressogenic per se, as shown by the lower rate of depression found among older kibbutz residents compared to community samples (Blumenstein et al., 2004); rather, relocation to congregate living is typically occasioned by health issues and/or loss of a caregiving spouse.
Prevalence of major depression in community samples of older adults reflects a significant decline from midlife prevalence rates for both men and women. In contrast, most studies that measure elevated scores on a depressive symptom checklist (rather than diagnosis of a depressive disorder) report higher rates of clinically significant depressive symptoms among older adults than in midlife (Newmann, 1989). How should these differences in prevalence be interpreted? The diagnostic rubric for major depressive disorder may underestimate disorder among older adults. Current diagnostic criteria privilege dysphoria, a symptom less frequently endorsed by older adults compared to younger adults (Gallo, Anthony, & Muthén, 1994), and require a judgment that symptoms are not attributable to the direct physiological effects of a medication or general medical condition, or to a recent bereavement. Conversely, depressive symptom checklists are inflated, as they do not exclude symptoms that are directly linked to a physical illness or bereavement, both of which increase in frequency with age. As Blazer (2003) and others have demonstrated, depressive symptoms actually decrease in frequency with age after accounting for the effects of gender, education, physical illness and bereavement, though it should be noted that physical illness and bereavement can be causes of depression rather than simply confounds. Thus, the preponderance of evidence indicates that depression becomes less common and less severe with age, but that lower-severity depressive symptoms, which can also be consequential and treatable (Judd et al., 2002), should not be overlooked. We elaborate reasons for age differences in depressive symptom prevalence below; first we turn to age differences in presentation of depression.
PRESENTATION
Differences from younger adults
Depression in older adults may present somewhat differently than in younger adults. For example, older adults are less likely to endorse cognitive-affective symptoms of depression, including dysphoria and worthlessness/guilt, than are younger adults (Gallo et al., 1994). Sleep disturbance, fatigue, psychomotor retardation, loss of interest in living, and hopelessness about the future may be more prevalent in late-life depression than in depression in younger or middle-aged adults (Christensen et al., 1999). Subjective complaints of poor memory and concentration are also common among depressed older adults. Slower cognitive processing speed and executive dysfunction are frequent findings from objective testing (Butters et al., 2004). Overall there do not appear to be substantial differences by gender or ethnicity. Some evidence suggests that older African Americans are even less likely to report dysphoria than European-Americans and more likely to report thoughts of death (Gallo, Cooper-Patrick, & Lesikar, 1998). With respect to somatic symptoms, depressed older women report more appetite disturbance than men, whereas older men report more agitation (Kockler & Heun, 2002).
Several geriatric-specific variants of depression have been proposed. One variant, reflecting the predominant age differences in presentation, has been called “depression without sadness” or “depletion syndrome” (Gallo, Rabins, Lyketsos, Tien, & Anthony, 1997; Newman, Engel, & Jensen, 1991). Another variant is the “depression-executive dysfunction syndrome” (Alexopoulos, 2005). As the name indicates, cognitive performance in this syndrome is typically impaired on measures of verbal fluency, naming, and initiation/perseveration. The syndrome also includes psychomotor retardation and anhedonia but less severe vegetative symptoms, agitation, and guilt than other types of depression.
Two other largely geriatric variants, “depression in Alzheimer's disease” and “depression in Parkinson's disease,” are discussed below.
Presentation in the Context of Physical and Neurological Illness
As noted, depression rates are markedly elevated in those with other medical conditions. However, measurement issues may confound the issue of comorbidity. According to the DSM-IV, major depressive disorder cannot be diagnosed when symptoms are the direct physiological result of a medical condition. Thus, depression may be either underdiagnosed or overdiagnosed in the presence of conditions such as cancer that can cause fatigue and weight loss. Overattributing these symptoms to the physical illness even when other mood symptoms are present represents underdiagnosis. Failing to take the physical illness into account can lead to overdiagnosis.
Depression presents differently among patients with neurological syndromes. Depression following stroke, especially with right hemisphere damage, is less likely to include dysphoria and is more strongly characterized by vegetative symptoms than are other forms of late life depression (Paradiso, Vaidya, Tranel, Kosier, & Robinson, 2008). Depression associated with Parkinson's disease (PD) is a milder form of depression and is less frequently associated with dysphoria and anhedonia than is depression in older adults without neurological illness (Ehrt, Bronnick, Leentjens, Larsen, & Aarsland, 2006). In order to avoid underdiagnosing depression in PD, a study group that proposed a specific syndrome, depression of Parkinson's disease, recommends an inclusive approach in which all symptoms are “counted” towards a diagnosis of major depression even if they overlap with PD symptoms (Marsh et al., 2006).
Diagnosing depression in the context of dementia is complicated by deficits in verbal expression and potential confounding with cognitive symptoms, which has led to the development of diagnostic criteria to describe co-morbid Alzheimer's disease (AD) and depression (see Olin et al., 2002). Depression of Alzheimer disease is diagnosed in the presence of three or more symptoms of major depression, not including difficulty concentrating, but including additional nonsomatic symptoms such as irritability and social withdrawal. Depression in vascular dementia, compared to depression in AD, is characterized by more vegetative symptoms such as fatigue, muscular weakness, and weight loss (Park et al., 2007).
ETIOLOGY AND RISK AND PROTECTIVE FACTORS
Etiology
Why might a person become depressed, especially for the first time, in old age? Figure 1 provides a lifespan view of risk factors that may help to explain the occurrence of depression in an older person. Biological factors loom large in late life. Both cardiovascular and neurological changes that occur with normal aging or with age-associated diseases appear to increase vulnerability to depression. But these explanations are not sufficient in light of the fact that neurobiological changes are ubiquitous with aging and physical disease is not uncommon, yet only a small fraction of older adults become depressed. It would also be easy to point to all of the losses that characterize later life; yet, most older adults experience stressful life events and only a small proportion become depressed. For these reasons, we suggest that the onset and maintenance of depression in late life can be understood as an interaction between certain vulnerabilities, including genetic factors, cognitive diathesis and age-associated neurobiological changes, and the types of stressful events that occur with greater frequency in late life than earlier in the lifespan.
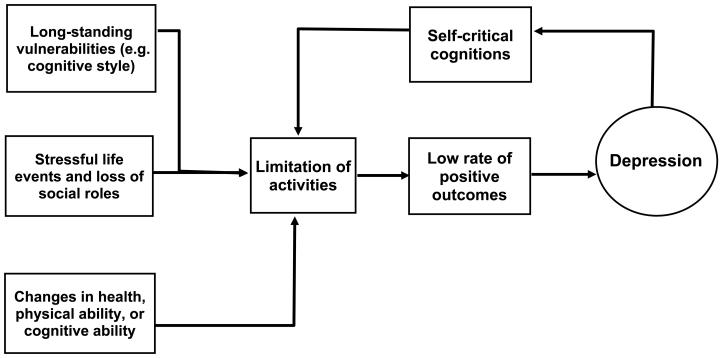
Behavioral explanations of depression that are not specific to late life disorder focus on a relative lack of events with positive outcomes (Lewinsohn, Muñoz, Youngren, & Zeiss, 1986). Because engagement in activities is not reinforced, frequency declines, resulting in turn in fewer opportunities for interactions with the environment that have positive outcomes. Compared to non-depressed individuals, those who are depressed exhibit social skill deficits that are likely to lead to less engagement and more negative outcomes. Although not emphasized in Lewinsohn et al. (1986), self-critical cognitions may also play a role in curtailing a depressed person's engagement in activities. In the depressed person, activities are often followed by self-critical cognitions, which would have a punishing effect on the person's efforts, resulting in a further decline in the engagement in activities. Because the self-critical internal verbalizations also function to provide a rationale for not engaging in future behaviors that are deemed likely to result in failure, the cognition may be negatively reinforced and thus more likely to occur in the future. The result would be a feedback loop in which negative cognitions reduce the level of active engagement with the environment, and the cognitions are maintained by the relief associated with not risking additional failure. Thus, both the lack of opportunity for positive outcomes and the aversive experience of self-critical cognitions may intensify and maintain a depressive state. Figure 2 illustrates this model.
Figure 2.
Behavioral model of late life depression. Model depicting onset and maintenance of depression in late life.
Aging is replete with reasons to reduce activity or even engage in occasional negative self-talk, but certain individuals may be more likely than others to do so when faced with the particular types of stressful events that are most common in late life. For example, stressful events that involve threats to competence (e.g., functional and cognitive limitations), which become predominant in late life, may pose special risks for people who more heavily value personal success and control. Role changes associated with spousal bereavement, e.g., taking on tasks such as household management, driving, and social planning that were formerly performed by the spouse, may lead to a reduction of activities and an increase in negative self-evaluation, particularly among older adults who are less flexible or less open to experience. Finally, pervasive negative stereotypes about aging may increase the likelihood that any older adult would engage in self-critical thoughts, especially for those with a neurotic style.
In summary, many of the changes that accompany aging could lead to reduced engagement with the environment, particularly among individuals with existing vulnerabilities; if this process is not interrupted (e.g., through encouragement or support for taking on new, meaningful activities and roles), the outcome is likely to be a depressed mood, maintained and intensified by concomitant self-critical cognitions.
The process described in this model has implications for intervention. In addition to behavioral activation and cognitive restructuring, which have substantial evidence as treatments for late life depression (reviewed below), interventions that emphasize acceptance rather than personal control, increase flexibility of responses, and combat stereotypes about aging may be effective for certain depressed older adults who present with these vulnerabilities.
In the following sections, we review in more detail factors that are associated with increased risk of depression in late life, including genetic risk, non-genetic biological factors and physical illnesses, anxiety, sleep disturbance, psychological risk factors, and social risk factors, and finally factors shown to buffer those risks. We caution that some evidence is cross-sectional and therefore can only definitively demonstrate that a given factor is a correlate; we indicate in the text where conclusions are based on longitudinal research. Where supported empirically, we include information on factors that moderate the effects of risk and protective factors.
Genetic Risk
Genetic risk seems to express itself most strongly earlier in the lifespan rather than later. Kendler and colleagues used data from a telephone interview with all members of the Swedish Twin Registry to estimate heritability of major depression in twins aged 42 and older (average age at assessment = 56). Heritability was 42% for females and 29% for males, with no difference by birth cohort (Kendler, Gatz, Gardner, & Pedersen, 2006a). Risk of major depression in the co-twin was higher when age of onset was earlier in the depressed twin, with first onset older than age 35 not meaningfully affecting risk of depression for the co-twin (Kendler, Gatz, Gardner, & Pedersen, 2005).
The search for specific genes associated with depression in older adults has encompassed both genes studied in the non-geriatric population and genes that might relate to distinctive aspects of late life depression. Genetic studies in the non-geriatric population have for the most part focused on the short variant of an insertion/deletion polymorphism located in the promoter region of the serotonin transporter gene (5-HTTLPR). In one of the few extensions of this work to older adults, Jansson and colleagues (2003) found a significant effect for the A/A genotype of the 5-HTR2A gene promoter polymorphism and depressed mood for older males but not for older females. In this study, the 5-HTT serotonin transporter gene was not associated with depressed mood.
Interest in identifying genes that might account specifically for late life depression has centered on genes known to be associated with vascular risks, including the ε4 allele of apolipoprotein E (APOE4), which influences lipid metabolism; the insertion/deletion polymorphism of the gene encoding for the angiotensin converter enzyme dipeptidyl carboxypeptidase-1 (DCP-1); the five-repeat polymorphism of the gene encoding for very-low-density lipoprotein-receptor (VLDL-R); and the C677T gene mutation of the methylenetetrahydrofolate reductase enzyme (MTHRF), which may lead to raised plasma homocysteine levels. Of these genes, the most studied is APOE4, an established genetic risk factor for Alzheimer's disease. Despite the plausibility of the association and one report of increased APOE4 frequency in older depressed patients (Krishnan et al., 1996), most subsequent studies have found APOE status to be unrelated to depression in older adults (e.g., Cervilla, Prince, Joels, Russ, & Lovestone, 2004; Hickie et al., 2001; Hwang et al., 2006). Some found depressed APOE4 carriers to have poorer cognitive performance than depressed non-carriers (Hwang et al., 2006; Krishnan et al., 1996), while others found APOE4 unrelated to level of cognitive functioning in depressed older adults (e.g., Hickie et al., 2001). There have been inconsistent findings as to whether having the ε4 allele is related to age of first onset of depression (Krishnan et al., 1996; Hickie et al., 2001; Hwang et al., 2006). Finally, one study reported that APOE4 in depressed older adults was related to history of suicide attempts (Hwang et al., 2006).
With respect to other polymorphisms related to vascular disease, Hickie et al. (2001) found that the MTHFR mutation did not differ between depressed and non-depressed, but that it was significantly more common among late onset (age of onset 50 and older) than early onset (onset before age 50) depression cases. Cervilla et al. (2004) reported that neither VLDL-R nor DCP-1 was associated with late-life depression. No analyses by age of onset were presented.
Biological Risk Factors and Physical Illness
Non-genetic biological risk factors for depression are particularly important in old age, largely because of age-related changes that make them more common in older adults. These biological risks include endocrine, inflammatory or immune, cardiovascular, and neuroanatomical factors. Furthermore, biological status may interact with efficacy of treatment.
It is well established that late life depression frequently occurs in the context of medical illness. Although virtually any serious or chronic condition can produce a depressive reaction, the conditions believed to be most strongly associated with depression include cardiac and cerebrovascular disease and neurological conditions, discussed in more detail below. Depression may also be caused by infections or malignancies. Diabetes has been investigated as a risk factor for depression, although recent research suggests that depression may actually be a risk factor for the development of diabetes.
Depression rates are elevated in hyper- as well as hypothyroidism, suggesting that endocrine dysregulation may cause late life depression (Tiemeier, 2003). Allostatic load, a construct that includes a number of biological variables such as increased adrenocortical activity, elevated insulin growth factor-1, and inflammatory markers, is associated both with accelerated aging on the cellular level and with depression in later life (Alexopoulos, 2005). Late life depression is also associated with bone loss; this may be due to the role of inflammatory markers in both conditions (Alexopoulos, 2005).
Depression may be caused by certain medications (such as beta blockers, CNS medications, calcium channel blockers, digitalis, corticosteroids, hormones, anti-Parkinson agents, respiratory or gastrointestinal medications, certain cancer medications, benzodiazepines and interferon) (Alexopoulos, 2005; Djernes, 2006). Diastolic hypotension is associated with low positive affect, which may explain why depression can be a side effect of certain anti-hypertensive drugs such as beta-blockers (Blazer, 2003).
It is important to note that biological risk factors may interact with psychosocial factors as well as depression itself. Depression in medically ill patients often leads to higher levels of morbidity and disability, although evidence for elevated mortality risk associated with depression is mixed (Charlson & Peterson, 2002). For many physical disorders, experiences related to the disorder such as the demands of managing a chronic disease, functional limitations or pain due to the disease, and vision or hearing loss can provoke a depressive reaction (Djernes, 2006; Vink, Aartsen, & Schoevers, 2008). In turn, depression makes treating the disease more difficult. For example, appetite disturbance secondary to depression is a major cause of weight loss in the elderly, and weight loss is associated with frailty and failure to thrive (Blazer, 2003). Loss of appetite can also lead to compromised nutritional status, and some evidence suggests that nutritional deficiencies may play a role in the development of depression. Low levels of vitamin B12 and the ratio of omega-6 to omega-3 fatty acids appear to be associated with late life depression even after controlling for other risk factors (Tiemeier, 2003).
Not all neurobiological risks have later life origins. For example, depression earlier in life may predispose an individual to late life depression through stress-related hormones leading to reduced secretion of neurotropic factors and decreased neurogenesis (Alexopoulos, 2005). Further, depression earlier in life may be a risk factor for vascular disease, which in turn can increase risk of late life depression. This association suggests that these two disorders may share a common pathological process (Tiemeier, 2003). For example, the serotonin transporter promoter polymorphism 5-HTTLPR associated with depression is also associated with higher platelet factor 4 and beta-thromboglobulin levels, leading to increased platelet activation (Alexopoulos, 2005; Blazer, 2003).
CARDIOVASCULAR DISEASE
Depression is particularly prevalent in cardiovascular disease. Approximately 20-25% of heart disease patients experience major depression, and another 20-25% report symptoms of depression that do not meet criteria for major depressive disorder (Carney & Freedland, 2003). Consequences of depression in heart disease patients include rehospitalization, slower recovery, disability, mortality, and increased health care costs (Krishnan et al., 2002).
Several mechanisms have been proposed for the link between heart disease and depression; these include poor adherence to treatment and lifestyle recommendations; shared genetic influences as described above; dysfunction in the sympathetic, neuroendocrine, autonomic, immune, and inflammatory systems; increased platelet activity; and cerebrovascular disease (Krishnan et al., 2002). One recent large-scale study among patients with coronary heart disease found evidence for genetic influences and poor adherence to medications but no evidence for a link between depression and inflammatory processes (Gehi, Haas, Pipkin, & Whooley, 2005; Otte, McCaffery, Ali, & Whooley, 2007; Whooley et al., 2007).
DIABETES
Prevalence estimates for depression in patients with Type II diabetes are as high as 15% for major depression and approximately 20% for elevated depressive symptoms (Li, Ford, Strine, & Mokdad, 2008). Although conventional wisdom holds that diabetes causes depression, studies have reached discrepant conclusions as to whether impaired glucose metabolism is a risk or protective factor for depression (Golden et al., 2008; Maraldi et al., 2007). Recent prospective research strongly suggests that risk of diabetes is higher in patients with major depressive disorder or elevated depressive symptoms and appears to be independent of health behaviors and other risk factors (Engum, 2007; Golden et al., 2008). Overall, contrary to what is commonly reported, the evidence appears to be stronger for depression as a risk factor for diabetes than the reverse.
DEMENTIA
There is substantial co-morbidity of major depression and dementia, and differential diagnosis is often challenging. Major depression with cognitive impairment was once considered a form of reversible dementia. In fact, cognitive impairment in conjunction with major depression may not completely reverse as the depression abates (e.g., Butters et al., 2000), and individuals who have late onset major depression with cognitive impairment are especially at risk of developing AD, with as many as 40% developing dementia within three to five years (Alexopoulos, 2005; Schweitzer et al., 2002).
Still controversial is whether depression prior to dementia represents a risk factor for dementia or a prodromal feature of dementia (see meta-analyses by Jorm, 2001 and Ownby, Crocco, Acevedo, John, & Loewenstein, 2006). What seems most likely is that depression can be both an early or midlife risk factor for dementia and also an early sign of incipient dementia, with both dementia and depression resulting from the same neuropathological changes. Most studies find that the risk of subsequently developing dementia is greater when there is a shorter interval between the diagnoses of depression and AD (e.g., Green et al., 2003). In another recent report, Geda and colleagues (2006) followed a cohort free of both depression and cognitive impairment. Those who developed depression were more likely subsequently to develop mild cognitive impairment or incident dementia, with the effect stronger for those who did not have a previous history of depression.
Finally, dementia may be a risk factor for depression due to psychological reaction to the cognitive and behavioral changes accompanying dementia. Because depression adds an additional burden to quality of life in demented patients (and their caregivers), it is important to treat.
OTHER NEUROLOGICAL DISORDERS
Rates of major depression are highest among stroke patients (20-25%; Park et al., 2007) and intermediate among those with PD (15-20%; Reijnders, Ehrt, Weber, Aarsland, & Leentjens, 2008), compared to 10-15% among those with AD (Park et al., 2007). Co-morbid depression is associated with functional impairment (e.g., Goodwin & Devanand, 2008). For example, in PD, depressive symptoms increase motor disturbance (Ravina et al., 2007). In addition to evidence indicating that depression often develops in the course of neurological illness, depressive symptoms appear to be a risk factor for incident stroke (Wouts et al., 2008) and PD (Ishiara & Brayne, 2006).
Much attention has been paid to neuroanatomical and chemical changes in the central nervous system as risk factors for depression and as predictors of poor response to treatment. Frontal, basal ganglia, and subcortical white matter lesions may be responsible for the phenomenon of depression-executive dysfunction syndrome (Alexopoulos, 2005; Krishnan, 2002). Structural abnormalities in various brain regions have been observed in depressed older adults (Alexopoulos, 2005; Blazer 2003). Functionally, depression is associated with hypoactivity in cortical structures and hyperactivity in limbic structures, and hypometabolism of the anterior cingulate is associated with treatment resistance (Alexopoulos, 2005). Reduced connectivity between the amygdala and structures in the thalamus and frontal cortex that regulate emotional processing may contribute to the maintenance of late-life depression (Alexopoulos, 2005). Studies have found a reduction in glial cells and neuronal abnormalities associated with late life depression, suggesting possible mechanisms for this decreased connectivity.
In summary, vascular, neuroanatomic, and inflammatory risk factors are associated with depression. These different classes of biological risk factors may furthermore be associated with distinct symptom profiles. Naarding et al. (2005) found vascular risk factors were associated with sleep disturbance, psychomotor change, and loss of energy; neuroanatomic risk factors were associated with psychomotor change and concentration disturbance; and inflammatory risk factors were associated with appetite and sleep disturbance, loss of energy, concentration disturbance, and thoughts of death. Minor depression appears more closely related to inflammatory risk factors than to vascular or degenerative changes.
Anxiety Disorder
As in younger adults, anxiety typically precedes depression (Wetherell, Gatz, & Pedersen, 2001), suggesting that anxiety disorders may be a risk factor for late life depression (Hettema, Kuhn, Prescott, & Kendler, 2006). Estimates of the prevalence of anxiety disorders in older adults with depression are as high as 50% (Beekman et al., 2000; Lenze et al., 2000). Prevalence estimates of depression in older adults with anxiety disorders range from 25% to more than 80% (Beekman et al., 2000; Schoevers, Beekman, Deeg, Jonker, & van Tilburg, 2003).
Late life depression is more severe, persistent, and difficult to treat when combined with anxiety (e.g., Andreescu et al., 2007; Schoevers et al., 2003). Rates of somatic symptoms, disability, and suicide are higher in older adults with anxiety superimposed upon depression than in those with depression alone (Jeste, Hays, & Steffens, 2006; Schoevers et al., 2003). Anxiety may also increase the risk of cognitive decline among older adults with treated depression (DeLuca et al., 2005). The impact of treating anxiety prior to or concurrent with treatment of depression has not been investigated.
Sleep
Sleep disturbance is a risk factor for depression among older adults, with a pooled odds ratio of 2.6 and a population attributable risk of 57.0% demonstrated in a meta-analysis (Cole & Dendukuri, 2003). Insomnia, a type of sleep disturbance, becomes more common with age, affecting a quarter of older men and as much as 40% for women in their 80s (Lichstein, Stone, Nau, McCrae, & Payne, 2006). Previously conceptualized as a symptom of depression, prospective studies have recently shown that insomnia often precedes the onset of depression (Perlis et al., 2006). Among older adults, insomnia is a risk factor for both onset and persistence of depression. Acute insomnia may be conditioned or may be maintained by a person's compensatory behaviors, such that it takes on a chronic course independent of the original precipitating factors. Residual insomnia symptoms often persist after remission of a depressive episode and predict earlier relapse. Promising recent research in a mixed age sample shows that concurrent treatment for comorbid insomnia may enhance effects of depression treatment (Manber et al., 2008).
Psychological Risk Factors
Psychological factors that increase the risk of depression in late life include many of the same characteristics that are related to depression earlier in the lifespan (Nolen-Hoeksema & Ahrens, 2002). High scores on personality scales measuring neuroticism are strongly related to depression in late life. A large part of the relation between neuroticism and depression in middle aged and older adults has been shown to be a function of shared genetic vulnerability, suggesting that neuroticism can be viewed as an index of genetic risk for depression as well as a psychological risk (Kendler, Gatz, Gardner & Pedersen, 2006b).
Both rumination and avoidance are associated with depression across the lifespan. Rumination is an ineffective coping style that involves repeatedly but passively thinking about one's distress. In older adults as well, a ruminative coping style has been associated with depression (Garnefski & Kraaij, 2006). Individuals who endorse a ruminative style benefit more from social support, but report receiving less of it than people who report that they ruminate less (Nolen-Hoeksema & Davis, 1999), presumably because the social support network may be overtaxed.
An avoidant coping style, which has largely been studied with respect to anxiety, has recently been implicated in depression. In an older adult sample, the effect of poor health on depression was stronger among those with higher scores on a measure of experiential avoidance (Andrew & Dulin, 2007).
Social Risk Factors
Social risks such as stressful life events and inadequate social or practical support do not figure as prominently in old age as earlier in the lifespan, although they may increase again in importance in very old age, when individuals are faced with greater losses in the context of fewer resources. Social disadvantage early in life can also have cumulative effects that have renewed importance in later life.
STRESSFUL LIFE EVENTS
The number of stressful life events a person experiences has been associated with depression in late life, as at other ages (Nolen-Hoeksema & Ahrens, 2002), although the relative frequency of different types of events may change with age. Stressful events in late life include such factors as financial difficulties, bereavement, a new physical illness or disability in self or family member, change in living situation, and interpersonal conflict. Retirement is not associated with depression in most older adults, although risk may be elevated for men who retire early, for reasons that remain to be explored (Butterworth et al., 2006). Studies examining recent events suggest that the greatest impact occurs within 6 months, suggesting that most individuals are fairly resilient. Nevertheless, even long-past events contribute to risk.
Long-standing vulnerabilities appear to modify the effects of stressful events on depression in older adults. For example, a variant of the serotonin transporter gene promoter region (s allele of the 5-HTTLPR) is associated with increased risk of depression following hip fracture (Lenze et al., 2005). Cognitive style also influences a person's response to stressful events, and the response appears to vary based on the interaction between cognitive style and type of event. Among older adults with higher scores on a measure of sociotropy (need for close relationships, interpersonal dependency, and a concern about approval), stressful events of an interpersonal nature were most closely associated with depression, whereas among older adults with high scores on an autonomy scale (emphasis on personal control and success), negative events associated with achievement (e.g., loss of long-term residence) were more strongly associated with depression (Mazure, Maciejewski, Jacobs, & Bruce, 2002).
A reciprocal relation between stressful life events and depressive symptoms in older adults has also been demonstrated (Fiske, Gatz & Pedersen, 2003), consistent with the notion that individuals who are depressed behave in ways that increase the likelihood of future stressful events. Although not yet tested, it is conceivable that depressed older adults may be particularly likely to create future problems of an interpersonal nature for themselves (e.g., alienating caregivers), as has been observed among younger depressed individuals (Hammen, 1991). Rumination, which has been linked to decreased social support, may play a role in this process.
A stressful event that occurs with greater frequency as one grows older is bereavement. Depressive symptoms are an expected reaction to loss, but pervasive symptoms lasting more than two months may signify a depressive disorder. Some have proposed that depression associated with bereavement is a distinct syndrome called complicated grief, characterized by symptoms of separation distress and traumatic distress (Prigerson et al., 1995).Others have argued, however, that the similarities between complicated grief and standard major depression outweigh the differences (Zisook & Kendler, 2007).
A meta-analysis of prospective studies of depressive symptoms and disorders in adults aged 50 or older found that bereavement more than tripled the risk of depression, with the largest effect size of any risk factors examined (Cole & Dendukuri, 2003). Even so, bereavement confers less risk of depression for older adults than for middle aged. Older adults are more likely than younger adults to resolve regrets associated with the loss, and such resolution has been linked to better adaptation after the loss (Torges, Stewart & Nolen-Hoeksema, 2008). Compared to women, men are more likely to become depressed following loss of a spouse and to remain depressed longer. This outcome may be due to the fact that the loss of a spouse involves different strains for men and women, reflecting their different roles in the marriage: for widowed women, financial strain is the primary mediator of depressive symptoms, whereas for men, the mediator is primarily household management (Umberson, Wortman & Kessler, 1992).
Providing care for an ill or disabled relative also represents a stressor that is more frequent in late life and may place some individuals at risk for depression. Although high rates of depression among caregivers have been reported, estimates vary widely and elevated rates are largely based on helpseeking samples. A recent population-based study found no differences in depression between caregivers and non-caregivers matched for ethnicity, gender and age (Knight, Flynn Longmire, Dave, Kim, & David, 2007). Aspects of the care recipient's illness are related to depression in the caregiver. Greater risk of depression is found among individuals caring for a person with dementia than among those caring for a person with a physical disability, and greater severity of behavior problems and distress in the care recipient also predict depression in the caregiver (Schulz et al., 2008). Some evidence suggests that the relation between severity of the care recipient's illness and depression in the caregiver may be explained by restriction of the caregiver's normal activities (Williamson & Schaffer, 2000).
PROBLEMS WITH SOCIAL SUPPORT
Deficits in social support, negative aspects of the social network, and even excessive amounts of support have been studied as risk factors for depression in late life, but discerning whether they are cause or effect of depression can be problematic. In particular, troubled relationships may be a factor in explaining late life depression (Nolen-Hoeksema & Ahrens, 2002), including marital conflict, perceived family criticism, and depression in the spouse. Although older adults are less lonely than their younger or middle aged counterparts, loneliness is associated with depression in this age group (Nolen-Hoeksema & Ahrens, 2002). Social support that is perceived as excessive or unhelpful may be a risk factor for depression. Increased levels of depressive symptoms associated with the receipt of social support have been found among older adults with physical limitations who endorsed a greater desire for independence (Martire, Stephens, Druley & Wojno, 2002). Thus, it appears that the quality, not quantity, of social support is important in the development of depression, and the effects of these social variables may vary based on factors associated with both the person and the context.
SOCIOECONOMIC FACTORS
Socioeconomic factors play an important role in late life depression. Deterioration in financial status is among the most frequently-endorsed stressful life events experienced by older adults (Fiske, Gatz & Pedersen, 2003). Older adults who are economically disadvantaged are more likely to experience persistent depressive symptoms (Mojtabai & Olfson, 2004), consistent with the chronic nature of the stressors associated with low income, including financial strain and exposure to unsafe and unstable environments. Practical issues such as these may also complicate treatment for those low income older adults who are depressed (Areán et al., 2005). In addition, socioeconomic disadvantage early in life may increase vulnerability to depression throughout the lifespan through the effects of poor nutrition, reduced opportunities for education, less access to health care, or other mechanisms. The effects of early disadvantage may become even more consequential with age, as economic and health disparities are compounded.
Protective Factors
Since most older adults experience disability, bereavement, or other stressful events in late life, and since most older adults have age-related changes in immune, neurological, and other biological systems, it is of considerable interest to know why most older adults do not experience depression. Of special interest would be to study individuals with early onset depression that did not persist into late life. There is, however, extensive research on psychological and social factors that appear to buffer against depression or depressive symptoms in the context of stressful events and biological risks (see review by Hendrie et al., 2006). Three themes emerge from that review and others: (a) the importance of resources—health, cognitive function, socioeconomic status; (b) the idea that the life experiences of older adults have taught them psychological strategies and ways to use social support to manage their health-related stresses; and (c) the role of meaningful engagement, whether in social activities, volunteer work, or religion.
Improvements in emotion regulation with age appear to play an important role in protecting against depression in older adults. Experiencing negative affect declines with age, with the lowest scores seen in older adults (Charles, Reynolds, & Gatz, 2001). Older adults are less reactive to stressors, particularly those of an interpersonal nature, than are younger adults (Neupert, Almeida, & Charles, 2007). When compared to younger adults with the same number of chronic health conditions, older adults endorsed less negative affect and demonstrated less reactivity to daily stressors than did younger adults (with the exception that older adults with the greatest number of illnesses displayed the same level of reactivity as younger adults; Piazza, Charles, & Almeida, 2007). Similiarly, older adults experienced less affective reactivity in response to a cognitive challenge task than did younger adults (Chow, Hamagami, & Nesselroade, 2007).
Older adults are as likely as younger and middle aged adults to report engaging in the cognitive strategy of positive reappraisal, which is associated with decreased depressive symptoms across age groups, and more likely to report putting into perspective, a cognitive strategy linked to lower depressive symptom scores only in the elderly (Garnefski & Kraaij, 2006). Older adults have been shown to focus more on positive and emotionally meaningful experiences than do younger adults, also suggesting better emotion regulation with aging (Carstensen, Fung, & Charles, 2003).
Other psychological factors associated with resiliency in late life include a positive self-concept, a sense of mastery or self-efficacy. Although these factors are often conceptualized as moderators, in a longitudinal analysis, sense of control and self-esteem were found to mediate the relation between functional disability and depressive symptoms. That is, disability was associated with decreases in mastery and self-efficacy, which were associated with increases in depressive symptom scores. The effects were large, accounting for 53% of the effect of baseline functional disability on depressive symptoms, and 43% of the effect of change in disability on change in depressive symptoms (Yang, 2006). Disability may lead directly to a reduction in a person's appraised ability to achieve goals, but it is also possible that individuals reduce their activities when disability makes it difficult to continue them, and the lack of regular engagement in activities leads to decrements in skills and associated lack of self-efficacy.
Whereas activity restriction is associated with increased levels of depression among older adults with functional impairment (Williamson & Shaffer, 2000), replacement of lost activities can lead to a normalization of depressive symptoms, but only satisfactory replacement activities have this effect (Benjamini & Lomranz, 2004). Whether proactive efforts to replace lost activities can protect against the onset of a depressive episode remains to be examined.
The preponderance of evidence indicates that perceived social support buffers the effect of stressful events in older adults. One way in which social support may help is through encouraging a person to engage in meaningful activities. As discussed above, delivery of social support must be tailored to the individual or may inadvertently lead to negative effects.
Religious involvement, which is more frequently endorsed by older adults than other age groups, may also reduce the risk of depression in this age group (George, Ellison & Larson, 2002). Effects are not entirely explained by social factors, and may reflect an increased sense of meaning in one's life or other variables yet to be fully examined.
Factors thought to buffer the effects of biological vulnerability to depression in late life have received less attention, but some recent work has examined physical exercise, stress reduction strategies, and hormone replacement therapy. Engaging in active behaviors to overcome health problems, referred to as health engagement control strategies, is associated not only with reduced levels of depressive symptoms, but also reduced secretion of the stress hormone cortisol (Wrosch, Schulz, Miller, Lupien & Dunne, 2007). Efforts to promote vascular health may also protect against late life depression associated with vascular risk factors, though prevention trials would be required to examine this question.
SUICIDE
A particularly tragic potential outcome of depression in late life is suicide. Although research in mixed age samples indicates that only four percent of individuals with an inpatient admission for depression will die by suicide (Bostwick & Pankratz, 2000), most people who do die by suicide were depressed. Furthermore, suicide among older adults is more likely to be associated with depression than suicide at any other age (Conwell & Brent, 1996). This fact is particularly troubling since depression can be effectively treated in late life (as we discuss below).
Suicide rates in most countries and cultures are 3-4 times higher among men than women at all ages, but the differential increases in late life due to a dramatic increase in risk for men and a slight decrease for women compared to midlife (Kung, Hoyert, Xu, & Murphy, 2008). Suicide rates vary by ethnicity, with highest risk in the U.S. for whites and Native Americans and lowest risk for Latinos. In recent years, however, an increase in risk has been observed for African American men in late life. Rates of suicide among older adults have been declining in the past decade. It is too early to determine whether the effect is due to prevention activities, such as increased use of antidepressant medication in this age group, or other trends that remain to be identified.
Suicidal behavior in late life differs in several ways from that observed earlier in the lifespan. Older adults tend to use more immediately lethal means, and suicidal behavior is more likely to be fatal among older adults than at any other age. In addition, the suicidal deaths of older adults reflect a higher level of intent and more planning compared to their younger counterparts (Conwell et al., 1998). Older adults are less likely to verbalize suicidal thoughts compared to younger or middle aged adults. In contrast, older adults have been reported to have higher rates of death ideation, such as a passive wish to die. A final important difference between older adults who are suicidal and their younger counterparts is that older adults are particularly likely to visit a physician shortly before the death (Luoma, Martin, & Pearson, 2002). Among adults who died by suicide at age 55 or older, up to 70% visited a primary care provider within a month of the death.
The predominant risk factor for suicide in late life is depression, which is present in approximately 85% of older adults who died by suicide (Conwell & Brent, 1996). Physical illnesses, including cancer, seizure disorder, chronic pulmonary disorder, renal failure, vision or hearing impairment, and even incontinence have also been associated with increased risk of suicide in late life, with effects partially but not fully explained by depression (Fiske, O'Riley & Widoe, 2008). Personality characteristics have also been associated with suicidal behavior in late life, including high scores on neuroticism scales and low scores on an openness to experience scale (Duberstein et al., 2000). Several investigators have suggested that a rigid personality style, as reflected by low openness to experience, may increase risk for suicide particularly in interaction with the types of events older adults are likely to experience, such as functional impairment and other challenges (Duberstein et al., 2000). Alcohol abuse increases risk for suicide among older adults. Consistent with the high rates of depression found in long term care, the prospect of impending placement in a skilled nursing facility was identified as a risk factor for suicide in one study (Loebel, Loebel, Dager & Centerwall, 1991). Several approaches to preventing suicide among older adults, mostly involving the identification and treatment of depression, have demonstrated effectiveness (see Prevention section below).
TREATMENTS
Evidence Based Treatments
A substantial body of evidence supports the use of various forms of psychotherapy as well as somatic treatments in the treatment of depression in older adults. With respect to pharmacologic treatments, randomized clinical trials with depressed older adults have demonstrated similar efficacy for selective serotonin re-uptake inhibitors, tricyclic antidepressants and monoamine oxidase inhibitors, with moderate to large effect sizes (for a review, see Beyer, 2007). Prognosis for older adults is equivalent to that for middle aged adults. Treatment efficacy has been observed in older adults with medical comorbidities. Among older adults with cognitive impairment, only those with impaired executive functioning have been shown to respond more poorly than do younger adults.
A number of psychological treatments for depression in late life meet evidence-based criteria (see Table 1). Most of these treatments have a behavioral activation component, which directly addresses the problem of activity limitation; some focus on meaningfulness of the activity; others target the cognitions that may intensify and maintain a depressive episode (see Figure 2). These interventions include behavioral therapy, cognitive behavioral therapy, cognitive bibliotherapy, problem-solving therapy, brief psychodynamic therapy and life review therapy (Scogin, Welsh, Hanson, Stump, & Coates, 2005). These manualized treatments have all been to some extent adapted for older adults. Life review therapy, which was developed specifically for use with older adults, differs from reminiscence activities more broadly in that it is a structured therapy that has been empirically evaluated. For all of these interventions, moderate to large effect sizes are seen in randomized controlled trials. Treatments that combine empirically supported psychological elements with a focus on accessing community resources to address practical problems may be more effective than either approach alone (Areán et al., 2005). Promising treatments that have not yet been extensively evaluated in older adults include mindfulness-based psychotherapies such as acceptance and commitment therapy (Hayes, Strosahl, & Wilson, 1999), and mindfulness-based cognitive therapy (Segal, Williams, Teasdale, & Kabat-Zinn, 2001). Mindfulness-based approaches involve teaching clients to be aware of and to accept their thoughts and feelings, rather than engaging in either avoidance or rumination. To the extent that this process results in a reduction in negative affect, through distancing from negative thoughts and feelings, it would interrupt the negative feedback loop depicted in Figure 2.
Table 1.
Psychological Interventions for Depression in Late Life
|
Evidence Based Interventions Behavioral therapy Cognitive behavioral therapy Cognitive bibliotherapy Problem solving therapy Brief psychodynamic therapy Life review therapy |
|
Promising Interventions Interpersonal therapy (IPT)a Clinical case managementb Personal construct therapyb Coping Together group therapyb Interpersonal counselingb Behavioral bibliotherapyb Goal-focused therapyb |
|
Evidence Based Interventions for Caregivers Cognitive behavioral therapy Multi-component interventions |
|
Evidence Based Interventions for Persons with Dementia Behavioral therapy Social engagement approaches Sensory/environmental approaches |
Efficacy has been demonstrated for continuation treatment of older adult patients who responded to acute treatment with pharmacotherapy or pharmacotherapy + IPT.
Efficacy has been demonstrated by only one study or only one set of investigators.
In the few studies that compare pharmacological and psychologial interventions, effect sizes are comparable and may favor psychotherapy (Pinquart, Duberstein & Lyness, 2006). In practice, empirically-supported psychological treatments are often combined with pharmacological interventions, but research on combined treatment lags behind practice.
Electroconvulsive therapy (ECT), an evidence-based treatment alternative for depression, is used more often in older adults than in any other age group (Kelly & Zisselman, 2000). Treatment efficacy is impressive, with improvement seen in more than 80% of patients in most trials, but adverse events such as cardiac complications, memory loss, and delirium, suggest caution in the use of ECT for older adults. Cognitive effects are transient in most but not all cases.
Cognitive changes complicate treatment options. For example, some research shows poorer response to pharmacotherapy for older adults with white matter hyperintensities on neuroimaging (Taylor et al., 2003), and cognitive-behavioral material may need to be simplified. Yet depression in the context of dementia is amenable to treatment and should be treated. Consensus guidelines describe the outcomes associated with pharmacotherapy as mixed, but recommend antidepressant medications for significant and persistent depressive symptoms (American Psychiatric Association, 2007). There is substantial evidence of efficacy for psychosocial treatments, including behavioral and social engagement approaches (Teri, McKenzie & LaFazia, 2005). Focus on the caregiver appears to be an important component of behavioral treatment, involving improvement in the caregiver's skills in communicating with the patient and adapting to the disease. Caregivers are instrumental in increasing the patient's engagement in pleasant activities. Both cognitive behavioral and multi-component treatment approaches are effective in reducing depression in the caregiver (Gallagher-Thompson & Coon, 2007).
In summary, the evidence clearly shows that there are multiple therapeutic alternatives, including somatic and psychotherapeutic approaches, each with demonstrable efficacy for treating depression in late life. Because depression in late life, even at subsyndromal levels, is associated with increased physical impairment (Judd et al., 2002), treatment of depression may provide an opportunity to improve physical function. Clinical trials of depression interventions for older adults have begun to evaluate functioning as an outcome measure. As yet, few studies have considered how individual differences may modify the efficacy of treatments.
Unfortunately, a large proportion of older adults with depression do not receive treatment of any kind, although recent research shows a positive trend (Blazer, Hybels, Fillenbaum, & Pieper, 2005). Lack of treatment among older adults may reflect, in part, the difficulty of detecting depression in older adults, due to age-associated differences in presentation described above. Because depressed older adults are more likely to seek care from a primary care provider than in the specialty mental health sector (Uebelacker, Wang, Berglund, & Kessler, 2006), collaborative care models have been developed, in which pharmacological and psychological treatments are delivered in primary care settings (Bruce et al., 2004; Unützer et al., 2002) or in the patient's home (Ciechanowski et al., 2004), supervised by a depression care manager. Studies have shown greater improvement, including reduced suicidal ideation, compared to management of depression treatment by the primary care physician alone. These favorable outcomes may be largely attributable to reduced dropout rates when psychological services are co-located in medical settings, highlighting the importance of access to psychological services for depressed older adults (Bartels et al., 2004).
The model of depression held by the depressed older adult and by the general practitioner may also affect whether treatment is sought, whether treatment is offered, and whether there is adherence to the program of treatment. Based on work with mixed aged depression patients, it is recommended that primary care physicians assess the patients' beliefs about depression and provide education about the role of life stressors in causing depression and the importance of activation to recovery (Brown et al., 2007). Moreover education about behavioral explanations for depression is generally more effective than education about biomedical explanations (Lam, Salkovskis, & Warwick, 2005). With older adults, however, it is important not to over-emphasize the role of life stressors in such a way that depression is normalized by older adult patients or their physicians. Rather the importance of behavioral disengagement and self-blame as contributing to depression as well as any biological risk factors that may interact with the psychosocial context need to be addressed.
New treatments
Repetitive transcranial magnetic stimulation (rTMS), a technique in which rapidly changing magnetic fields are used to induce electrical currents in the brain, was not more effective than sham stimulation in two studies of older adults with treatment-resistant depression of diverse etiologies (Manes et al., 2001; Mosimann et al., 2004), but appears to be effective relative to sham treatment for poststroke and vascular depression (Jorge et al., 2004; Jorge, Moser, Acion, & Robinson, 2008), and as effective as fluoxetine for depression in Parkinson's disease (Fregni et al., 2004). Although age did not appear to influence results in the poststroke sample, older patients in the vascular depression group showed poorer response. Across studies, smaller frontal lobe volume was associated with poorer response.
Some research suggests the efficacy of aerobic exercise as a complementary or alternative treatment for depression among older adults (Sjösten & Kivelä, 2006). Weight training may also have an antidepressant effect (Singh et al., 2005). Exercise has been shown to be as effective as antidepressant SSRI medication (specifically, sertraline) and more effective than attention placebos such as health lectures or supportive contact for depressed older adults (Barbour & Blumenthal, 2005). Exercise is effective even in older people with medication-resistant depression, post-stroke depression, and in those with depressive symptoms as well as major depression (Barbour & Blumenthal, 2005; Sjösten & Kivela, 2006). Studies with long-term follow-up have found lower relapse rates over as long as five years for those who continue to exercise (Motl et al., 2005).
This literature has been criticized for poor quality methodology, including failure to adequately describe the randomization concealment method and blinding procedure, small samples, and poor data analytic techniques (Sjösten & Kivela, 2006). These flaws do not appear sufficient to justify disregarding this important body of work. A more serious concern is that depression itself may reduce the appeal of exercise, and therefore the samples recruited for exercise studies may be highly selected and unrepresentative of depressed older adults. Overall, however, exercise appears to be an efficacious treatment for late life depression, with additional important benefits for health in later life.
PREVENTION
Prevention efforts may aim to prevent a first onset, a recurrence in late life, or a relapse following treatment. Since over half of older adults with depression have the first onset in late life, it is as appropriate to design prevention efforts targeting first onsets in this age group as at earlier ages.
Preventive efforts are often targeted at those who are at increased risk of disorder. The most promising preventive approach may be treating older adults with subsyndromal depressive symptoms in order to prevent full-blown disorder. In the Amsterdam Study of the Elderly, the authors calculated that only 5.8 older adults with subsyndromal depressive symptoms needed to be treated in order to prevent one depression onset within three years, and that treatment of all patients with subsyndromal depressive symptoms could prevent 24.6% of new depression onsets in that period (Schoevers et al., 2006).
The treatment of comorbid insomnia or other sleep disturbance may represent a particularly valuable opportunity to prevent future depressive episodes in older adults (Cole & Dendukuri, 2003), as insomnia symptoms are a known risk factor for future depressive episodes. Fortunately, cognitive behavioral treatments for insomnia in this age group are highly effective, even among individuals with secondary insomnia and those who are dependent on sleep medications (Nau, McCrae, Cook & Lichstein, 2005).
Other prevention interventions target older adults at risk of depression due to physical illness and disability, bereavement and caregiver status. Interventions that have the most empirical support include individual therapy for at-risk bereaved older adults, educational interventions for subjects with chronic illness, cognitive-behavioral interventions to reduce negative thinking, and life review (reviewed by Cole, 2008). Stroke patients who preventively receive antidepressant medication are less likely to become depressed than those who received placebo (Whyte, Mulsant, Rovner, & Reynolds, 2006). Promising strategies for caregivers of ill or disabled persons include group support and skills training. Because depression in this group is strongly associated with restriction of activities, behavioral activation may be a particularly appropriate preventive intervention. Given the association of loneliness to depression among older adults, programs to reduce social isolation may be of benefit. A telephone support and emergency response program that serves a large number of isolated older adults in Italy, many of whom were in frail health, found that suicide rates over a ten year period were lower than expected, suggesting that a reduction of depressive symptoms may have occurred (DeLeo, Dello Buono, & Dwyer, 2002).
Prevention strategies may also be used to reduce the risk of adverse outcomes of depression in older adults. Screening for suicide risk among older adults with depression, followed by effective depression treatment, reduces suicidal thoughts (Bruce et al., 2004) and may, therefore, reduce risk of suicidal behaviors.
Approaches not targeted according to identified risk factors may also be helpful, including programs that educate professional and lay audiences regarding recognition of depression in older adults, stressing particularly that depression is not a normal part of aging. In an important study that has since been replicated in several other locales, all the primary care physicians on the island of Gotland, Sweden, were trained to detect and respond to depression (Rutz, von Knorring, & Wålinder, 1992). Rates of diagnosed depression subsequently increased, and rates of suicide decreased. Such training may be particularly helpful in long term care settings, where high rates of depression may obscure the reality that depression is not inevitable—nor even the norm—in this age group. High rates of depression in skilled nursing facilities could also be taken as a sign that environmental changes are necessary (Zeiss, 2005).
CONCLUSIONS
Empirical literature converges to support that conclusion that depression is not a normal part of aging. Depression is less common in late life than in midlife, except in a more delimited form. Although late life depression is often less severe, the consequences can be devastating.
Depression in older adults can be understood from a lifespan developmental diathesis-stress perspective. Risk and protective factors become more or less prominent in the etiology of depression as they change in frequency or importance over the course of the life span. Biological risks become dramatically more prevalent in late life, as do certain life events, whereas psychological vulnerability decreases and psychological resilience increases. Considering the biological and social challenges associated with older adulthood, the fact that depressive disorders become less rather than more prevalent in this age group is evidence of the importance of protective factors.
The etiological picture of depression in late life is complex. Late life depression is characterized by heterogeneity, with age of first onset a likely marker of etiological differences. Early-onset depression is influenced by genes for depression, whereas late onset may represent either a prodrome of dementia or a biological or psychological response to the events that are more common in late life (e.g., physical illness, bereavement, caregiving). Comorbidity is particularly common in late life depression, rising from probable biological, psychological and social mechanisms.
There is substantial consensus regarding broad categories of risk factors for late life depression, which include most prominently neurological vulnerability, physical illness and disability, and stressful life events such as bereavement and caregiving. Research is only beginning to examine interactions between these risk factors. As the evidence regarding risk and protective factors accumulates, the design and testing of novel preventive approaches becomes possible. [10,545 words]
Summary Points.
Depression is less prevalent among older adults than younger adults, but merits special attention because it can have serious negative consequences, including increased burden of physical illness, impaired functioning, and risk of suicide. More than half of depressed older adults had the first episode after age 60.
The presentation of depression differs in older adults compared to younger adults. Older adults are less likely to endorse affective symptoms and more likely to display cognitive changes, somatic symptoms, and loss of interest than are younger adults.
Factors leading to the development of late life depression likely comprise complex interactions of genetic vulnerabilities, cognitive diathesis, and age-associated neurobiological changes with the particular types of stressful events that occur more often in late life.
A common pathway to depression in older adults, regardless of whether predisposing risks are biological, psychological, or social, may be curtailment of daily activities. Accompanying self-critical thinking may exacerbate and maintain a depressed state.
Age-related increases in psychological strengths, and reductions in psychological vulnerabilities, offset the increasing prevalence of certain risk factors in late life. Other protective factors include higher education and socioeconomic status, good health and cognitive function, engagement in valued activities, and religious involvement.
Depression in late life is treatable, even among older adults with dementia. Empirical evidence indicates that behavioral therapy, cognitive behavioral therapy, cognitive bibliotherapy, problem-solving therapy, brief psychodynamic therapy, and life review/reminiscence therapy are effective but too infrequently used with older adults. Specialized, evidence-based approaches have been developed for individuals with dementia and for caregivers.
Emerging evidence supports the use of psychological and somatic interventions to prevent the onset of depression in late life, including cognitive and behavioral interventions for bereaved older adults, individuals with chronic illnesses and caregivers, and prophylactic antidepressant treatment in individuals who have had a stroke. The adequate treatment of residual symptoms following an acute depressive episode, including insomnia symptoms, may prevent relapse.
Acknowledgments
The authors wish to thank Merideth D. Smith for assistance in preparing the figures.
Supported by grants from the National Institute of Mental Health (R15-MH80399) and the National Institute on Aging (R01-AG10175 and P50-AG05142).
Acronyms
- AD
Alzheimer's disease
- APOE
Apolipoprotein epsilon
- CNS
central nervous system
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ECT
electroconvulsive therapy
- PD
Parkinson's disease
- rTMS
repetitive transcranial magnetic stimulation
- SSRI
selective serotonin reuptake inhibitor
References
- Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual for Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- American Psychiatric Association (APA) Practice guideline for the treatment of patients with Alzheimer's disease and other dementias. American Psychiatric Association; Arlington (VA): 2007. Accessed at http://www.guideline.gov/summary/summary.aspx?doc_id=11533. [PubMed] [Google Scholar]
- Andreescu C, Lenze EJ, Dew MA, Begley AE, Mulsant BH, et al. Effect of comorbid anxiety on treatment response and relapse risk in late-life depression: controlled study. Br. J. Psychiatry. 2007;190:344–9. doi: 10.1192/bjp.bp.106.027169. [DOI] [PubMed] [Google Scholar]
- Andrew DH, Dulin PL. The relationship between self-reported health and mental health problems among older adults in New Zealand: Experiential avoidance as a moderator. Aging Ment. Health. 2007;11:596–603. doi: 10.1080/13607860601086587. [DOI] [PubMed] [Google Scholar]
- Areán PA, Gum A, McCulloch CE, Bostrom A, Gallagher-Thompson D, Thompson L. Treatment of depression in low-income older adults. Psychol. Aging. 2005;20:601–9. doi: 10.1037/0882-7974.20.4.601. [DOI] [PubMed] [Google Scholar]
- Barbour KA, Blumenthal JA. Exercise training and depression in older adults. Neurobiol. Aging. 2005;26(Suppl 1):119–23. doi: 10.1016/j.neurobiolaging.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Coakley EH, Zubritzky C, Ware JH, Miles KM, et al. Improving access to geriatric mental health services: A randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at risk alcohol use. Am. J. Psychiatry. 2004;161:1455–62. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- Beekman AT, de Beurs E, van Balkom AJ, Deeg DJ, van Dyck R, van Tilburg W. Anxiety and depression in later life: Co-occurrence and communality of risk factors. Am. J. Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Lomranz J. The relationship of activity restriction and replacement with depressive symptoms among older adults. Psychol. Aging. 2004;19:362–6. doi: 10.1037/0882-7974.19.2.362. [DOI] [PubMed] [Google Scholar]
- Beyer JL. Managing depression in geriatric populations. Ann. Clin. Psychiatry. 2007;19:221–28. doi: 10.1080/10401230701653245. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: Review and commentary. J. Gerontol. A Biol. Sci. Med. Sci. 2003;58:249–65. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Hybels CF, Fillenbaum GG, Pieper CF. Predictors of antidepressant use among older adults: Have they changed over time? Am. J. Psychiatry. 2005;162:705–10. doi: 10.1176/appi.ajp.162.4.705. [DOI] [PubMed] [Google Scholar]
- Blumstein T, Benyamini Y, Fuchs Z, Shapira Z, Novikov I, et al. The effect of a communal lifestyle on depressive symptoms in late life. J. Aging Health. 2004;16:151–74. doi: 10.1177/0898264303262650. [DOI] [PubMed] [Google Scholar]
- Bostwick JM, Pankratz VS. Affective disorders and suicide risk: A reexamination. Am. J. Psychiatry. 2000;157:1925–32. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- Brodaty H, Luscombe G, Parker G, Wilhelm K, Hickie I, et al. Early and late onset depression in old age: Different aetologies, same phenomenology. J. Affect. Disord. 2001;66:225–36. doi: 10.1016/s0165-0327(00)00317-7. [DOI] [PubMed] [Google Scholar]
- Brown C, Battista DR, Sereika SM, Bruehlman RD, Dunbar-Jacob J, Thase ME. Primary care patients' personal illness models for depression: Relationship to coping behavior and functional disability. Gen. Hosp. Psychiatry. 2007;29:492–500. doi: 10.1016/j.genhosppsych.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce ML, McAvay GJ, Raue PJ, Brown EL, Meyers BS, et al. Major depression in elderly home health care patients. Am. J. Psychiatry. 2002;159:1367–74. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- Bruce ML, Ten Have TR, Reynolds CF, III, Katz IR, Schulberg HC, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA. 2004;291:1081–91. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- Butters MA, Becker JT, Nebes RD, Zmuda MD, Mulsant BH, et al. Changes in cognitive functioning following treatment of late life depression. Am. J. Psychiatry. 2000;157:1949–54. doi: 10.1176/appi.ajp.157.12.1949. [DOI] [PubMed] [Google Scholar]
- Butters MA, Whyte EM, Nebes RD, Begley AE, Dew MA, et al. The nature and determinants of neuropsychological functioning in late-life depression. Arch. Gen. Psychiatry. 2004;61:587–95. doi: 10.1001/archpsyc.61.6.587. [DOI] [PubMed] [Google Scholar]
- Butterworth P, Gill SC, Rodgers B, Anstey KJ, Villamil E, Melzer D. Retirement and mental health: Analysis of the Australian national survey of mental health and well-being. Soc. Sci. Med. 2006;62:1179–91. doi: 10.1016/j.socscimed.2005.07.013. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol. Psychiatry. 2003;54:241–7. doi: 10.1016/s0006-3223(03)00111-2. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Fung HH, Charles ST. Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion. 2003;27:103–23. [Google Scholar]
- Cervilla J, Prince M, Joels S, Russ C, Lovestone S. Genes related to vascular disease (APOE, VLDL-R, DCP-1) and other vascular factors in late-life depression. Am. J. Geriatr. Psychiatry. 2004;12:202–10. [PubMed] [Google Scholar]
- Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. J. Pers. Soc. Psychol. 2001;80:136–51. [PubMed] [Google Scholar]
- Charlson M, Peterson JC. Medical comorbidity and late life depression: What is known and what are the unmet needs? Biol. Psychiatry. 2002;52:226–35. doi: 10.1016/s0006-3223(02)01422-1. [DOI] [PubMed] [Google Scholar]
- Chow SM, Hamagami F, Nesselroade JR. Age differences in dynamical emotion-cognition linkages. Psychol Aging. 2007;22:765–80. doi: 10.1037/0882-7974.22.4.765. [DOI] [PubMed] [Google Scholar]
- Christensen H, Jorm AF, Mackinnon AJ, Korten AE, Jacomb PA, et al. Age differences in depression and anxiety symptoms: A structural equation modelling analysis of data from a general population sample. Psychol. Med. 1999;29:325–39. doi: 10.1017/s0033291798008150. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, et al. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA. 2004;291:1569–77. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. Am. J. Psychiatry. 2003;160:1147–56. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- Cole MG. Brief interventions to prevent depression in older subjects: A systematic review of feasibility and effectiveness. Am. J. Geriatr. Psychiatry. 2008;16:435–43. doi: 10.1097/JGP.0b013e318162f174. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Brent D. Suicide and aging I: Patterns of psychiatric diagnosis. In: Pearson JL, Conwell Y, editors. Suicide: International Perspectives. Springer; New York: 1996. pp. 15–30. [Google Scholar]
- Conwell Y, Duberstein PR, Cox C, Hermann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am. J. Geriatr. Psychiatry. 1998;6:122–6. [PubMed] [Google Scholar]
- De Leo D, Dello Buono M, Dwyer J. Suicide among the elderly: The long-term impact of a telephone support and assessment intervention in northern Italy. Br. J. Psychiatry. 2002;181:226–9. doi: 10.1192/bjp.181.3.226. [DOI] [PubMed] [Google Scholar]
- DeLuca AK, Lenze EJ, Mulsant BH, Butters MA, Karp JF, et al. Comorbid anxiety disorder in late life depression: Association with memory decline over four years. Int. J. Geriatr. Psychiatry. 2005;20:848–54. doi: 10.1002/gps.1366. [DOI] [PubMed] [Google Scholar]
- Djernes JK. Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatr. Scand. 2006;113:372–87. doi: 10.1111/j.1600-0447.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Seidlitz L, Denning D, Cox C, Caine ED. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000;55:18–26. doi: 10.1093/geronb/55.1.p18. [DOI] [PubMed] [Google Scholar]
- Ehrt U, Brønnick K, Leentjens AF, Larsen JP, Aarsland D. Depressive symptom profile in Parkinson's disease: A comparison with depression in elderly patients without Parkinson's disease. Int. J. Geriatr. Psychiatry. 2006;21:252–8. doi: 10.1002/gps.1456. [DOI] [PubMed] [Google Scholar]
- Engum A. The role of depression and anxiety in onset of diabetes in a large population-based study. J. Psychosom. Res. 2007;62:31–8. doi: 10.1016/j.jpsychores.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Fiske A, Gatz M, Pedersen NL. Depressive symptoms and aging: The effects of illness and non-health related events. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003;58:P320–8. doi: 10.1093/geronb/58.6.p320. [DOI] [PubMed] [Google Scholar]
- Fiske A, O'Riley AA, Widoe RK. Physical health and suicide in late life. Clin. Gerontol. 2008;31:31–50. [Google Scholar]
- Fregni F, Santos CM, Myczkowski ML, Rigolino R, Gallucci-Neto J, et al. Repetitive transcranial magnetic stimulation is as effective as fluoxetine in the treatment of depression in patients with Parkinson's disease. J. Neurol. Neurosurg. Psychiatry. 2004;75:1171–4. doi: 10.1136/jnnp.2003.027060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol. Aging. 2007;22:37–51. doi: 10.1037/0882-7974.22.1.37. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Anthony JC, Muthén BO. Age differences in the symptoms of depression: A latent trait analysis. J. Gerontol. 1994;49:P251–64. doi: 10.1093/geronj/49.6.p251. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Cooper-Patrick L, Lesikar S. Depressive symptoms of whites and African Americans aged 60 years and older. J. Gerontol. B Psychol. Sci. Soc. Sci. 1998;53:P277–86. doi: 10.1093/geronb/53b.5.p277. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Rabins PV, Lyketsos CG, Tien AY, Anthony JC. Depression without sadness: Functional outcomes of nondysphoric depression in later life. J. Am. Geriatr. Soc. 1997;45:570–8. doi: 10.1111/j.1532-5415.1997.tb03089.x. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Pers. Individ. Dif. 2006;40:1659–69. [Google Scholar]
- Geda YE, Knopman DS, Mrazek DA, Jicha GA, Smith GE, et al. Depression, apolipoprotein E genotype, and the incidence of mild cognitive impairment: a prospective cohort study. Arch. Neurol. 2006;63:435–40. doi: 10.1001/archneur.63.3.435. [DOI] [PubMed] [Google Scholar]
- Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: Findings from the Heart and Soul Study. Arhc. Intern. Med. 2005;165:2508–13. doi: 10.1001/archinte.165.21.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George LK, Ellison CG, Larson DB. Explaining the relationships between religious involvement and health. Psychol. Inq. 2002;13:190–200. [Google Scholar]
- Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–9. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Devanand DP. Stroke, depression, and functional health outcomes among adults in the community. J. Geriatr. Psychiatry Neurol. 2008;21:41–6. doi: 10.1177/0891988707311041. [DOI] [PubMed] [Google Scholar]
- Green RC, Cupples LA, Kurz A, Auerbach S, Go R, et al. Depression as a risk factor for Alzheimer disease: the MIRAGE Study. Arch. Neurol. 2003;60:753–9. doi: 10.1001/archneur.60.5.753. [DOI] [PubMed] [Google Scholar]
- Hammen CL. The generation of stress in the course of unipolar depression. J. Abnorm. Psychol. 1991;100:555–61. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch. Gen.Psychiatr. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. Guilford Press; New York: 1999. [Google Scholar]
- Hendrie HC, Albert MS, Butters MA, Gao S, Knopman DS, et al. The NIH Cognitive and Emotional Health Project: Report of the Critical Evaluation Study Committee. Alzheimers Dement. 2006;2:12–32. doi: 10.1016/j.jalz.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Kuhn JW, Prescott CA, Kendler KS. The impact of generalized anxiety disorder and stressful life events on risk for major depressive episodes. Psychol. Med. 2006;36:789–95. doi: 10.1017/S0033291706007367. [DOI] [PubMed] [Google Scholar]
- Heun R, Papassotiropoulos A, Jessen F, Maier W, Breitner JC. A family study of Alzheimer disease and early- and late-onset depression in elderly patients. Arch. Gen. Psychiatry. 2001;58:190–6. doi: 10.1001/archpsyc.58.2.190. [DOI] [PubMed] [Google Scholar]
- Hickie I, Scott E, Naismith S, Ward P, Turner K, et al. Late-onset depression: Genetic, vascular and clinical contributions. Psychol. Med. 2001;31:1403–12. doi: 10.1017/s0033291701004731. [DOI] [PubMed] [Google Scholar]
- Hwang JP, Yang CH, Hong CJ, Lirng JF, Yang YM, Tsai SJ. Association of APOE genetic polymorphism with cognitive function and suicide history in geriatric depression. Dement. Geriatr. Cogn. Disord. 2006;22:334–8. doi: 10.1159/000095599. [DOI] [PubMed] [Google Scholar]
- Ishihara L, Brayne C. A systematic review of depression and mental illness preceding Parkinson's disease. Acta Neurol. Scand. 2006;113:211–20. doi: 10.1111/j.1600-0404.2006.00579.x. [DOI] [PubMed] [Google Scholar]
- Jansson M, Gatz M, Berg S, Johansson B, Malmberg B, et al. Association between depressed mood in the elderly and a 5-HTR2A gene variant. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2003;120B:79–84. doi: 10.1002/ajmg.b.20016. [DOI] [PubMed] [Google Scholar]
- Jeste ND, Hays JC, Steffens DC. Clinical correlates of anxious depression among elderly patients with depression. J. Affect. Disord. 2006;90:37–41. doi: 10.1016/j.jad.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Jorge RE, Moser DJ, Acion L, Robinson RG. Treatment of vascular depression using repetitive transcranial magnetic stimulation. Arch. Gen. Psychiatry. 2008;65:268–76. doi: 10.1001/archgenpsychiatry.2007.45. [DOI] [PubMed] [Google Scholar]
- Jorge RE, Robinson RG, Tateno A, Narushima K, Acion L, et al. Repetitive transcranial magnetic stimulation as treatment of poststroke depression: A preliminary study. Biol. Psychiatry. 2004;55:398–405. doi: 10.1016/j.biopsych.2003.08.017. [DOI] [PubMed] [Google Scholar]
- Jorm AF. History of depression as a risk factor for dementia: An updated review. Aust N Z J Psychiatry. 2001;35:776–81. doi: 10.1046/j.1440-1614.2001.00967.x. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Akiskal HS. The prevalence, clinical relevance, and public health significance of subthreshold depressions. Psychiatr. Clin. N. Am. 2002;25:685–98. doi: 10.1016/s0193-953x(02)00026-6. [DOI] [PubMed] [Google Scholar]
- Kelly KG, Zisselman M. Update on electroconvulsive therapy (ECT) in older adults. J. Am. Geriatr. Soc. 2000;48:560–6. doi: 10.1111/j.1532-5415.2000.tb05005.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. Age at onset and familial risk for major depression in a Swedish national twin sample. Psychol. Med. 2005;35:1573–9. doi: 10.1017/S0033291705005714. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish national twin study of lifetime major depression. Am. J. Psychiatry. 2006;163:109–14. doi: 10.1176/appi.ajp.163.1.109. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. Personality and major depression: A Swedish longitudinal population-based twin study. Arch. Gen. Psychiatry. 2006;63:1113–20. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- Knight BG, Flynn Longmire CV, Dave J, Kim JH, David S. Mental health and physical health of family caregivers for persons with dementia: A comparison of African American and white caregivers. Aging Ment. Health. 2007;11:538–46. doi: 10.1080/13607860601086561. [DOI] [PubMed] [Google Scholar]
- Kockler M, Heun R. Gender differences of depressive symptoms in depressed and nondepressed elderly persons. Int. J. Geriatr. Psychiatry. 2002;17:65–72. doi: 10.1002/gps.521. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, Tupler LA, Ritchie JC, Jr, McDonald WM, Knight DL, et al. Apolipoprotein E-epsilon 4 frequency in geriatric depression. Biol. Psychiatry. 1996;40:69–71. doi: 10.1016/0006-3223(95)00424-6. [DOI] [PubMed] [Google Scholar]
- Krishnan KR. Biological risk factors in late life depression. Biol. Psychiatry. 2002;52:185–92. doi: 10.1016/s0006-3223(02)01349-5. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, Delong M, Kraemer H, Carney R, Spiegel D, et al. Comorbidity of depression with other medical diseases in the elderly. Biol. Psychiatry. 2002;52:559–88. doi: 10.1016/s0006-3223(02)01472-5. [DOI] [PubMed] [Google Scholar]
- Kung H-S, Hoyert DL, Xu J, Murphy SL. Deaths: Final Data for 2005. National Vital Statistics Reports. 2008 56(10) [Downloaded 7/14/2008 from: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf] [PubMed]
- Lam DCK, Salkovskis PM, Warwick HMC. An experimental investigation of the impact of biological versus psychological explanations of the cause of mental illness. Journal of Mental Health. 2005;14:453–64. [Google Scholar]
- Lenze EJ, Minin JC, Ferrell RE, Pollock BG, Skidmore E, et al. Association of the serotonin transporter gene-linked polymorphic region (5-HTTLPR) genotype with depression in elderly persons after hip fracture. Am. J. Geriatr. Psychiatry. 2005;13:428–32. doi: 10.1176/appi.ajgp.13.5.428. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, et al. Comorbid anxiety disorders in depressed elderly patients. Am. J. Psychiatry. 2000;157:722–8. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Muñoz RF, Youngren, MA, Zeiss AM. Control your depression. 2nd ed. Prentice Hall Press; New York, NY: 1986. [Google Scholar]
- Li C, Ford ES, Strine TW, Mokdad AH. Prevalence of depression among U.S. adults with diabetes: Findings from the 2006 behavioral risk factor surveillance system. Diabetes Care. 2008;31:105–7. doi: 10.2337/dc07-1154. [DOI] [PubMed] [Google Scholar]
- Lichstein KL, Stone KC, Nau SD, McCrae CS, Payne KL. Insomnia in the elderly. Sleep Med. Clin. 2006;1:221–9. [Google Scholar]
- Loebel J, Loebel J, Dager S, Centerwall B. Anticipation of nursing home placement may be a precipitant of suicide among the elderly. J. Am. Geriatr. Soc. 1991;39:407–8. doi: 10.1111/j.1532-5415.1991.tb02910.x. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: A review of the evidence. Am. J. Psychiatry. 2002;159:909–16. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manes F, Jorge R, Morcuende M, Yamada T, Paradiso S, Robinson RG. A controlled study of repetitive transcranial magnetic stimulation as a treatment of depression in the elderly. Int. Psychogeriatr. 2001;13:225–31. doi: 10.1017/s1041610201007608. [DOI] [PubMed] [Google Scholar]
- Maraldi C, Volpato S, Penninx BW, Yaffe K, Simonsick EM, et al. Diabetes mellitus, glycemic control, and incident depressive symptoms among 70-to 79-year-old persons: The health, aging, and body composition study. Arch. Intern. Med. 2007;167:1137–44. doi: 10.1001/archinte.167.11.1137. [DOI] [PubMed] [Google Scholar]
- Marsh L, McDonald WM, Cummings J, Ravina B, NINDS/NIMH Work Group on Depression and Parkinson's Disease Provisional diagnostic criteria for depression in Parkinson's disease: Report of an NINDS/NIMH Work Group. Mov. Disord. 2006;21:148–58. doi: 10.1002/mds.20723. [DOI] [PubMed] [Google Scholar]
- Martire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychol. 2002;21:167–76. [PubMed] [Google Scholar]
- Mazure CM, Maciejewski PK, Jacobs SC, Bruce ML. Stressful life events interacting with cognitive/personality styles to predict late-onset major depression. Am. J. Geriatr. Psychiatry. 2002;10:297–304. [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. Major depression in community-dwelling middle-aged and older adults: Prevalence and 2-year and 4-year follow-up symptoms. Psychol. Med. 2004;34:623–34. doi: 10.1017/S0033291703001764. [DOI] [PubMed] [Google Scholar]
- Mosimann UP, Schmitt W, Greenberg BD, Kosel M, Müri RM, et al. Repetitive transcranial magnetic stimulation: A putative add-on treatment for major depression in elderly patients. Psychiatry Res. 2004;126:123–33. doi: 10.1016/j.psychres.2003.10.006. [DOI] [PubMed] [Google Scholar]
- Motl RW, Konopack JF, McAuley E, Elavsky S, Jerome GJ, Marquez DX. Depressive symptoms among older adults: Long-term reduction after a physical activity intervention. J. Behav. Med. 2005;28:385–94. doi: 10.1007/s10865-005-9005-5. [DOI] [PubMed] [Google Scholar]
- Naarding P, Schoevers RA, Janzing JG, Jonker C, Koudstaal PJ, Beekman AT. A study on symptom profiles of late-life depression: The influence of vascular, degenerative and inflammatory risk-indicators. J. Affect. Disord. 2005;88:155–62. doi: 10.1016/j.jad.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Nau SD, McCrae CS, Cook KG, Lichstein KL. Treatment of insomnia in older adults. Clin. Psychol. Rev. 2005;25:645–72. doi: 10.1016/j.cpr.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Neupert SD, Almeida DM, Charles ST. Age differences in reactivity to daily stressors: The role of personal control. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007;62:P216–25. doi: 10.1093/geronb/62.4.p216. [DOI] [PubMed] [Google Scholar]
- Newmann JP. Aging and depression. Psychol. Aging. 1989;4:150–65. doi: 10.1037//0882-7974.4.2.150. [DOI] [PubMed] [Google Scholar]
- Newmann JP, Engel RJ, Jensen JE. Age differences in depressive symptom experiences. J. Gerontol. 1991;46:P224–35. doi: 10.1093/geronj/46.5.p224. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Ahrens C. Age differences and similarities in the correlates of depressive symptoms. Psychol. Aging. 2002;17:116–24. doi: 10.1037//0882-7974.17.1.116. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Davis CG. “Thanks for sharing that”: Ruminators and their social support networks. J. Pers. Soc. Psychol. 1999;4:801–14. doi: 10.1037//0022-3514.77.4.801. [DOI] [PubMed] [Google Scholar]
- Olin JT, Schneider LS, Katz IR, Meyers BS, Alexopoulos GS, et al. Provisional diagnostic criteria for depression of Alzheimer disease. Am. J. Geriatr. Psychiatry. 2002;10:125–8. [PubMed] [Google Scholar]
- Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: The Heart and Soul Study. Am. J. Psychiatry. 2007;164:1379–84. doi: 10.1176/appi.ajp.2007.06101617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: Systematic review, meta-analysis, and meta-regression analysis. Arch. Gen. Psychiatry. 2006;63:530–8. doi: 10.1001/archpsyc.63.5.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradiso S, Vaidya J, Tranel D, Kosier T, Robinson RG. Nondysphoric depression following stroke. Neuropsychiatry. Clin. Neurosci. 2008;20:52–61. doi: 10.1176/jnp.2008.20.1.52. [DOI] [PubMed] [Google Scholar]
- Park JH, Lee SB, Lee TJ, Lee DY, Jhoo JH, et al. Depression in vascular dementia is quantitatively and qualitatively different from depression in Alzheimer's disease. Dement. Geriatr. Cogn. Disord. 2007;23:67–73. doi: 10.1159/000097039. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Smith LJ, Lyness JM, Matteson SR, Pigeon WR, et al. Insomnia as a risk factor for onset of depression in the elderly. Behav. Sleep Med. 2006;4:104–13. doi: 10.1207/s15402010bsm0402_3. [DOI] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Almeaida DM. Living with chronic health conditions: Age differences in affective well-being. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007;62:P313–21. doi: 10.1093/geronb/62.6.p313. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: A meta-analytic comparison of pharmacotherapy and psychotherapy. Am. J. Psychiatry. 2006;163:1493–1501. doi: 10.1176/ajp.2006.163.9.1493. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Frank E, Kasl SV, Reynolds CF, Anderson B, et al. Complicated grief and bereavement-related depression as distinct disorders: Preliminary empirical validation in elderly bereaved spouses. Am. J. Psychiatry. 1995;152:22–30. doi: 10.1176/ajp.152.1.22. [DOI] [PubMed] [Google Scholar]
- Ravina B, Camicioli R, Como PG, Marsh L, Jankovic J, et al. The impact of depressive symptoms in early Parkinson disease. Neurology. 2007;69:342–7. doi: 10.1212/01.wnl.0000268695.63392.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reijnders JS, Ehrt U, Weber WE, Aarsland D, Leentjens AF. A systematic review of prevalence studies of depression in Parkinson's disease. Mov. Disord. 2008;23:183–9. doi: 10.1002/mds.21803. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Zimmerman M, McGlinchey JB, Chelminski I, Young D. Diagnosing major depressive disorder XI: A taxometric investigation of the structure underlying DSM-IV symptoms. J. Nerv. Ment. Dis. 2007;195:10–9. doi: 10.1097/01.nmd.0000252025.12014.c4. [DOI] [PubMed] [Google Scholar]
- Rutz W, von Knorring L, Wålinder J. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr. Scand. 1992;85:83–8. doi: 10.1111/j.1600-0447.1992.tb01448.x. [DOI] [PubMed] [Google Scholar]
- Schoevers RA, Beekman AT, Deeg DJ, Jonker C, van Tilburg W. Comorbidity and risk-patterns of depression, generalised anxiety disorder and mixed anxiety-depression in later life: Results from the AMSTEL study. Int. J. Geriatr. Psychiatry. 2003;18:994–1001. doi: 10.1002/gps.1001. [DOI] [PubMed] [Google Scholar]
- Schoevers RA, Smit F, Deeg DJH, Cuijpers P, Dekker J, et al. Prevention of late-life depression in primary care: Do we know where to begin? Am. J. Psychiatry. 2006;163:1611–21. doi: 10.1176/ajp.2006.163.9.1611. [DOI] [PubMed] [Google Scholar]
- Schulz R, McGinnis KA, Zhang S, Martire LM, Hebert RS, Beach SR, et al. Dementia patient suffering and caregiver depression. Alzheimer Disease and Associated Disorders. 2008;22:170–6. doi: 10.1097/WAD.0b013e31816653cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweitzer I, Tuckwell V, O'Brien J, Ames D. Is late onset depression a prodrome to dementia? Int. J. Geriatr. Psychiatry. 2002;17:997–1005. doi: 10.1002/gps.525. [DOI] [PubMed] [Google Scholar]
- Scogin F, Welsh D, Hanson A, Stump J, Coates A. Evidence-based psychotherapies for depression in older adults. Psychol. Sci. Prac. 2005;12:222–37. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD, Kabat-Zinn J. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford; New York: 2001. [Google Scholar]
- Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, Fiatarone Singh MA. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005;60:768–76. doi: 10.1093/gerona/60.6.768. [DOI] [PubMed] [Google Scholar]
- Sjösten N, Kivelä SL. The effects of physical exercise on depressive symptoms among the aged: A systematic review. Int. J. Geriatr. Psychiatry. 2006;21:410–8. doi: 10.1002/gps.1494. [DOI] [PubMed] [Google Scholar]
- Swenson CJ, Baxter J, Shetterly SM, Scarbro SL, Hamman RF. Depressive symptoms in Hispanic and non-Hispanic White rural elderly. The San Luis Valley Health and Aging Study. Am J Epidemiol. 2000;152:1048–55. doi: 10.1093/aje/152.11.1048. [DOI] [PubMed] [Google Scholar]
- Taylor W, Steffens D, MacFall J, McQuoid D, Payne M, et al. White matter hyperintensity progression and late-life depression outcomes. Arch. Gen. Psychiatry. 2003;60:1090–6. doi: 10.1001/archpsyc.60.11.1090. [DOI] [PubMed] [Google Scholar]
- Teri L, McKenzie G, LaFazia D. Psychosocial treatment of depression in older adults with dementia. Clin. Psychol. Sci. Prac. 2005;12:303–16. [Google Scholar]
- Tiemeier H. Biological risk factors for late life depression. Eur. J. Epidemiol. 2003;18:745–50. doi: 10.1023/a:1025388203548. [DOI] [PubMed] [Google Scholar]
- Torges CM, Stewart AJ, Nolen-Hoeksema S. Regret resolution, aging, and adapting to loss. Psychol. Aging. 2008;23:169–80. doi: 10.1037/0882-7974.23.1.169. [DOI] [PubMed] [Google Scholar]
- Uebelacker LA, Wang PS, Berglund P, Kessler RC. Clinical differences among patients treated for mental health problems in general medical and specialty mental health settings in the National Comorbidity Survey Replication. General Hospital Psychiatry. 2006;28:387–95. doi: 10.1016/j.genhosppsych.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Wortman CB, Kessler RC. Widowhood and depression: Explaining long-term gender differences in vulnerability. Journal of Health and Social Behavior. 1992;33:10–24. [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, et al. JAMA. 2002;288:2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Vink D, Aartsen MJ, Schoevers RA. Risk factors for anxiety and depression in the elderly: A review. J. Affect. Disord. 2008;106:29–44. doi: 10.1016/j.jad.2007.06.005. [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Gatz M, Pedersen NL. A longitudinal analysis of anxiety and depressive symptoms. Psychol. Aging. 2001;16:187–95. doi: 10.1037//0882-7974.16.2.187. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Caska CM, Hendrickson BE, Rourke MA, Ho J, Ali S. Depression and inflammation in patients with coronary heart disease: Findings from the Heart and Soul Study. Biol. Psychiatry. 2007;62:314–20. doi: 10.1016/j.biopsych.2006.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whyte EM, Mulsant BH, Rovner BW, Reynolds CF. Preventing depression after stroke. International Review of Psychiatry. 2006;18:471–81. doi: 10.1080/09540260600935470. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR. The activity restriction model of depressed affect: Antecedents and consequences of restricted normal activities. In: Williamson GM, Shaffer DR, Parmelee PA, editors. Physical Illness and Depression in Older Adults: A Handbook of Theory, Research, and Practice. Kluwer Academic/Plenum Publishers; New York: 2000. pp. 173–200. [Google Scholar]
- Wouts L, Oude Voshaar RC, Bremmer MA, Buitelaar JK, Penninx BW, Beekman AT. Cardiac disease, depressive symptoms, and incident stroke in an elderly population. Arch. Gen. Psychiatry. 2008;65:596–602. doi: 10.1001/archpsyc.65.5.596. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Schulz R, Miller GE, Lupien S, Dunne E. Physical health problems, depressive mood, and cortisol secretion in old age: Buffer effects of health engagement control strategies. Health Psychol. 2007;26:341–9. doi: 10.1037/0278-6133.26.3.341. [DOI] [PubMed] [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. J. Health Soc. Behav. 2006;47:355–72. doi: 10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]
- Zeiss AM. Depression in long-term care: Contrasting a disease model with attention to environmental impact. Clin. Psychol. Sci. Prac. 2005;12:300–2. [Google Scholar]
- Zisook S, Kendler KS. Is bereavement-related depression different than non-bereavement-related depression? Psychol. Med. 2007;37:779–94. doi: 10.1017/S0033291707009865. [DOI] [PubMed] [Google Scholar]