Abstract
Purpose
Benzo[a]pyrene 7,8-diol 9,10-epoxide (BPDE), an ultimate metabolite of benzo[a]pyrene, attacks deoxyguanosine to form a BPDE-N2-dG adduct resulting in p53 mutations. Both cytochrome P4501A1 (CYP1A1) and glutathione S-transferase M1 (GSTM1) have been demonstrated to be involved in the metabolism of polycyclic aromatic hydrocarbons. The relationship between BPDE-like DNA adduct levels and CYP1A1 and GSTM1 gene polymorphisms in pterygium is not clear. Therefore, BPDE-like DNA adducts and CYP1A1 and GSTM1 polymorphisms were detected in this study to provide more molecular evidence to understand the cause of BPDE-like DNA adduct formation in pterygium.
Methods
In this study, immunohistochemical staining using a polyclonal antibody on BPDE-like DNA adducts was performed on 103 pterygial specimens. For the analysis of CYP1A1 and GSTM1 polymorphisms, DNA samples were extracted from epithelial cells and then subjected to restriction fragment length polymorphism (RFLP) and polymerase chain reaction (PCR) for the determination of mutation and genotype of CYP1A1 and GSTM1.
Results
BPDE-like DNA adducts were detected in 33.0% (34/103) of the pterygium samples. The differences in DNA adduct levels were associated with the genetic polymorphisms of CYP1A1 but not GSTM1. Additionally, the risk of BPDE-like DNA adduct formation for patients with CYP1A1 m1/m2 (C/T) andm2/m2 (T/T) was 9.675 fold higher than that of patients with CYP1A1 m1/m1 (C/C) types (p=0.001, 95% Confidence Interval 2.451–38.185).
Conclusions
Our data provide evidence that the BPDE-like DNA adduct formation in pterygium samples was associated with CYP1A1 polymorphisms.
Introduction
Pterygium is a chronic condition characterized by the encroachment of a fleshy triangle of conjunctival tissue into the cornea. It has long been considered a chronic degenerative condition; however, after finding abnormal expression of the p53 protein in epithelium, pterygium is now considered to be an ultraviolet-related uncontrolled cell proliferation, like a tumor [1-7]. The p53 tumor suppressor gene is one of the most commonly mutated genes observed in human tumors. Mutations within the p53 gene were detected in 15.7% of the pterygial samples of our previous study, and deletion mutations were found in the same samples with p53-negative staining, while substitution mutations were found in samples with p53-positive staining [8]. However, the cause of p53 mutation in pterygium is still unclear. Polycyclic aromatic hydrocarbons (PAHs) might be responsible for the mutagenicity of airborne particulates in Taiwan [9,10]. The environmental pollutant, benzo[a]pyrene (BaP), which is one of the PAHs, has been found to cause p53 mutations and then lung tumorigenesis. The levels of PAHs in airborne particulates in Taiwan are higher than levels found in other countries, especially levels of BaP, benzo[b]fluoranthrene, and benzo[g,h,i]perylene [9,10]. BaP 7,8-diol 9,10-epoxide (BPDE), an ultimate metabolite of BaP, attacks deoxyguanosine to form a BPDE-N2-dG adduct that results in p53 mutations. The mutation hotspots of p53 in human lung tumors (codons 154, 157, 158, 245, 248, and 273) are caused by the BPDE-N2-dG adduct [11]. Thus, an evaluation of DNA adducts induced by BaP and other PAHs is suitable as a risk marker for p53 mutation.
Bap is oxidized by a series of well-characterized enzymes, such as cytochrome p450 1A1, 2C9, and 3A4 [12,13]. A thymine/cytosine point mutation in the MspI restriction site of cytochrome P4501A1 (CYP1A1) has been reported to result in increased enzyme activity [14]. The CYP1A1 MspI polymorphism has been linked to the susceptibility for smoking-related cancers, such as lung [15,16], colon, breast, and oral cancers [17]. Not only cytochrome P450 but also other enzymes, such as glutathion s-transferase M1 (GSTM1), was shown to be involved in BaP metabolism [18-20]. GSTM1 has also been shown to be polymorphic. A deletion is responsible for the existence of a null allele associated with the lack of expression of a functional protein [21,22]. The polymorphic GSTM1 null genotype has been found in 20–50% of populations of various ethnic origins, and this genotype has been correlated with the risk for various tobacco-related cancers [23-26]. Therefore, genetic polymorphisms of CYP1A1 and GSTM1 may contribute to BPDE-like DNA adduct formation and pterygium progression.
In this study, we try to detect the BPDE-like DNA adducts, using immunohistochemistry in 103 pterygium specimens, and we compare them with CYP1A1 and GSTM1 polymorphisms to understand the relationship between environmental exposure and genetic polymorphism in pterygium.
Methods
Patients and methods
Pterygial samples were harvested from 103 patients (68 males and 35 females) with primary pterygium undergoing pterygium surgery at China Medical University Hospital, Taichung, Taiwan. The age range was 52 to 85, and the average age was 70.2-years old. All specimens were formalin fixed and paraffin embedded. Then, 3-µm-thick sections were cut, mounted on glass, and dried overnight at 37 °C for immunohistochemical analysis. All participants were asked to submit a written informed consent approved by the Institutional Review Board of the Chung-Shan Medical University Hospital.
Immunohistochemical analysis of BaP 7,8-diol 9,10-epoxide (BPDE)-like DNA adduct detection
All sections were deparaffinized in xylene, rehydrated with alcohol, and washed in PBS (3.2 mM Na2HPO4, 0.5 mM KH2PO4, 1.3 mM KCl, 135 mM NaCl, pH 7.4). This buffer was used for all subsequent washes. Sections for BPDE-like DNA adduct detection were heated in a microwave oven (TMO-2050; TATUNG, Taiwan) with 700 W power, twice, each time for 5 min in citrate buffer (pH 6.0). Anti-BPDE-like DNA adduct polyclonal antibody (which was kindly provided by Dr. Huei Lee, Institute of Medical & Molecular Toxicology, Chung Shan Medical University, Taichung, Taiwan; at a dilution of 1:1,000 [27]) was used as the primary antibody, and the incubation time was 60 min at room temperature (25 °C) followed by a conventional streptavidin peroxidase method for antibody detection (LSAB Kit K675; DAKO,Glostrup, Denmark). The sections were incubated with biotinylated secondary antibody 10 min at room temperature (25 °C). After washed with PBS, the section were incubated with HRP conjugates Streptavidin 10 min at room temperature (25 °C). Signals were developed with 3, 3′-diaminobenzidine (LSAB Kit K675; DAKO) for 5 min and counter-stained with hematoxylin (DAKO). The positive and negative controls used for the BPDE immunohistochemical stain were lung tissue, [28] which had high and nondetectable BPDE DNA adduct levels, respectively, as analyzed by 32P-post labeling and enzyme-linked immunosorbent assay (ELISA) [28]. The results were evaluated independently by three observers and scored for the percentage of positive nuclei: score 0, no positive staining; score +, from 1% to 10%; score ++, from 11% to 50%; and score +++, more than 50% positive cells. In this study, scores of +, ++, and +++ were considered to be positive immunostaining, and a score of 0 was considered to be negative immunostaining.
Polymorphisms of CYP1A1 and GSTM1
DNA was extracted from the paraffin-embedded pterygium tissues for genetic polymorphism analysis [29]. DNA lysis buffer (10 mM Tris-HCl, pH 8.0, 0.1 M NaCl, 25 mM EDTA, and 0.5% SDS) was applied to lyse the epithelial cells on the slide, and then the DNA solution was transferred into an Eppendorf tube for traditional proteinase K digestion and phenol-chloroform extraction. The suspension was incubated at 56 °C for 2 h in the presence of proteinase K. The suspension was sequentially extracted with phenol-chloroform (25: 24).. Finally, the DNA was precipitated with 500 μl of 100% ethanol with an addition of linear polyacrylamide to increase DNA amounts [30]. Genotyping of the MspI polymorphism of CYP1A1 was performed by PCR amplification using the primer set of 5′-TAG GAG TCT TGT CTC AGC CT-3′ and 5′-CAG TGA AGA GGT GTA GCC GCT-3′ [31]. The amplified products were digested with MspI and analyzed by electrophoresis on a 1.5% agarose gel. The MspI restriction site polymorphism resulted in three genotypes: a predominant homozygous m1 allele without the MspI site (genotype m1/m1; C/C), the heterozygote (genotype m1/m2; C/T) and a rare homozygous m2 allele with the MspI site (genotype m2/m2; T/T). Detailed information of the PCR assays can be found elsewhere [32]. Briefly, the PCR reaction containined: DNA 1 μl, 0.5 mM dNTP, 5 μl 10× reaction buffer, 2.5 U Taq polymorase and 0.5 mM primer. An initial denaturing step of 5 min at 94 °C followed by 35 cycles of 94 °C for 30 s, 60 °C for 45 s, and 72 °C for 1 min and then a final extension at 72 °C for six min. Genotypes of GSTM1 were determined by the presence or absence of the PCR product, according to the method of Groppi et al. [32]. The genotypes of GSTM1 are defined as present and null types. Two primers, 5′-GAA GGT GGC CTC CT-CC TTG G-3′ and 5′-AAT TCT GGA TTG TAG CAG AT-3′, were used for PCR. If samples had no PCR product, the PCR experiment was repeated with the addition of a set of β-actin (ACTB) primers together with GSTM1 primers to confirm that the absence of the GSTM1 PCR product represented the null genotype.
Statistical analysis
Statistical analysis was performed using the SPSS 13.0 statistical software program (SPSS Inc., Chicago, IL). The χ2, logistic regression test, and Fisher’s exact test were applied for statistical analysis. A p<0.05 was considered to be statistically significant.
Results
BaP 7,8-diol 9,10-epoxide (BPDE)-like DNA adduct detected in pterygium
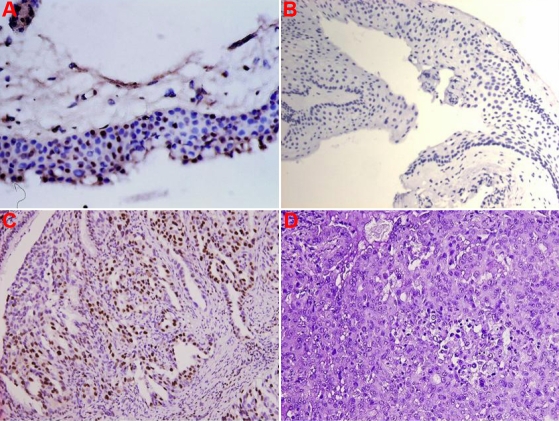
In the pterygium group, 69 (67.0%) pterygial specimens scored 0, eight (7.8%) were +, 12 (11.6%) were ++, and 14 (13.6%) were +++. The detection rate of the BPDE-like DNA adduct was 25.2% if a score of 0 and + were considered to be negative for BPDE-like DNA adduct staining and ++ and +++ were considered positive (setting the cutoff level at 10%). If a score of 0 was considered to be negative and +, ++, and +++ to be positive (setting the cutoff level at 1%), the positive rate of detection was 33.0%. The BPDE-like DNA adduct staining was limited to the nuclei of the epithelial layer and subepithelial fibrovascular layers (Table 1; Figure 1). This result was similar to our previous report [33].
Table 1. The BPDE-like DNA adduct levels in pterygium analyzed by immunohistochemistry.
| Parameter | BPDE-like DNA adducts | % |
|---|---|---|
| - |
69 |
67.0 |
| + |
8 |
7.8 |
| ++ |
12 |
11.6 |
| +++ | 14 | 13.6 |
The results were evaluated independently by three observers and scored for the percentage of positive nuclei: score -, no positive staining; score +, from 1% to 10%; score ++, from 11% - 50%; score +++, more than 50% positive cells. BPDE DNA adducts analyzed in this study are based on prior pterygium samples [25].
Figure 1.
Representative positive and negative immunostaining for BaP 7,8-diol 9,10-epoxide (BPDE)like DNA adducts in paraffin sections of pterygium epithelial cells. Representative positive immunostaining (brown signal) in the epithelial layer is shown in A (200×), negative immunostaining is shown in B (200×), a lung cancer section with high BPDE-like DNA adduct levels used as the positive control is shown in C (brown; 200×), and a lung cancer section with no detectable BPDE-like DNA adduct levels, which was used as the negative control, is shown in D (200×).
CYP1A1 and GSTM1 polymorphisms in pterygium
To verify the distribution of CYP1A1 and GSTM1 polymorphisms in pterygium, the polymorphisms of CYP1A1 and GSTM1 in pterygium and control groups were analyzed by PCR-RFLP (restriction fragment length polymorphism) and PCR. The results for the genotypes of CYP1A1 and GSTM1 in pterygium are shown in Table 2. The analysis of the CYP1A1 MSPI polymorphisms in pterygium showed that 34 (33.0%) were homozygous for the m1/m1 genotype, 15 (14.6%) were homozygous for the m2/m2 genotype, and 54 (52.4%) were heterozygous for the m1/m2 genotype. The analysis of the presence of GSTM1 polymorphisms or the null type in pterygium showed that 60 (58.3%) were the present type and 43 (41.7%) were the null type.
Table 2. CYP1A1 and GSTM1 polymorphisms in pterygium analyzed by PCR-RFLP and PCR.
| Gene | Number | % |
|---|---|---|
|
CYP1A1 | ||
| A (m1/m1) |
34 |
33.0 |
| B (m1/m2) |
54 |
52.4 |
| C (m2/m2) |
15 |
14.6 |
|
GSTM1 | ||
| Null |
43 |
41.7 |
| Present | 60 | 58.3 |
Correlation of BaP 7,8-diol 9,10-epoxide (BPDE)-like DNA adduct levels and CYP1A1 and GSTM1 polymorphisms in pterygium
Previous reports have indicated that CYP1A1 and GSTM1 polymorphisms correlated with BPDE-like DNA adduct formation [34,35]. To verify this point, the relationships between BPDE-like DNA adduct levels and CYP1A1 and GSTM1 polymorphisms in pterygium were analyzed. As shown in Table 3, only the CYP1A1 polymorphisms correlated with BPDE-like DNA adduct levels. The BPDE-like DNA adduct in patients with the m2/m2 polymorphism was higher than in the m1/m1 and m1/m2 groups (p=0.006). Additionally, there was no correlation between the GSTM1 polymorphism and the BPDE-like DNA adduct in this study group.
Table 3. Relationship of BPDE-like DNA adduct levels and CYPA1 and GSTM1 polymorphisms in pterygium patients.
|
|
BPDE-like DNA adduct levels |
|
|
|---|---|---|---|
| Gene | Negative | Positive | p value |
|
CYP1A1 | |||
| A |
29 |
5 |
|
| B |
29 |
25 |
|
| C |
11 |
4 |
0.006 |
|
GSTM1 | |||
| Null |
17 |
17 |
|
| Present | 25 | 44 | 0.205 |
The results were evaluated independently by three observers and scored for the percentage of positive nuclei: negative, 0%; positive, more than 11% positive cells. BPDE DNA adducts analyzed in this study are based on prior pterygium samples [25].
CYP1A1 polymorphism is a risk factor of BaP 7,8-diol 9,10-epoxide (BPDE)-like DNA adduct formation
The influences of CYP1A1 and GSTM1 polymorphisms and gender in BPDE-like DNA adduct formation were calculated by logistic regression analysis. Among the characteristics, only the CYP1A1 polymorphisms were significant risk factors (Table 4; p=0.001, 95% Confidence Interval 2.451–38.185). The risk of BPDE-like DNA adduct formation for patients with CYP1A1 m2/m2 and m1/m2 was 9.675 fold more than that of patients with m1/m1 types. This suggests that CYP1A1 polymorphisms are significant as risk factors in BPDE-like DNA adduct formation in pterygium patients.
Table 4. The effects of gender, CYP1A1, and GSTM1 polymorphisms on DNA adduct levels in pterygium patients.
| Parameters | OR | Unfavorable/favorable | 95%CI | p |
|---|---|---|---|---|
| Gender |
0.343 |
Female/Male |
0.082–1.432 |
0.142 |
|
CYP1A1 |
9.675 |
A/B+C |
2.451–38.185 |
0.001 |
| GSTM1 | 0.453 | Null/Present | 0.159–1.292 | 0.139 |
Discussion
To our knowledge, this is the first study to analyze the correlation of genetic polymorphism and BPDE-like DNA adduct formation in pterygium. Previous studies have shown that DNA adduct levels are associated with CYP1A1 and GSTM1 polymorphisms [34-39]. However, in our study we found that only the CYP1A1 polymorphisms were associated with BPDE-DNA adduct formation in pterygium. If genetic polymorphisms are not associated with individual susceptibility to carcinogenic PAHs, DNA repair capacity may play an important role in the susceptibility to DNA damage. Previous reports support the idea that the capacity of BPDE-DNA adducts to be removed from peripheral lymphocytes after exposure to BPDE in vitro, measured by 32P-postlabeling and host-cell reactive assay, is significantly lower in cancer patients compared to healthy persons [40-42]. Common polymorphisms in DNA repair enzymes have been hypothesized to result in reduced capability to repair DNA damage [43,44]. Several reports have indicated that polymorphisms of DNA repair genes are associated with pterygium formation [45,46]. Thus, reduced DNA repair capacity appears to contribute to DNA adduct formation in pterygium.
GST is one of the antioxidant defense enzymes that contributes to the protection against reactive oxygen species [47,48]. The GSTM1-null type was reported to be associated with cutaneous photosensitivity [49,50], so GSTM1 null may be associated with the photosensitivity of corneal limbal cells. Our previous report indicated that lack of GSTM1 (GSTM1-null type) contributes to susceptibility of pterygium formation in early onset pterygium but is not associated with late onset pterygium [46]. In the present study we did not find an association between the GSTM1 polymorphism and BPDE DNA adduct levels. Therefore, we suggest that the role of GSTM1 in pterygium formation is more important in antioxidant defense than in PAH metabolism.
PAH compounds are the products of incomplete combustion of organic material and are thus ubiquitous in the environment (IARC, 1983). Occupational exposure to PAH compounds increases the risk of lung and, putatively, other cancers and is highest in coke oven workers, other workers in the steel industry, asphalt and bitumen workers, and those exposed to gasoline exhaust and working with gasoline. The best known carcinogen in cigarette smoke, BaP, has been experimentally shown to induce G:C–T:A transversions [51], which are the main mutation types in smoking-related lung cancer [52]. Our present study shows that BPDE-like DNA adduct levels correlated with a CYP1A1 polymorphism. The mutation hotspots of p53 in human lung tumors (codons 154, 157, 158, 245, 248, and 273) are caused by the BPDE-N2-dG adduct [11]. Thus, an evaluation of DNA adducts induced by BaP and other PAHs is suitable as a risk marker of p53 mutation. The p53 tumor suppressor gene is one of the most commonly mutated genes observed in human tumors. The mutation of p53 has been noted in more than 50% of all human cancers [53-55].
Additionally, our previous study showed that BPDE-like DNA adducts are indeed detected in pterygium samples and are minor contributors to the abnormal p53 gene [33]. Therefore, we hypothesize that after exposure to environmental PAHs, the CYP1A1 polymorphism may result in high levels of BPDE-like DNA adduct formation contributing to p53 or other tumor suppressor gene mutations to induce pterygium formation.
Our previous study detected BPDE-like DNA adducts in pterygium paraffin sections [33]. In the present study, we also found that the CYP1A1 polymorphism correlated with BPDE-like DNA adduct formation in pterygium. These findings seem to provide molecular evidence to support the idea that not only ultraviolet radiation but also environmental exposure is involved in pterygium pathogenesis.
Acknowledgments
This work was supported by grants from the National Science Council (NSC96–2314-B-039–009-MY2). The authors have no proprietary or financial interest in any material or device.
References
- 1.Tan DT, Lim AS, Goh HS, Smith DR. Abnormal expression of the p53 tumor suppressor gene in the conjunctiva of patients with pterygium. Am J Ophthalmol. 1997;123:404–5. doi: 10.1016/s0002-9394(14)70141-2. [DOI] [PubMed] [Google Scholar]
- 2.Dushku N, Reid TW. P53 expression in altered limbal basal cells of pingula, pterygia, and limbal tumors. Curr Eye Res. 1997;16:1179–92. doi: 10.1076/ceyr.16.12.1179.5036. [DOI] [PubMed] [Google Scholar]
- 3.Onur C, Orhan D, Orhan M, Dizbay Sak S, Tulunay O, Irkeç M. Expression of p53 protein in pterygia. Eur J Ophthalmol. 1998;8:157–61. doi: 10.1177/112067219800800307. [DOI] [PubMed] [Google Scholar]
- 4.Chowers I, Pe’er J, Zamir E, Livni N, Ilsar M, Frucht-Pery J. Proliferative activity and p53 expression in primary and recurrent pterygia. Ophthalmology. 2001;108:985–8. doi: 10.1016/s0161-6420(00)00651-5. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein O, Rosenthal G, Zirkin H, Monos T, Lifshitz T, Argov S. Overexpression of p53 tumor suppressor gene in pterygia. Eye. 2002;16:619–21. doi: 10.1038/sj.eye.6700150. [DOI] [PubMed] [Google Scholar]
- 6.Tan DT, Tang WY, Liu YP, Goh HS, Smith DR. Apoptosis and apoptosis related gene expression in normal conjunctiva and pterygium. Br J Ophthalmol. 2000;84:212–6. doi: 10.1136/bjo.84.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dushku N, Hatcher SLS, Albert DM. P53 expression and relation to human papillomavirus infection in pinguecula, pterygia, and limbal tumors. Arch Ophthalmol. 1999;117:1593–9. doi: 10.1001/archopht.117.12.1593. [DOI] [PubMed] [Google Scholar]
- 8.Tsai YY, Cheng YW, Lee H, Tsai FJ, Tseng SH, Chang KC. P53 gene mutation spectrum and the relationship between gene mutation and protein expression in pterygium. Mol Vis. 2005;11:50–5. [PubMed] [Google Scholar]
- 9.Lee H, Su SY, Liu KS, Chou MC. Correlation between meteorological conditions and mutagenicity of airborne particulate samples in a tropical monsoon climate area from Kaohsiung city, Taiwan. Environ Mol Mutagen. 1994;23:200–7. doi: 10.1002/em.2850230309. [DOI] [PubMed] [Google Scholar]
- 10.Kuo CY, Cheng YW, Chen CY, Lee H. Correlation between the amounts of polycyclic aromatic hydrocarbons and mutagenicity of airborne particulate samples from Taichung city, Taiwan. Environ Res. 1998;78:43–9. doi: 10.1006/enrs.1998.3838. [DOI] [PubMed] [Google Scholar]
- 11.Hussain SP, Amstad P, Raja K, Sawyer M, Hofseth L, Shields PG, Hewer A, Phillips DH, Ryberg D, Haugen A, Harris CC. Mutability of p53 hotspot codons to benzo(a)pyrene diol epoxide (BPDE) and the frequency of p53 mutations in nontumorous human lung. Cancer Res. 2001;61:6350–5. [PubMed] [Google Scholar]
- 12.Shimada T, Yun CH, Yamasaki H, Gautier C, Beaune PH, Guengerich P. Characterization of human lung microsomal cytochrome P450 1A1 and its role in the oxidation of chemical carcinogens. Mol Pharmacol. 1992;41:856–64. [PubMed] [Google Scholar]
- 13.London SJ, Daly AK, Leathart JBS, Navidi WC, Idle JR. Lung cancer risk in relation to the CYP2C9*1/CYP2CP*2 genetic polymorphism among Africa-Americans and Caucasians in Los Angeles County, California. Pharmacogenetics. 1996;6:527–33. doi: 10.1097/00008571-199612000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Bartsch H, Nair U, Risch A, Rojas M, Wilkman H, Alexandrov K. Genetic polymorphism of CYP genes, alone or in combination, as a risk modifier of tobacco-related cancers. Cancer Epidemiol Biomarkers Prev. 2000;9:3–28. [PubMed] [Google Scholar]
- 15.Kawajiri K, Nakachi K, Imai K, Yoshii A, Shinoda N, Watanabe J. Identification of genetically high risk individuals to lung cancer by DNA polymorphisms of the cytochrome P450IA1 gene. FEBS Lett. 1990;263:131–3. doi: 10.1016/0014-5793(90)80721-t. [DOI] [PubMed] [Google Scholar]
- 16.Hayashi S, Watanabe J, Kawajiri K. High susceptibility to lung cancer analyzed in terms of combined genotypes of P450IA1 and Mu-class glutathione S-transferase genes. Jpn J Cancer Res. 1992;83:866–70. doi: 10.1111/j.1349-7006.1992.tb01992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kao SY, Wu CH, Lin SC, Yap SK, Chang CS, Wong YK, Chi LY, Liu TY. Genetic polymorphism of cytochrome P4501A1 and susceptibility to oral squamous cell carcinoma and oral precancer lesions associated with smoking/betel use. J Oral Pathol Med. 2002;31:505–11. doi: 10.1034/j.1600-0714.2002.00158.x. [DOI] [PubMed] [Google Scholar]
- 18.Ketterer B, Harris JM, Talaska G, Meyer DJ, Pemble SE, Taylor JB, Lang NP, Kadlubar FF. The human glutathioneS-transferase supergene family, its polymorphism, and its effects on susceptibility to lung cancer. Environ Health Perspect. 1992;98:87–94. doi: 10.1289/ehp.929887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sundberg K, Seidel A, Mannervik B, Jernstrom B. Detoxification of carcinogenic fjord-region diol epoxides of polycyclic aromatic hydrocarbons by glutathione transferase P1–1 variants and glutathione. FEBS Lett. 1998;438:206–10. doi: 10.1016/s0014-5793(98)01291-5. [DOI] [PubMed] [Google Scholar]
- 20.Coles B, Ketterer B. The role of glutathione and glutathione transferases in chemical carcinogenesis. Crit Rev Biochem Mol Biol. 1990;25:47–70. doi: 10.3109/10409239009090605. [DOI] [PubMed] [Google Scholar]
- 21.Seidegard J, Pero RW, Markowitz MM, Roush G, Miller DG, Beattie EJ. Isoenzyme(s) of glutathione transferase (class A) as a marker for the susceptibility to lung cancer: a follow up study. Carcinogenesis. 1990;11:33–6. doi: 10.1093/carcin/11.1.33. [DOI] [PubMed] [Google Scholar]
- 22.Pemble S, Schroeder KR, Spencer SR, Meyer DJ, Hallier E, Bolt HM, Ketterer B, Taylor JB. Human glutathione S-transferase (GSTT1): cDNA cloning and the characterization of a genetic polymorphism. Biochem J. 1994;300:271–6. doi: 10.1042/bj3000271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McWilliams JE, Sanderson BJ, Harris EL, Richert-Boe KE, Henner WD. Glutathione S-transferase M1 (GSTM1) deficiency and lung cancer risk. Cancer Epidemiol Biomarkers Prev. 1995;4:589–94. [PubMed] [Google Scholar]
- 24.Sato M, Sato T, Izumo T, Amagasa T. Genetic polymorphism of drug-metabolizing enzymes and susceptibility to oral cancer. Carcinogenesis. 1999;20:1927–31. doi: 10.1093/carcin/20.10.1927. [DOI] [PubMed] [Google Scholar]
- 25.Katoh T, Kaneko S, Kohshi K, Munaka M, Kitagawa K, Kunugita N, Kunugita N, Ikemura K, Kawamoto T. Genetic polymorphisms of tobacco- and alcohol-related metabolizing enzymes and oral cavity cancer. Int J Cancer. 1999;83:606–9. doi: 10.1002/(sici)1097-0215(19991126)83:5<606::aid-ijc6>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 26.Bell DA, Taylor JA, Paulson DF, Robertson CN, Mohler JL, Lucier GW. Genetic risk and carcinogen exposure: a common inherited defect of the carcinogen-metabolism gene glutathione S-transferase M1 (GSTM1) that increases susceptibility to bladder cancer. J Natl Cancer Inst. 1993;85:1159–64. doi: 10.1093/jnci/85.14.1159. [DOI] [PubMed] [Google Scholar]
- 27.Cheng YW, Hsieh LL, Lin P, Chen CP, Chen CY, Lin TS, Su JM, Lee H. Gender difference in DNA adduct levels among non-smoking lung cancer patients. Environ Mol Mutagen. 2001;37:304–10. doi: 10.1002/em.1037. [DOI] [PubMed] [Google Scholar]
- 28.Cheng YW, Hsieh LL, Lin P, Chen CP, Chen CY, Lin TS, Su JM, Lee H. Gender difference in DNA adduct levels among non-smoking lung cancer patients. Environ Mol Mutagen. 2001;37:304–10. doi: 10.1002/em.1037. [DOI] [PubMed] [Google Scholar]
- 29.Tsai YY, Cheng YW, Lee H, Tsai FJ, Tseng SH, Chang KC. P53 gene mutation spectrum and the relationship between gene mutation and protein expression in pterygium. Mol Vis. 2005;11:50–5. [PubMed] [Google Scholar]
- 30.Gaillard C, Strauss F. Ethanol precipitation of DNA with linear polyacrylamide as carrier. Nucleic Acids Res. 1990;18:378. doi: 10.1093/nar/18.2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hayashi S, Watanabe J, Nakachi K, Kawajiri K. Genetic linkage of lung cancer-associated MspI polymorphisms with amino acid replacement in the heme binding region of the human cytochrome P4501A1 gene. J Biochem. 1991;110:407–11. doi: 10.1093/oxfordjournals.jbchem.a123594. [DOI] [PubMed] [Google Scholar]
- 32.Groppi A, Couttele C, Fleury B, Iron A, Beugeret J, Couzigous P. Glutathione S-transferase class mu in French alcoholic cirrhotic patients. Hum Genet. 1991;87:628–30. doi: 10.1007/BF00209028. [DOI] [PubMed] [Google Scholar]
- 33.Lai TJ, Tsai YY, Cheng YW, Chiang CC, Lee H, Chou MC, Chang JH. An association between BPDE-like DNA adducts levels and P53 gene mutation in pterygium. Mol Vis. 2006;12:1687–91. [PubMed] [Google Scholar]
- 34.Lodovici M, Luceri C, Guglielmi F, Bacci C, Akpan V, Fonnesu ML, Boddi V, Dolara P. Benzo(a)pyrene diolepoxide (BPDE)-DNA adduct levels in leukocytes of smokers in relation to polymorphism of CYP1A1, GSTM1, GSTP1, GSTT1, and mEH. Cancer Epidemiol Biomarkers Prev. 2004;13:1342–8. [PubMed] [Google Scholar]
- 35.Alexandrov K, Cascorbi I, Rojas M, Bouvier G, Kriek E, Bartsch H. CYP1A1 and GSTM1 genotypes affect benzo[a]pyrene DNA adducts in smokers' lung: comparison with aromatic/hydrophobic adduct formation. Carcinogenesis. 2002;23:1969–77. doi: 10.1093/carcin/23.12.1969. [DOI] [PubMed] [Google Scholar]
- 36.Perera FP. Environment and cancer: who are susceptible? Science. 1997;278:1068–73. doi: 10.1126/science.278.5340.1068. [DOI] [PubMed] [Google Scholar]
- 37.Kato S, Bowman ED, Harrington AM, Blomeke B, Shields PG. Human lung carcinogen-DNA adduct levels mediated by genetic polymorphisms in vivo. J Natl Cancer Inst. 1995;87:902–7. doi: 10.1093/jnci/87.12.902. [DOI] [PubMed] [Google Scholar]
- 38.Rojas M, Alexandrov K, Cascorbi I, Brockmoller J, Likhachev A, Pozharisski K, Bouvier G, Auburtin G, Mayer L, Kopp-Schneider A, Roots I, Bartsch H. High benzo[a]pyrene diol-epoxide DNA adduct levels in lung and blood cells from individuals with combined CYP1A1 MspI/MsPI-GSTM1*0/*0 genotypes. Pharmacogenetics. 1998;8:109–18. [PubMed] [Google Scholar]
- 39.Tang DL, Rundle A, Warburton D, Santella RM, Tsai WY, Chiamprasert S, Hsu YZ, Perera FP. Association between both genetic and environmental biomarkers and lung cancer: evidence of a greater risk of lung cancer in women smokers. Carcinogenesis. 1998;19:1949–53. doi: 10.1093/carcin/19.11.1949. [DOI] [PubMed] [Google Scholar]
- 40.Wei Q, Cheng L, Hong WK, Spitz MR. Reduced DNA repair capacity in lung cancer patients. Cancer Res. 1996;56:4103–7. [PubMed] [Google Scholar]
- 41.Cheng L, Eicher SA, Guo Z, Hong WK, Spitz MR, Wei Q. Reduced DNA capacity in head and neck cancer patients. Cancer Epidemiol Biomarkers Prev. 1998;7:465–8. [PubMed] [Google Scholar]
- 42.Gao YT, Blor WJ, Zheng W, Ershow AG, Hsu CW, Levin LI, Zhang R. FraumeniJr JF. Lung cancer among Chinese women. Int J Cancer. 1987;40:604–9. doi: 10.1002/ijc.2910400505. [DOI] [PubMed] [Google Scholar]
- 43.Hilgers JH. Pterygium: its incidence, heredity and etiology. Am J Ophthalmol. 1960;50:635–44. doi: 10.1016/0002-9394(60)90245-2. [DOI] [PubMed] [Google Scholar]
- 44.Saw SM, Tan D. Pterygium: prevalence, demography and risk factors. Ophthalmic Epidemiol. 1999;6:219–28. doi: 10.1076/opep.6.3.219.1504. [DOI] [PubMed] [Google Scholar]
- 45.Tsai YY, Bau DT, Chiang CC, Cheng YW, Tseng SH, Tsai FJ. Pterygium and genetic polymorphism of DNA double strand break repair gene Ku70. Mol Vis. 2007;13:1436–40. [PubMed] [Google Scholar]
- 46.Tsai YY, Lee H, Tseng SH, Cheng YW, Tsai CH, Wu YH, Tsai FJ. Null type of glutathione S-transferase M1 polymorphism is associated with early onset pterygium. Mol Vis. 2004;10:458–61. [PubMed] [Google Scholar]
- 47.Kerb R, Brockmoller J, Reum T, Roots I. Deficiency of glutathione S-transferases T1 and M1 as heritable factors of increased cutaneous UV sensitivity. J Invest Dermatol. 1997;108:229–32. doi: 10.1111/1523-1747.ep12335337. [DOI] [PubMed] [Google Scholar]
- 48.Halliwell B, Gutteridge JMC. Antioxidant defences. In: Halliwell B, Gutteridge JMC, editors. Free Radicals in Biology and Medicine. 3rd ed. Oxford: Clarendon Press; 1999. p. 105–245. [Google Scholar]
- 49.Strange RC, Lear JT, Fryer AA. Polymorphism in glutathione Stransferase loci as a risk factor for common cancers. Arch Toxicol Suppl. 1998;20:419–28. doi: 10.1007/978-3-642-46856-8_37. [DOI] [PubMed] [Google Scholar]
- 50.Ollier W, Davies E, Snowden N, Alldersea J, Fryer A, Jones P, Strange R. Association of homozygosity for glutathione-S-transferase GSTM1 null alleles with the Ro+/La- autoantibody profile in patients with systemic lupus erythematosus. Arthritis Rheum. 1996;39:1763–4. doi: 10.1002/art.1780391023. [DOI] [PubMed] [Google Scholar]
- 51.Hainaut P, Va¨ha¨kangas K. p53 as a sensor of carcinogenic exposures: mechanisms of p53 protein induction and lessons from p53 gene mutations. Pathol Biol (Paris) 1997;45:833–44. [PubMed] [Google Scholar]
- 52.Wei M, Wanibuchi H, Morimura K, Iwai S, Yoshida K, Endo G, Nakae D, Fukushima S. Carcinogenicity of dimethylarsinic acid in male F344 rats and genetic alterations in induced urinary bladder tumors. Carcinogenesis. 2002;23:1387–97. doi: 10.1093/carcin/23.8.1387. [DOI] [PubMed] [Google Scholar]
- 53.Hollstein M, Sidransky D, Vogelstein B. at al. p53 mutations in human cancers. Science. 1991;253:49–53. doi: 10.1126/science.1905840. [DOI] [PubMed] [Google Scholar]
- 54.Greenblatt MS, Bennett WP, Hollstein M. at al. Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Cancer Res. 1994;54:4855–78. [PubMed] [Google Scholar]
- 55.Hussain SP, Harris CC. Molecular epidemiology of human cancer: contribution of mutation spectra studies of tumor suppressor genes. Cancer Res. 1998;58:4023–37. [PubMed] [Google Scholar]