Abstract
Objective
To study when afterdischarges (ADs) are more likely to occur during cortical stimulation.
Methods
We examined 6,250 electrical stimulation trials in 13 patients with subdural electrodes, studying whether AD occurrence during a trial was influenced by electrode pair stimulated or AD occurrence during the previous trial. In total 545 electrodes were stimulated, 119 frontal (pre-perirolandic), 289 perirolandic, 36 parietal (post-perirolandic), 95 temporal, and 6 occipital.
Results
When the same electrode pair was stimulated as the prior trial, 19% produced ADs compared to 5% of trials when a different electrodes pair was stimulated (p<0.0001). When trials showed ADs, and the next trial stimulated the same electrode pair, ADs occurred in 46% of cases, compared to 13% of trials following trials without ADs (p<0.0001). AD probability decreased with increased inter-trial interval length only when the prior trial was at the same electrode pair and had produced an AD (p=0.001). AD probability increased with stimulation duration, whether the trial followed a trial with (p<0.001) or without (p<0.0001) an AD.
Conclusions
ADs were more likely to occur when an electrode pair showed ADs and was stimulated again, especially when stimulating after short inter-trial intervals or for longer duration.
Significance
When ADs occur, waiting about a minute before resuming stimulation might lessen the likelihood of AD recurrence.
Introduction
Afterdischarges (ADs) are characterized by distinctive rhythmic discharges of spikes and sharp waves that can occur as unwanted side effects after electrical stimulation of a cortical region (Lesser et. al., 1984b;Lesser et. al., 1999;Motamedi et. al., 2002;Blume et. al., 2004;Pouratian et. al., 2004). Stimulating cortical area can produce ADs, sometimes followed by clinical seizures, whether or not that region causes spontaneous seizures (Lesser et al., 1984b;Lesser et al., 1999;Blume et al., 2004;Pouratian et al., 2004). ADs can be used to study corticocortical functional connectivity, patterns of cortical activation (Lesser et. al., 2008), or as a model of human seizures (Lesser et al., 1999).
We previously reported that the electrocorticographic responses to electrical stimulation can fluctuate considerably between repeated trials conducted within the same individual over short periods of time (Lesser et al., 2008). In that study, we observed patterns of ADs over repeated trials and investigated how rapidly response patterns could vary in intact human brain. We found that occurrence of ADs could change within seconds. Also, ADs could occur at a given location during one trial but not the next and they could occur at electrodes adjacent or not adjacent to those directly stimulated.
In this study, we further examined short term changes of cortical responses following stimulation. We examined whether the probability of AD occurrence depended on (1) whether or not there was an AD at the prior trial or (2) whether the prior trial stimulated the same or different electrode pair. We also examined whether the probability of AD occurrence was affected by inter-trial interval length, duration of electrical stimulation, testing session, or by whether stimulated electrodes had shown ictal or interictal epileptiform discharges.
Methods
Patients
We studied 13 patients, in whom subdural electrodes had been implanted for clinical testing, and in whom afterdischarges (ADs) were noted after a run of electrical cortical stimulation given to assist in localizing motor, sensory, or language function. In keeping with our previous report, we call this localization stimulation (LS) (Lesser et al., 1999). Subdural electrodes remained in place in their left hemispheres for several days, with patients in the epilepsy monitoring unit for video-electroencephalography for seizure recordings and for functional mapping using LS (Lesser et. al., 1994). Six patients were male and seven were female. Ages at seizure onset ranged from 14 months to 39 years, and ages at surgery were from 4.7 to 54 years. We previously have described other clinical details regarding these patients (Lesser et al., 2008).
Most testing, and all decisions regarding electrode placement, were based on clinical considerations. All research testing, and the analyses on which this report is based, were approved by our institutional review board.
Electrodes
The subdural electrode arrays we use are 1.5-mm-thick, soft Silastic sheets embedded with platinum-iridium disc electrodes (3-mm total diameter, 2.3-mm diameter exposed to the cortical surface) equally spaced with 1 cm center-to-center distances, in a rectangular or linear array (Adtech, Racine, WI, USA). Electrode position relative to the underlying cortex was determined by direct observation in the operating room (all patients) and by coregistration of pre-implantation volumetric brain magnetic resonance imaging (MRI) (1- to 1.8-mm coronal slice thickness) with post-implantation volumetric brain computed tomography (CT) (1-mm axial slice thickness) in 11 patients according to anatomic fiducials using Curry (Compumedics Neuroscan, El Paso, TX, USA). The electrode positions found with this were displayed with a brain surface rendering, with electrode labelling performed using Photoshop (Adobe Systems, San Jose, California)..
Electroencephalographic (EEG) Recordings
EEGs were recorded on a digital electroencephalogram (Telefactor Twin, Astro-Med, Inc., West Warwick, RI, USA) that could simultaneously record up to 128 channels, with 200 samples per second per channel. Low pass filter was set to 70 Hz and high pass to 0.3 Hz (−3 dB).
Electrical Cortical Stimulation
Testing of motor, sensory or language functions occurred over 1–5 sessions. One testing session was in the morning and another in the afternoon. Within each session, there was a sequence of trials, each trial characterized by electrical stimulation of a pair of electrodes followed by observation of the effects of this stimulation on the patient. Testing used biphasic, charge balanced, square wave pulses of 0.3 millisecond duration, repeated at 50 Hz and presented in trains lasting 4 to 5 seconds, with the first 0.3 millisecond positive pulse immediately followed by a 0.3 millisecond pulse of opposite polarity (Grass S12 stimulator; Astro-Med, Inc., West Warwick, RI). In general, stimulation was between pairs of adjacent electrodes, using methods previously described (Lesser et al., 1984b;Lesser et al., 1994;Lesser et al., 1999;Pouratian et al., 2004).
A total of 1156 electrodes had been implanted, 352 in frontal lobe anterior to the perirolandic region, 392 in the perirolandic region, 152 in the parietal lobe posterior to the perirolandic region, 252 in the temporal lobe, and 8 in the occipital lobe. Stimulation was performed on 545 electrodes, 119 frontal (pre-perirolandic), 289 perirolandic, 36 parietal (post-perirolandic), 95 temporal, and 6 occipital. A previous report found that AD thresholds differences vary considerably throughout the brain, by as much as 9.5, 8, and 12 mA between adjacent electrodes and by as much as 11, 8, and 12 mA in individual patients in the frontal, parietal, and temporal lobes respectively.(Lesser et al., 1984b)
Although the characteristics of ADs are the focus of this paper, from the clinical perspective we hope to avoid their occurrence and minimize their duration (Lesser et al., 1999). To do this, we start at 0.5 – 1 mA, increasing in steps of 0.5–1 mA until motor or sensory changes occur, but decreasing by 0.5 – 1 mA if ADs occur, in an effort to avoid further ADs.(Lesser et. al., 1984a;Lesser et. al., 1987;Jayakar et. al., 1992;Lesser et al., 1994;Jayakar and Lesser RP, 1997;Lesser et al., 1999) There was no precise timing for the interval between trials. This might increase, for example, if the patient had a question, or wanted to relax for a moment before resuming testing. It might also be longer if one of the testing personnel needed to adjust the testing equipment, or make notes about the testing. Finally, if ADs occurred, the next trial didn’t occur until they stopped.
Only one of the 13 patients experienced an AD during the first trial of a session, and this only occurred during one out of four sessions for that individual. The remaining analyses therefore were restricted to subsequent trials only. For instance, if a session was 3 hours long, running from 13:00 – 16:00 hours, only the one at 13:00 was the first trial and all the others were subsequent trials, and these were the ones we further analyzed. We analyzed what occurs among all the testing sessions. For example, there could be session 1 on Monday morning, session 2 Monday afternoon, session 3 Tuesday morning.
EEG Analysis
We used previous definitions and descriptions of ADs (Lesser et al., 1999;Blume et al., 2004). In summary, ADs vary in morphology but can occur as spikes, polyspikes, spike-and-slow-wave complexes, or rhythmic sinusoidal or semi-sinusoidal discharges.(figure 1) We reviewed EEGs on a locally developed EEG viewer that displayed up to 128 channels simultaneously, and allowed us to mark the location of ADs and other events as precisely as desired. Preliminary assessments of portions of the recordings were performed by several individuals, but one board certified electroencephalographer (RPL) performed the final markings of all recordings.
Figure 1.
Example of afterdischarges. The first three seconds show the baseline EEG. Then cortical stimulation occurs for slightly less than five seconds. Then ADs occur on both channels. Afterdischarges vary in morphology and examples of other morphologies have been published previously. (Lesser et al., 1999;Motamedi et al., 2002;Blume et al., 2004)
We found that there were times when it was difficult to decide whether a particular waveform was, or was not an AD. Because of this, although preliminary assessments of portions of the recordings were performed by several individuals, one board certified electroencephalographer (RPL) performed the final markings of all recordings. We discussed previously (Lesser et al., 2008) that it can be difficult to decide whether an individual EEG waveform is, or is not, an AD, and there are a number of articles in the literature that describe difficulties in classifying individual events and findings, not only with EEG (Williams et. al., 1985;Williams et. al., 1990;Webber et. al., 1993) including computer based EEG analysis (Webber et. al., 1994), but also with polysomnography (Ferri et. al., 1989), electrocardiography (Eddy, 1988), radiologic imaging (Revesz and Kundel, 1977;Beam et. al., 2003), and clinical observation (Eddy, 1988;Groopman, 2007). Because of this, in our previous study, RPL marked the entire data set twice.(Lesser et al., 2008) We found differences between the two reviews for 257 out of 11,944 events marked, but there were no differences in the conclusions with or without the 257 events. These differences, however, regarded whether there were ADs on a particular channel. There were no differences regarding whether ADs occurred at a particular time, and this was what we investigated in the present study.
After stimulation occurs, there can be “blocking,” saturation of the amplifiers for a period of time, and this can obscure any ADs that might be present. This could last for several seconds on the channels actually stimulated. For this reason we could not know whether ADs occurred on the stimulated channels until the saturation cleared.
Statistical Analysis
We calculated the number and percentage of trials that produced ADs by whether the trial was a first or subsequent trial in a session, and for subsequent trials, whether the prior trial stimulated the same or a different electrode pair and whether the prior trial produced an AD. We also recorded the sites where spontaneous epileptiform activity occurred, and determined whether such activity was more likely at sites where ADs occurred.
We used logistic regression to examine whether the probability of a trial producing any ADs depended on whether the same electrode pair was stimulated as the prior trial within a session and whether that prior trial produced ADs. Logistic regression models included the patient identification number as a fixed effect and were fit using generalized estimating equations (GEE) to take into account possible correlation among trials for which the same channel pair was stimulated (Lesser et al., 1999).
Inter-trial interval length (length from end of immediately prior trial to start of current trial) and LS duration were calculated for each of the following conditions: (1) same electrode pair as prior trial, no AD at prior trial, (2) same electrode pair, AD at prior trial, (3) new electrode pair, no AD at prior trial, and (4) new electrode pair, AD at prior trial. We plotted the probability of an AD by the inter-trial interval length, with separate smoothed lines fit for each patient. We fit logistic regression models to examine whether the probability of a trial producing any ADs depended on inter-trial interval length or LS duration, conditional on whether the trial was at the same electrode pair as the prior trial or a new electrode pair and whether or not the prior trial produced ADs. Models included the patient identification number as a fixed effect, and were fit using GEE to take into account possible correlation among trials for which the same channel pair was stimulated.
We used logistic regression fit via GEE to examine whether there was an increase or decrease in the overall probability of ADs over testing sessions after adjusting for whether the prior trial stimulated the same or a different electrode pair and whether the prior trial produced an AD. We also used logistic regression fit via GEE to examine whether there was an increase or decrease in the overall probability of ADs when the stimulated channels were at locations where there were epileptiform discharges, compared to locations where there were no epileptiform discharges. We evaluated sites where epileptiform discharges were ictal only, interictal only, or both ictal and interictal,
All tests were two-sided with an alpha level of 0.05 used to determine statistical significance. From the logistic regression models, we report odds ratio (OR) along with 95% confidence intervals (CI) and p-values.
Results
The number of sessions per patient ranged from 1 to 5 and the number of trials per patient ranged from 71 to 1,206. Total testing time for the entire admission ranged from 48–370 minutes per patient. There were a total of 6,250 trials included for the analysis. Of these, 41 were the first trial of a session, and the other 6,209 were subsequent trials. Among all 6,250 trials, 18% produced ADs (Table 1A). For the 41 first trials of a session, ADs were observed during only 1 trial (2%).
Table 1.
(A) Percentage of trials with ADs during all trials or during the first trials of testing sessions. (B) Percentage of subsequent trials with ADs, divided by those with and those without ADs during the immediately prior trial. (C) Percentage of subsequent trials with ADs, divided into those for which the same pair of electrodes was stimulated as during the immediately preceding trial and those during wich a different pair was stimulated. (D) Percentage of subsequent trials as in C, further separated into those with or without ADs during the immediately preceding trial.
| A |
B |
C |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | First | AD prior trial | No AD prior trial | Subsequent - Same Pair | Subsequent - Different Pair | |||||||
| Patient | N | AD% | N | AD% | N | AD% | N | AD% | N | AD% | N | AD% |
| All | 6,250 | 18% | 41 | 2% | 1,139 | 43% | 5,070 | 13% | 5,960 | 19% | 249 | 5% |
| P#01 | 312 | 18% | 4 | 0% | 53 | 43% | 255 | 13% | 302 | 19% | 6 | 0% |
| P#02 | 239 | 12% | 1 | 0% | 28 | 11% | 210 | 12% | 232 | 12% | 6 | 0% |
| P#03 | 602 | 54% | 3 | 0% | 324 | 68% | 275 | 38% | 580 | 56% | 19 | 5% |
| P#04 | 670 | 17% | 5 | 0% | 113 | 28% | 552 | 15% | 645 | 18% | 20 | 10% |
| P#05 | 454 | 17% | 2 | 0% | 79 | 38% | 373 | 13% | 436 | 18% | 16 | 13% |
| P#06 | 74 | 41% | 1 | 0% | 29 | 38% | 44 | 43% | 72 | 42% | 1 | 0% |
| P#07 | 797 | 8% | 5 | 0% | 65 | 23% | 727 | 7% | 729 | 9% | 63 | 3% |
| P#08 | 445 | 15% | 5 | 0% | 65 | 52% | 375 | 9% | 412 | 16% | 28 | 7% |
| P#09 | 122 | 13% | 4 | 0% | 14 | 43% | 104 | 10% | 110 | 14% | 8 | 13% |
| P#10 | 71 | 25% | 1 | 0% | 18 | 17% | 52 | 29% | 65 | 26% | 5 | 20% |
| P#11 | 275 | 22% | 2 | 0% | 59 | 53% | 214 | 14% | 265 | 22% | 8 | 13% |
| P#12 | 1,206 | 11% | 4 | 0% | 126 | 25% | 1,076 | 9% | 1,174 | 11% | 28 | 0% |
| P#13 | 983 | 17% | 4 | 25% | 166 | 33% | 813 | 14% | 938 | 18% | 41 | 0% |
| D | ||||||||
|---|---|---|---|---|---|---|---|---|
| Subsequent - Same Pair | Subsequent - Different Pair | |||||||
| AD prior trial | No AD prior trial | AD prior trial | No AD prior trial | |||||
| Patient | N | AD% | N | AD% | N | AD% | N | AD% |
| All | 1,076 | 46% | 4,884 | 13% | 63 | 8% | 186 | 4% |
| P#01 | 49 | 47% | 253 | 13% | 4 | 0% | 2 | 0% |
| P#02 | 27 | 11% | 205 | 12% | 1 | 0% | 5 | 0% |
| P#03 | 311 | 71% | 269 | 39% | 13 | 0% | 6 | 17% |
| P#04 | 106 | 29% | 539 | 15% | 7 | 14% | 13 | 8% |
| P#05 | 75 | 37% | 361 | 14% | 4 | 50% | 12 | 0% |
| P#06 | 28 | 39% | 44 | 43% | 1 | 0% | 0 | N/A |
| P#07 | 56 | 27% | 673 | 7% | 9 | 0% | 54 | 4% |
| P#08 | 60 | 55% | 352 | 9% | 5 | 20% | 23 | 4% |
| P#09 | 10 | 50% | 100 | 10% | 4 | 25% | 4 | 0% |
| P#10 | 18 | 17% | 47 | 30% | 0 | N/A | 5 | 20% |
| P#11 | 57 | 54% | 208 | 13% | 2 | 0% | 6 | 17% |
| P#12 | 120 | 27% | 1,054 | 9% | 6 | 0% | 22 | 0% |
| P#13 | 159 | 35% | 779 | 14% | 7 | 0% | 34 | 0% |
Total = total number of trials.
First = first trial of each session (If a testing session lasted from 1300–1600 hours only the one at 1300 hours is the first trial).
Subsequent – trials that were not a session’s first trial, as defined just above.
“Same Pair” / “Different Pair” = electrode pairs stimulated was same as / different from the immediately preceding trial.
N=number of trials;
AD% = percent of the trials listed under N with ADs, for example 18% of 6250 trials.
“AD prior trial”, “No AD prior trial” refers to the immediately preceding trial.
We found that 43% of the 1,139 trials following a prior trial with an AD resulted in an AD compared to only 13% of the 5,070 trials following a prior trial without an AD (Table 1B, OR = 5.1, 95% CI = 3.4 to 7.8, p<0.0001). For the 6,209 subsequent trials within a session, ADs were more likely to occur if the same electrode pair was stimulated as during the prior trial or if the trial followed a trial that produced an AD (Table 1C). Among the 5,960 trials during which the same electrode pair was stimulated as the prior trial, 19% produced ADs compared to only 5% of the 249 trials during which a different pair of electrodes were stimulated compared to the prior trial (OR = 4.7, 95% CI = 2.4 to 9.1, p<0.0001).
Trials following a trial that resulted in an AD were significantly more likely to produce an AD if the same electrode pair was stimulated. We divided the 5,960 subsequent trials during which the same electrode pair was stimulated as in the prior trial into those where the prior trial did not produce an AD, and those where the prior trial produced an AD (Table 1D). For subsequent trials for which the same electrode pair was stimulated as the prior trial, 46% of the 1,076 trials following a prior trial with an AD resulted in an AD compared to only 13% of the 4,884 trials following a prior trial without an AD (OR = 5.4, 95% CI = 3.4 to 8.4, p<0.0001).
For the other 249 trials where a new electrode pair was stimulated compared to the prior trial (Table 1D), the odds of having an AD was almost twice as large if there was an AD at the prior trial; however, this was not statistically significant (8% of 63 trials with a prior AD vs. 4% of 186 trials without an AD, OR = 2.2, 95% CI = 0.62 to 7.8, p=0.22).
As might be expected, the length of inter-trial intervals (time from the end of one stimulation trial to the start of the next stimulation trial) was shorter when testing was performed at the same electrode pair as the prior trial and when the prior trial did not have an AD (Table 2A). When testing was performed at the same electrode pair, more than 95% of trials started less than a minute after the end of the prior trial, though trial lengths were somewhat longer when they followed a trial with an AD. For example, the inter-trial interval length was less than 10 seconds for 61% of trials at the same electrode pair when there was not an AD at the prior trial, compared to only 31% of trials when testing was done at the same electrode pair but there was an AD at the prior trial. When testing was performed at a new electrode pair, 30% of trials began 150 seconds or longer after the prior trial when there was no AD, compared to 43% of trials following a trial with an AD. This is most likely because testers wait until the ADs stop before starting a new test, and this adds time to that taken to switch the electrode pairs.
Table 2.
(A) Intertrial interval length by whether the trial was at the same electrode pair as the immediately prior trial or a new electrode pair (same vs. new) and whether or not that prior trial produced ADs. (B) Relationship between intertrial interva
| A | ||||||||||||||
| Same Electrode Pair | ||||||||||||||
| Intertrial interval | <10 sec | 10–19 sec | 20–39 sec | 40–59 sec | 60–79 sec | 80+ sec | All | <1 min | ||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| No AD during prior trial | 2,992 | 61% | 1,282 | 26% | 433 | 9% | 111 | 2% | 22 | 0.5% | 44 | 0.9% | 4,884 | 99% |
| AD during prior trial 3 | 337 | 31% | 358 | 33% | 251 | 23% | 77 | 7% | 34 | 3% | 19 | 2% | 1,076 | 95% |
| New Electrode Pair | ||||||||||||||
| <30 sec | 30–59 sec | 60–89 sec | 90–119 sec | 120–149 sec | 150+ sec | All | <1 min | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| No AD during prior trial | 11 | 6% | 23 | 12% | 52 | 28% | 32 | 17% | 12 | 6% | 56 | 30% | 186 | 18% |
| AD during prior trial 3 | 1 | 2% | 2 | 3% | 11 | 17% | 12 | 19% | 10 | 16% | 27 | 43% | 63 | 5% |
| B | ||||||||||||||
| Same Electrode Pair | ||||||||||||||
| <10 sec | 10–19 sec | 20–39 sec | 40–59 sec | 60–79 sec | 80+ sec | |||||||||
| N | AD% | N | AD% | N | AD% | N | AD% | N | AD% | N | AD% | |||
| No AD at prior trial | 2,992 | 12% | 1,282 | 16% | 433 | 15% | 111 | 15% | 22 | 32% | 44 | 14% | ||
| AD at prior trial | 337 | 59% | 358 | 47% | 251 | 32% | 77 | 34% | 34 | 29% | 19 | 42% | ||
| New Electrode Pair | ||||||||||||||
| <30 sec | 30–59 sec | 60–89 sec | 90–119 sec | 120–149 sec | 150+ sec | |||||||||
| N | AD% | N | AD% | N | AD% | N | N | N | AD% | N | AD% | |||
| No AD at prior trial 3 | 11 | 18% | 23 | 9% | 52 | 0% | 32 | 0% | 12 | 0% | 56 | 5% | ||
| AD at prior trial | 1 | 0% | 2 | 0% | 11 | 9% | 12 | 8% | 10 | 20% | 27 | 4% | ||
Same / New Electrode Pair - same / new electrode pair, compared to the immediately prior trial.
Sec = second; min = minutes
No AD / AD during prior trial refers to the immediately prior trial.
All = all trials regardless of inter-trial interval. < 1 minute = all inter-trial intervals less than one minute.
Table 2(A) is simply descriptive and there is no statistical test performed, as the differences are simply due to how the testing occurs: we wait longer before starting the next trial when there are ADs.
Figure 2 and Table 2B show the probability of an AD by the inter-trial interval length, with separate lines for each patient. The probability of an AD depended significantly on the inter-trial interval length only when the prior trial was at the same electrode pair and had produced an AD (p=0.001) (Figure 2A). In this case, the probability of another AD decreased as inter-trial interval length increased (OR = 0.45, 95% CI = 0.25 to 0.79, p=0.005). For subsequent trials at the same electrode pair when the prior trial did not have an AD, the probability of an AD did not depend on the inter-trial interval length (p=0.16, Figure 2B). For trials at a new electrode pair, the probability of an AD did not depend on inter-trial interval length, regardless of whether the prior trial had an AD (p=0.58) or not (p=0.42) (Figure 2C).
Figure 2.

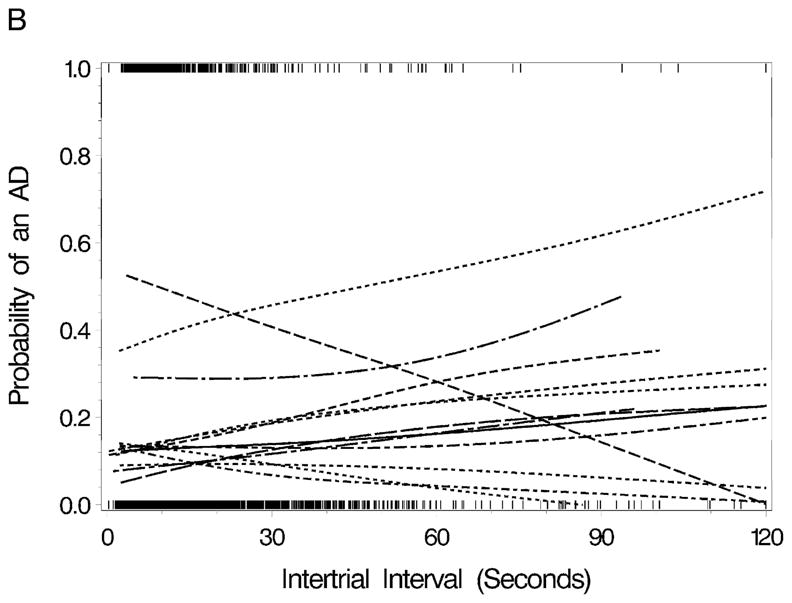
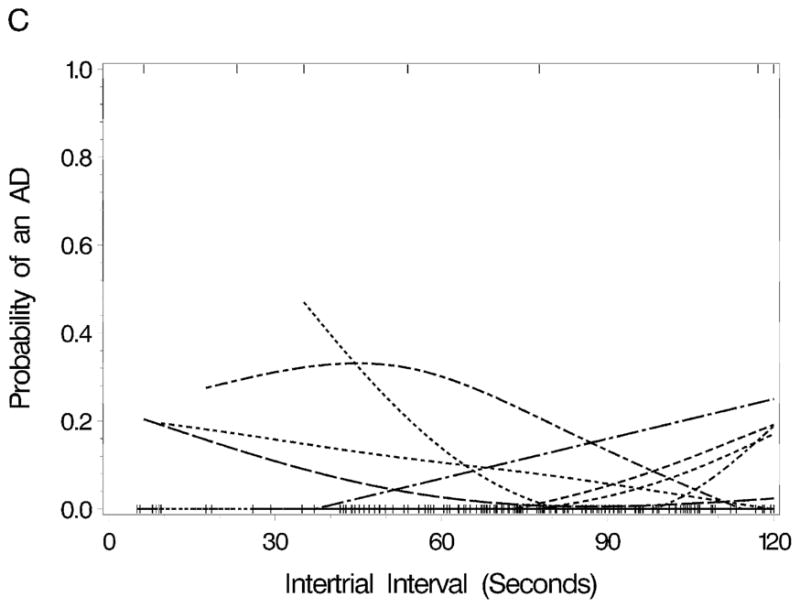
Probability of an AD by the inter-trial interval length with separate lines for each patient. (A) Inter-trial interval with trials at the same electrode pair as during the immediately preceding trial and an AD occurred at the previous trial, (B) inter-trial interval with trials at the same electrode pair as during the immediately preceding trial and when ADs did not occur at the previous trial, and (C) inter-trial interval when the electrode pair stimulated differed from the pair during the immediately preceding trial. Some lines in C have only or primarily zero values, and therefore overlap one another at the bottom of the figure. The lines were created using smoothing splines. The tics at the top and bottom of the graphs show each observation. A tic at the top of the graph corresponds to a trial with an AD, whereas a tic at the bottom of the graph corresponds to a trial without an AD.
The LS duration ranged from 1 to 5.5 seconds, and tended to be longer when the same electrode pair was stimulated following a trial with an AD as follows:
Same electrode pair, no AD at prior trial: median = 2.2, range = 1.0–5.5 seconds
Same electrode pair, AD at prior trial: median = 3.1, range = 1.0–5.4 seconds
New electrode pair, no AD at prior trial: median = 2.0, range = 1.0–4.8 seconds
New electrode pair, AD at prior trial: median = 2.0, range = 1.1–4.8 seconds
The probability of ADs increased with increasing LS duration most strongly for trials at a new electrode pair compared to the prior trial (OR = 4.5, 95% CI = 1.5 to 13.3, p=0.0068). This relationship did not depend on whether the prior trial produced ADs (p=0.78). In contrast, for trials performed at the same electrode pair as the prior trial, there was a significant interaction between the LS duration and whether the prior trial produced ADs (p=0.0015), where the positive association between the LS duration and the probability of an AD was stronger when the trial followed a trial without an AD (OR=1.70, 95% CI = 1.54 to 1.89, p<0.0001) compared to when the trial followed a trial with an AD (OR = 1.51, 95% CI = 1.33 to 1.72, p<0.001).
After adjusting for whether testing was done at the same or a different electrode pair as the prior trial and whether or not there was an AD at the prior trial, there was no association between the probability of an AD and the session during which the AD occurred either within a day (OR = 1.05, 95% CI = 0.81 to 1.35, p=0.74) or over all days (OR = 0.95, 95% CI = 0.85 to 1.06, p=0.37). There was no association between the probability of an AD and the trial number within a session (OR = 1.0, 95% CI = 0.998 to 1.001, p=0.29) or within a day (OR = 1.0, 95% CI = 0.9992 to 1.001, p=0.81).
ADs occurred more often when the stimulated channels were at locations where the only epileptiform discharges seen were ictal epileptiform discharges (OR vs. no discharges= 1.84, 95% CI = 1.08 to 3.16, p=0.026); however, there was no increased risk of ADs at locations with interictal epileptiform discharges only (OR vs. no discharges = 0.98, 95% CI = 0.62 to 1.15, p=0.93) or where both ictal and interictal epileptiform discharges occurred (OR vs. no discharges = 1.81, 95% CI = 0.85 to 3.92, p=0.13). At locations with only ictal epileptiform discharges, ADs occurred during 27% of the trials, compared to 21% of trials at locations with both ictal and interictal epileptiform discharges, 16% of trials at locations with only interictal epileptiform discharges, and 17% of trials with neither ictal nor interictal epileptiform discharges.
Discussion
Cortical stimulation is used clinically to localize regions important for motor, sensory, language or other functions. When setting up procedures for this, accuracy, safety and efficiency all are important. For accuracy, testing to be done carefully, using optimized testing parameters. To improve safety, we would like to take care to avoid causing seizures with the electrical stimulation used for testing. However, efficiency implies that testing should be done as quickly as feasible. There are tradeoffs among these.
First, we found that, once ADs occurred during stimulation of a pair of electrodes, they were more likely to recur on the next trial at that pair. As mentioned in the Methods, our practice is to reduce stimulus intensity by 0.5 – 1 mA when ADs occur, but ADs could recur despite this. In a sense, each electrode pair served as its own control. There were no ADs at a given current intensity or set of intensities, then ADs occurred at another intensity, and when ADs occurred, they could continue to occur despite reduction in stimulation intensity. Second, in these cases, increasing the inter-trial interval helped to decrease the likelihood of AD recurrence. These two findings are consistent with the idea that cortical stimulation increased excitability, but also suggest that this increase was limited in duration. Third, increased stimulus duration increased the likelihood of ADs only when there hadn’t been an AD during the previous trial. Put another way, this suggests that once the level of excitability had increased in the activated cortical region, to the point that ADs occurred, changes of stimulus duration, at least those within the range we used, didn’t further increase excitability. They did not appear to be an additive effect for the coincidence of stimulating at the same electrode pair as during the previous trial, plus the occurrence of ADs during the previous trial. This could have been a sampling effect, since stimulating a new pair of electrodes was less common than stimulating the same pair of electrodes. Also, we begin stimulating a new pair of electrodes at low intensity, so ADs are less likely during the initial trial at an electrode pair in any case.
Changes in the level of activation of cortical cells, or in the occurrence of refractory periods, occur due to changes in ion channel activity and in the balance between intracellular and extracellular ion concentrations, these in turn occurring in large part due to neurotransmitter release, and resulting both in changes to the synaptic strength of existing connections and in the functional state of these connections, both locally and in multiple regions throughout the cortex (Buonomano and Merzenich, 1998;Sanes and Donoghue, 2000;Sjostrom and Nelson, 2002;Sheng and Kim, 2002;Nudo, 2003;Shu et. al., 2003;Destexhe and Marder, 2004;Abbott and Regehr, 2004;Chklovskii et. al., 2004;Feldman and Brecht, 2005;Pinto et. al., 2005;Haider et. al., 2007). The variations of excitability which we found can occur in awake humans under apparently stable conditions (Destexhe and Contreras, 2006;Haider et al., 2007), and can occur in response to stimulation (Lee et. al., 2003;Lesser et al., 2008). Normally these may be important in facilitating cortical plasticity (Duffau, 2006;Lesser et al., 2008). In any case, it seems likely that all of these factors could have affected whether ADs occurred or did not occur during individual trials. In some cases, the tested regions might simply have been refractory to stimulation, due to the ADs that had just occurred. Also, other changes in the strength of connections within or between regions of the cortex might have resulted in changes in AD occurrence or recurrence.
The on-again, off-again, then on-again activation patterns we found seem best explained by alterations in neuronal excitability or refractory periods, in synaptic strengths of existing connections (Buonomano et al., 1998;Abbott et al., 2004;Chklovskii et al., 2004), or in the functional state of the network as a whole (Buonomano et al., 1998;Sanes et al., 2000;Nudo, 2003;Haider et al., 2007), and are consistent with the idea that rapid adaptive mechanisms can be present in the cerebral cortex of an awake human, even during apparently stable conditions (Destexhe et al., 2006;Haider et al., 2007) Perhaps neuronal activity can act as a gate or switch, preventing ADs on some occasions and allowing them on others. Changes in the neuronal processes underlying learning can occur over days or weeks. However, in theory, some adjustments in neuronal function should occur continuously, with adaptations to synaptic inputs occurring over seconds to minutes (Stemmler and Koch, 1999). The mechanisms underlying these changes are unknown: they could be due to random fluctuations in thresholds of neuronal activity, a use dependent plastic process, or a deterministic process, not presently understood. Factors such as attention or activity levels, blood flow, cortical and subcortical neuromodulation, and metabolic fluctuations all could influence these changes.
Our principle findings should be taken in the context of the parameters actually used in our laboratory. Also, one should keep in mind that saturation of the amplifiers (“blocking”) occurs for a period of seconds after stimulation, and ADs occurring during blocking might be missed. Because of this, our findings are relevant to circumstances in which ADs are seen, but might not be relevant to circumstances in which they are not seen. However, the parameters we used are similar to those reported by others, and so are likely to be applicable to cortical stimulation testing performed elsewhere.
It also would be important to assess the effects of current and voltage on ADs, but at the time these data were collected, we recorded current (the Grass S12 is a constant current stimulator) but did not assess voltage (which of course might vary), and both would be needed for proper analysis. We now have a system that records both current and voltage, and plan to report an analysis of the effects of these on AD occurrence in the future.
In summary, from the practical point of view, our findings suggest that, when ADs occur, and they don’t respond to other means of terminating them, such as brief pulse stimulation, waiting about a minute before resuming stimulation-based testing might lesson the likelihood of AD recurrence.
Acknowledgments
Hyang Woon Lee was supported by the Korea Science and Engineering Foundation (KOSEF) Grant funded by the Korean Government (MOST) (No. R01-2007-000-11080-0) and the Korea Research Foundation Grant funded by the Korean Government (MEST) (KRF-2009-007-2164). Nathan E. Crone was supported by grant NINDS R01NS40596 from the National Institutes of Health. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines. None of the authors has any conflict of interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Abbott LF, Regehr WG. Synaptic computation. Nature. 2004;431:796–803. doi: 10.1038/nature03010. [DOI] [PubMed] [Google Scholar]
- 2.Beam CA, Conant EF, Sickles EA. Association of volume and volume-independent factors with accuracy in screening mammogram interpretation. J Natl Cancer Inst. 2003;95:282–290. doi: 10.1093/jnci/95.4.282. [DOI] [PubMed] [Google Scholar]
- 3.Blume WT, Jones DC, Pathak P. Properties of after-discharges from cortical electrical stimulation in focal epilepsies. Clin Neurophysiol. 2004;115:982–989. doi: 10.1016/j.clinph.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 4.Buonomano DV, Merzenich MM. Cortical plasticity: from synapses to maps. Annu Rev Neurosci. 1998;21:149–86. 149–186. doi: 10.1146/annurev.neuro.21.1.149. [DOI] [PubMed] [Google Scholar]
- 5.Chklovskii DB, Mel BW, Svoboda K. Cortical rewiring and information storage. Nature. 2004;431:782–788. doi: 10.1038/nature03012. [DOI] [PubMed] [Google Scholar]
- 6.Destexhe A, Contreras D. Neuronal computations with stochastic network states. 2006. [DOI] [PubMed] [Google Scholar]
- 7.Destexhe A, Marder E. Plasticity in single neuron and circuit computations. Nature. 2004;431:789–795. doi: 10.1038/nature03011. [DOI] [PubMed] [Google Scholar]
- 8.Duffau H. Brain plasticity: from pathophysiological mechanisms to therapeutic applications. J Clin Neurosci. 2006;13:885–897. doi: 10.1016/j.jocn.2005.11.045. [DOI] [PubMed] [Google Scholar]
- 9.Eddy D. Variations in physician practice: The role of uncertainty. In: Dowie J, Elstein A, editors. Professional judgment : a reader in clinical decision making. Cambridge University Press; Cambridge, New York: 1988. pp. 45–59. [Google Scholar]
- 10.Feldman DE, Brecht M. Map plasticity in somatosensory cortex. Science. 2005;310:810–815. doi: 10.1126/science.1115807. [DOI] [PubMed] [Google Scholar]
- 11.Ferri R, Ferri P, Colognola RM, Petrella MA, Musumeci SA, Bergonzi P. Comparison between the results of an automatic and a visual scoring of sleep EEG recordings. 1989. [PubMed] [Google Scholar]
- 12.Groopman J. How Doctors Think. Houghton Mifflin Company; Boston, New York: 2007. The Eye of the Beholder; pp. 177–202. [Google Scholar]
- 13.Haider B, Duque A, Hasenstaub AR, Yu Y, McCormick DA. Enhancement of visual responsiveness by spontaneous local network activity in vivo. 2007. [DOI] [PubMed] [Google Scholar]
- 14.Jayakar P, Alvarez LA, Duchowny MS, Resnick TJ. A safe and effective paradigm to functionally map the cortex in childhood. J Clin Neurophysiol. 1992;9:288–293. doi: 10.1097/00004691-199204010-00009. [DOI] [PubMed] [Google Scholar]
- 15.Jayakar P, Lesser RP. Extraoperative Methods. In: Engel J Jr, Pedley TA, editors. Epilepsy A Comprehensive Textbook. Lipppincott-Raven; Philadelphia-New York: 1997. pp. 1785–1793. [Google Scholar]
- 16.Lee L, Siebner HR, Rowe JB, Rizzo V, Rothwell JC, Frackowiak RS, Friston KJ. Acute remapping within the motor system induced by low-frequency repetitive transcranial magnetic stimulation. J Neurosci. 2003;23:5308–5318. doi: 10.1523/JNEUROSCI.23-12-05308.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lesser R, Gordon B, Uematsu S. Electrical stimulation and language. J Clin Neurophysiol. 1994;11:191–204. doi: 10.1097/00004691-199403000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Lesser RP, Kim SH, Beyderman L, Miglioretti DL, Webber WRS, Bare M, Cysyk B, Krauss G, Gordon B. Brief bursts of pulse stimulation terminate afterdischarges caused by cortical stimulation. Neurology. 1999;53:2073–2081. doi: 10.1212/wnl.53.9.2073. [DOI] [PubMed] [Google Scholar]
- 19.Lesser RP, Lee HW, Webber WR, Prince B, Crone NE, Miglioretti DL. Short-term variations in response distribution to cortical stimulation. Brain. 2008;131:1528–1539. doi: 10.1093/brain/awn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lesser RP, Lüders H, Dinner DS, Hahn JF, Cohen L. The location of speech and writing functions in the frontal language area. Results of extraoperative cortical stimulation. Brain. 1984a;107:275–291. doi: 10.1093/brain/107.1.275. [DOI] [PubMed] [Google Scholar]
- 21.Lesser RP, Luders H, Klem G, Dinner DS, Morris HH, Hahn J. Cortical afterdischarge and functional response thresholds: results of extraoperative testing. Epilepsia. 1984b;25:615–621. doi: 10.1111/j.1528-1157.1984.tb03471.x. [DOI] [PubMed] [Google Scholar]
- 22.Lesser RP, Lüders H, Klem G, Dinner DS, Morris HH, Hahn JF, Wyllie E. Extraoperative cortical functional localization in patients with epilepsy. J Clin Neurophysiol. 1987;4:27–53. doi: 10.1097/00004691-198701000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Motamedi GK, Lesser RP, Miglioretti DL, Mizuno-Matsumoto Y, Gordon B, Webber WR, Jackson DC, Sepkuty JP, Crone NE. Optimizing parameters for terminating cortical afterdischarges with pulse stimulation. Epilepsia. 2002;43:836–846. doi: 10.1046/j.1528-1157.2002.24901.x. [DOI] [PubMed] [Google Scholar]
- 24.Nudo RJ. Adaptive plasticity in motor cortex: implications for rehabilitation after brain injury. J Rehabil Med. 2003:7–10. doi: 10.1080/16501960310010070. [DOI] [PubMed] [Google Scholar]
- 25.Pinto DJ, Patrick SL, Huang WC, Connors BW. Initiation, propagation, and termination of epileptiform activity in rodent neocortex in vitro involve distinct mechanisms. J Neurosci. 2005;25:8131–8140. doi: 10.1523/JNEUROSCI.2278-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pouratian N, Cannestra AF, Bookheimer SY, Martin NA, Toga AW. Variability of intraoperative electrocortical stimulation mapping parameters across and within individuals. J Neurosurg. 2004;101:458–466. doi: 10.3171/jns.2004.101.3.0458. [DOI] [PubMed] [Google Scholar]
- 27.Revesz G, Kundel HL. Psychophysical studies of detection errors in chest radiology. Radiology. 1977;123:559–562. doi: 10.1148/123.3.559. [DOI] [PubMed] [Google Scholar]
- 28.Sanes JN, Donoghue JP. Plasticity and primary motor cortex. Annu Rev Neurosci. 2000;23:393–415. doi: 10.1146/annurev.neuro.23.1.393. [DOI] [PubMed] [Google Scholar]
- 29.Sheng M, Kim MJ. Postsynaptic signaling and plasticity mechanisms. Science. 2002;298:776–780. doi: 10.1126/science.1075333. [DOI] [PubMed] [Google Scholar]
- 30.Shu Y, Hasenstaub A, McCormick DA. Turning on and off recurrent balanced cortical activity. Nature. 2003;423:288–293. doi: 10.1038/nature01616. [DOI] [PubMed] [Google Scholar]
- 31.Sjostrom PJ, Nelson SB. Spike timing, calcium signals and synaptic plasticity. Curr Opin Neurobiol. 2002;12:305–314. doi: 10.1016/s0959-4388(02)00325-2. [DOI] [PubMed] [Google Scholar]
- 32.Stemmler M, Koch C. How voltage-dependent conductances can adapt to maximize the information encoded by neuronal firing rate. Nat Neurosci. 1999;2:521–527. doi: 10.1038/9173. [DOI] [PubMed] [Google Scholar]
- 33.Webber WR, Litt B, Lesser RP, Fisher RS, Bankman I. Automatic EEG spike detection: what should the computer imitate? Electroencephalogr. Clin Neurophysiol. 1993;87:364–373. doi: 10.1016/0013-4694(93)90149-p. [DOI] [PubMed] [Google Scholar]
- 34.Webber WR, Litt B, Wilson K, Lesser RP. Practical detection of epileptiform discharges (EDs) in the EEG using an artificial neural network: a comparison of raw and parameterized EEG data. Electroencephalogr Clin Neurophysiol. 1994;91:194–204. doi: 10.1016/0013-4694(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 35.Williams GW, Lesser RP, Silvers JB, Brickner A, Goormastic M, Fatica KJ, Klass DW. Clinical diagnoses and EEG interpretation. Cleve Clin J Med. 1990;57:437–440. doi: 10.3949/ccjm.57.5.437. [DOI] [PubMed] [Google Scholar]
- 36.Williams GW, Lüders H, Brickner A, Goormastic M, Klass DW. Interobserver variability in EEG interpretation. Neurology. 1985;35:1714–1719. doi: 10.1212/wnl.35.12.1714. [DOI] [PubMed] [Google Scholar]



