Abstract
Delayed gastric emptying in the absence of mechanical obstruction is referred to as gastroparesis. Symptoms that are often attributed to gastroparesis include postprandial fullness, nausea, and vomiting. Although tests of gastric motor function may aid diagnostic labeling, their contribution to determining the treatment approach is often limited. Although clinical suspicion of gastroparesis warrants the exclusion of mechanical causes and serum electrolyte imbalances, followed by empirical treatment with a gastroprokinetic such as domperidone or metoclopramide, evidence that these drugs are effective for patients with gastroparesis is far from overwhelming. In refractory cases with severe weight loss, invasive therapeutics such as inserting a feeding jejunostomy tube, intrapyloric injection of botulinum toxin, surgical (partial) gastrectomy, and implantable gastric electrical stimulation are occasionally considered.
Keywords: Gastroparesis, Diabetes mellitus, Delayed gastric emptying, Prokinetic therapy, Gastric electrical stimulation
NORMAL GASTRIC MOTOR FUNCTION
From an anatomical point of view, the stomach consists of the cardia, the fundus, the gastric body, the antrum and the pylorus. Functionally, the stomach consists of a proximal part and a distal part, with a sphincter muscle at both ends. The proximal stomach consists of the fundus and the proximal part of the gastric corpus. The main function of the proximal stomach is to provide a reservoir to the meal. The distal part of the stomach consists of the distal part of the gastric corpus, the gastric antrum and the pylorus. Its main function is to grind and empty the meal from the stomach.1
Structures involved in the control of gastric motility are smooth muscle cells, interstitial cells of Cajal, enteric nerves and the vagus nerve. The muscle layers of the stomach comprise an outer longitudinal layer, and an inner circular muscle layer. Originating from the gastroesophageal junction, in the proximal stomach, near the lesser curvature, an intermediate oblique muscle layer is also present. The myenteric plexus is found between the circular and longitudinal muscle layers in the stomach. Cell bodies of intrinsic neurons are grouped in ganglia whose number increases toward the distal antrum. Although these neurons receive input from vagal and sympathetic extrinsic nerves, the gastric myenteric plexus has major functional autonomy.
Smooth muscle cells in the proximal stomach do not display electrical oscillatory activity and this part is characterized by a tonic contractile activity. Smooth muscle cells in the distal part of the stomach are characterized by the presence of rhythmic electrical activity, so-called slow waves, and phasic contractile activity. Slow waves are oscillations of the membrane potential at a frequency of 3 cycles per minute, that are triggered from an area in the corpus near the greater curvature, the so-called pacemaker region of the stomach. Slow waves are generated by the interstitial cells of Cajal, a specialized type of cell of mesodermal origin, located near the myenteric plexus, are the generators of the slow waves.2 The slow waves determine the timing of gastric contractions. Action potential discharge, triggered by neurotransmitter release from the myenteric plexus, occurs at the crest of a slow wave. Thus, the slow waves determine the maximal frequency of contractions and the number of spikes determines the strength of the contractions.
In the fasting state, the proximal gastrointestinal tract displays the migrating motor complex (MMC), a cyclical motor pattern of the stomach and the small intestine.3 The MMC consists of three different phases. Phase I is characterized by the absence of contractile activity; phase II displays irregular contractile activity and phase III is a phase of intense contractions at maximal frequency (3 per minute in the stomach, 12 per minute in the duodenum), which is again followed by phase I.
When food is ingested, the MMC is suppressed and, through the vagus nerve, upper gastrointestinal motility switches to the fed or postprandial pattern. During and after ingestion of a meal, a relaxation of the proximal stomach occurs, which provides the meal with a reservoir and enables a gastric volume increase without a rise in pressure.4 This also allows the stomach to retain food and to allow passage to the duodenum at a rate that matches the duodenal absorptive capacity. Two phases can be distinguished in the gastric reservoir function, and both are vagally mediated. Immediately after deglutition, the lower esophageal sphincter and the proximal stomach relax to allow passage and storage of the food bolus. These enterogastric reflexes appear to be vagally mediated, with evidence that fat-induced proximal gastric relaxation is mediated by nitric oxide.5,6 This rapid inhibitory phenomenon of gastric motility is called receptive relaxation. During gastric filling by food ingestion, a long-lasting relaxation of the proximal stomach occurs which is called adaptive relaxation or gastric accommodation.
After ingestion of a meal, circular peristaltic waves move from the mid-corpus to the pylorus. In the antrum, these contractions will grind the food and mix it with gastric juices through retropulsion, to finally lead to propulsion and evacuation of small particles. The flow of chyme from the stomach to the duodenum is pulsatile and is determined by the balance between the strength of antral contraction, the degree of pyloric relaxation, and the duodenal resistance. The pylorus is also involved in regulation of flow to the small intestine, and helps to discriminate fluid, viscous and solid gastric contents. When gastric content is fluid, antral contractions occlude the lumen and liquid is easily transferred to the duodenum. In case of a more viscous or solid gastric content, contractions are not lumen-obliterating, and retropulsion to the proximal stomach serves to mix and grind gastric contents. Duodenal contractions serve to delay further gastric emptying when the duodenum is not empty.
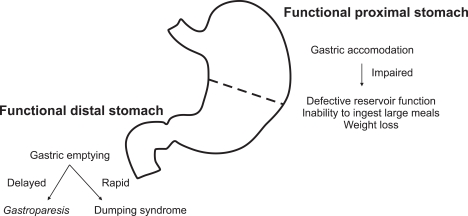
Disordered gastric motility occurs whenever the processes of interdigestive motility, gastric reservoir function or gastric emptying are not properly controlled. Impaired control of gastric accommodation may lead to defective reservoir function, inability to ingest large meals and weight loss.7 Abnormally rapid gastric emptying may lead to duodenal caloric overload and dumping syndrome8 Abnormally delayed emptying leads a gastroparesis syndrome with prolonged gastric stasis and fermentation of food (Fig. 1).9
Fig. 1.
Functional parts of stomach and their disorders.
DEFINITION AND PATHOGENESIS OF GASTROPARESIS
Delayed gastric emptying in the absence of mechanical obstruction is referred to as gastroparesis. Symptoms that are often attributed to gastroparesis include postprandial fullness, nausea, vomiting - especially when this occurs late postprandially, anorexia and weight loss. The distinction between functional dyspepsia (FD) with delayed gastric emptying and idiopathic gastroparesis has not been clearly defined. Hence, it has been proposed to use the term gastroparesis only when persistently and severely delayed gastric emptying is found in the absence of mechanical obstruction.10,11
Women constitute the majority of patients with a female: male ratio of 4:1 and the mean age of onset is 34 years. The reason for the sex ratio imbalance remains unknown. There is also evidence of a gender difference in solid and liquid emptying between men and women with female gastric emptying slower than men.12 Soykan et al.13 reported that 62% of patients with idiopathic gastroparesis revealed a past history of physical or sexual abuse. However, in a cohort of FD patients, Geeraerts et al.14 found an association of a history of abuse with impaired accommodation and with hypersensitivity to gastric distention, but not with delayed gastric emptying. The association of abuse history and gastroparesis probably deserves further studies.
Gastroparesis is the end result of neuromuscular failure or excessive inhibitory influence, or both, on the components of the gastric emptying process. The most important pathophysiological abnormalities contributing to the gastroparesis syndrome include fundal hypomotility, antral hypomotility, gastric arrhythmia and lack of antropyloroduodenal coordination. In addition, excessive negative feedback mechanisms may also further delay gastric emptying rate.
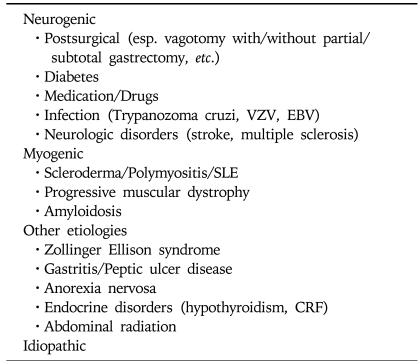
Delayed gastric emptying may be caused by a variety of mechanical and non-mechanical causes. Table 1 summarizes a number of causes of gastroparesis, subdivided according to the putative underlying abnormality. A number of drugs such as anticholinergics, opioids, L-dopa, tricyclic antidepressants and phenothiazines may contribute to a slowing of gastric emptying. When drug effects are ruled out, the predominant causes of gastroparesis are idiopathic (33%), diabetes mellitus (24%) and post-surgical (19%).15 Gastroparesis may complicate both type I and type II diabetes, with reported prevalences of up to 75% of the patients, depending on the patients studied and on the definition of gastroparesis. Diabetic gastroparesis involves mainly solid meals and is often associated with the presence of autonomic neuropathy. Poor glycemic control may also contribute to delayed emptying, which in its turn may also impair glycemic control. Vagotomy causes rapid emptying of liquids and delayed emptying of solids. However, after partial gastrectomy, a complex situation exists which may lead to gastric stasis or rapid emptying with dumping syndrome, or bile reflux gastritis and even small intestinal bacterial overgrowth. Gastroparesis may also occur in association with less frequent disorders such as anorexia nervosa, renal failure, Parkinson's disease and chronic intestinal pseudo-obstruction. In a subgroup of patients with gastroparesis, no underlying cause is apparent, so their disorder is considered idiopathic. In some of these, an acute onset and the presence of viral antibodies suggest involvement of acute infections in the pathogenesis of gastroparesis.11,15
Table 1.
Causes of Gastroparesis
DIAGNOSIS
Prior to any assessment of gastric motor activity or emptying rate, organic disease needs to be excluded. This is preferentially done by upper G.I. endoscopy and radiology. Whilst endoscopy is often normal in patients with delayed gastric emptying, in profound gastroparesis, endoscopy may reveal food debris remnants, so-called bezoar, in the stomach.16 Laboratory tests should exclude abnormalities of ion balance, glycemia and thyroid function. As a next step, tests of gastric motor function can be considered. These are useful for diagnostic labelling, but whether they really contribute to determining treatment approach has been a matter of controversy. In the absence of alarm symptoms or risk factors, the optimal indication and timing of additional examinations in patients with symptoms suggestive of gastroparesis have not been established. Many clinicians will use prokinetics without having established delayed emptying, and emptying testing may be most appropriate in those with poor symptom response (see below).
Radionuclide gastric emptying measurement is considered the gold standard method to assess gastric emptying rate.17 Solid and liquid emptying can be assessed separately or simultaneously. The solid and/or liquid meals are labeled with a (different) radio-isotope, usually 99Tc or 111In. A gamma-camera measures the number of counts in an investigator-determined region of interest (total, proximal or distal stomach, small intestine) for a certain time frame after ingestion of a meal. Mathematical processing involves corrections for distance to the camera and isotope decay, and curve fitting which allows calculating the half emptying time, the lag phase (period of delay after meal ingestion before emptying starts) and % of labeled meal retention at intervals up to four hours after ingestion.
Comparing gastric emptying results from different hospitals has been hampered by lack of standarization of the radioisotope emptying meal. In an international collaborative study, the range of normality has been established for a low-fat egg beater meal, with the gastric residual at 4 hours providing the most accurate parameter for the detection of delayed gastric emptying, with a sensitivity of 100 percent and specificity of 70 percent. In contrast, the two hour measurement was not useful for detecting delayed emptying (sensitivity 100 percent but specificity 20 percent).18 Although not routinely applied, the radioisotope technique also has the ability to provide information on distribution within the stomach.19 Disadvantages include the use of radioactive substances, considerable costs and the poor level of standardization of meal composition and measuring times over different laboratories.
Another way of assessing the gastric emptying rate is a gastric emptying breath test. The solid or liquid phase of a meal is labeled with a 13C containing substrate (octanoic acid, acetic acid, glycin or spirulina).20 As soon as the labeled food enters the duodenum, absorption occurs with generation of 13CO2 which appears in the breath.20 Breath sampling at regular intervals and mathematical processing of its 13CO2 content over time allows calculating a gastric emptying curve. The advantages of this test are the use of non-radioactive materials and the ability to perform the test outside a hospital setting. Several studies have shown that 13C acid breath tests are valid alternatives for scintigraphy, given its safety and highly significant correlation with scintigraphy.21,22 Disadvantages are the absence of standardization of meal and substrate, and the absence of anatomical details.
Ultrasound has been used to measure the diameter of the gastric antrum as a marker of the emptying rate of a liquid meal.17 The advantages of real-time ultrasound are its non-invasive nature and wide availability. However, the ultrasound technique is time-consuming and not suitable for solid meals. It generally measures liquid meals only and liquid emptying rate is often preserved until gastroparesis is well advanced, and may be paradoxically enhanced under some conditions.
In 1992 it was already reported that magnetic resonance imaging (MRI) was a valid method for measuring gastric emptying in comparison to scintigraphy.23 Recent data confirm these findings,24 but the limited availability and high costs of MRI limit the use in daily practice. Moreover, MRI is usually done in the less physiological supine position.
MEDICAL THERAPY
The long term prognosis of gastroparesis has not been well studied. One study in 20 patients with diabetic gastroparesis found no change in gastric emptying rates after a 12 year follow-up.25 Hence, in most patients presenting with important symptoms, therapeutic measures will be necessary.
1. Dietary measures
In case of gastroparesis, dietary interventions consisting of smaller more frequent meals throughout the day with restricted fat content are often proposed. Meals of larger weight and kcal are associated with longer emptying times.26 Fat intake releases cholecystokinin which can further delay gastric emptying. However, the efficacy of these measures has not been established, and most patients have already implemented these on their own initiative. In addition, patients can be advised to use liquid nutrients as a larger part of the daily food intake. Finally, low-fibre meals are advised to prevent bezoar formation. In patients with diabetic gastroparesis, additional measures are taken to optimalise glycemic control. The effect of better glycemic control on gastroparesis is not fully proven, but it is known that acute hyperglycaemia slows gastric emptying27 and attenuates the efficacy of prokinetic drugs.28,29
2. Prokinetic drugs
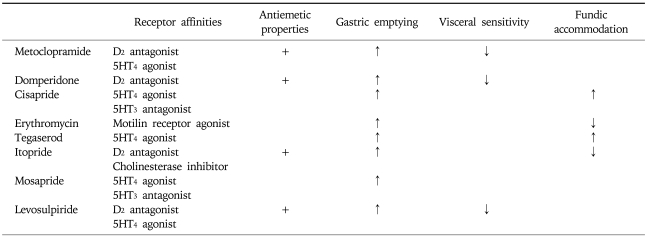
Several prokinetic agents have been shown to enhance gastric emptying rate in patients with idiopathic or diabetic gastroparesis (Table 2). The underlying assumption is that these drugs, through enhancement of delayed gastric emptying, should improve symptoms. However, studies available so far fail to convincingly prove this hypothesis and evidence that the symptomatic improvement is related to enhancement of gastric emptying is lacking.30-33 For diabetic gastroparesis, several studies have reported improvement of gastric emptying with prokinetic drugs, but no consistent effects on symptoms or glycemic control were obtained.34,35
Table 2.
Overview of Prokinetic Drugs
The best studied prokinetics are metoclopramide, domperidone, cisapride and erythromycin. Clinical suspicion of gastroparesis warrants ruling out of mechanical causes and serum electrolyte imbalances, followed by empirical treatment with a gastroprokinetic like domperidone or metoclopramide.11,15,36 Metoclopramide is a dopamine antagonist with both central and peripheral activity. It is available for both oral and parenteral use. Besides its anti-emetic effect it has some prokinetic activity. Because of its CNS side effects, high-dose oral metoclopramide is not advised for long term use. The parenteral form can be useful in the acute phase, when no oral intake is possible. Domperidone is a dopamine antagonist with only peripheral activity. Domperidone is the drug of choice as metoclopramide may be associated with extrapyramidal side effects. Both metoclopramide and domperidone can cause hyperprolactinemia. Cisapride facilitates acetylcholine release from myenteric neurons through a 5-HT4 receptor mediated effect.37 Superior efficacy and tolerance has been suggested for domperidone over metoclopramide,38,39 and for cisapride over metoclopramide.40 However, due to enhanced risk of QT prolongation with cardiac arrhythmia's, cisapride is no longer available for use in routine clinical practice.41 There are only anecdotal reports supporting the efficacy of other prokinetic approaches such as mosapride, renzapride, levosulpiride, and clonidine in diabetic gastroparesis.36
Erythromycin act as a motilin receptor agonist and has prokinetic properties, available for both i.v and p.o. use. Short term studies in diabetic and postsurgical gastroparesis have reported beneficial effects of treatment with erythromycin (3×250-500 mg).42 It is the most potent gastric prokinetic with major improvement in gastric emptying. Due to its antibiotic properties long term use can lead to the induction of resistant strains. There are other possible side effects like ototoxicity and pseudomembranic colitis, which limits long-term use in patients with gastroparesis. Furthermore, the problem of tachyphylaxis makes long term use less attractive. In a literature review, Maganti et al. concluded that, although erythromycin was proven to be a strong prokinetic, the available studies do not establish efficacy of erythromycin in relieving symptoms of gastroparesis.43 Studies with a related macrolide compound, ABT-229, failed to demonstrate any symptomatic benefit of this non-antibiotic macrolide prokinetic in idiopathic and diabetic gastroparesis.44,45
Overall, the evidence that classical gastroprokinetics like metoclopramide, domperidone, cisapride or erythromycin are effective in gastroparesis is far from overwhelming.32 Several newer gastroprokinetics have been evaluated or are under evaluation.36 These include other 5-HT4 agonists such as renzapride, tegaserod or TD-5108, newer macrolide compounds such as mitemcinal, and ghrelin receptor agonists such as TZP-101.36 None of these is presently commercially available.
INVASIVE THERAPEUTIC MODALITIES
In refractory cases with severe weight loss, invasive therapies like insertion of a feeding jejunostomy tube,11 intrapyloric injection of botulinum toxin, surgical (partial) gastrectomy or implantable gastric electrical stimulation (GES) are occasionally considered. Home parenteral nutrition is another option, but unlike enteral tube feeding, this is not devoid of potentially life-threatening complications like septicaemia or thrombo-embolism. The efficacy of these modalities has not been clearly established. A feeding jejunostomy is more frequently used to maintain hydration, nutrition and glycemic control. The available studies assessed symptom improvement through subjective reporting of symptoms in diabetic patients with gastroparesis. Although symptoms seemed to improve, the evidence is not substantial. Moreover, jejunostomy is associated with a high complication rate, requiring hospitalization or surgery in more than half of the cases.46-48
Botulinum toxin is a strong inhibitor of neuromuscular transmission. Injection of the toxin directly in the pyloric sphincter has the potential to reduce gastric outlet resistance and thereby improve gastric emptying and symptoms associated with delayed gastric emptying. Anecdotal evidence suggests the use of intrapyloric injection of botulinum toxin in idiopathic or diabetic gastroparesis,49-51 but in two controlled studies, no benefit over saline injection was found.52,53
Especially for surgical therapy, supportive evidence of good quality is not available. Only few studies assessed symptom improvement in a standardized way, and most studies focused mainly on technical aspects. Extensive subtotal or completion gastrectomy seems to be the most advocated surgical option for patients with refractory, postsurgical gastroparesis. Symptom improvements are claimed in 67 to 100% of patients, but without a beneficial effect in terms of weight gain.54 A venting gastrostomy was reported to reduce symptoms and improve nutritional status,55 but no other study confirmed this experience. Completion of gastrectomy for severe postgastrectomy stasis is successful in 43% of patients. The combination of nausea, need for total parenteral nutrition and retained food at endoscopy are negative prognostic factors.54,56
In the light of the unsatisfactory results from conventional medical therapy, the development of implantable GES devices, which received Food and Drug Administration approval as a humanitarian device exemption in March 2000 (Enterra, Medtronics), provides a potentially attractive alternative for the medical or surgical treatment of difficult gastroparesis. The gastric stimulation device is implanted subcutaneously in the abdominal wall and the electrodes are placed in the smooth muscle along the greater curvature. The stimulator delivers electrical pulses at 12 cpm. To date, beneficial effects of GES that have been reported from uncontrolled case series include improvement in nutritional status, symptoms of nausea and vomiting as well as improved quality of life.57 Only one randomized double blind cross over trial with GES; the WAVESS-trial was reported. Unfortunately, the published results and the results presented to the US FDA are discrepant.58 In one-month blinded controlled phase with the device off or on, vomiting frequency was significantly reduced during the month when the device was in the 'ON' mode compared to the 'OFF' mode. In a longer open label phase, symptom scores and quality of life were significantly improved up to 12 months after the start of gastric stimulation. The gastric emptying rate, in contrary, was not significantly accelerated and there was no correlation between the improvement in symptom score and gastric emptying rate.59 To date, the mechanism underlying the symptomatic improvement has not been established, and favourable results on symptoms of vomiting seem to occur regardless of whether gastric emptying was delayed or normal.60 Although some longer-follow up series have been published, it remains unclear whether the long-term efficacy of this modality is superior to the natural history of severe gastroparesis.61 Uncontrolled data suggest improvement of symptoms and reduced HbA1C-levels in patients with diabetic gastroparesis.62,63 Hence, it is at present unclear whether this is really a treatment for gastroparesis, or mainly symptomatic therapy for nausea and vomiting. Given the high cost, and paucity of available data, generalised use of the device cannot be recommended and patients should undergo gastric electrical stimulation treatment only in the setting of a research protocol.61
References
- 1.Tack J. Gastric motor disorders. Best Pract Res Clin Gastroenterol. 2007;21:633–644. doi: 10.1016/j.bpg.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Sanders KM, Koh SD, Ward SM. Interstitial cells of cajal as pacemakers in the gastrointestinal tract. Annu Rev Physiol. 2006;68:307–343. doi: 10.1146/annurev.physiol.68.040504.094718. [DOI] [PubMed] [Google Scholar]
- 3.Vantrappen G, Janssens J, Hellemans J, Ghoos Y. The interdigestive motor complex of normal subjects and patients with bacterial overgrowth of the small intestine. J Clin Invest. 1977;59:1158–1166. doi: 10.1172/JCI108740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azpiroz F, Malagelada JR. Gastric tone measured by an electronic barostat in health and postsurgical gastroparesis. Gastroenterology. 1987;92:934–943. doi: 10.1016/0016-5085(87)90967-x. [DOI] [PubMed] [Google Scholar]
- 5.Schuurkes JA, Meulemans AL. Nitric oxide and gastric relaxation. Dig Dis Sci. 1994;39:79S–81S. doi: 10.1007/BF02300378. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi T. Pathophysiological significance of neuronal nitric oxide synthase in the gastrointestinal tract. J Gastroenterol. 2003;38:421–430. doi: 10.1007/s00535-003-1094-y. [DOI] [PubMed] [Google Scholar]
- 7.Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352. doi: 10.1016/s0016-5085(98)70012-5. [DOI] [PubMed] [Google Scholar]
- 8.Abell TL, Bernstein RK, Cutts T, et al. Treatment of gastroparesis: a multidisciplinary clinical review. Neurogastroenterol Motil. 2006;18:263–283. doi: 10.1111/j.1365-2982.2006.00760.x. [DOI] [PubMed] [Google Scholar]
- 9.Vecht JA, Masclee A, Lamers CB. The dumping syndrome: current insights into pathophysiology, diagnosis and treatment. Scand J Gastroenterol Suppl. 1997;223:21–27. [PubMed] [Google Scholar]
- 10.Stanghellini V, Tosetti C, Paternico A, et al. Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology. 1996;110:1036–1042. doi: 10.1053/gast.1996.v110.pm8612991. [DOI] [PubMed] [Google Scholar]
- 11.Tack J. The difficult patient with gastroparesis. Best Pract Res Clin Gastroenterol. 2007;21:379–391. doi: 10.1016/j.bpg.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Datz FL, Christian PE, Moore J. Gender-related differences in gastric emptying. J Nucl Med. 1987;28:1204–1207. [PubMed] [Google Scholar]
- 13.Soykan I, Sivri B, Sarosiek I, Kiernan B, McCallum RW. Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci. 1998;43:2398–2404. doi: 10.1023/a:1026665728213. [DOI] [PubMed] [Google Scholar]
- 14.Geeraerts B, Van Oudenhove L, Fischler B, et al. Influence of abuse history on gastric sensorimotor function in functional dyspepsia. Neurogastroenterol Motil. 2009;21:33–41. doi: 10.1111/j.1365-2982.2008.01178.x. [DOI] [PubMed] [Google Scholar]
- 15.Horowitz M, Su YC, Rayner CK, Jones KL. Gastroparesis: prevalence, clinical significance and treatment. Can J Gastroenterol. 2001;15:805–813. doi: 10.1155/2001/628102. [DOI] [PubMed] [Google Scholar]
- 16.Patrick A, Epstein O. Review article: gastroparesis. Aliment Pharmacol Ther. 2008;27:724–740. doi: 10.1111/j.1365-2036.2008.03637.x. [DOI] [PubMed] [Google Scholar]
- 17.Parkman HP, Hasler WL, Fischer RS. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology. 2004;127:1592–1622. doi: 10.1053/j.gastro.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 18.Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462. doi: 10.1111/j.1572-0241.2000.02076.x. [DOI] [PubMed] [Google Scholar]
- 19.Piessevaux H, Tack J, Walrand S, Pauwels S, Geubel A. Intragastric distribution of a standardized meal in health and functional dyspepsia: correlation with specific symptoms. Neurogastroenterol Motil. 2003;15:447–455. doi: 10.1046/j.1365-2982.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- 20.Ghoos YF, Maes BD, Geypens BJ, et al. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology. 1993;104:1640–1647. doi: 10.1016/0016-5085(93)90640-x. [DOI] [PubMed] [Google Scholar]
- 21.Chew CG, Bartholomeusz FD, Bellon M, Chatterton BE. Simultaneous 13C/14C dual isotope breath test measurement of gastric emptying of solid and liquid in normal subjects and patients: comparison with scintigraphy. Nucl Med Rev Cent East Eur. 2003;6:29–33. [PubMed] [Google Scholar]
- 22.Zahn A, Langhans CD, Hoffner S, et al. Measurement of gastric emptying by 13C-octanoic acid breath test versus scintigraphy in diabetics. Z Gastroenterol. 2003;41:383–390. doi: 10.1055/s-2003-39331. [DOI] [PubMed] [Google Scholar]
- 23.Schwizer W, Maecke H, Fried M. Measurement of gastric emptying by magnetic resonance imaging in humans. Gastroenterology. 1992;103:369–376. doi: 10.1016/0016-5085(92)90823-h. [DOI] [PubMed] [Google Scholar]
- 24.Lauenstein TC, Vogt FM, Herborn CU, DeGreiff A, Debatin JF, Holtmann G. Time-resolved three-dimensional MR imaging of gastric emptying modified by IV administration of erythromycin. AJR Am J Roentgenol. 2003;180:1305–1310. doi: 10.2214/ajr.180.5.1801305. [DOI] [PubMed] [Google Scholar]
- 25.Jones KL, Russo A, Berry MK, Stevens JE, Wishart JM, Horowitz M. A longitudinal study of gastric emptying and upper gastrointestinal symptoms in patients with diabetes mellitus. Am J Med. 2002;113:449–455. doi: 10.1016/s0002-9343(02)01228-7. [DOI] [PubMed] [Google Scholar]
- 26.Moore SA, Peterson RG, Felten DL, O'Connor BL. Glycogen accumulation in tibial nerves of experimentally diabetic and aging control rats. J Neurol Sci. 1981;52:289–303. doi: 10.1016/0022-510x(81)90012-5. [DOI] [PubMed] [Google Scholar]
- 27.Schvarcz E, Palmer M, Aman J, Horowitz M, Stridsberg M, Berne C. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology. 1997;113:60–66. doi: 10.1016/s0016-5085(97)70080-5. [DOI] [PubMed] [Google Scholar]
- 28.Petrakis IE, Vrachassotakis N, Sciacca V, Vassilakis SI, Chalkiadakis G. Hyperglycaemia attenuates erythromycin-induced acceleration of solid-phase gastric emptying in idiopathic and diabetic gastroparesis. Scand J Gastroenterol. 1999;34:396–403. doi: 10.1080/003655299750026416. [DOI] [PubMed] [Google Scholar]
- 29.Horowitz M, Jones KL, Harding PE, Wishart JM. Relationship between the effects of cisapride on gastric emptying and plasma glucose concentrations in diabetic gastroparesis. Digestion. 2002;65:41–46. doi: 10.1159/000051930. [DOI] [PubMed] [Google Scholar]
- 30.Corinaldesi R, Stanghellini V, Raiti C, Rea E, Salgemini R, Barbara L. Effect of chronic administration of cisapride on gastric emptying of a solid meal and on dyspeptic symptoms in patients with idiopathic gastroparesis. Gut. 1987;28:300–305. doi: 10.1136/gut.28.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Finney JS, Kinnersley N, Hughes M, O'Bryan-Tear CG, Lothian J. Meta-analysis of antisecretory and gastrokinetic compounds in functional dyspepsia. J Clin Gastroenterol. 1998;26:312–320. doi: 10.1097/00004836-199806000-00022. [DOI] [PubMed] [Google Scholar]
- 32.Sturm A, Holtmann G, Goebell H, Gerken G. Prokinetics in patients with gastroparesis: a systematic analysis. Digestion. 1999;60:422–427. doi: 10.1159/000007687. [DOI] [PubMed] [Google Scholar]
- 33.Veldhuyzen van Zanten SJ, Jones MJ, Verlinden M, Talley NJ. Efficacy of cisapride and domperidone in functional (nonulcer) dyspepsia: a meta-analysis. Am J Gastroenterol. 2001;96:689–696. doi: 10.1111/j.1572-0241.2001.03521.x. [DOI] [PubMed] [Google Scholar]
- 34.Braden B, Enghofer M, Schaub M, Usadel KH, Caspary WF, Lembcke B. Long-term cisapride treatment improves diabetic gastroparesis but not glycaemic control. Aliment Pharmacol Ther. 2002;16:1341–1346. doi: 10.1046/j.1365-2036.2002.01257.x. [DOI] [PubMed] [Google Scholar]
- 35.Stacher G, Schernthaner G, Francesconi M, et al. Cisapride versus placebo for 8 weeks on glycemic control and gastric emptying in insulin-dependent diabetes: a double blind cross-over trial. J Clin Endocrinol Metab. 1999;84:2357–2362. doi: 10.1210/jcem.84.7.5859. [DOI] [PubMed] [Google Scholar]
- 36.Tack J. Prokinetics and fundic relaxants in upper functional GI disorders. Curr Opin Pharmacol. 2008;8:690–696. doi: 10.1016/j.coph.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 37.Schuurkes J. Effect of cisapride on gastric motility. Z Gastroenterol. 1990;28(Suppl 1):27–30. [PubMed] [Google Scholar]
- 38.Dumitrascu DL, Wienbeck M. Domperidone versus metoclopramide in the treatment of diabetic gastroparesis. Am J Gastroenterol. 2000;95:316–317. doi: 10.1111/j.1572-0241.2000.01721.x. [DOI] [PubMed] [Google Scholar]
- 39.Patterson D, Abell T, Rothstein R, Koch K, Barnett J. A double-blind multicenter comparison of domperidone and metoclopramide in the treatment of diabetic patients with symptoms of gastroparesis. Am J Gastroenterol. 1999;94:1230–1234. doi: 10.1111/j.1572-0241.1999.00456.x. [DOI] [PubMed] [Google Scholar]
- 40.Feldman M, Smith HJ. Effect of cisapride on gastric emptying of indigestible solids in patients with gastroparesis diabeticorum: a comparison with metoclopramide and placebo. Gastroenterology. 1987;92:171–174. doi: 10.1016/0016-5085(87)90854-7. [DOI] [PubMed] [Google Scholar]
- 41.Michalets EL, Williams CR. Drug interactions with cisapride: clinical implications. Clin Pharmacokinet. 2000;39:49–75. doi: 10.2165/00003088-200039010-00004. [DOI] [PubMed] [Google Scholar]
- 42.Janssens J, Peeters TL, Vantrappen G, et al. Improvement of gastric emptying in diabetic gastroparesis by erythromycin: preliminary studies. N Engl J Med. 1990;322:1028–1031. doi: 10.1056/NEJM199004123221502. [DOI] [PubMed] [Google Scholar]
- 43.Maganti K, Onyemere K, Jones MP. Oral erythromycin and symptomatic relief of gastroparesis: a systematic review. Am J Gastroenterol. 2003;98:259–263. doi: 10.1111/j.1572-0241.2003.07167.x. [DOI] [PubMed] [Google Scholar]
- 44.Talley NJ, Verlinden M, Geenen DJ, et al. Effects of a motilin receptor agonist (ABT-229) on upper gastrointestinal symptoms in type 1 diabetes mellitus: a randomised, double blind, placebo controlled trial. Gut. 2001;49:395–401. doi: 10.1136/gut.49.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Talley NJ, Verlinden M, Snape W, et al. Failure of a motilin receptor agonist (ABT-229) to relieve the symptoms of functional dyspepsia in patients with and without delayed gastric emptying: a randomized double-blind placebo-controlled trial. Aliment Pharmacol Ther. 2000;14:1653–1661. doi: 10.1046/j.1365-2036.2000.00868.x. [DOI] [PubMed] [Google Scholar]
- 46.Devendra D, Millward BA, Travis SP. Diabetic gastroparesis improved by percutaneous endoscopic jejunostomy. Diabetes Care. 2000;23:426–427. doi: 10.2337/diacare.23.3.426. [DOI] [PubMed] [Google Scholar]
- 47.Jacober SJ, Narayan A, Strodel WE, Vinik AI. Jejunostomy feeding in the management of gastroparesis diabeticorum. Diabetes Care. 1986;9:217–219. doi: 10.2337/diacare.9.2.217. [DOI] [PubMed] [Google Scholar]
- 48.Fontana RJ, Barnett JL. Jejunostomy tube placement in refractory diabetic gastroparesis: a retrospective review. Am J Gastroenterol. 1996;91:2174–2178. [PubMed] [Google Scholar]
- 49.Ezzeddine D, Jit R, Katz N, Gopalswamy N, Bhutani MS. Pyloric injection of botulinum toxin for treatment of diabetic gastroparesis. Gastrointest Endosc. 2002;55:920–923. doi: 10.1067/mge.2002.124739. [DOI] [PubMed] [Google Scholar]
- 50.Miller LS, Szych GA, Kantor SB, et al. Treatment of idiopathic gastroparesis with injection of botulinum toxin into the pyloric sphincter muscle. Am J Gastroenterol. 2002;97:1653–1660. doi: 10.1111/j.1572-0241.2002.05823.x. [DOI] [PubMed] [Google Scholar]
- 51.Arts J, van Gool S, Caenepeel P, Verbeke K, Janssens J, Tack J. Influence of intrapyloric botulinum toxin injection on gastric emptying and meal-related symptoms in gastroparesis patients. Aliment Pharmacol Ther. 2006;24:661–667. doi: 10.1111/j.1365-2036.2006.03019.x. [DOI] [PubMed] [Google Scholar]
- 52.Arts J, Holvoet L, Caenepeel P, et al. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26:1251–1258. doi: 10.1111/j.1365-2036.2007.03467.x. [DOI] [PubMed] [Google Scholar]
- 53.Friedenberg FK, Palit A, Parkman HP, Hanlon A, Nelson DB. Botulinum toxin A for the treatment of delayed gastric emptying. Am J Gastroenterol. 2008;103:416–423. doi: 10.1111/j.1572-0241.2007.01676.x. [DOI] [PubMed] [Google Scholar]
- 54.Jones MP, Maganti K. A systematic review of surgical therapy for gastroparesis. Am J Gastroenterol. 2003;98:2122–2129. doi: 10.1111/j.1572-0241.2003.07721.x. [DOI] [PubMed] [Google Scholar]
- 55.Kim CH, Nelson DK. Venting percutaneous gastrostomy in the treatment of refractory idiopathic gastroparesis. Gastrointest Endosc. 1998;47:67–70. doi: 10.1016/s0016-5107(98)70301-3. [DOI] [PubMed] [Google Scholar]
- 56.Forstner-Barthell AW, Murr MM, Nitecki S, et al. Near-total completion gastrectomy for severe postvagotomy gastric stasis: analysis of early and long-term results in 62 patients. J Gastrointest Surg. 1999;3:15–21. doi: 10.1016/s1091-255x(99)80003-1. [DOI] [PubMed] [Google Scholar]
- 57.Abell TL, Van Cutsem E, Abrahamsson H, et al. Gastric electrical stimulation in intractable symptomatic gastroparesis. Digestion. 2002;66:204–212. doi: 10.1159/000068359. [DOI] [PubMed] [Google Scholar]
- 58.Jones MP. Gastric electrical stimulation for refractory gastroparesis. Gastroenterology. 2004;126:629–630. doi: 10.1053/j.gastro.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 59.Abell T, McCallum R, Hocking M, et al. Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology. 2003;125:421–428. doi: 10.1016/s0016-5085(03)00878-3. [DOI] [PubMed] [Google Scholar]
- 60.Gourcerol G, Leblanc I, Leroi AM, Denis P, Ducrotte P. Gastric electrical stimulation in medically refractory nausea and vomiting. Eur J Gastroenterol Hepatol. 2007;19:29–35. doi: 10.1097/01.meg.0000250584.15490.b4. [DOI] [PubMed] [Google Scholar]
- 61.Ang D, Tack J. Gastric electrical stimulation for the treatment of gastroparesis: ready for prime time? Digestion. 2007;75:80–82. doi: 10.1159/000102960. [DOI] [PubMed] [Google Scholar]
- 62.Lin Z, Forster J, Sarosiek I, McCallum RW. Treatment of diabetic gastroparesis by high-frequency gastric electrical stimulation. Diabetes Care. 2004;27:1071–1076. doi: 10.2337/diacare.27.5.1071. [DOI] [PubMed] [Google Scholar]
- 63.van der Voort IR, Becker JC, Dietl KH, Konturek JW, Domschke W, Pohle T. Gastric electrical stimulation results in improved metabolic control in diabetic patients suffering from gastroparesis. Exp Clin Endocrinol Diabetes. 2005;113:38–42. doi: 10.1055/s-2004-830525. [DOI] [PubMed] [Google Scholar]