Abstract
Background/Aims
The lifestyle changes that have accompanied economic growth have influenced disease patterns in Korea. Changing patterns of gastrointestinal (GI) diseases over the past two decades were investigated in the present study.
Methods
Data from inpatients with specific GI diseases, as defined by the International Classification of Diseases code, were extracted from the database at a tertiary medical facility for 1990, 1996, and 2006.
Results
Admission rates for GI diseases increased between 1990 and 2006. The most prevalent disease in 1990 was gastric cancer, followed by appendicitis and colorectal cancer. However, by 2006, gastric cancer, colon cancer, and colon adenoma or polyps had become the most prevalent diseases. Although gastric cancer showed a decreasing trend, the rate of colon cancer doubled over two decades. Furthermore, rates of detection and endoscopic treatment of early gastric cancer and adenoma of the stomach and colon have increased noticeably. Newly emerging diseases include inflammatory bowel disease and gastroesophageal reflux. There was no change in the incidence of peptic ulcer, but ulcer-related complications and the numbers treated surgically decreased.
Conclusions
The findings of this study indicate that the clinical trends of GI diseases in Korea have changed in a similar way to those in the West. Early detection of a GI neoplasm will continue to increase with the establishment of cancer-screening programs, resulting in a rising need for minimally invasive treatments.
Keywords: Gastrointestinal diseases, Korea, Trends, Epidemiology
INTRODUCTION
Korea has witnessed remarkable economic growth over the past two decades, and this had been accompanied by rapid life style changes. Disease trends have been changed and once rare diseases have now become prevalent. Recent advancements of medical science, diagnostic methods, and treatments also influence disease trends. These include discovery of Helicobacter-pylori (H. pylori), wide availability of electronic video endoscopy, and introduction of minimally invasive surgery. The development of an advanced healthcare system also had a major effect on epidemiologic patterns. In 1989, medical insurance policies became nationwide in Korea. The National Cancer Screening Program (NCSP) was initiated in 1999, and has since been expanded to include five common cancers, namely, stomach, liver, colon, breast, and uterine cervical cancer. These medical policy advances have increased public awareness of cancer.
It has been suggested that the clinical spectrum of diseases has moved toward the Western model across the whole Asia-Pacific region. However, few studies have been conducted to analyze the quantitative and qualitative aspects of the changing patterns of gastrointestinal diseases.1-3 The majority of studies performed in Asian have been focused only a single disease or a cross sectional survey at one point of time.4-8 The aim of this study was to investigate changing patterns of gastrointestinal diseases over the past two decades.
MATERIALS AND METHODS
1. Population and diseases
The medical records of inpatients with gastrointestinal diseases at Kangnam St. Mary's Hospital in 1990, 1996, and 2006 were analyzed retrospectively. Kangnam St. Mary's hospital is a tertiary university hospital, which was established in Seoul in 1980 with 520 beds. In 1988, 249 beds were added and a further expansion in 1992 increased the total number to 834. The number of households serviced by the hospital increased from 68,157 in 1990 to 93,010 in 2005. This study was originally planned to use 2006 records as the basis, and to investigate records dating back 10 and 20 years. However, in 1986, health benefits were restricted and medical records were not computerized; the nationwide health insurance scheme was introduced in 1989. Therefore, we analyzed medical records from 1990; the year after computerization was introduced at the hospital.
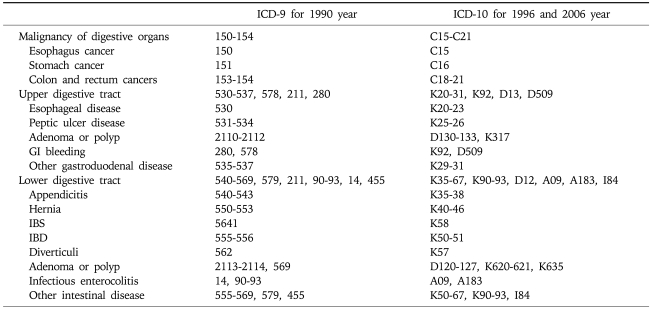
The records of four major departments where patients with gastrointestinal disease were typically admitted to surveyed for data analysis, namely, the departments of gastroenterology, oncology, general surgery, and cardiothoracic surgery. As a preliminary step, the data of inpatients with gastrointestinal diseases from randomly selected months from each year were analyzed according to International Statistical Classification of Diseases (ICD) codes. The data obtained showed that percentages of inpatients with gastrointestinal disease admitted to departments other than the major four departments mentioned above were only 8.6% in 1990, 3.4% in 1996, and 3.1% in 2006. Since hospital policy specifies that patients transfers to a corresponding department, we analyzed patients admitted to the aforementioned departments. Gastrointestinal diseases are classified and defined according to the ICD coding system, as shown in Table 1. The study protocol was approved by the institutional review board of our institution (KCMC07OT148, Jun 24, 2007).
Table 1.
Diseases of the Digestive System - Grouping according to the ICD Code
ICD, international (statistical) classification of diseases; GI, gastrointestinal; IBS, irritable bowel syndrome; IBD, inflammatory bowel disease.
2. Data analysis
The medical records contained data entered into administrative databases. Some of this data derived from such coding based only on charts have shortcomings, which can lead misclassifications of principal diagnoses. Accordingly, secondary and principal diagnosis were reviewed and classified manually in order to minimize errors. Data for patients under the age of 18 were excluded from the analysis. To organize data, multiple ICD codes were grouped together by anatomic site to create single disease entities. For example, colon cancer included subjects coded as having appendiceal cancer (C18.1), ascending colon cancer (C18.2), rectal cancer (C20), and anal cancer (C21.1). Several similar diagnoses were combined into one entry, such as, a premalignant lesion of colon and stomach (D126, K635 and D131, K317). When a patient was admitted more than once a year with the same disease, admittance was viewed as a single event. For example, if a patient with colon cancer was repeatedly admitted for chemotherapy, these admissions were treated as a single admission for colon cancer. However, if a patient was admitted several times, but for different diseases, each admission was considered a separate event. The frequencies of diseases were calculated as percentages of the total number of gastrointestinal diseases. Collated data was then arranged in frequency order.
3. Statistical analysis
All analyses were performed using SPSS software version 14.0 (SPSS Inc., Chicago, IL, USA). Trends for disease categories and sex ratio were determined by linear-by-linear association analysis. Age differences were analyzed by ANOVA, and statistical significance was accepted for p values of <0.05.
RESULTS
1. Demographics of hospital inpatients
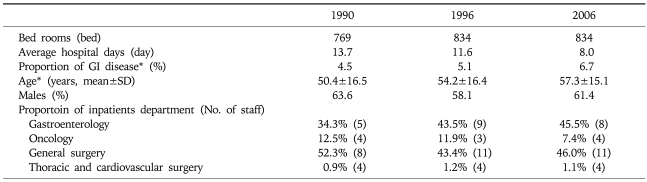
A summary of the analysis results is provided in Table 2. Admissions of inpatients for gastrointestinal disease among total inpatients increased a 1.5 fold from 4.5% in 1990 to 6.7% in 2006. Average number of hospitalization days per patient decreased from 13.7 days in 1990 to 8 days in 2006. Mean patient age also increased between 1990 and 2006 (p=0.000), but sex ratios were unchanged. Patients admitted to the departments of gastroenterology and general surgery accounted for more than 85% of all total patients diagnosed with a gastrointestinal disease. The percentage of patients admitted into the department of gastroenterology increased between 1990 and 2006, whereas the percentage of patients admitted into the department of general surgery decreased. The number of staff members in the departments of gastroenterology and general surgery also increased over the study period.
Table 2.
Hospital Details and Inpatient Demographics between 1990 and 2006
The ratio of inpatients from GI disease among the total inpatients.
GI, gastrointestinal disease.
*p<0.001 by ANOVA test.
2. Trends of hospitalization for gastrointestinal diseases
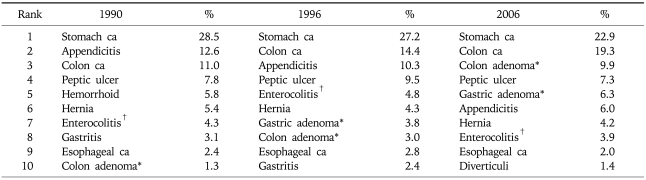
Table 3 shows the most common diseases among inpatients diagnosed with gastrointestinal diseases between 1990 and 2006.
Table 3.
Most Common Gastrointestinal Discharge Diagnoses for Inpatients Treated between 1990 and 2006
ca, cancer.
*Including polyp; †Including both infectious and noninfectious forms.
1) Disease with increasing rates based on admissions
The rate of colon cancer increased significantly between 1990 and 2006 (p=0.000), and the rates of adenoma and polyps and precancerous lesions of the colon and stomach have increased as well (p=0.000) (Table 3). Gastroesophageal reflux disease (GERD) (0.0% in 1990, 0.2% in 1996, 0.6% in 2006, p=0.004) and inflammatory bowel diseases (IBD) (0.0% in 1990, 1.2% in 1996, 1.3% in 2006, p=0.000) were uncommon in 1990, but appear to have increased recently. Diverticuli related diseases have also increased (0.3% in 1990, 0.9% in 1996, 1.4% in 2006, p=0.011).
2) Disease with decreasing rates based on admissions
Gastric cancer remained the most common disease among inpatients in 2006, but admissions have been falling (p=0.001). Rates of appendicitis (p=0.000), gastritis (p=0.000), and hemorrhoids (p=0.000) have also declined.
3) Diseases showing minor changes
Admission rates of peptic ulcer and malignant diseases, such as, esophageal cancer and small intestinal cancer, did not change significantly during the study period.
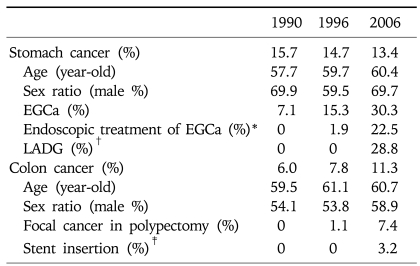
3. Malignancies of gastrointestinal organs
Admissions for gastric cancer show a decreasing trend, whereas admissions for early gastric cancer (EGCa) exhibit a continuously increasing trend (Table 4). In addition, the peak age of gastric cancer onset has increased. The proportion of EGCa for all gastric cancer cases that underwent surgery increased almost two-fold, from 20.8% in 1990 to 54% in 2006 (data not shown). In addition, the EGCa cases treated by endoscopic resection increased more than five-fold, that is, from 1.9% in 1996 to 11.2% in 2006. In 2006, laparoscopic surgery was performed in 28.8% of gastric cancer patients that underwent partial gastrectomy. Furthermore, advances in virtual endoscopy, appear to have dramatically increased admissions for gastric adenoma and polyps.
Table 4.
Most Common Malignant Gastrointestinal and Liver Diseases
EGCa, early gastric cancer; LADG, laparoscopy associated distal gastrectomy.
*Endoscopic treatment includes endoscopic mucosal resection or endoscopic submucosal dissection; †Ratio of LADG with respect to subtotal gastrectomy for stomach cancer; ‡Stent insertion for obstructive colon cancer.
Admissions for colon cancer doubled over the study period, and following the development of colonoscopy, polyp detections and the number of polypectomy increased. Consequently, the detection of focal colon cancer, which attributed to increased polypectomy, has also increased. Self-expanding metal stents were introduced in 2003 for the treatment of acute malignant colon obstruction as an alternative to palliative diverting colostomy for the treatment of incurable obstructing colon cancer and preoperative bridge therapy. In addition, the numbers of patients hospitalized for anti-cancer treatments, such as, chemotherapy for colon cancer, also increased significantly over the study period.
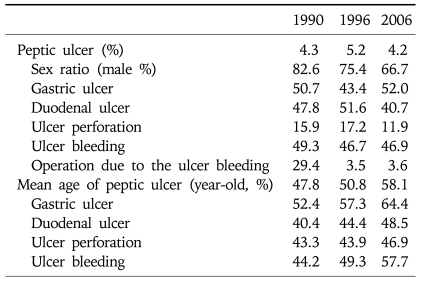
4. Changing patterns of peptic ulcers
Despite the eradication of H. pylori, no commensurate decreases in admission rates for peptic ulcer and bleeding ulcer was found (Table 5). The number of surgeries conducted for bleeding ulcer decreased noticeably, whereas endoscopic treatments increased. Furthermore, admissions for gastric ulcer increased, whereas those for duodenal ulcer decreased. Finally, the mean age of inpatients with a peptic ulcer increased (47.8 year-old in 1990 vs 58.1 year-old in 2006), and patients with gastric ulcer were 13.6 year-older than patients with a duodenal ulcer.
Table 5.
Changes in Peptic Ulcer Admission Patterns
DISCUSSION
Our data analysis spans almost two decades at Kangnam St. Mary's hospital and shows that admission rates due to gastrointestinal diseases have increased. This increasing trend was found to be substantially due to increases in admissions for GI malignant diseases and precancerous lesions in the elderly. The admissions for colon neoplasm have been increased rapidly in past two decades, while admission rates for gastric cancer, which was the top ranking disease in 1990, have decreased. Admission rates for peptic ulcer and bleeding ulcer remained unchanged over the study period, but numbers of surgical treatment decreased. These changes might be attributed to an aging population, a westernization of lifestyle, improved cancer surveillance in medical insurance policies and advancements in diagnostic and treatment techniques for gastrointestinal diseases. Admissions for IBD and GERD are newly emerging and appear to have increased recently, but they were still not common.9-11
Increases in the early detection of GI cancer and precancerous lesions appear to be related to the establishment of endoscopic surveillance for dyspepsia and improved public awareness regarding the merits of cancer screening. Furthermore, the higher mean age of EGCa cases during the study period, suggests that this trend will continue in parallel with population aging. Korea and Japan are the only two countries that perform endoscopic screening of the whole population for gastric cancer, and thus it is not surprising that the incidence of early cancer and the number of minimally invasive treatments have increased.12-15 In the present study, surgery was the favored modality for gastric cancer in 1990, but in 2006, the number of patients with EGCa that received endoscopic treatment and laparoscopy assisted gastrectomy greatly increased. These changes are due to the higher rates of complications of open surgery in elderly patients and increased expectations regarding quality of life after surgery. This trend was also observed for colon diseases; admission rates for colon polypectomy and the detection of focal carcinoma during polypectomy have also increased. According to the results of NCSP in Korea in 2004, 31% of those screened by colonoscopy were found to have polyps, which raised expectations regarding the detection of focal carcinoma.16 Furthermore, bypass surgery for advanced GI cancer has now been replaced with stent insertion.17,18 Accordingly, treatments will tend to become less and less invasive.
Admission rates for peptic ulcer with ulcer bleeding did not decrease over the study period, although admission rates for a perforated ulcer reduced. This may have been because of increased use of NSAIDs among the elderly, despite the eradication of H. pylori.19,20 NSAIDs related ulcers are known to be prevalent among elderly individuals with a co-morbid illness, who are known to be more prone to gastric ulcers than duodenal ulcers, which have a greater tendency to bleed than H. pylori ulcers.21 The present study also shows that the average age of peptic ulcer patients has increased. As a result of these changes, medical staff must be aware of the increasing need for NSAIDs related ulcer management in aging populations.
Increases in the incidences of colon cancer, GERD, and IBD found during this study might reflect lifestyle and diet changes associated with urbanization and growing affluence. According to recent epidemiologic studies, some of the more developed and Westernized Asian countries, such as, Japan, South Korea, and Singapore have already experienced a rapid increase in colon cancer.3,7 Old age, increased intakes of protein and fat, and lack of exercise are well known to increase the risk of colon cancer.22,23 Similarly, life style changes, such as a reduction in the amount of sodium consumed and improved hygiene, may be responsible for the decreases in gastric cancer admission rates, although the eradication of H. pylori is also considered to be an important factor for the reduction of gastric cancer rates.24-28
GERD has also been reported to be increasing in Asian countries in parallel with an increase in obesity.2,8,29-31 Increases in fat intake due to globalization and life style changes are known to increased the incidence of GERD. The frequency of GERD has been increasing in Asia, though it is less prevalent than in the West. In one comparative study, a single endoscopist found reflux esophagitis in 25% of British patients but in only 6% of Singaporean patients with similar reflux symptoms.32 In another example, the prevalence of at least monthly heartburn has been estimated to be about 29-44% in UK and US, where GERD is highly prevalent.9 However, the admissions related with complications of GERD were still very rare in this study although it appears to increase with time. Furthermore, in present study, admission rates for Barrett's esophagus and esophageal adenocarcinoma were very rare and did not increase over the study period.
Our data also showed that IBD is newly emerging over last two decades, which is believed to be uncommon in Asians. Recent studies have found significant increase in IBD rates in the Asia-Pacific region.33-37 IBD rates were found to have raised by more than three-fold in 2000s as compared with the 1980s in several studies, moving from the range of 0.1 to 7.5 cases per 100,000 persons to the rage of 7.5 to 22.3 cases by year 2000s.6,38,39 However, both incidence and prevalence rates of IBD are still low compared with Europe and North America; the prevalence of IBD in North America ranges from 37 to 246 cases per 100,000 persons for ulcerative colitis and from 26 to 199 cases per 100,000 persons for Crohn's disease.11
The data collected from a single institution for this study is considered not sufficient to represent the true data for the whole nation. However, Kangnam St. Mary's Hospital is regarded as relatively suitable to assess the changing patterns of diseases for the following reasons. First, the medical resources of this hospital have been stable and consistent over the last 20 years. Second, the surrounding area where this hospital has been serving is mostly residential and this has not changed in the last twenty years. This is in contrast to other regions of Seoul where so many drastic changes have been made over time. Despite taking into consideration all these factors, the data extracted from a single institutional study could not overcome the bias that it does not represent the true trends of GI diseases in Korea. However, on a positive note, the results obtained in this study are similar to those reported by Korean national data, for instance, the trends of change in prevalence of malignancy such as stomach and colon cancer, and IBD.5,12,16,35,37,40 Moreover, this study could provide a detailed analysis of diseases that cannot be extracted from general national data. A manual review of diagnoses in this study also minimized errors which might occur with the computerized administrative coding system.
In summary, the admission rates of gastrointestinal diseases among total inpatients at our hospital over the period 1990 to 2006 increased, as has mean inpatient age. The increased rates of colon cancer, GERD, and IBD found during this study reflect the trend toward 'Westernization' of GI disease. GI malignant diseases are still the most common cause of admission in Korea, and this is a major concern given population aging. In addition, rates of early diagnosis and of less invasive treatments for malignant diseases have increased, which is attributed to increased public awareness of cancer screening and the expansion of medical policy. In the future, it is expected that the early detection of cancer will increase and that a greater focus will be placed on quality of life.
ACKNOWLEDGEMENTS
All authors contributed significantly to this article and agree with the contents of the manuscript. Furthermore, the authors declare that they have no vested interest that could be construed to have inappropriately influenced this study.
No financial support was received for this study.
References
- 1.Shaheen NJ, Hansen RA, Morgan DR, et al. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 2006;101:2128–2138. doi: 10.1111/j.1572-0241.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- 2.Goh KL. Changing trends in gastrointestinal disease in the Asia-Pacific region. J Dig Dis. 2007;8:179–185. doi: 10.1111/j.1751-2980.2007.00304.x. [DOI] [PubMed] [Google Scholar]
- 3.International Agency for Research on Cancer (IARC) Lyon, France: IARC; 2005. [updated 2009 Oct 12]. 2007 Cancer Mondial [Internet] Available from: http://www-dep.iarc.fr. [Google Scholar]
- 4.Rajendra S, Ackroyd R, Robertson IK, Ho JJ, Karim N, Kutty KM. Helicobacter pylori, ethnicity, and the gastroesophageal reflux disease spectrum: a study from the East. Helicobacter. 2007;12:177–183. doi: 10.1111/j.1523-5378.2007.00489.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee JY, Kim HY, Kim KH, et al. No changing trends in incidence of gastric cardia cancer in Korea. J Korean Med Sci. 2003;18:53–57. doi: 10.3346/jkms.2003.18.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsugane S, Sasazuki S. Diet and the risk of gastric cancer: review of epidemiological evidence. Gastric Cancer. 2007;10:75–83. doi: 10.1007/s10120-007-0420-0. [DOI] [PubMed] [Google Scholar]
- 7.Sung JJ, Lau JY, Goh KL, Leung WK. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005;6:871–876. doi: 10.1016/S1470-2045(05)70422-8. [DOI] [PubMed] [Google Scholar]
- 8.Goh KL, Chang CS, Fock KM, Ke M, Park HJ, Lam SK. Gastro-oesophageal reflux disease in Asia. J Gastroenterol Hepatol. 2000;15:230–238. doi: 10.1046/j.1440-1746.2000.02148.x. [DOI] [PubMed] [Google Scholar]
- 9.Ho KY, Cheung TK, Wong BC. Gastroesophageal reflux disease in Asian countries: disorder of nature or nurture? J Gastroenterol Hepatol. 2006;21:1362–1365. doi: 10.1111/j.1440-1746.2006.04341.x. [DOI] [PubMed] [Google Scholar]
- 10.Ouyang Q, Tandon R, Goh KL, Ooi CJ, Ogata H, Fiocchi C. The emergence of inflammatory bowel disease in the Asian Pacific region. Curr Opin Gastroenterol. 2005;21:408–413. [PubMed] [Google Scholar]
- 11.Loftus EV., Jr Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–1517. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 12.Korean Gastric Cancer Association. Nationwide gastric cancer report in Korea. J Korean Gastric Cancer Assoc. 2002;2:105–114. [Google Scholar]
- 13.Gotoda T. Endoscopic resection of early gastric cancer. Gastric Cancer. 2007;10:1–11. doi: 10.1007/s10120-006-0408-1. [DOI] [PubMed] [Google Scholar]
- 14.Ohgami M, Otani Y, Kumai K, Kubota T, Kim YI, Kitajima M. Curative laparoscopic surgery for early gastric cancer: five years experience. World J Surg. 1999;23:187–192. doi: 10.1007/pl00013167. [DOI] [PubMed] [Google Scholar]
- 15.Kitagawa Y, Kitano S, Kubota T, et al. Minimally invasive surgery for gastric cancer--toward a confluence of two major streams: a review. Gastric Cancer. 2005;8:103–110. doi: 10.1007/s10120-005-0326-7. [DOI] [PubMed] [Google Scholar]
- 16.Korean National Cancer Center. Goyang, Korea: Korean National Cancer Center; 2009. Evaluation of the national cancer screening program 2006 [Internet] Available from: http://www.ncc.re.kr/index.jsp. [Google Scholar]
- 17.Stephenson BM, Shandall AA, Farouk R, Griffith G. Malignant left-sided large bowel obstruction managed by subtotal/total colectomy. Br J Surg. 1990;77:1098–1102. doi: 10.1002/bjs.1800771007. [DOI] [PubMed] [Google Scholar]
- 18.Siddiqui A, Khandelwal N, Anthony T, Huerta S. Colonic stent versus surgery for the management of acute malignant colonic obstruction: a decision analysis. Aliment Pharmacol Ther. 2007;26:1379–1386. doi: 10.1111/j.1365-2036.2007.03513.x. [DOI] [PubMed] [Google Scholar]
- 19.Higham J, Kang JY, Majeed A. Recent trends in admissions and mortality due to peptic ulcer in England: increasing frequency of haemorrhage among older subjects. Gut. 2002;50:460–464. doi: 10.1136/gut.50.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonnenberg A. Time trends of ulcer mortality in Europe. Gastroenterology. 2007;132:2320–2327. doi: 10.1053/j.gastro.2007.03.108. [DOI] [PubMed] [Google Scholar]
- 21.Ong TZ, Hawkey CJ, Ho KY. Nonsteroidal anti-inflammatory drug use is a significant cause of peptic ulcer disease in a tertiary hospital in Singapore: a prospective study. J Clin Gastroenterol. 2006;40:795–800. doi: 10.1097/01.mcg.0000225610.41105.7f. [DOI] [PubMed] [Google Scholar]
- 22.Yiu HY, Whittemore AS, Shibata A. Increasing colorectal cancer incidence rates in Japan. Int J Cancer. 2004;109:777–781. doi: 10.1002/ijc.20030. [DOI] [PubMed] [Google Scholar]
- 23.Chiu BC, Ji BT, Dai Q, et al. Dietary factors and risk of colon cancer in Shanghai, China. Cancer Epidemiol Biomarkers Prev. 2003;12:201–208. [PubMed] [Google Scholar]
- 24.Lu JB, Qin YM. Correlation between high salt intake and mortality rates for oesophageal and gastric cancers in Henan Province, China. Int J Epidemiol. 1987;16:171–176. doi: 10.1093/ije/16.2.171. [DOI] [PubMed] [Google Scholar]
- 25.Hirayama T. Relationship of soybean paste soup intake to gastric cancer risk. Nutr Cancer. 1982;3:223–233. doi: 10.1080/01635588109513726. [DOI] [PubMed] [Google Scholar]
- 26.You WC, Blot WJ, Chang YS, et al. Diet and high risk of stomach cancer in Shandong, China. Cancer Res. 1988;48:3518–3523. [PubMed] [Google Scholar]
- 27.Nan HM, Park JW, Song YJ, et al. Kimchi and soybean pastes are risk factors of gastric cancer. World J Gastroenterol. 2005;11:3175–3181. doi: 10.3748/wjg.v11.i21.3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim JH, Kim HY, Kim NY, et al. Seroepidemiological study of Helicobacter pylori infection in asymptomatic people in South Korea. J Gastroenterol Hepatol. 2001;16:969–975. doi: 10.1046/j.1440-1746.2001.02568.x. [DOI] [PubMed] [Google Scholar]
- 29.Ho KY, Cheung TK, Wong BC. Gastroesophageal reflux disease in Asian countries: disorder of nature or nurture? J Gastroenterol Hepatol. 2006;21:1362–1365. doi: 10.1111/j.1440-1746.2006.04341.x. [DOI] [PubMed] [Google Scholar]
- 30.Wong WM, Lam SK, Hui WM, et al. Long-term prospective follow-up of endoscopic oesophagitis in southern Chinese--prevalence and spectrum of the disease. Aliment Pharmacol Ther. 2002;16:2037–2042. doi: 10.1046/j.1365-2036.2002.01373.x. [DOI] [PubMed] [Google Scholar]
- 31.Lim SL, Goh WT, Lee JM, Ng TP, Ho KY. Changing prevalence of gastroesophageal reflux with changing time: longitudinal study in an Asian population. J Gastroenterol Hepatol. 2005;20:995–1001. doi: 10.1111/j.1440-1746.2005.03887.x. [DOI] [PubMed] [Google Scholar]
- 32.Kang JY, Ho KY. Different prevalences of reflux oesophagitis and hiatus hernia among dyspeptic patients in England and Singapore. Eur J Gastroenterol Hepatol. 1999;11:845–850. doi: 10.1097/00042737-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Morita N, Toki S, Hirohashi T, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30(Suppl 8):1–4. [PubMed] [Google Scholar]
- 34.Jiang XL, Cui HF. An analysis of 10218 ulcerative colitis cases in China. World J Gastroenterol. 2002;8:158–161. doi: 10.3748/wjg.v8.i1.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang SK. Current status and clinical characteristics of inflammatory bowel disease in Korea. Korean J Gastroenterol. 2002;40:1–14. [Google Scholar]
- 36.Lee YM, Fock K, See SJ, Ng TM, Khor C, Teo EK. Racial differences in the prevalence of ulcerative colitis and Crohn's disease in Singapore. J Gastroenterol Hepatol. 2000;15:622–625. doi: 10.1046/j.1440-1746.2000.02212.x. [DOI] [PubMed] [Google Scholar]
- 37.Yang SK, Hong WS, Min YI, et al. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol. 2000;15:1037–1042. doi: 10.1046/j.1440-1746.2000.02252.x. [DOI] [PubMed] [Google Scholar]
- 38.Yao T, Matsui T, Hiwatashi N. Crohn's disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000;43(10 Suppl):S85–S93. doi: 10.1007/BF02237231. [DOI] [PubMed] [Google Scholar]
- 39.Ouyang Q, Tandon R, Goh KL, Ooi CJ, Ogata H, Fiocchi C. The emergence of inflammatory bowel disease in the Asian Pacific region. Curr Opin Gastroenterol. 2005;21:408–413. [PubMed] [Google Scholar]
- 40.Bae JM, Jung KW, Won YJ. Estimation of cancer deaths in Korea for the upcoming years. J Korean Med Sci. 2002;17:611–615. doi: 10.3346/jkms.2002.17.5.611. [DOI] [PMC free article] [PubMed] [Google Scholar]