Abstract
Background/Aims
Although gastric hyperplastic polyps are usually considered as benign lesions, a low risk of carcinomatous conversion is currently recognized. We aimed to identify the characteristics of hyperplastic polyps undergoing neoplastic transformation.
Methods
A total of 269 gastric hyperplastic polyps from 216 patients removed by endoscopic polypectomy (EP) or surgical resection were enrolled in this study, and their endoscopic pictures and pathology slides were reviewed.
Results
Neoplastic transformation was detected on forceps biopsy specimen in 11 cases. However, the pathology findings from the EP or surgical specimen revealed neoplastic transformation in 14 cases (5.2%; 4 with dysplasia and 10 with adenocarcinoma). No significant difference was found between hyperplastic polyps with and without neoplastic transformation in age, sex, location, number of polyps or gross appearance. However, neoplastic transformations were more frequently found in gastric hyperplastic polyps >1 cm than in polyps ≤1 cm (12 of 143; 8.4% vs. 2 of 126; 1.6%) (p=0.013).
Conclusions
Neoplastic transformations were more frequently found in gastric hyperplastic polyps >1 cm. Therefore, EP should be considered for gastric hyperplastic polyps >1 cm for the accurate diagnosis and definitive treatment.
Keywords: Hyperplastic polyp, Neoplastic transformation, Endoscopic polypectomy
INTRODUCTION
Gastric hyperplastic polyps are lesions characterized by hyperplastic, elongated, or dilated foveolar epithelium within a congested and inflamed lamina propria.1 They comprise approximately 70 to 90% of all gastric epithelial polyps.1-3 Although gastric hyperplastic polyps are generally regarded as benign lesions, malignant transformations have been reported in several studies.4-8 The reported incidence of malignant transformation ranged from 1.5 to 2.1% of gastric hyperplastic polyps.4,6,9,10 Previous studies showed that the larger gastric hyperplastic polyps had a higher possibility of malignant transformation.4,10,11 Therefore, Rosen et al.8 suggested that gastric hyperplastic polyps larger than 2 cm should be removed by either endoscopic or surgical resection. However, hyperplastic polyps smaller than 2 cm in size have also been reported as showing malignant changes.9,10,12 Furthermore, the diagnosis solely based on forceps biopsy specimens carries the risk of missing the neoplastic foci within hyperplastic polyps due to sampling errors.9,12,13 Actually, we recently experienced several cases whose initial diagnoses of gastric hyperplastic polyps based on forceps biopsy specimen were changed after endoscopic polypectomy (EP) was performed; where the specimens obtained from same lesions revealed the coexisting dysplasia or cancer foci. For these reasons, some authorities have argued that gastric hyperplastic polyps exceeding 5 mm should be removed.12,13 However, considering the low risk of malignant transformations and the complications and costs of EP or surgical resection, it may be unreasonable and impractical to resect all gastric hyperplastic polyps exceeding 5 mm. Therefore, if we could identify the characteristics of hyperplastic polyps undergoing neoplastic transformation, it would be very helpful for making a clinical decision between endoscopic resection and close follow-up.
In this study, we aimed to identify the characteristics of hyperplastic polyps undergoing neoplastic transformation.
MATERIALS AND METHODS
1. Patients
Between May 1995 and September 2008, a total of 355 gastric hyperplastic polyps from 256 patients were resected by EP or surgery at the Samsung Medical Center. After excluding the cases associated with polyposis syndrome (n=34) and cases without endoscopic pictures (n=52), a total of 269 gastric hyperplastic polyps from 216 patients were finally enrolled in this study. Of these polyps, three were surgically removed and all the others were removed by EP. At our institution, EP is indicated and recommended for the lesion diagnosed as hyperplastic polyp by forceps biopsy if the lesion is ≥1.0 cm in size. In cases with a lesion <1.0 cm, we explain the natural history of hyperplastic polyp and the risks associated with EP to the patients and discuss the treatment plan with them to decide between a resection and close follow-up. All the cases undergoing surgical resection were initially diagnosed to have cancerous transformation by forceps biopsy. All the patients undergoing EP or surgery provided written informed consent for the procedures.
Endoscopy reports were reviewed for size and location of gastric hyperplastic polyp. In this study, the size was defined as the longest diameter of the lesion measured by biopsy forceps during endoscopy procedure. Endoscopy pictures were reviewed for shape of lesion, presence of hyperemia and presence of nodularity. This review was performed by an experienced endoscopist (A.R. Han) who was blinded to the original pathological results. Medical records were also reviewed for clinical features using hospital intranet resources. The histopathology of the specimens was reviewed by an experienced pathologist (C.O. Sung) who had no information on the original pathological results. The diagnosis of malignant transformation and gastric dysplasia was based on the Vienna classification of gastrointestinal neoplasia.14
2. Statistical analysis
Comparisons of clinicopathological and endoscopic data between the hyperplastic polyps with and without neoplastic transformation were performed using Pearson χ2 test, Fisher's exact test and Mann-Whitney U test. Values of p<0.05 were considered to be significant.
RESULTS
1. Gastric hyperplastic polyps with neoplastic transformation
Among the 269 gastric hyperplastic polyps enrolled, fourteen polyps showed neoplastic transformations in EMR or surgical specimens. Characteristics of these fourteen hyperplastic polyps with neoplastic transformation are shown in Table 1. There were 8 (57%) males and 6 (43%) females. The median age was 64 years with a range of 49-71 years. Initial diagnoses by endoscopic forceps biopsy were as follows; hyperplastic polyps in 3 cases, gastric dysplasia in 5 cases and adenocarcinoma in 6 cases. Gastric hyperplastic polyps were single in 10 (71%) patients and multiple in 4 (29%) patients. The body was the most common location of these polyps, which were distributed as follows: 9 (64%) in the body, 3 (22%) in the antrum and 2 (14%) in the cardia. One (7%) gastric polyp was sessile and ten (93%) were pedunculated. The size of these polyps ranged from 0.5 cm to 3.5 cm in their major diameter. Only two (14%) of these polyps were smaller than 1 cm, while twelve (86%) were larger than 1 cm. Twelve (86%) hyperplastic polyps showed hyperemia. Eleven (79%) hyperplastic polyps showed nodularity (Figs. 1 and 2).
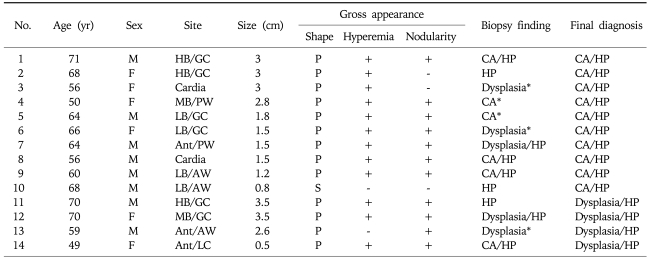
Table 1.
Summary of Data on Gastric Hyperplastic Polyps with Neoplastic Transformations
M, male; HB, high body; GC, great curvature; P, pedunculated; CA, adenocarcinoma; HP, hyperplastic polyp; F, female; MB, mid body; PW, posterior wall; LB, low body; AW, anterior wall; S, sessile; Ant, antrum; LC, lesser curvature.
*Initial forceps biopsies failed to identify the presence of hyperplastic polyp.
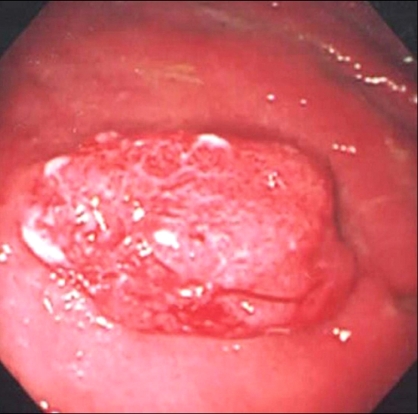
Fig. 1.
Endoscopic finding of the case of hyperplastic polyp with neoplastic transformation. A 3.5 cm sized pedunculated lesion was observed at the greater curvature side of the high body. The polyp showed nodular surface and hyperemic discoloration. The pathology findings from the forceps biopsy showed hyperplastic polyp. However, pathology findings following endoscopic mucosal resection showed dysplasia arising from hyperplastic polyp.
Fig. 2.

Endoscopic finding of the case of hyperplastic polyp with malignant transformation. A 1.5 cm sized pedunculated lesion was observed at the posterior portion of the antrum. The polyp showed nodular surface and hyperemic discoloration. The pathology findings from the forceps biopsy showed hyperplastic polyp with dysplasia. However, pathology findings following endoscopic mucosal resection showed adenocarcinoma arising from hyperplastic polyp.
As mentioned above, cancerous changes were found in 10 (3.7%) of 269 hyperplastic polyps. Histology showed well or moderately differentiated tubular adenocarcinoma in nine lesions and papillary adenocarcinoma in one lesion. Nine of these cancers were localized to the mucosal layer, and only one case showed invasion of the submucosal layer. Dysplastic changes were found around the cancerous components in all of the ten lesions. In 4 (1.5%) of 269 gastric hyperplastic polyps, dysplastic changes were found. Three of these lesions showed high-grade dysplasia. The boundary between the dysplastic area and hyperplastic component was comparatively distinct (Figs. 3 and 4).
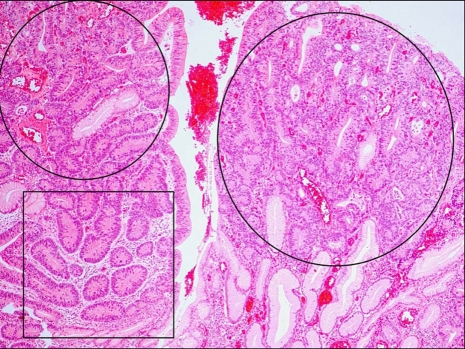
Fig. 3.
Micrograph of an adenocarcinoma arising from a hyperplastic polyp (circle) (H&E stain, ×40). Dysplastic foci were found around the cancerous components (square).
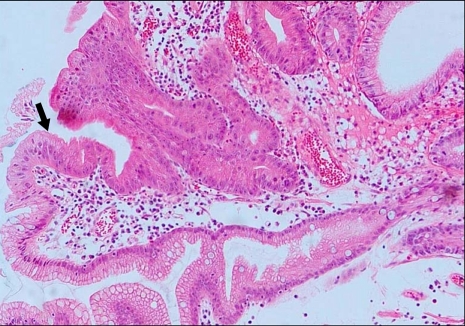
Fig. 4.
Micrograph of a hyperplastic polyp with dysplasia (H&E stain, ×100). The boundary between the dysplastic foci and the hyperplastic foveolar epithelium was distinct (long arrow).
2. Comparison of clinical and endoscopic features between the pure gastric hyperplastic polyps and gastric hyperplastic polyps with neoplastic transformation
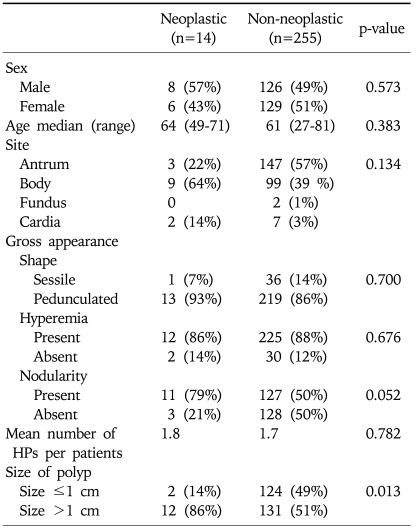
No significant difference was found between the age or sex of patients with hyperplastic polyps with or without neoplastic transformations. In addition, there was no significant difference between the two groups in the number, location, or gross appearance of polyps (Table 2). However, neoplastic transformations were more frequently found in gastric hyperplastic polyps larger than 1 cm (12 of 143; 8.4%) than in polyps smaller than 1 cm (2 of 126; 1.6%) (p=0.013).
Table 2.
Comparison Data on Gastric Hyperplastic Polyps with or without Neoplastic Transformations
HP, hyperplastic polyp.
DISCUSSION
Gastric hyperplastic polyps are the most common gastric polyps and are generally considered as relatively harmless lesions. However, several studies showed that malignant transformations occur in approximately 2% of gastric hyperplastic polyps.4,6,9,10 In this study, fourteen (5.2%) of the 269 gastric hyperplastic polyps showed neoplastic transformations, and ten (3.7%) of these polyps contained cancerous components.
The mechanism of carcinogenesis in gastric hyperplastic polyps is still unknown. However, it has been suggested that malignant transformations of gastric hyperplastic polyps arise from the dysplastic epithelium rather than directly from the hyperplastic epithelium because cancerous lesions exist either in the dysplastic lesions or adjacent to the dysplastic lesions.4,6,9,12 In this study, adenomatous changes were observed around the cancerous component in all of the gastric hyperplastic polyps with malignant transformations. Therefore, our study supports the previous findings that cancer cells arise from dysplastic areas in hyperplastic polyps rather than directly from the non-dysplastic hyperplastic epithelium. In other studies, p53 protein overexpression was detected in neoplastic components of gastric hyperplastic polyps, and its incidence did not differ between polyps with dysplasia and those with carcinoma.10,15 Yao et al.15 suggested that p53 protein accumulation was associated with early phase carcinogenesis in gastric hyperplastic polyps because of the high prevalence of immunoreactivity found in dysplasia.
In this study, three of the hyperplastic polyps with neoplastic transformation failed to demonstrate any dysplastic foci on forceps biopsy. This discrepancy between the forceps biopsy samples and endoscopically resected specimens including whole hyperplastic polyps has been shown in other studies.9,12,13 Therefore, a diagnosis based on the endoscopic forceps biopsy may sometimes be inaccurate. In our study, neoplastic transformations were more frequently found in gastric hyperplastic polyps larger than 1 cm than in polyps smaller than 1 cm (8.4% vs 1.6%). Other studies also showed that most hyperplastic polyps harboring cancer were larger than 1 cm in size.4,9,16,17 Therefore, EP should be considered for gastric hyperplastic polyps larger than 1 cm to avoid the risk of missing lesions with neoplastic transformations, although attention should also be paid to hyperplastic polyps less than 1 cm.
The present study was limited by the possible selection bias as this study enrolled and analyzed only the cases undergoing endoscopic or surgical resection. However, this kind of study design was inevitable as this study aimed to identify the characteristics of gastric hyperplastic polyps undergoing neoplastic transformations which were difficult to diagnose only by forceps biopsy specimens.
In conclusion, we found that neoplastic transformations were more frequently found in gastric hyperplastic polyps >1 cm than in polyps ≤1 cm. In addition, the results of this study showed the diagnoses solely based on forceps biopsy specimens carried the risk of missing dysplasia or cancer foci within gastric hyperpalstic polyps. Considering these points, EP should be considered for gastric hyperplastic polyps >1 cm to avoid the risk of missing the lesions with neoplastic transformations.
ACKNOWLEDGEMENTS
This work was supported by a grant from the Samsung Medical Center Clinical Research Development Program (CRS-107-33-3).
References
- 1.Snover DC. Benign epithelial polyps of the stomach. Pathol Annu. 1985;20 Pt 1:303–329. [PubMed] [Google Scholar]
- 2.Deppisch LM, Rona VT. Gastric epithelial polyps. A 10-year study. J Clin Gastroenterol. 1989;11:110–115. doi: 10.1097/00004836-198902000-00028. [DOI] [PubMed] [Google Scholar]
- 3.Seifert E, Gail K, Weismuller J. Gastric polypectomy. Long-term results (survey of 23 centres in Germany) Endoscopy. 1983;15:8–11. doi: 10.1055/s-2007-1018596. [DOI] [PubMed] [Google Scholar]
- 4.Daibo M, Itabashi M, Hirota T. Malignant transformation of gastric hyperplastic polyps. Am J Gastroenterol. 1987;82:1016–1025. [PubMed] [Google Scholar]
- 5.Orlowska J, Pietrow D. Multifocal gastric carcinoma arising from hyperplastic and adenomatous polyps. Am J Gastroenterol. 1990;85:1629–1634. [PubMed] [Google Scholar]
- 6.Orlowska J, Jarosz D, Pachlewski J, Butruk E. Malignant transformation of benign epithelial gastric polyps. Am J Gastroenterol. 1995;90:2152–2159. [PubMed] [Google Scholar]
- 7.Remmele W, Kolb EF. Malignant transformation of hyperplasiogenic polyps of the stomach: case report. Endoscopy. 1978;10:63–65. doi: 10.1055/s-0028-1098265. [DOI] [PubMed] [Google Scholar]
- 8.Rosen S, Hoak D. Intramucosal carcinoma developing in a hyperplastic gastric polyp. Gastrointest Endosc. 1993;39:830–833. doi: 10.1016/s0016-5107(93)70280-1. [DOI] [PubMed] [Google Scholar]
- 9.Hizawa K, Fuchigami T, Iida M, et al. Possible neoplastic transformation within gastric hyperplastic polyp. Application of endoscopic polypectomy. Surg Endosc. 1995;9:714–718. doi: 10.1007/BF00187948. [DOI] [PubMed] [Google Scholar]
- 10.Zea-Iriarte WL, Sekine I, Itsuno M, et al. Carcinoma in gastric hyperplastic polyps. A phenotypic study. Dig Dis Sci. 1996;41:377–386. doi: 10.1007/BF02093832. [DOI] [PubMed] [Google Scholar]
- 11.Kamiya T, Morishita T, Asakura H, Munakata Y, Miura S, Tsuchiya M. Histoclinical long-standing follow-up study of hyperplastic polyps of the stomach. Am J Gastroenterol. 1981;75:275–281. [PubMed] [Google Scholar]
- 12.Ginsberg GG, Al-Kawas FH, Fleischer DE, Reilly HF, Benjamin SB. Gastric polyps: relationship of size and histology to cancer risk. Am J Gastroenterol. 1996;91:714–717. [PubMed] [Google Scholar]
- 13.Muehldorfer SM, Stolte M, Martus P, Hahn EG, Ell C. Diagnostic accuracy of forceps biopsy versus polypectomy for gastric polyps: a prospective multicentre study. Gut. 2002;50:465–470. doi: 10.1136/gut.50.4.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–255. doi: 10.1136/gut.47.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yao T, Kajiwara M, Kuroiwa S, et al. Malignant transformation of gastric hyperplastic polyps: alteration of phenotypes, proliferative activity, and p53 expression. Hum Pathol. 2002;33:1016–1022. doi: 10.1053/hupa.2002.126874. [DOI] [PubMed] [Google Scholar]
- 16.Yamaguchi K, Shiraishi G, Maeda S, Kitamura K. Adenocarcinoma in hyperplastic polyp of the stomach. Am J Gastroenterol. 1990;85:327–328. [PubMed] [Google Scholar]
- 17.Gotoh Y, Fujimoto K, Sakata Y, Fujisaki J, Nakano S. Poorly differentiated adenocarcinoma in a gastric hyperplastic polyp. South Med J. 1996;89:453–454. doi: 10.1097/00007611-199604000-00026. [DOI] [PubMed] [Google Scholar]