Abstract
Background/Aims
Common bile duct stones are associated with the extent of dilation of the common bile duct as well as its angulation. Multidetector computed tomography (MD CT) has a good resolution for the definition of the anatomical features of the common bile duct.
Methods
The multiplanar reformation images of 398 patients that underwent multidetector CT for the diagnosis of disorders not related to the bile duct were examined. The diameter and angulation were categorized by gender and age.
Results
The average diameter and angulation of the common bile duct was 6.7 mm and 132.6°. There was a statistically significant correlation between age and the common bile duct diameter. The Pearson correlation analysis for age and diameter resulted in a value of 0.415 (p<0.001). And the common bile duct (CBD) diameter in people older than 51 years of age showed a significant difference compared to the subjects younger than 50 years of age (p<0.01). However, the degree of angulation has no correlation with age.
Conclusions
We suggest that CBD diameters in patients more than 50 years of age can be more than 7 mm and be within normal limits.
Keywords: Computed tomography, Common bile duct, Angle, Diameter
INTRODUCTION
Technologic advances in computed tomography (CT) scanning have resulted in continued improvement of the spatial resolution and CT evaluation of the biliary system. Current CT technology provides sufficient anatomic resolution to visualize the extrahepatic bile ducts in the majority of patients.1 The common bile duct (CBD) is generally described as deviating to the right as it descends toward the duodenum.2 This deviation, is referred to as "angulation," in the current study. It has been suggested that the angulation, along the course of the CBD, may predispose patients to bile stasis and thus promote stone formation.3 Duct dilation also may promote stasis.4 However, there is limited standard measurement data available on the normal CBD in Koreans that could be used to refer to for the diagnosis of choledocholitiasis. The aim of this study was to determine the normal angulation and dilation parameters of the CBD in Koreans using multidetector computed tomography (MD CT). Measurements of the CBD diameter, and angulation using the MD CT were categorized by gender and age.
MATERIALS AND METHODS
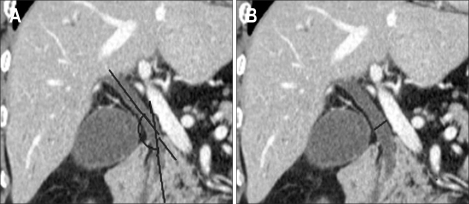
We retrospectively collected data on 398 patients, aged 20 years or older that underwent MD CT at our center, between January 2005 and April 2008. The study group consisted of patients who underwent CT for viral hepatitis, alcoholic liver disease, alcoholic pancreatitis, and cancer staging in Department of Gastroenterology. None of the patients had a history of biliary disease or surgery. Patients with choledocholithiasis or any gallbladder abnormality, previous cholecystectomy, or cholangitis were excluded. And the multiplanar reconstruction (MPR) image was not satisfactory to measure CBD diameter or angle also excluded. A 16-detector row spiral CT scanner with a gantry rotation time of 0.5 seconds was used for the biliary system. The investment volume included the whole abdomen from the dome of the diaphragm to the lower margin of the symphysis pubis. The CT examination was performed using 16×1.5 mm collimation and a table feed rate of 24 mm per gantry rotation. The volume data of both the arterial and portal-phased scans was reconstructed at 2 mm thickness with a 1 mm interval. The axial images of both the portal and arterial phases and the coronal image of the arterial phase were reformatted for routine study. We acquired additional MPR images at various angles and the curved MPR images from the volume data using PC based three dimensional software. The CBD was defined as the entire bile duct from the ampulla to the bifurcation. The angulation and diameter of the CBD were measured from the MPR images. The angulation was measured as the sharpest angle along the CBD from 1 cm below the bifurcation to 1 cm above the papilla. On the MPR image, the angle was measured at the intersection of imaginary lines drawn down the center of the bile duct. The CBD diameter was measured at its widest point (Fig. 1). Measurements were performed from inner to inner walls of the ducts using electronic calipers. MD CT analysis was performed by one investigator. All statistical analyses were performed with a statistical software program (SPSS ver. 12.0; SPSS Inc., Chicago, IL, USA). Data were expressed as the mean standard error of the mean. The Pearson's correlation, linear regression, and one-way ANOVA were used for statistical analysis. Statistical significance was set at p<0.05.
Fig. 1.
The method of measured the angulation and diameter of the common bile duct (CBD). (A) The angulation was measured as the sharpest angle. On the MPR image, the angle was measured at the intersection of imaginary lines drawn down the center of the bile duct. (B) The CBD diameter was measured at its widest point.
RESULTS
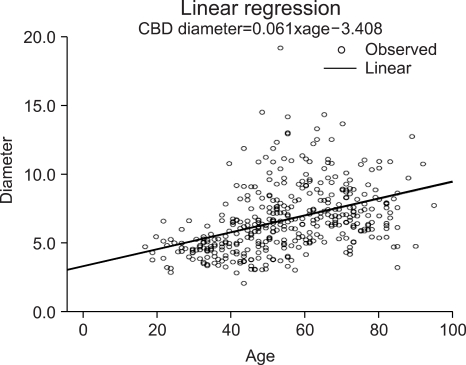
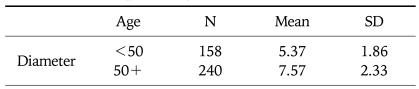
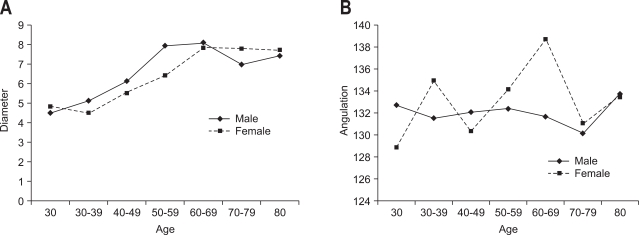
The study group consisted of 398 patients that underwent MD CT for reasons other than biliary disease such as liver cirrhosis, viral hepatitis, liver abscess, or alcoholic pancreatitis. No patient had evidence of a CBD stone or cholangitis. The study population consisted of 159 women and 239 men with a mean age of 54.4±16.49 years (Table 1). The average diameter of the CBD was 6.70±2.41 mm. The CBD diameter for men and women were 6.757±2.594 mm and 6.618±2.100 mm, respectively, which did not show a significant difference. However, the CBD diameter was strongly correlated with increasing age. The Pearson correlation analysis for age and diameter resulted in a value of 0.415 (p<0.001). According to the linear periodic model, the confidence level was 0.123(r2) and showed a regression equation with a diameter=0.061×age-0.3408. These data are presented in Fig. 2. The CBD diameter in people older than 51 years of age showed a significant difference compared to the subjects younger than 50 years of age (Table 2). The one way ANOVA of the CBD diameter and age showed a statistically significant difference between the two age groups (p<0.05). A significant difference was also observed with the Tukey method (Table 3). The mean CBD angulation was 132.56±13.47° in patients. The results of the univariate analysis for angulation of the CBD in association with age and gender are presented in Fig. 3. Angulation did not show a significant difference between men (131.93±13.656°) and women (133.499±13.189°). There was no correlation (Pearson correlation 0.041) between age and the degree of angulation.
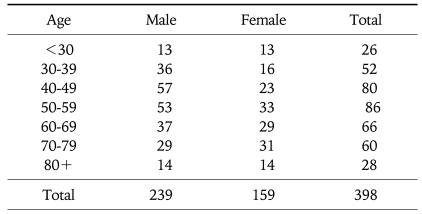
Table 1.
The Study Population by Age and Gender
p<0.001.
Fig. 2.
The correlation between the common bile duct diameter and age of patients.
Table 2.
The Difference in the Common Bile Duct Diameter between the Groups: Younger than 50 and Older than 51
p<0.05.
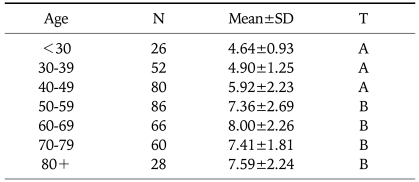
Table 3.
Means, SDs, and Ranges of the Common Bile Duct Diameter by Age
p<0.05.
*T: The same letters indicate non-significant difference between groups based on Tukey's multiple comparison test.
Fig. 3.
Univariate analysis of the common bile duct diameter (A) and angulation (B) by age and gender.
DISCUSSION
The imaging evaluation of patients with suspected extrahepatic bile duct abnormalities includes noninvasive imaging modalities such as ultrasound and magnetic resonance imaging (MRI). The primary use of CT for extrahepatic biliary duct lesions has traditionally had limited detection. However, with intravenously administered contrast agents, combined with high resolution helical scanning the diagnosis of the biliary system has improved. Furthermore, the development of the MD CT has increased the accuracy of CT. Many patients presenting with acute abdominal pain undergo a diagnostic CT scan as part of the acute workup. Thus, CT is more frequently used as an initial diagnostic modality for biliary disease. However, the normal range of CT findings for the biliary anatomy is unknown. Therefore, determination of the normal measurements of the CBD by CT will be helpful for the diagnosis of abnormal findings of the biliary system. Angulation and dilatation of the CBD may predispose to bile stasis. Bile stasis is thought to be an important factor in the pathogenesis of bile duct stones.5 Our results showed a significant correlation between enlargement of the CBD diameter and age. These results are in agreement with the findings of Bachar et al.6 where 251 patients without biliary, pancreatic, or hepatic disease were studied. They measured the maximal anteroposterior and transverse diameters of the extrahepatic bile duct at three locations with ultrasound: in the porta hepatic region, the most distal aspect of the head of the pancreas, the distal aspect of the head of the pancreas, and midway between these points. They found a significant correlation between the CBD diameter and age (r=0.535; p<0.001; r2=0.28). The enlargement of the CBD diameter with increasing age may be explained by fragmentation of the longitudinal smooth myocyte bands and intervening connective tissues, and loss of the reticulo-elastic network of the duct wall with aging.7 Same result was reported from Barthet et al.8 To determine the influence of age and biliary lithiasis, they measured CBD diameter with endoscopic retrograde cholagniopancreatography in patients presenting or with a past-history of biliary lithiasis. The diameter of the biliary ducts was significantly correlated with age (r=0.27; p=0.001). We found a significant difference between the younger than 50 age group and the group older than 51 years of age. The diameter was significantly increased in the patients older than 51. In a study form Korea, Kim et al.9 also reported that the mean maximal and midportion diameter of CBD were significantly wider in patients over the age of 40 years compared with patients less than 40 years of age (p<0.05). This suggests that an age-related progressive increase in CBD duct diameter occurs physiologically. These results are consistent with those of Bacher et al.6 who found a significant difference between the groups younger than 50 and older than 51 years of age: 3.13±0.86 vs 4.19±1.15 mm (p<0.001). In addition, they also found that the duct gradually dilated 0.04 mm/y. Wu et al.10 reported that the diameter of the CBD normally increases by 1 mm every decade. However, according to the results of our investigation, the mean diameter of the duct did not show a gradual increase by decade. The commonly cited upper normal diameter of the adult CBD has been reported to be 6 to 7 mm.11,12 We found that the mean CBD diameter in the patients older than 51 was enlarged to more than 7 mm. These findings suggest that CBD diameters in patients more than 50 years of age can be more than 7 mm and be within normal limits. However, we could not determine the upper limit of normal of the CBD diameter in this study. We did not have a representative sample of all age ranges. The CBD angulation is a feature that has attracted little investigative attention. A few investigators have reported that an angulated bile duct might contribute to bile stasis. Warren reported an association between choledocholithiasis and a more acute cholangiographic angulation of the CBD at cholecystectomy.2 The mean angulation of the duct was 135.7° in patients with cholecystolithiasis only, compared to 103.4° in patients with concurrent choledocholithiasis. We found that the angulation of the CBD in Koreans was 132.56°. The angulation did not show a significant difference between men (131.93±13.656°) and women (133.499±13.189°). In addition, we found that the CBD angulation was not correlated with age. There were some limitations in our study. This is a retrospective study. Thus, we could not evaluated flank size and body weight of patient that would be related with CBD diameter of patient. We will be study that the correlation with the body weight and flank size of patient and CBD diameter. In conclusion, the average diameter and angle of CBD in Koreans was 6.70 mm and 132.56°. The CBD diameter changed with age. And we found that the mean CBD diameter in the patients older than 51 was enlarged to more than 7 mm. These findings suggest that CBD diameters in patients more than 50 years of age can be more than 7 mm and be within normal limits. However, the CBD angulation was not associated with age. In addition, there was no association found between gender and CBD diameter or angulation. Future prospective studies are warranted to confirm the clinical significance of these findings.
References
- 1.Schulte SJ, Baron RL, Teefey SA, et al. CT of the extrahepatic bile ducts: wall thickness and contrast enhancement in normal and abnormal ducts. AJR Am J Roentgenol. 1990;154:79–85. doi: 10.2214/ajr.154.1.2104731. [DOI] [PubMed] [Google Scholar]
- 2.Warren BL. Association between cholangiographic angulation of the common bile duct and choledocholithiasis. S Afr J Surg. 1987;25:13–15. [PubMed] [Google Scholar]
- 3.Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc. 2006;20:1594–1599. doi: 10.1007/s00464-005-0656-x. [DOI] [PubMed] [Google Scholar]
- 4.Burdiles P, Csendes A, Diaz JC, et al. Histological analysis of liver parenchyma and choledochal wall, and external diameter and intraluminal pressure of the common bile duct in controls and patients with common bile duct stones with and without acute suppurative cholangitis. Hepatogastroenterology. 1989;36:143–146. [PubMed] [Google Scholar]
- 5.Bergman JJ, van der Mey S, Rauws EA, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–649. doi: 10.1016/s0016-5107(96)70045-7. [DOI] [PubMed] [Google Scholar]
- 6.Bachar GN, Cohen M, Belenky A, Atar E, Gideon S. Effect of aging on the adult extrahepatic bile duct: a sonographic study. J Ultrasound Med. 2003;22:879–882. doi: 10.7863/jum.2003.22.9.879. [DOI] [PubMed] [Google Scholar]
- 7.Kialian GP, Aznaurian AV. The age-related characteristics of the muscular layer of the common bile duct in man. Morfologiia. 1995;108:10–12. [PubMed] [Google Scholar]
- 8.Barthet M, Spinoza S, Affriat C, Berthezene P, Sahel J. Influence of age and biliary lithiasis on the diameter of the common bile duct. Gastroenterol Clin Biol. 1995;19:156–160. [PubMed] [Google Scholar]
- 9.Kim HJ, Kim MH, Lee SK, et al. Normal structure, variations, and anomalies of the pancreaticobiliary ducts of Koreans: a nationwide cooperative prospective study. Gastrointest Endosc. 2002;55:889–896. doi: 10.1067/mge.2002.124635. [DOI] [PubMed] [Google Scholar]
- 10.Wu CC, Ho YH, Chen CY. Effect of aging on common bile duct diameter: a real-time ultrasonographic study. J Clin Ultrasound. 1984;12:473–478. doi: 10.1002/jcu.1870120804. [DOI] [PubMed] [Google Scholar]
- 11.Perret RS, Sloop GD, Borne JA. Common bile duct measurements in an elderly population. J Ultrasound Med. 2000;19:727–730. doi: 10.7863/jum.2000.19.11.727. [DOI] [PubMed] [Google Scholar]
- 12.Kaim A, Steinke K, Frank M, et al. Diameter of the common bile duct in the elderly patient: measurement by ultrasound. Eur Radiol. 1998;8:1413–1415. doi: 10.1007/s003300050563. [DOI] [PubMed] [Google Scholar]