Abstract
Background/Aims
Deterioration of renal function in cirrhotic patients with spontaneous bacterial peritonitis (SBP) is a predictor for in-hospital mortality; however, the clinical significance of renal dysfunction during bacterial infection other than SBP is unknown. The aim of this study was to investigate the prevalence and clinical significance of renal dysfunction due to bacterial infections other than SBP in patients with liver cirrhosis.
Methods
Retrospective data from inpatients with bacterial infections other than SBP were analyzed.
Results
Eighty patients were recruited for the analysis. The types of infections included that of urinary tract (37.5%), pneumonia (23.8%), biliary tract (20%), cellulitis (12.5%), and bacteremia of unknown origin (6.3%). Renal dysfunction developed in 29 patients (36.3%), of which 11 patients had irreversible renal dysfunction. The initial MELD score, neutrophil count, albumin, and blood pressure were significant risk factors in the univariate analysis, whereas only the MELD score was an independent risk factor for the development of renal dysfunction (p<0.001) after multivariate analysis.
Conclusions
The prevalence of renal dysfunction during bacterial infection other than SBP in patients with liver cirrhosis was 36.3%, and its development was related to the severity of the liver disease. Occurrence of irreversible renal dysfunction seemed to affect the prognosis of these patients.
Keywords: Liver cirrhosis, Bacterial infection, Renal dysfunction
INTRODUCTION
Bacterial infection is a complication that occurs at a higher incidence in patients with liver cirrhosis.1-4 In particular, cases in which renal dysfunction occurs during the course of bacterial infection have a poor prognosis, and renal dysfunction is a key indicator predicting death in patients with bacterial infection.1 Bacterial infections commonly observed in patients with liver cirrhosis are, in descending order of frequency, urinary tract infection, pneumonia, and spontaneous bacterial peritonitis (SBP).5-8
Most of the studies concerned about the clinical significance of renal dysfunction in patients with SBP.9-11 In patients with bacterial infection other than SBP, despite its higher prevalence, the clinical significance of renal dysfunction which might have the same pathophysiology as SBP, has not been thoroughly examined.
The objectives of this study were to examine the incidence of renal dysfunction in the presence of bacterial infections other than SBP and to evaluate the incidence, risk factors, and prognosis for irreversible renal dysfunction.
MATERIALS AND METHODS
1. Patients
The current study included patients with liver cirrhosis resulted from bacterial infections other than SBP and who were hospitalized at our medical institution between 1 January 2005 and 30 May 2008. Diagnosis of liver cirrhosis was made based on clinical, radiological, or histopathological findings. Diagnostic criterias for each bacterial infection were as follows. Pneumonia was diagnosed when chest X-ray abnormalities was accompanied by fever, coughing, and leukocytosis. Urinary tract infection was diagnosed when fever and recurrent urinary tract symptoms that were positive for bacteriuria by urine culture existed. Biliary tract infection was suggested when fever, abdominal pain, leukocytosis, coexisted with findings suggestive of biliary tract infection on ultrasonography or abdominal CT scans. Gastrointestinal infection was defined as having vomiting, diarrhea, fever, abdominal pain, leukocytosis, and positive findings on a stool culture test. Cellulitis was defined as a skin infection, fever, and leukocytosis. Bacteremia of unknown origin was defined as positive findings on a blood culture in the absence of other infectious causes.4,8 For cases who had ascite, ascitic fluid culture and analysis were done to exclude SBP and culture-negative neutrocytic ascites.
Renal dysfunction following bacterial infection was defined as >50% increase in serum creatinine level over the base line value with abnormal peak serum creatinine level (>1.5 mg/dL) after the bacterial infection was diagnosised.12 Reversible renal dysfunction was defined as return to that of the normal value in 2 weeks of treatment period after renal dysfunction occurred. For cases in which the serum creatinine levels did not return to that of the normal value in 2 weeks of treatment period or were persistently elevated, an irreversible renal dysfunction was diagnosed.
2. Methods
The clinical characteristics and serum biochemistry findings, including age, gender, blood pressure, liver cirrhosis etiology, type of bacterial infection, Child-Pugh score, WBC count, prothrombin time, Model for End-Stage Liver Disease (MELD) score, and serum sodium, BUN, creatinine, bilirubin, and albumin concentrations during the course of bacterial infection, were retrospectively analyzed in all patients to determine risk factors for renal dysfunction.
3. Statistical analysis
The data are expressed as mean±standard error (SE) or number and percentage. Continuous variables were analyzed using independent t-test, and discontinuous variables were analyzed with Pearson's chi-square or Fisher's exact test. Multivariate analysis was performed using a multiple logistic regression for variables with significant p-values in univariate analysis. All statistical analyses were performed with SPSS (Windows release 10.0; SPSS Inc., Chicago, IL, USA). A p value <0.05 was considered significant.
RESULTS
1. Patient characteristics and overall incidence of renal dysfunction
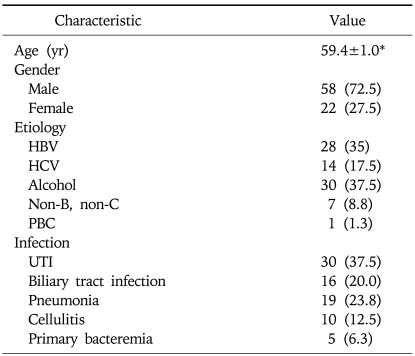
The current study was conducted with 80 patients who were hospitalized at our medical institution due to liver cirrhosis accompanied by a bacterial infection other than SBP. The mean age was 59.4±1.0 years; the male-to-female ratio was 7:3. Causative factors for liver cirrhosis included alcoholic liver disease in 30 patients, chronic hepatitis B in 28, chronic hepatitis C in 14, unknown causes in seven, and primary biliary cirrhosis in one. There were 30 cases of urinary tract infection, 19 cases of pneumonia, 16 cases of biliary tract infection, 10 cases of cellulites, and five cases of bacteremia of unknown origin (Table 1). Renal dysfunction developed in 29 (36%) of the patients with liver cirrhosis who concurrently had a bacterial infection.
Table 1.
Baseline Characteristics of the 80 Patients with Bacterial Infection
HBV, hepatitis B virus; HCV, hepatitis C virus; PBC, primary biliary cirrhosis; UTI, urinary tract infection.
*Mean years±SE. Other data are number (%) of patients.
2. Risk factors for developing renal dysfunction
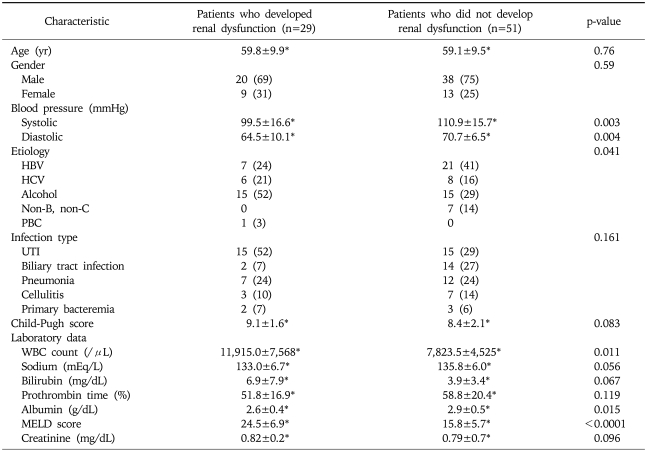
The clinical characteristics of the 29 patients who had renal dysfunction occurred after diagnosis of bacterial infection and the 51 patients who did not had renal dysfunction were comparatively evaluated. The mean age was 59.8±9.9 years in patients with renal dysfunction and 59.1±9.5 years in patients without renal dysfunction. There were no significant differences in gender, Child-Pugh score, or type of bacterial infection between the two groups. However, systolic and diastolic pressures were 99.5±16.6 mmHg and 64.5±10.1 mmHg, respectively, in 29 patients who had renal dysfunction developed and 110.9±15.7 mmHg and 70.7±6.5 mmHg, respectively, in 51 patients who did not have renal dysfunction (p<0.01). Renal dysfunction was more prevalent in patients with alcoholic liver disease (Table 2).
Table 2.
Comparison of Characteristics of Groups according to Development of Renal Dysfunction
HBV, hepatitis B virus; HCV, hepatitis C virus; PBC, primary biliary cirrhosis; UTI, urinary tract infection; MELD, Model for End-Stage Liver Disease.
*Mean±SE. Other data are number (%) of patients.
There was no significant difference in serum sodium, serum bilirubin, serum creatinine, or prothrombin time during the course of bacterial infection between the two groups. However, in patients with renal dysfunction, the WBC count (11,915/µL) and MELD score (24.5) were significantly higher than those in patients without renal dysfunction (p=0.011 and p<0.0001, respectively). The albumin level also differed significantly between the groups (p=0.015) (Table 2).
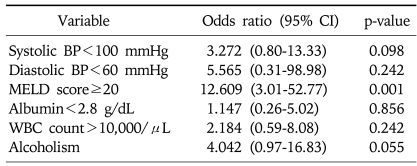
A multiple logistic regression analysis was performed on systolic and diastolic pressures, presence of alcoholic liver disease, WBC count, albumin level, and MELD score, which were all significant in the univariate analysis. The MELD score was significantly associated with the occurrence of renal dysfunction resulting from bacterial infection. The incidence of renal dysfunction in cases with a MELD score >20 was 12.6 times the incidence in the other cases (OR, 12.609; 95% confidence interval, 3.01-52.77, p=0.001) (Table 3).
Table 3.
Multiple Logistic Regression Analysis for the Variables Affecting Renal Dysfunction Development after Bacterial Infection
CI, confidence interval; BP, blood pressure; MELD, Model for End-Stage Liver Disease; WBC, white blood cell.
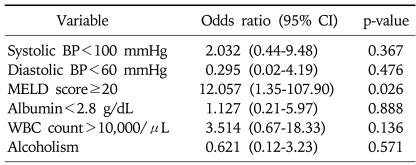
3. Incidence, risk factors, and prognosis of irreversible renal dysfunction
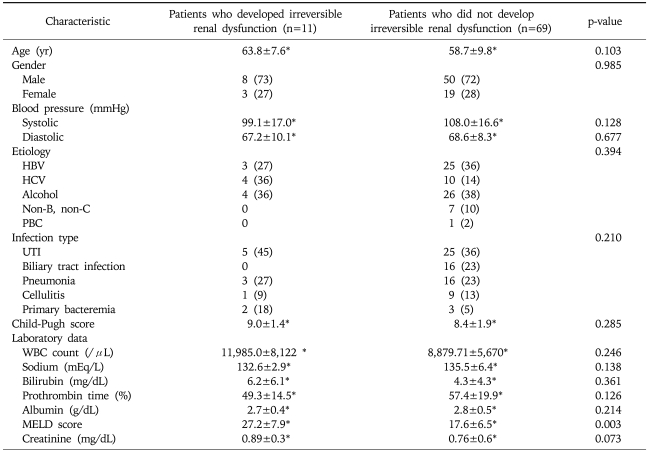
Irreversible renal dysfunction occurred in 11 patients, representing 14% of the total number of patients and 38% of those who had renal dysfunction. When cases with reversible and irreversible renal dysfunction were compared, there were no statistically significant differences in variables including MELD score. However, when patients with irreversible renal dysfunction were compared with those without irreversible renal dysfunction (reversible renal dysfunction and no renal dysfunction), the MELD score showed significant difference (p=0.003) (Table 4). This was in agreement with the results of the multivariate analysis in which only the MELD score was a significant risk factor for developing renal dysfunction (p=0.026) (Table 5).
Table 4.
Comparison of Characteristics of Groups according to Development of Irreversible Renal Dysfunction
HBV, hepatitis B virus; HCV, hepatitis C virus; PBC, primary biliary cirrhosis; UTI, urinary tract infection; MELD, Model for End-Stage Liver Disease.
*Mean±SE. Other data are number (%) of patients.
Table 5.
Multiple Logistic Regression Analysis for the Variables Affecting Irreversible Renal Dysfunction after Bacterial Infection
CI, confidence interval; BP, blood pressure; MELD, Model for End-Stage Liver Disease; WBC, white blood cell.
Of the 80 patients with bacterial infection, seven patients, all of whom had irreversible renal dysfunction occurred, died during the hospitalization. There were no significant differences in clinical characteristics and blood test results between patients who died and those who did not; only the MELD score was significantly different between the two groups (p=0.004).
DISCUSSION
Bacterial infection is one of the most common complications in patients with liver cirrhosis, and mortality has been higher.1-4 Urinary tract infection, pneumonia, and SBP are bacterial infections commonly seen in patients with liver cirrhosis.5-8
Studies concerning bacterial infection in patients with liver cirrhosis have focused mainly on those with SBP. Renal dysfunction is concurrently present in approximately one-third of SBP cases and is one of the most powerful indicators predicting death during the hospitalization.9 In patients with liver cirrhosis accompanied by ascites, there is a concurrent presence of circulatory dysfunction characterized by arterial dilatation, hypotension, increased cardiac output, and decreased effective circulating volume. In patients with liver cirrhosis and concurrent SBP, cytokine (TNF-alpha and IL-6) and nitric oxide levels are elevated, resulting in the dilatation of blood vessels and decreased renal blood flow. The deterioration of compensatory mechanisms leads to renal dysfunction.9,13 It is well known that albumin infusion can prevent renal dysfunction and enhance survival in patients with liver cirrhosis and concurrent SBP.10,14 In all types of bacterial infection, the increased release of inflammatory cytokines and vasodilatory substances can lead to renal dysfunction and circulatory dysfunction.
According to a recent study, there was a concurrent presence of bacterial infection, including SBP, in 44.6% of hospitalized patients with liver cirrhosis and ascites. Of these, 33.6% had renal dysfunction.15 Other studies have reported renal dysfunction in 26% of patients who concurrently had a bacterial infection other than SBP.16 In our series, in which SBP was excluded, renal dysfunction occurred in 36% of all patients, which is close to the incidence of renal dysfunction previously reported in patients with liver cirrhosis and bacterial infection include SBP.
In our study, type of bacterial infection were similar to the recent studies,5-8 urinary tract infection was the most common, followed by pneumonia and biliary tract infection. In a recent study, renal dysfunction reportedly occurred more frequently in patients with biliary tract infection,15 however, we found no significant difference in the occurrence of renal dysfunction based on the type of infection.
The improvement in infection is well-known independent risk factors for developing renal dysfunction in patients with liver cirrhosis who concurrently have a bacterial infection.14 The MELD score is the best prognostic marker of patients with cirrhosis and sepsis.16 Other study which have examined renal dysfunction after SBP, reported that blood urea nitrogen, serum sodium concentration before peritonitis and band neutrophils count in blood at diagnosis were independent predictors for the development renal dysfunction.9 In the present study, the only risk factor identified for developing renal dysfunction was the MELD score, indicating that severe hepatic dysfunction is a risk factor for developing renal dysfunction in patients with liver cirrhosis and bacterial infection. Patients with liver cirrhosis in whom renal dysfunction occurred due to bacterial infections other than SBP had a poor prognosis; the hospitalization mortality rate is 42.8% (7.24% in cases without renal dysfunction),15 and the 3-month mortality is 66% (13% in cases without renal dysfunction).16 Particularly in cases with irreversible renal dysfunction, the 3-month mortality may reach 100%. In our series, the hospitalization mortality was 24% in patients who developed renal dysfunction, and all those who died during the hospitalization had developed irreversible renal dysfunction. The MELD score was a factor for predicting hospitalization death.
In summary, renal dysfunction occurred in 36% of patients with liver cirrhosis who developed a bacterial infection other than SBP. The MELD score was the only factor that independently predicted the occurrence of renal dysfunction. Patients with liver cirrhosis who concurrently had a bacterial infection and renal dysfunction had a poor prognosis. In particular, the prognosis was poor for those with irreversible renal dysfunction.
There were several limitations to the current study. This was retrospective in design and lacked data about the use of plasma expanders. Further studies are warranted to examine whether albumin treatment can prevent the occurrence of renal dysfunction and enhance survival in patients with bacterial infections other than SBP.
ACKNOWLEDGEMENTS
This work was supported by 2008 Inje University Research Grant.
References
- 1.Navasa M, Rodes J. Bacterial infections in cirrhosis. Liver Int. 2004;24:277–280. doi: 10.1111/j.1478-3231.2004.0934.x. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001;120:726–748. doi: 10.1053/gast.2001.22580. [DOI] [PubMed] [Google Scholar]
- 3.Bolognesi M, Merkel C, Bianco S, et al. Clinical significance of the evaluation of hepatic reticuloendothelial removal capacity in patients with cirrhosis. Hepatology. 1994;19:628–634. doi: 10.1002/hep.1840190313. [DOI] [PubMed] [Google Scholar]
- 4.Deschenes M, Villeneuve JP. Risk factors for the development of bacterial infections in hospitalized patients with cirrhosis. Am J Gastroenterol. 1999;94:2193–2197. doi: 10.1111/j.1572-0241.1999.01293.x. [DOI] [PubMed] [Google Scholar]
- 5.Borzio M, Salerno F, Piantoni L, et al. Bacterial infection in patients with advanced cirrhosis: a multicentre prospective study. Dig Liver Dis. 2001;33:41–48. doi: 10.1016/s1590-8658(01)80134-1. [DOI] [PubMed] [Google Scholar]
- 6.Caly WR, Strauss E. A prospective study of bacterial infections in patients with cirrhosis. J Hepatol. 1993;18:353–358. doi: 10.1016/s0168-8278(05)80280-6. [DOI] [PubMed] [Google Scholar]
- 7.Rosa H, Silverio AO, Perini RF, Arruda CB. Bacterial infection in cirrhotic patients and its relationship with alcohol. Am J Gastroenterol. 2000;95:1290–1293. doi: 10.1111/j.1572-0241.2000.02026.x. [DOI] [PubMed] [Google Scholar]
- 8.Yang YY, Lin HC. Bacterial infections in patients with cirrhosis. J Chin Med Assoc. 2005;68:447–451. doi: 10.1016/S1726-4901(09)70072-3. [DOI] [PubMed] [Google Scholar]
- 9.Follo A, Llovet JM, Navasa M, et al. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: incidence, clinical course, predictive factors and prognosis. Hepatology. 1994;20:1495–1501. doi: 10.1002/hep.1840200619. [DOI] [PubMed] [Google Scholar]
- 10.Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403–409. doi: 10.1056/NEJM199908053410603. [DOI] [PubMed] [Google Scholar]
- 11.Angeli P, Guarda S, Fasolato S, et al. Switch therapy with ciprofloxacin vs. intravenous ceftazidime in the treatment of spontaneous bacterial peritonitis in patients with cirrhosis: similar efficacy at lower cost. Aliment Pharmacol Ther. 2006;23:75–84. doi: 10.1111/j.1365-2036.2006.02706.x. [DOI] [PubMed] [Google Scholar]
- 12.Augoustides JG, Pochettino A, Ochroch EA, et al. Renal dysfunction after thoracic aortic surgery requiring deep hypothermic circulatory arrest: definition, incidence, and clinical predictors. J Cardiothorac Vasc Anesth. 2006;20:673–677. doi: 10.1053/j.jvca.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 13.Navasa M, Follo A, Filella X, et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology. 1998;27:1227–1232. doi: 10.1002/hep.510270507. [DOI] [PubMed] [Google Scholar]
- 14.Tandon P, Garcia-Tsao G. Bacterial infections, sepsis, and multiorgan failure in cirrhosis. Semin Liver Dis. 2008;28:26–42. doi: 10.1055/s-2008-1040319. [DOI] [PubMed] [Google Scholar]
- 15.Fasolato S, Angeli P, Dallagnese L, et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology. 2007;45:223–229. doi: 10.1002/hep.21443. [DOI] [PubMed] [Google Scholar]
- 16.Terra C, Guevara M, Torre A, et al. Renal failure in patients with cirrhosis and sepsis unrelated to spontaneous bacterial peritonitis: value of MELD score. Gastroenterology. 2005;129:1944–1953. doi: 10.1053/j.gastro.2005.09.024. [DOI] [PubMed] [Google Scholar]