Abstract
Purpose
Combined coronary artery bypass (CAB) and valve surgery is one of the most challenging surgical procedures, but the operative results have improved over the years.
Materials and Methods
From 1989 through 2004, combined CAB and valve operations were performed in 125 patients. Mean age was 63 years, and 86 patients were male. Forty-six patients were diagnosed with coronary artery disease during preoperative evaluation for valvular heart disease (VHD). All patients underwent CAB, and one or more underwent valve replacement or repair (mitral: 54, aortic: 61, tricuspid: 3, DVR: 7) simultaneously.
Results
Mean number of distal graft was 1.98 ± 1.07, and LIMA was used in 68% of patients. Early mortality occurred in 6 patients (4.8%), and the causes were heart failure (4) and sepsis (2). Mean follow-up duration was 91.4 ± 40.9 months (range: 47-245), and late mortality occurred in 4 patients. Kaplan Meier estimated survival rates at 1, 5, and 10 years were 94.4%, 92.3%, and 89.9%, respectively.
Conclusion
Combined coronary and valve operations can be performed safely with optimal surgical results. Although the surgical mortality of coexisting coronary and VHD is higher than either isolated coronary or valvular operations, it may not affect the long-term survival.
Keywords: Coronary artery disease, coronary artery bypass, valvular diseases
INTRODUCTION
Recently, a considerable percentage of patients with valvular heart disease also have coronary artery disease requiring coronary revascularization during valvular operation, due to the increasing number of elderly patients in the general population, the improving safety of coronary artery bypass grafting (CABG), the increasing incidence of coronary artery disease, and the higher mortality rate after acute myocardial infarction, an incidence of which may be reduced by CABG.1 Combined valvular heart surgery and CABG had a substantially higher hospital mortality than those having either procedure alone, which ranged from 7% to 18%.2-9 Since there have not been many reports about this issue, we reviewed the clinical results of our 15-year experience of combined valvular heart operations and coronary revascularization to evaluate the clinical results, and to determine if co-existing coronary artery disease affected long-term survival.
MATERIALS AND METHODS
Patients' characteristics
From January 1989 through December 2004, 125 patients underwent valvular surgery combined with coronary artery bypass grafting at the Yonsei Cardiovascular Center, Yonsei University College of Medicine. Mean age of the patients was 63 ± 8.9 (range: 35-78) years, and 86 patients (69%) were male. Mean ages were 64.7 ± 7.9 (range: 43-78) years in patients with aortic valve disease, and 60.4 ± 9.7 (range, 35-75) years in patients with mitral valve disease. Preoperative clinical diagnosis for coronary artery disease included acute myocardial infarction (MI) in 6 patients, unstable angina in 23 patients, stable angina in 34 patients, previous MI in 16 patients, and 46 patients (37%) were diagnosed during preoperative evaluation for valvular heart disease (VHD). Aortic valve disease was present in 61 patients, mitral valve disease in 45 patients, tricuspid valve disease in 3 patients, and multiple valve disease in 16 patients. Among the sixty-one patients with aortic valve disease, 52 patients (85%) had severe calcification on the aortic valve. The etiologies of VHD included rheumatic in 37 patients, degenerative in 52 patients, congenital in 5 patients, chordae rupture or elongation without regional wall motion abnormality or tethering in 29 patients, and infective in 2 patients. VHDs of ischemic origin were excluded from this study.
Extent and location of valvular disease was determined by echocardiography, and preoperative coronary arteriography was performed in all patients over the age of 40 years to assess the extent of coronary artery disease. For patients under 40 years old, only those who had ischemic symptoms such as typical chest pain or evidence of ischemia on preoperative electrocardiogram underwent coronary angiography. A 60 percent reduction or greater in luminal diameter of a major coronary artery was considered significant disease and an indication for bypass grafting. On this basis, 48 patients had single vessel involvement, 31 patients had double vessel involvement, 36 patients had triple vessel involvement, and 10 patients had left main disease.
Surgical procedures
In all cases, combined valve operation and coronary revascularization was performed under conventional cardiopulmonary bypass technique in moderate hypothermia (32-34℃). Either antegrade or both antegrade and retrograde cold blood was administered to elicit cardioplegic arrest, and the distal anastomoses of saphenous vein grafts were carried out first, using a monofilament suture with a continuous running suture technique followed by valve repair or replacement. In cases of using left internal mammary artery (LIMA), the anastomosis of LIMA was carried out after the valve replacement. Mitral valve repair was performed in 28 patients, mostly carried out by annuloplasty using a Carpentier ring (n = 13) or Duran ring (n = 14), or a Kay plasty of the commissures (n = 1) with or without additional complicated reconstructions of valve leaflets or chordae tendinae. In cases of mitral valve replacement, subvalvular apparatus of the mitral valve was preserved to reduce the negative effect of mitral replacement in ventricular geometry and function.
Definitions
The number of diseased vessels was defined as the number of the three major coronary perfusion territories affected. The Canadian Cardiovascular Society (CCS) Classification was used to define the severity of angina and the New York Heart Association (NYHA) criteria to define severity of congestive heart failure. The patients were considered to have neurologic complication when there was a change in the brain verified by computed tomography to symptoms clinically suspected to be of neurologic origin. Perioperative myocardial injury was considered when there were EKG changes compatible with myocardial injury accompanied with either elevated cardiac enzyme or wall motion abnormality observed on the echocardiography. Hospital death was defined as mortality that occurred within 30 days after the operation or during the hospitalization. A cardiac event was defined as recurrent symptoms of angina or dyspnea, myocardial infarction, or congestive heart failure that required hospitalization more than once during the follow-up period.
Statistical analysis
All data was retrospectively collected and statistical data along with values of continuous variables in the text and tables were expressed as a mean ± standard deviation. A comparison of means was conducted using Student's t-test. Survival curves were constructed using the Kaplan-Meier method. Logistic regression analysis helped to examine the relationship between potential risk factors and in-hospital mortality. A p value of < 0.05 was considered to be statistically significant. The statistical package used was SPSS version 11 (version 11 SPSS, Inc., Chicago, IL, USA).
RESULTS
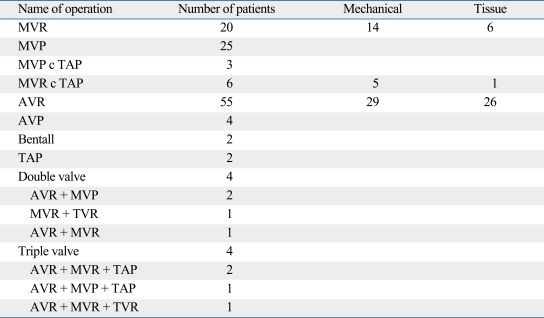
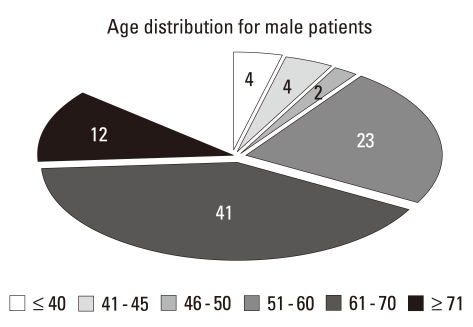
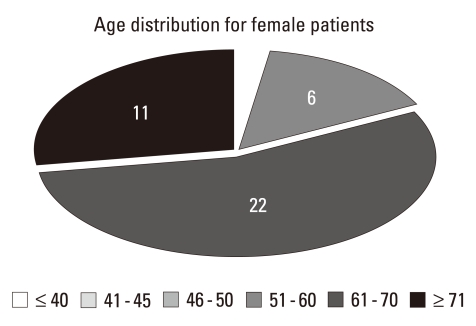
Among 125 patients, 6 patients had previous open-heart operations (2 had previous CABG, 1 had MVR, 1 had mitral valvuloplasty, and 2 had ASD patch repair). Among the patients who had mitral valve surgery, 19 received a mechanical prosthesis, 7 received a biological prosthesis, and 28 had a mitral valve repair. Among the patients who had aortic valve surgery, 29 received a mechanical prosthesis, 26 received a biological prosthesis, 4 had an aortic valve repair, and 2 had a Bentall procedure. Valvular operations performed are described in Table 1. Preoperative mean left ventricular ejection fraction was 56.9% and 74% of patients were NYHA functional class III or IV. The distributions of coronary artery disease according to the age and sex are shown in Figs. 1 and 2.
Table 1.
Valvular Operations Performed
MVR, mitral valve replacement; MVP, mitral valve repair; TAP, tricuspid annuloplasty; AVR, aortic valve replacement; AVP, aortic valve repair; TVR, tricuspid valve replacement.
Fig. 1.
Age distribution of coronary artery disease in male patients.
Fig. 2.
Age distribution of coronary artery disease in female patients.
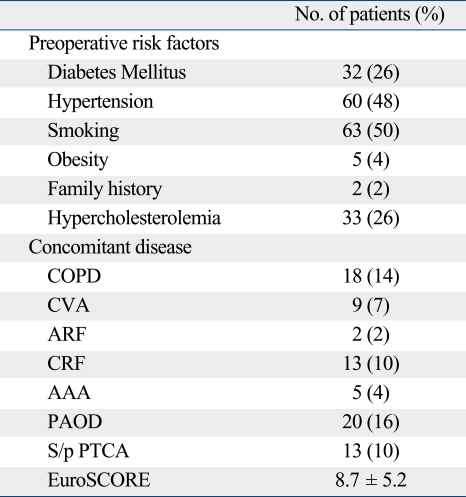
Preoperative risk factors for coronary artery disease included diabetes mellitus in 32 patients, hypertension in 60 patients, smoking in 63 patients, obesity in 5 patients, family history of coronary artery disease in 2 patients, and hypercholesterolemia in 33 patients (Table 2). Seventy-five percent of patients had a Canadian Class III or IV chest pain. Coronary revascularization was performed in all patients with a mean of 2.0 distal grafts/patient. Left internal mammary artery (IMA) was used in 84 patients (67%), right IMA in 2 patients, and bilateral IMA in 1 patient. Intraoperative data are described in Table 3.
Table 2.
Preoperative Risk Factors for Coronary Artery Disease and Concomitant Disease
COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; ARF, acute renal failure; CRF, chronic renal failure; AAA, abdominal aortic aneurysm; PAOD, peripheral artery occlusive disease; PTCA, percutaneous transluminal coronary angioplasty.
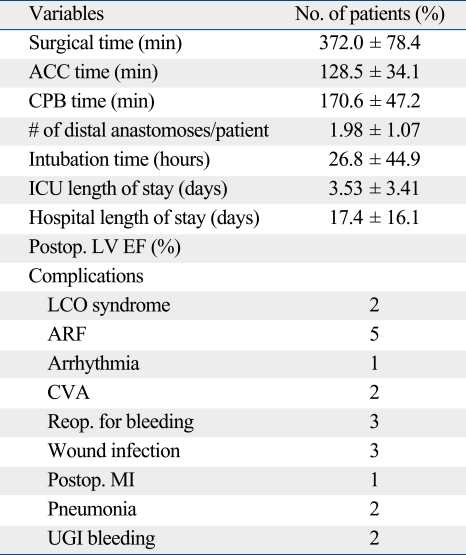
Table 3.
Intraoperative and Postoperative Data
ACC, aortic cross clamping; CPB, cardiopulmonary bypass; ICU, intensive care unit; Postop., postoperative; LVEF, left ventricular ejection fraction; LCO, low cardiac output; ARF, acute renal failure; Reop., reoperation; MI, myocardial infarction; UGI, upper gastrointestinal.
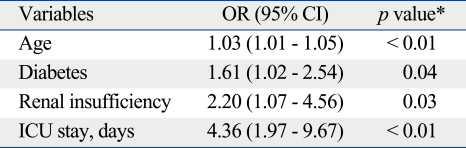
The overall hospital mortality was 4.8% (6/125 patients). The causes of early death were low cardiac output due to left ventricular failure in 4 patients and septic multi-organ failure in 2 patients. Postoperative complications included CVA in 2 patients, ARF requiring dialysis in 5 patients, reexploration for bleeding in 3 patients, IABP insertion due to low cardiac output in 2 patients, wound infection in 3 patients, pneumonia in 2 patients, and perioperative MI in 1 patient. Postoperative LV EF increased from 56.9 ± 14.2 to 58.6 ± 11.07% without statistical significance (p = 0.09). Postoperative Canadian (2.33 ± 0.85 to 1.13 ± 0.45, p < 0.05) and NYHA functional class (2.84 ± 0.60 to 1.29 ± 0.57, p < 0.001) improved significantly. The mean follow-up duration was 91.4 ± 40.9 months (range: 47-245 months), and late mortality occurred in 4 patients during the follow-up period. The causes of late deaths were cardiac related in one patient (sudden death) and non-cardiac related in 3 patients (CVA, malignancy, and sepsis). Two patients required a reoperation during the follow-up period, and the causes of reoperations were residual severe aortic regurgitation 19 months after aortic valvuloplasty in one patient and paravalvular leakage of the previous mechanical prosthesis after 86 months of mechanical prosthetic valve implantation in mitral position in the other patient. Three patients developed CVA and 3 patients developed lung cancer. Among the three patients who developed lung cancer, 1 patient died and 2 patients are currently undergoing chemotherapy. Six patients were readmitted for cardiac related problems (recurred angina in 3 patients, congestive heart failure in 1 patient, and arrhythmia in 2 patients). In all three patients with recurred angina, a follow-up coronary angiogram showed patent grafts with progression of native coronary artery disease that was successfully treated with medication. Independent predictors of in-hospital death were age, presence of diabetes, preoperative renal insufficiency, and prolonged ICU stay (Table 4). Kaplan-Meier estimated survival rates at 1, 5, and 10 years were 94.4%, 92.3%, and 89.9%, respectively, and freedom from MACE (major cardiovascular event) rates at 1, 5, and 10 years were 93.6%, 89.7%, and 76.4%, respectively.
Table 4.
Logistic Regression Model to Predict the In-Hospital Mortality
OR, odd ratio; CI, confidence interval; ICU, intensive care unit.
*only significant variables (p < 0.05) are listed.
DISCUSSION
The combined valvular and coronary artery disease is increasing, and the increasing numbers of patients suffering from such coexisting diseases have been offered cardiac surgery. The most important reason for this is the aging of the population of patients being candidates for CABG.4,10 In addition, the operative therapy of patients with combined valvular and coronary artery disease has evolved significantly since the early 1970s when the first cases were performed and routine coronary angiography was advocated for all patients with valve disease.
Approximately 8 percent of patients undergoing cardiac surgery have combined valvular and coronary artery disease worldwide.11,12 Even though ischemic symptoms such as angina are important indicators of coronary artery disease, angina is a less specific indicator of coronary artery disease in patients with valvular heart disease than in the general population. Because ischemic symptoms in patients with valvular heart disease may have other causes such as left ventricular chamber enlargement, increased wall stress, or wall thickening with subendocardial ischemia and right ventricular hypertrophy.
Currently, ACC/AHA practice guidelines recommend coronary angiography for preoperative evaluation in patients with anginal symptoms, other objective evidence of ischemia, decreased LV systolic function, history of coronary artery disease, or coronary risk factors. In asymptomatic patients, coronary angiography is recommended in men older than 45 years and women older than 55 years.13 Since 1980, our institute adopted a policy of obtaining coronary arteriography before valvular operations in patients over the age of 40 in men and 45 in women, and of performing CABG and valvular repair or replacement at the same time. In this study, no patient less than 50 years old had combined coronary artery disease in women; however, in male patients, 12% (10/86) of patients were less than 50 years old, and 4 patients were in their 30s. The prevalence of premature coronary disease was reported to be 2-11% of all hospitalized myocardial infarcts described in the literature.14-18 And in the most recent series, an increase of incidence, probably due to earlier exposure to some risk factors, such as smoking habit, hyperlipidemia, and stress as a result of rapid changing of diet habits, and life-styles which facilitate development of coronary artery disease in young patients, have been reported.16-18 Therefore, a coronary angiography should be considered even in younger patients with risk factors, especially for men and postmenopausal women. In addition, less expensive and noninvasive diagnostic tools such as multi-detector-row helical computed tomography (MDCT), a simple, useful, and accurate method to evaluate concomitant coronary artery disease, might be a good alternative in these patients, if appropriately selected.19,20
In this study, we excluded the patients with ischemic MR since that is thought to be a different disease entity, which results in higher mortality. In patients with ischemic MR, the diseases of the coronary artery and valve are not combined; rather the valvular heart disease is the result from the coronary artery disease. Therefore, the result of valvular heart surgery regardless of the type of surgery is often affected by the extent or the surgical results of the coronary artery disease.
During the study period of fifteen years, 4,276 valvular and 4,457 coronary operations were performed in our institute, and only 1.4% of the patients underwent combined coronary and valvular operations, which is less than other reported series.11,12 The exact reason was not known; however, we speculated that it may be because the percutaneous coronary intervention (PCI) ratio to coronary artery surgery is higher in our institute, almost 10 to 1, and primary or secondary PCI might have been tried before or after the valve operations in some patients with high risks. Also the cardiologists might have been reluctant to recommend surgery in these patients because of the high expected mortality and morbidity especially during 1980s and early 1990s. For example, about 40% of patients with symptomatic severe aortic stenosis older than 65 years were never referred to surgery during the same period. However, the referring rates in these patients are increasing, and even though the mortality rate was still higher than the isolated procedures, this study showed that the clinical results in these patients were promising with satisfactory long-term survival.
In this study, the early mortality of the patient was higher than the patients with isolated valvular or coronary artery disease, respectively. However, the early surgical results have been improving since 2000 as a result of improvement of surgical technique, better understanding of myocardial protection, and postoperative management. Among 125 patients, 56 patients (45%) were operated on after the year 2000, and only 1 of these patients died in the immediate postoperative period (1.8%), which was reduced from 7.2% (5/69) of mortality rate before 2000. In addition, the long-term mortality for isolated valvular heart and coronary artery disease were reported to be 78-92%21-23 and 48-95%24-26 at 10 years, which meant that the long term survival for concomitant coronary and valve operation is comparable to those of isolated coronary or valvular operations. Therefore, surgical management should be considered for the primary treatment in patients with a coexisting coronary artery and valvular heart disease.
Study limitations
Since this was a retrospective study, it suffers from the potential limitations of any retrospective analysis. Also, although the results showed comparable mortality and morbidity with other reported series, our study excluded patients with ischemic MR, which might have resulted in a higher mortality and morbidity.
In conclusion, combined coronary and valve operations can be performed safely with optimal surgical results. Even though the surgical mortality of coexisting coronary and valve disease is higher than either isolated coronary or valvular operations, it does not affect the long-term survival. Since the prevalence of premature coronary disease is increasing, coronary angiography should be considered regardless of age or sex in patients with risk factors for possible concomitant coronary artery disorders.
ACKNOWLEDGEMENTS
This study was supported by Yonsei University Research Fund of 2007.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.He GW, Grunkemeier GL, Starr A. Aortic valve replacement in elderly patients: Influence of concomitant coronary grafting on late survival. Ann Thorac Surg. 1996;61:1746–1751. doi: 10.1016/0003-4975(96)00143-9. [DOI] [PubMed] [Google Scholar]
- 2.DiSesa VJ, Cohn LH, Collins JJ, Jr, Koster JK, Jr, VanDevanter S. Determinants of operative survival following combined mitral valve replacement and coronary revascularization. Ann Thorac Surg. 1982;34:482–489. doi: 10.1016/s0003-4975(10)62992-x. [DOI] [PubMed] [Google Scholar]
- 3.Czer LS, Gray RJ, DeRobertis MA, Bateman TM, Stewart ME, Chaux A, et al. Mitral valve replacement: impact of coronary artery disease and determinants of prognosis after revascularization. Circulation. 1984;70:I198–I207. [PubMed] [Google Scholar]
- 4.Lytle BW, Cosgrove DM, Gill CC, Stewart RW, Golding LA, Goormastic M, et al. Mitral valve replacement combined with myocardial revascularization: early and late results for 300 patients, 1970 to 1983. Circulation. 1985;71:1179–1190. doi: 10.1161/01.cir.71.6.1179. [DOI] [PubMed] [Google Scholar]
- 5.Kirklin JK, Naftel DC, Blackstone EH, Kirklin JW, Brown RC. Risk factors for mortality after primary combined valvular and coronary artery surgery. Circulation. 1989;79:I185–I190. [PubMed] [Google Scholar]
- 6.Ferguson TB, Jr, Dziuban SW, Jr, Edwards FH, Eiken MC, Shroyer AL, Pairolero PC, et al. The STS National Database: current changes and challenges for the new millennium. Committee to Establish a National Database in Candiothoracic Surgery, The Society of Thoracic Surgeons. Ann Thorac Surg. 2000;69:680–691. doi: 10.1016/s0003-4975(99)01538-6. [DOI] [PubMed] [Google Scholar]
- 7.Minale C, Messmer BJ. Combination of mitral and coronary artery surgery. J Cardiovasc Surg (Torino) 1986;27:480–487. [PubMed] [Google Scholar]
- 8.Ashraf SS, Shaukat N, Odom N, Keenan D, Grotte G. Early and late results following combined coronary bypass surgery and mitral valve replacement. Eur J Cardiothorac Surg. 1994;8:57–62. doi: 10.1016/1010-7940(94)90091-4. [DOI] [PubMed] [Google Scholar]
- 9.He GW, Hughes CF, McCaughan B, Thomson DS, Leckie BD, Yang CQ, et al. Mitral valve replacement combined with coronary artery operation: determinants of early and late results. Ann Thorac Surg. 1991;51:916–922. doi: 10.1016/0003-4975(91)91005-g. [DOI] [PubMed] [Google Scholar]
- 10.Herlitz J, Brandrup-Wognsen G, Caidahl K, Haglid M, Karlsson BW, Karlsson T, et al. Mortality and morbidity among patients who undergo combined valve and coronary artery bypass surgery: early and late results. Eur J Cardiothorac Surg. 1997;12:836–846. doi: 10.1016/s1010-7940(97)00278-9. [DOI] [PubMed] [Google Scholar]
- 11.National adult cardiac surgical database report, 2000-2001. The Society for Cardiothoracic Surgery in Great Britain and Ireland. 2002. Oct, http://www.scts.org/sections/audit/cardiac/index.html.
- 12.Karthik S, Srinivasan AK, Grayson AD, Jackson M, Sharpe DA, Keenan DJ, et al. Limitations of additive EuroSCORE for measuring risk stratified mortality in combined coronary and valve surgery. Eur J Cardiothorac Surg. 2004;26:318–322. doi: 10.1016/j.ejcts.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Jr, Faxon DP, Freed MD, et al. American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease); Society of Cardiovascular Anesthesiologists. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing Committee to Revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2006;48:e1–e148. doi: 10.1016/j.jacc.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107:254–261. doi: 10.1016/s0002-9343(99)00218-1. [DOI] [PubMed] [Google Scholar]
- 15.Zimmerman F, Cameron A, Fisher LD, Ng G. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry) J Am Coll Cardiol. 1995;26:654–661. doi: 10.1016/0735-1097(95)00254-2. [DOI] [PubMed] [Google Scholar]
- 16.Doughty M, Mehta R, Bruckman D, Das S, Karavite D, Tsai T, et al. Acute myocardial infarction in the young--The University of Michigan experience. Am Heart J. 2002;143:56–62. doi: 10.1067/mhj.2002.120300. [DOI] [PubMed] [Google Scholar]
- 17.Barbash GI, White HD, Modan M, Diaz R, Hampton JR, Heikkila J, et al. Acute myocardial infarction in the young--the role of smoking. The Investigators of the International Tissue Plasminogen Activator/Streptokinase Mortality Trial. Eur Heart J. 1995;16:313–316. [PubMed] [Google Scholar]
- 18.Fournier JA, Cabezón S, Cayuela A, Ballesteros SM, Cortacero JA, Díaz De La Llera LS. Long-term prognosis of patients having acute myocardial infarction when </=40 years of age. Am J Cardiol. 2004;94:989–992. doi: 10.1016/j.amjcard.2004.06.051. [DOI] [PubMed] [Google Scholar]
- 19.Ohnesorge BM, Hofmann LK, Flohr TG, Schoepf UJ. CT for imaging coronary artery disease: defining the paradigm for its application. Int J Cardiovasc Imaging. 2005;21:85–104. doi: 10.1007/s10554-004-5346-6. [DOI] [PubMed] [Google Scholar]
- 20.Yoo KJ, Choi D, Choi BW, Lim SH, Chang BC. The comparison of the graft patency after coronary artery bypass grafting using coronary angiography and multi-slice computed tomography. Eur J Cardiothorac Surg. 2003;24:86–91. doi: 10.1016/s1010-7940(03)00192-1. [DOI] [PubMed] [Google Scholar]
- 21.Emery RW, Erickson CA, Arom KV, Northrup WF, 3rd, Kersten TE, Von Rueden TJ, et al. Replacement of the aortic valve in patients under 50 years of age: long-term follow-up of the St. Jude Medical prosthesis. Ann Thorac Surg. 2003;75:1815–1819. doi: 10.1016/s0003-4975(03)00016-x. [DOI] [PubMed] [Google Scholar]
- 22.Berrebi AJ, Carpentier SM, Phan KP, Nguyen VP, Chauvaud SM, Carpentier A. Results of up to 9 years of high-temperature-fixed valvular bioprostheses in a young population. Ann Thorac Surg. 2001;71:S353–S355. doi: 10.1016/s0003-4975(01)02558-9. [DOI] [PubMed] [Google Scholar]
- 23.Ruel M, Kulik A, Lam BK, Rubens FD, Hendry PJ, Masters RG, et al. Long-term outcomes of valve replacement with modern prostheses in young adults. Eur J Cardiothorac Surg. 2005;27:425–433. doi: 10.1016/j.ejcts.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Gao G, Wu Y, Grunkemeier GL, Furnary AP, Starr A. Long-term survival of patients after coronary artery bypass graft surgery: comparison of the pre-stent and post-stent eras. Ann Thorac Surg. 2006;82:806–810. doi: 10.1016/j.athoracsur.2006.04.032. [DOI] [PubMed] [Google Scholar]
- 25.El-Hamamsy I, Cartier R, Demers P, Bouchard D, Pellerin M. Long-term results after systematic off-pump coronary artery bypass graft surgery in 1000 consecutive patients. Circulation. 2006;114:I486–I491. doi: 10.1161/CIRCULATIONAHA.105.001651. [DOI] [PubMed] [Google Scholar]
- 26.van Domburg RT, Kappetein AP, Bogers AJ. The clinical outcome after coronary bypass surgery: a 30-year follow-up study. Eur Heart J. 2009;30:453–458. doi: 10.1093/eurheartj/ehn530. [DOI] [PubMed] [Google Scholar]