Abstract
Twenty-four hours multichannel intraesophageal impedance and pH monitoring in a patient who suffered from recurrent hiccups for more than a year revealed frequent supragastric belching and pathological oesophageal acid exposure. Furthermore, a temporal relationship between the start of a hiccup episode and gastric belching was observed. The data support the hypothesis that there is an association between supragastric belching, persistent recurrent hiccups and gastro-oesophageal reflux disease, and that gastric belching may evoke hiccup attacks.
Keywords: Hiccup, Impedance and pH monitoring, Gastro-oesophageal reflux, Supragastric belching
INTRODUCTION
Hiccups are mostly a transient phenomenon that do not require medical attention. Prolonged hiccups are rare and can be indicative of a serious underlying disease process. Gastro-oesophageal reflux disease (GORD) has been associated with protracted hiccups[1-3]. Previous reports on functional disturbances of the oesophagus in patients with hiccups are sporadic and confined to conventional manometry and pH monitoring. Multichannel oesophageal impedance measurement is a recently developed technique that detects both liquid and gas transport in the oesophagus. In this report we present detailed results of 24 h intraesophageal impedance measurement and pH monitoring in a patient who suffered from persistent recurrent hiccups for more than a year. In addition, we had the unique opportunity to monitor intraluminal pressure and impedance signals of the oesophagus during the spontaneous onset of a hiccup attack.
CASE REPORT
A 74-year-old man suffered from chronic recurrent hiccups for more than 18 mo. Upper gastrointestinal endoscopy showed reflux oesophagitis grade A (Los Angeles classification). Proton pump inhibitor (PPI) therapy was successful for heartburn, but hiccups and belching persisted. Extensive clinical evaluation did not reveal other abnormalities that could explain the hiccups. Treatment with metoclopramide, baclofen and gabapentin did not relieve symptoms. During hiccup episodes, hicccups were continuous, lasted all day and were even present at night. Severe belching sometimes preceded the start of a hiccup attack. Hiccups were absent approximately 1 d per week.
24-h ambulatory impedance-pH monitoring
Electrical impedance was recorded at 3, 5, 7, 9, 15 and 17 cm and pH at 5 cm above the upper border of the lower oesophageal sphincter (LOS) with a transnasally positioned disposable catheter (reference code K6011-EI-0632 Unisensor AG, Attikon, Switzerland). A commercially available ambulatory system (Ohmega, MMS, Enschede, The Netherlands) was used for storage and subsequent analysis of data according to previously described criteria[4-7]. The study was performed once on and once off PPI therapy.
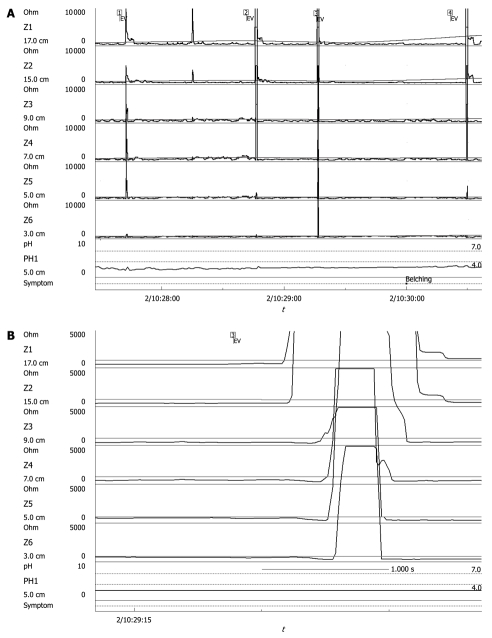
pH-metry off PPI revealed severely pathologic oesophageal acid exposure (Table 1). Basal impedance was below 1000 Ohm for more than 90% of the time at all measurement sites in the oesophagus, prohibiting reliable detection of swallow- or reflux-induced impedance drops. Impedance patterns consistent with “supragastric belches (SGBs)” were observed frequently[6]. These consisted of impedance increments exceeding 3000 Ohm with a rapid aboral propagation (velocity > 10 cm/s). These impedance peaks started in the proximal oesophagus and were followed by a retrograde return of impedance to baseline (Figure 1). A total of 188 SGBs were observed in our patient (Table 1). Based on these findings the patient was treated with PPI (20 mg rabeprazole twice daily) and referred for behavioral therapy in an attempt to reduce supragastric belching.
Table 1.
24 h ambulatory impedance-pH measurement
| Off PPI | On PPI | Normal | |
| % time pH < 4.0 | |||
| Total | 50 | 27 | < 4.0% |
| Upright | 45 | 10 | < 4.7% |
| Supine | 57 | 55 | < 2.0% |
| Supragastric belches | |||
| Total | 188 | 17 | Absent |
| Symptom episodes | |||
| Severe belching | 4 | - | |
| Heartburn | 5 | - | |
| % time with hiccup | > 60% | > 60% | Absent |
PPI: Proton pump inhibitor.
Figure 1.
Oesophageal intraluminal impedance monitoring combined with oesophageal pH measurements. A: Three minutes stretch of the tracings showing an abnormally low basal impedance with repetitive impedance peaks in all channels marked EV 1-4; B: Zoomed-in segment of the recording shows that an impedance peak (EV3) starts in the proximal channel, moves in the antegrade direction and is cleared in the retrograde direction. The horizontal bar represents 1.000 s. The patient reported severe belching at 10:30:00 during this period of repetitive supragastric belches (SGBs). Oesophageal pH is continuously below 4.
Twenty-four hours ambulatory impedance-pH monitoring on PPI 1 mo after behavioral therapy revealed a considerable reduction of SGBs by 90% (Table 1). The treatment by a speech therapist focused on teaching abdominal breathing and controlled swallowing to avoid influx of air. Oesophageal acid exposure was reduced (Table 1) and heartburn completely disappeared after PPI therapy. However, after 1 year follow-up, the patient reported only a minor and transient reduction of hiccups.
Oesophageal impedance measurement and perfusion manometry
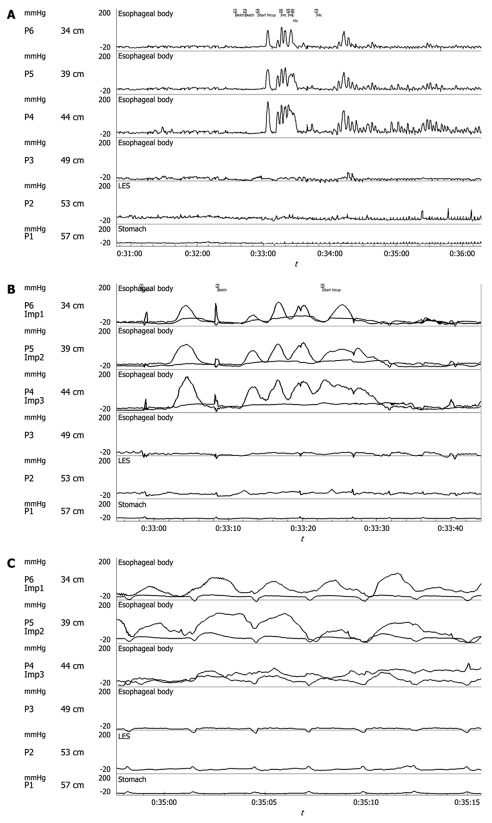
Stationary manometry and impedance measurements were performed with a perfused multi-lumen manometric and impedance assembly in combination with a sleeve sensor (reference code CE5-0010, Dentsleeve international, Mississauga, Ontario, Canada) connected to the Solar GI system (MMS) as described previously[8]. Intraesophageal pressures and impedance signals at 2, 7, 12 and 17 cm above the upper border of the LOS revealed ineffective oesophageal motility characterized by non-transmitted contractions with absence of pressure responses at 2 cm and in 3 out of 14 liquid swallows also at 17 cm. In 2 out of 14 swallows a simultaneous contraction was observed with mean amplitude > 30 mmHg. In addition, impedance tracings showed abnormal bolus transport as only 41% (normal ≥ 80%) of saline swallows were followed by normal transit. During these routine measurements hiccups were absent. Recording was continued for 3 h with the patient comfortably seated in a chair. After 20 min an episode of hiccups began. Approximately 20 s before the onset of the hiccups a sequence of gastric belching followed by simultaneous oesophageal contractions was observed (Figure 2).
Figure 2.
Combined impedance and perfusion manometry. A: Pressure tracings from 31-36 min during spontaneous onset of a hiccup attack at time 33:20 min; B: Combined impedance and manometry of a zoomed in segment of Figure 2A shows that the hiccup episodes are preceded by 2 gastric belches and high pressure simultaneous, repetitive contractions; C: Another zoomed in segment of Figure 2A shows that hiccups are accompanied by sharp positive pressure peaks in the lower oesophageal sphincter and stomach, and by negative peaks in the oesophagus. The upper border of the lower oesophageal sphincter (LOS) was located at 51 cm from the nostrils.
DISCUSSION
In our patient presenting with recurrent hiccups, excessive supragastric belching was found by 24-h impedance measurement. In addition, gastric belching and oesophageal spasms were observed by combined oesophageal impedance monitoring and manometry immediately preceding the onset of a hiccup attack.
The typical impedance pattern of SGBs was previously observed in patients with severe belching by Bredenoord et al[6]. It was attributed to rapid entrance of air into the oesophagus from proximal that was almost immediately expulsed. The pattern was clearly distinct from normal air swallowing in which a fall in impedance was associated with a more slowly propagated impedance peak and also from gas reflux or gastric belches in which the impedance peak started in the distal oesophagus and moved in a retrograde direction[4-6]. SGBs were not reported in healthy controls and in patients with functional dyspepsia[4-6]. In patients with GORD SGBs were found to occur more frequently, either as a putative trigger of reflux episodes or as a response to a perceived reflux episode[9].
The pathophysiology of hiccups is not clear. It has been suggested that sudden rapid distension of the proximal oesophagus by excessive food ingestion, carbonated beverages or aerophagia can trigger the hiccup reflex[10,11]. The present report provides evidence for an association between belching and hiccups. The observation that two gastric belches preceded the onset of a hiccup episode in our patient supports the hypothesis that rapid distension by oesophageal gas transport can trigger hiccups. Our patient also suffered from severe pathological acid reflux, ineffective oesophageal motility and impaired transit for liquid boluses. GORD was associated with protracted hiccups in previous case reports[1-3]. Disappearance of protracted hiccups after treatment with PPI in some patients suggests that reflux may precipitate hiccups[2]. However, persistence of hiccups after antireflux surgery in some reports[1,3] or treatment with PPI, as in our patient, suggests that other factors may be involved in patients with GORD.
In conclusion, in a patient with recurrent hiccups and GORD multichannel intraluminal impedance, pH and pressure measurements show (1) excessive supragastric belching and (2) a temporal relationship between the start of a hiccup episode and gastric belching.
Footnotes
Peer reviewer: Akio Inui, MD, PhD, Professor, Department of Behavioral Medicine, Kagoshima University Graduate School of Medical and Dental Sciences, 8-35-1 Sakuragaoka, Kagoshima 890-8520, Japan
S- Editor Tian L L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Shay SS, Myers RL, Johnson LF. Hiccups associated with reflux esophagitis. Gastroenterology. 1984;87:204–207. [PubMed] [Google Scholar]
- 2.Pooran N, Lee D, Sideridis K. Protracted hiccups due to severe erosive esophagitis: a case series. J Clin Gastroenterol. 2006;40:183–185. doi: 10.1097/00004836-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Marshall JB, Landreneau RJ, Beyer KL. Hiccups: esophageal manometric features and relationship to gastroesophageal reflux. Am J Gastroenterol. 1990;85:1172–1175. [PubMed] [Google Scholar]
- 4.Conchillo JM, Selimah M, Bredenoord AJ, Samsom M, Smout AJ. Air swallowing, belching, acid and non-acid reflux in patients with functional dyspepsia. Aliment Pharmacol Ther. 2007;25:965–971. doi: 10.1111/j.1365-2036.2007.03279.x. [DOI] [PubMed] [Google Scholar]
- 5.Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Air swallowing, belching, and reflux in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2006;101:1721–1726. doi: 10.1111/j.1572-0241.2006.00687.x. [DOI] [PubMed] [Google Scholar]
- 6.Bredenoord AJ, Weusten BL, Sifrim D, Timmer R, Smout AJ. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut. 2004;53:1561–1565. doi: 10.1136/gut.2004.042945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shay S, Tutuian R, Sifrim D, Vela M, Wise J, Balaji N, Zhang X, Adhami T, Murray J, Peters J, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–1043. doi: 10.1111/j.1572-0241.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 8.Conchillo JM, Nguyen NQ, Samsom M, Holloway RH, Smout AJ. Multichannel intraluminal impedance monitoring in the evaluation of patients with non-obstructive Dysphagia. Am J Gastroenterol. 2005;100:2624–2632. doi: 10.1111/j.1572-0241.2005.00303.x. [DOI] [PubMed] [Google Scholar]
- 9.Hemmink GJ, Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Supragastric belching in patients with reflux symptoms. Am J Gastroenterol. 2009;104:1992–1997. doi: 10.1038/ajg.2009.203. [DOI] [PubMed] [Google Scholar]
- 10.Lewis JH. Hiccups: causes and cures. J Clin Gastroenterol. 1985;7:539–552. doi: 10.1097/00004836-198512000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Fass R, Higa L, Kodner A, Mayer EA. Stimulus and site specific induction of hiccups in the oesophagus of normal subjects. Gut. 1997;41:590–593. doi: 10.1136/gut.41.5.590. [DOI] [PMC free article] [PubMed] [Google Scholar]