Abstract
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor in the alimentary tract. To the best of our knowledge, few cases have been reported in the literature about the peripheral lymph node metastasis of GIST. Here we report an unusual case of gastric GIST with inguinal lymph nodes metastasis. After the metastatic lymph nodes were resected, the. patient started to take imatinib 400 mg/d for 12 mo. There were no signs of tumor recurrence at follow-up after 29 mo. This case suggests that the inguinal lymph nodes can be a potential metastatic site of GIST.
Keywords: Gastrointestinal stromal tumor, Inguinal, Lymph node, Metastasis
INTRODUCTION
Gastrointestinal stromal tumor (GIST) is the most common gastrointestinal (GI) mesenchymal tumor, which accounts for 0.2% of all GI tumors and 80% of sarcomas[1]. GIST most commonly arises from the stomach and accounts for about 1% of gastric malignancies[2]. Liver and peritoneal metastatic lesions are often observed but lymph nodes metastasis is rarely found in GIST[3]. Moreover, there are few reports about the peripheral lymph nodes metastasis of GIST in literature. Here we report one interesting GIST case with inguinal lymph nodes metastases 3 years after distal gastrectomy and hepatolobectomy due to gastric GIST with liver metastasis.
CASE REPORT
A 60-year-old Chinese man came to the clinic on August 8th, 2007, complaining of his feeling of an inguinal mass gradually growing for 5 mo. He received distal gastrectomy, perigastric lymphadenectomy and hepatectomy in July 2004 for gastric GIST with liver metastasis. Physical examination revealed a 4 cm × 3 cm round and nontender mass which was located in the right inguinal region. Inguinal ultrasonography showed a low echo-level mass (Figure 1). Computed tomography (CT) revealed a 4 cm × 5 cm low density mass (CT value = 68.8 HU) which was unenhanced during contrast-enhanced scan (Figure 2). A complete gross excision of the mass was carried out for this patient on August 13, 2007. Grossly, the surgical specimen consisted of a 4.0 cm × 3.5 cm × 3.0 cm large, nodular, whitish-gray and firm lymph node. Microscopically, it was confluent and was infiltrated with spindle cells. These spindle cells were predominantly arranged in interweaving fascicles (Figure 3). Immunohistochemical stains demonstrated a strong positivity for both c-kit (CD117) and CD34 (Figure 4), which was consistent with the primary tumor. Gene sequence analysis showed that all the primary tumors, the metastatic tumor in liver and the resected inguinal lymph nodes harbored deletion mutations affecting codons 557/558 of exon 11 in the KIT. After the operation, the patient took imatinib 400 mg/d for 1 year. And there was no sign of tumor recurrence during 29 mo of follow-up.
Figure 1.

Ultrasonography. Inguinal ultrasonography shows a low echo-level lesion in the right inguinal region.
Figure 2.
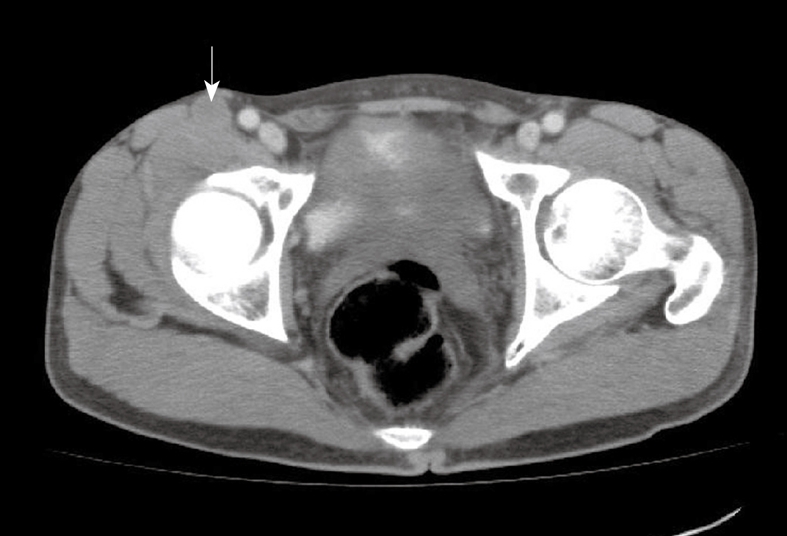
Computed tomography (CT). A low density lesion with weak, uneven enhancement during contrast-enhanced scan (arrow).
Figure 3.
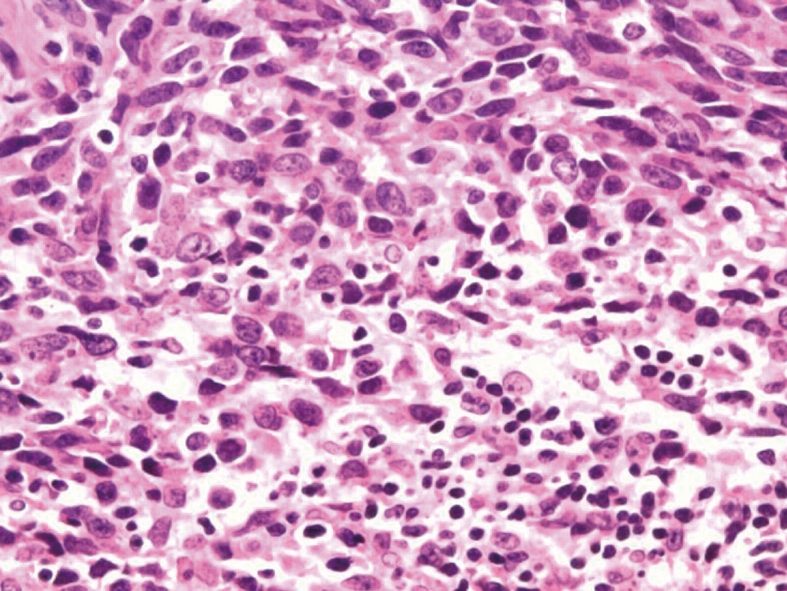
Hematoxylin & eosin (HE) staining. Spindle cells were predominantly arranged in interweaving fascicles (HE stain, × 100).
Figure 4.
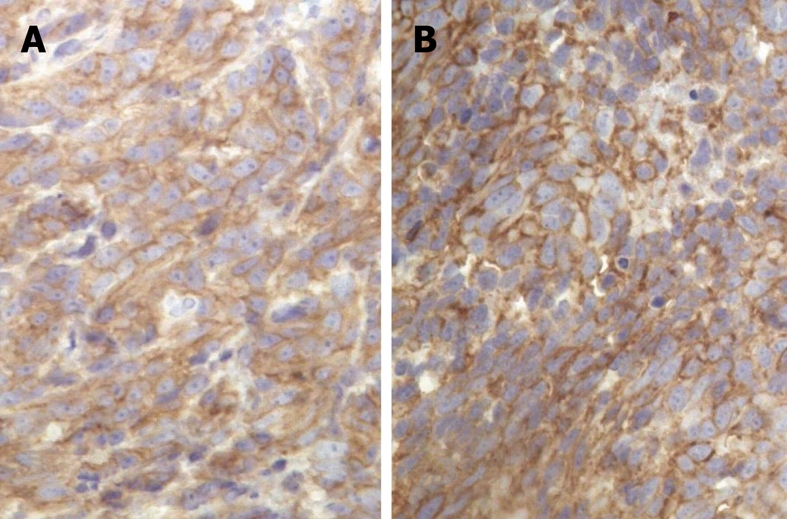
Immunohistochemical staining. A strong positivity for both CD117 (A) and CD34 (B) (CD117 stain, × 400, CD34 stain, × 400).
DISCUSSION
The case we reported herein is a high grade GIST according to the Bucher grading system[4]. Unlike gastric adenocarcinoma, regional lymph nodes including perigastric and mesenteric lymph nodes metastasis of GIST is unusual. The prevalence is reported to range from 1.1% to 3.4%[5-7]. In this case, perigastric lymphadenectomy was performed and no metastasis was observed in all of 19 lymph nodes at the first operation, although liver metastasis was detected.
To the best of our knowledge, this is the first reported case of GIST with inguinal lymph nodes metastasis. However, the distinct pattern of inguinal lymph node metastasis of gastric neoplasm is unclear. In the case of gastric adenocarcinoma, tumor cells can metastasize to para-aortic lymph nodes which have a chance of retrograde dissemination to the pelvic lymph nodes and also inguinal lymph nodes. It is unclear whether this metastatic mechanism is applicable for GIST with inguinal lymph nodes metastasis. In this case, since liver is the first organ of metastasis occurrence, we can hypothesize that when tumor cells invade the liver, they have a higher probability to spread into peripheral blood, and tumor cells can migrate into peripheral lymph node via high endothelial venule, which finally results in lymph nodes metastasis.
At present, surgery remains the mainstay of treatment in GIST patients with isolated resectable GIST. Imatinib is currently indicated for the first-line treatment of metastatic or unresectable KIT-positive GIST. The persistent use of imatinib was necessary for this patient after complete resection of primary gastric and hepatic metastatic GIST. Unfortunately, this patient did not take imatinib after his first operation which led to further metastasis. After his second operation, the patient started imatinib treatment and survived without recurrence till now.
In conclusion, GIST can involve the inguinal lymph nodes as a metastatic site and further studies are necessary to clarify the mechanism of this metastasis.
Footnotes
Peer reviewer: Bernabe Matias Quesada, MD, Department of Surgery, Hospital Cosme Argerich, Talcahuano 944 9°A, Buenos Aires 1013, Argentina
S- Editor Tian L L- Editor Ma JY E- Editor Lin YP
References
- 1.Blay JY, Bonvalot S, Casali P, Choi H, Debiec-Richter M, Dei Tos AP, Emile JF, Gronchi A, Hogendoorn PC, Joensuu H, et al. Consensus meeting for the management of gastrointestinal stromal tumors. Report of the GIST Consensus Conference of 20-21 March 2004, under the auspices of ESMO. Ann Oncol. 2005;16:566–578. doi: 10.1093/annonc/mdi127. [DOI] [PubMed] [Google Scholar]
- 2.Lehnert T. Gastrointestinal sarcoma (GIST)--a review of surgical management. Ann Chir Gynaecol. 1998;87:297–305. [PubMed] [Google Scholar]
- 3.Miettinen M, Furlong M, Sarlomo-Rikala M, Burke A, Sobin LH, Lasota J. Gastrointestinal stromal tumors, intramural leiomyomas, and leiomyosarcomas in the rectum and anus: a clinicopathologic, immunohistochemical, and molecular genetic study of 144 cases. Am J Surg Pathol. 2001;25:1121–1133. doi: 10.1097/00000478-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Bucher P, Egger JF, Gervaz P, Ris F, Weintraub D, Villiger P, Buhler LH, Morel P. An audit of surgical management of gastrointestinal stromal tumours (GIST) Eur J Surg Oncol. 2006;32:310–314. doi: 10.1016/j.ejso.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 5.Arber DA, Tamayo R, Weiss LM. Paraffin section detection of the c-kit gene product (CD117) in human tissues: value in the diagnosis of mast cell disorders. Hum Pathol. 1998;29:498–504. doi: 10.1016/s0046-8177(98)90066-1. [DOI] [PubMed] [Google Scholar]
- 6.Aparicio T, Boige V, Sabourin JC, Crenn P, Ducreux M, Le Cesne A, Bonvalot S. Prognostic factors after surgery of primary resectable gastrointestinal stromal tumours. Eur J Surg Oncol. 2004;30:1098–1103. doi: 10.1016/j.ejso.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 7.Tashiro T, Hasegawa T, Omatsu M, Sekine S, Shimoda T, Katai H. Gastrointestinal stromal tumour of the stomach showing lymph node metastases. Histopathology. 2005;47:438–439. doi: 10.1111/j.1365-2559.2005.02133.x. [DOI] [PubMed] [Google Scholar]


