ABSTRACT
The importance of quality of life (QOL) outcomes following treatments for head and neck tumors are now increasingly appreciated and measured to improve medical and surgical care for these patients. An understanding of the definitions in the setting of health care and the use of appropriate QOL instruments and measures are critical to obtain meaningful information that guides decision making in various aspects of patient health care. QOL outcomes following cranial base surgery is only recently being defined. In this article, we describe the current published data on QOL outcomes following cranial base surgery and provide preliminary prospective data on QOL outcomes and sinonasal morbidity in patients who underwent endonasal cranial base surgery for management of various skull base tumors at our institution. We used a disease-specific multidimensional instrument to measure QOL outcomes in these patients. Our results show that although sinonasal morbidity is increased, this is temporary, and the vast majority of patients have a very good QOL by 4 to 6 months after endonasal approach to the cranial base.
Keywords: Quality of life, skull base surgery, endoscopic approach
Cranial base lesions constitute a diverse group of diseases that are associated with a spectrum of morbidities. Therapeutic options may include surgery, radiotherapy, and medical treatment that can offer a favorable prognosis but may differ considerably in the quality of life (QOL) outcomes. Recent advances in the treatment of cranial base malignancies have had a major positive impact on the long-term survival of patients.1,2 However, the treatments and reconstruction methods may be associated with significant inherent morbidities that may negatively affect a patient's physical function and emotional well-being. Consequently, a patient's QOL associated with various treatment modalities and reconstruction strategies assumes greater importance. This is reflected by the numerous studies that have assessed QOL in patients treated for brain and head and neck cancer in the last decade.3,4,5,6,7,8
The development and growing utility of the expanded endonasal approach to the cranial base provides another option for the surgical treatment of skull base neoplasms. Although the oncological principle of total tumor extirpation confirmed by negative margins is still maintained, its impact on patients' QOL is not defined. An endonasal approach avoids some of the morbidity of a transcranial/transfacial approach and offers the potential of a faster recovery. However, it may have a unique set of morbidities associated with the endonasal corridor and nasoseptal flap reconstruction that affects QOL in a different way. This article reviews the current data on QOL outcomes following cranial base surgery and provides prospective data on QOL outcomes and sinonasal morbidity in patients who underwent endonasal cranial base surgery for management of skull base tumors.
MATERIALS AND METHODS
We examined the QOL outcomes using the anterior skull base questionnaire and the sinonasal outcome test (SNOT)-22 questionnaire in 51 patients and evaluated the clinical nasal morbidity in 109 patients undergoing the endonasal approach for a variety of skull base lesions at our institution, including transsellar, transplanum, transpterygoid, transcribriform, transclival, and multiple approaches (unpublished data). To our knowledge, there is no disease- and approach-specific instrument for assessing QOL following endonasal surgery of the skull base. Therefore, we used the multidimensional disease-specific questionnaire for anterior skull base neoplasms developed by Gil and associates to estimate the effect of the endonasal surgical approach for various cranial base lesions on patients' QOL.9 A higher score in the QOL questionnaire indicates a good outcome, with a minimum score of 1.0 and a maximum score of 5.0.
We also used the disease-specific validated SNOT-22 questionnaire that provides a symptom score (range 0 to 5.0) for parameters relating to sinonasal function in 51 patients who underwent the endonasal approach.10 A higher score indicates worse outcome.
RESULTS
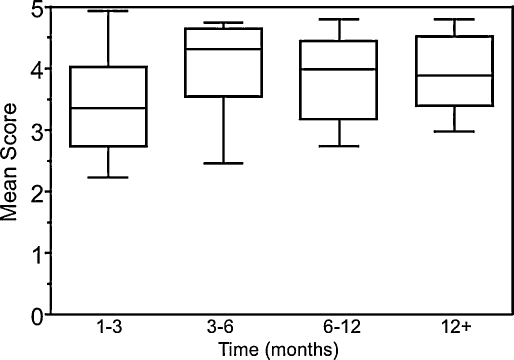
Fifty-one patients participated in the QOL study. Overall, patients had good (mean score of 3.0) to very good (mean score of 4.0) QOL scores following the endonasal approach. There was no statistically significant difference in the mean overall QOL score over the time periods. By 1 to 3 months after surgery, 75% of patients had a mean score of 4.0 or more for the overall QOL and for all domains except for those associated with emotion and specific symptoms. The overall mean QOL score over time is depicted in Fig. 1. By 3 to 6 months, 75% of patients had a mean score of 4.6 or more for the overall QOL and a mean score of 4.0 or more for domain-specific QOL. The overall and domain-specific QOL scores were significantly higher in patients undergoing primary surgery compared with those undergoing secondary operations and significantly higher in patients undergoing transsellar approach compared with those who underwent nontranssellar approaches. The overall QOL score across various time points was also significantly better in patients who did not have nasal septal flap reconstruction compared with those who did.
Figure 1.
Mean overall quality of life scores over time (1 to 3, 3 to 6, 6 to 12, and 12 months and beyond) for all patients undergoing endoscopic endonasal approach. Lower and upper limits of the boxes represent the 25th and 75th percentiles, respectively. The horizontal line represents the median and bars, the range.
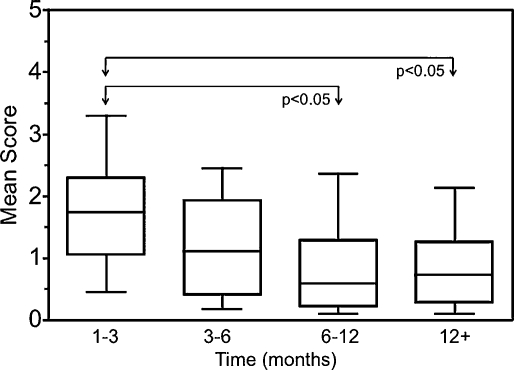
The disease-specific validated SNOT-22 questionnaire, which provides a symptom score (range 0 to 5.0) for parameters relating to sinonasal function, was used in 51 patients who underwent the endonasal approach. A higher score indicates worse outcome. There was a significant difference in the mean SNOT-22 scores over time (Fig. 2; p = 0.004, Kruskal-Wallis test). A statistically significant improvement in the mean score was observed between the periods 1 to 3 and 6 to 12 months and between 1 to 3 months and >12 months after surgery (p < 0.05, Kruskal-Wallis test with post hoc Dunn test). The best postoperative SNOT-22 score was achieved in more than 75% of patients by 6 to 12 months after surgery. The scores were significantly better in patients undergoing transsellar approach compared with those undergoing other approaches. The SNOT-22 scores were also significantly better in patients who did not have nasal septal flap reconstruction compared with those who did. The five most common items identified by patients that were considered to be the most important items affecting their health included loss of smell or taste, nasal obstruction, postnasal discharge, waking up at night, and lack of a good night's sleep. Overall, ~27% of patients scored 4.0 or greater indicating a severe problem relating to loss of smell or taste.
Figure 2.
SNOT-22 scores over time (1 to 3, 3 to 6, 6 to 12, and 12 months and beyond) for all patients undergoing expanded endonasal approach. The lower and upper limits of the boxes represent the 25th and 75th percentiles, respectively. The horizontal line represents the median, and bars, the range. There was a significant difference in the mean SNOT-22 scores between the time periods shown (p = 0.004, Kruskal-Wallis test). The bars and arrows depict significant differences between the time periods 1 to 3 months and 6 to 12 months, and between 1 to 3 months and 12 months and beyond (p < 0.05, post hoc Dunn test).
To define the morbidity specific to the endonasal approach, we evaluated the sinonasal complications in 109 patients clinically. The average duration of nasal crusting was 126 days (±87 days). The use of nasal septal nasal flap reconstruction did not affect the duration of nasal crusting compared with cases where these flaps were not used. Other sinonasal complications experienced by these patients included nasal synechiae (9%), alar sill burn (5%), maxillary nerve hypoesthesia (2%), palatal hypoesthesia (7%), incisor hypoesthesia (11%), serous otitis media (2%), taste disturbance (7%), and malodor (19%). Vidian nerve dysfunction and velopharyngeal incompetence were not observed in any patients.
DISCUSSION
Quality of Life: Definitions, Measures, and Instruments in Skull Base Surgery
Although QOL is an accepted concept in the setting of health care, it is not very well defined or measured frequently. There are several perspectives on the broad concept of the term “quality of life.” It encompasses a person's general feeling of well-being regarding various dimensions, also known as domains, of one's life conditions and includes a range of physical and psychological characteristics.11 Domains include development and activity, physical, emotional, social, and material well-being. In the setting of health care, the addition of pain and disease-specific dimensions constitute the multidimensional construct of QOL. The QOL in patients with cranial base tumors may be influenced by several factors, including the intrinsic nature of the disease and the modality of treatment and reconstruction methods, in one or more domains of QOL that can be assessed using the multidimensional construct.
Important aspects of assessment of QOL include a validated site-specific multidimensional instrument and accurate and appropriate administration of the instrument and longitudinal studies.11,12,13 A site-specific multidimensional instrument has significant advantages over some commonly used scales including the Glasgow Benefit Inventory, which is a general outcome measure, and the Karnofsky scale, which is an overall measure of patient level of activity and medical care needs and is not site-specific or multidimensional.14,15 Some common QOL instruments used for assessment of QOL outcomes following skull base surgery are shown in Table 1. A valid interpretation and application of QOL data require disease-specific instruments that assess morbidity associated with a particular diagnosis (e.g., anterior skull base tumors) or treatment (e.g., anterior craniofacial resection).16 The best instruments to measure QOL are (1) reliable, with reproducible and consistent results under constant conditions; (2) valid, thereby covering the full range of topics relevant to the condition and consistent with established measures; and (3) responsive, thereby sensitive in detecting change.13 The QOL instrument can be utilized to assess QOL on several levels by a combination of (1) an objective assessment of the domains of QOL; (2) subjective feeling of well-being, based on one's satisfaction with the domains of QOL; and (3) personal values and aspirations, based on the importance one places on a domain of QOL.12
Table 1.
Quality of Life Instruments Utilized in Skull Base Surgery Patients
| Quality of Life Instrument | Measure |
|---|---|
| Anterior skull base questionnaire9 | Multidimensional and site-specific |
| Karnofsky performance status scale14 | Assesses patient independence; not site-specific, not multidimensional |
| Short Form Health Survey Questionnaire30 | Multidimensional, not site-specific |
| Modified questionnaire from Woertgen22 | Not site-specific |
| Glasgow Benefit Inventory15 | Measures benefit obtained from a procedure; not site-specific, not multidimensional |
| Sickness Impact Profile31 | Sickness-related behavioral dysfunction; not site-specific, not multidimensional |
The administration of the QOL instrument by the patient is essential to obtain the most important perspective on the effects of treatment on QOL. Self-assessment has been shown to be more sensitive and reliable compared with clinician's assessment.11,17 Furthermore, there is often considerable discrepancy between patient and clinician. The assessment provided by partners and family members has also conflicted with patient assessments.17,18 Given that QOL is an individual phenomenon, an assessment over time should ideally be administered by the same patient. If intergroup and cross-sectional comparisons are performed, pretreatment assessment of QOL ensures that the study groups were comparable from the beginning.
The assessment of a patient's QOL can provide an estimate of the effect of the disease and of its treatment on the patient's normal life. An assessment over time may define the rate and proportion of patients who regain normal to near-normal function. This information is an important component in establishing pretreatment expectations. Furthermore, factors that minimize and promote early restoration of function can be identified and implemented. Understanding the effects of treatment and of different modalities of treatment on QOL may influence the decision to treat and determine the type of treatment based on the patient's current condition and future expectations. Specific impediments may be identified early during follow-up, and relevant interventions provided to high-risk patients.13,19
Skull Base Surgery and QOL
Several studies have examined the QOL outcomes following a wide range of surgical treatments for a variety of tumors at various locations in the cranial base.16,20,21,22,23,24,25,26,27,28 Accordingly, the QOL outcomes from these studies are variable, reflecting the heterogeneity of the pathologies, surgical treatments, study designs, and QOL instruments utilized during the assessments. Although these confounding variables make it difficult to identify specific areas where changes may be implemented, there is little doubt that there is a clear need for surgical approaches to the skull base that reduce morbidity and improve the QOL.
Current surgical approaches to the ventral skull base include anterior (transcranial, transfacial) and lateral (transcranial, infratemporal) approaches. Classically, an anterior craniofacial resection utilizes a transcranial subfrontal approach in combination with a transfacial approach (lateral rhinotomy, midfacial degloving, or transpalatal). In some cases, the morbidity caused by the tumor may preclude surgical treatment via an external approach due to approach-related morbidity. The advent of endoscopic techniques now allows a completely endoscopic endonasal craniofacial resection without the need for a craniotomy or facial incisions. This approach maintains the oncological principles of tumor removal along with preservation of function and cosmesis. Ideally, this would have a positive effect on QOL. However, site-specific QOL outcomes following the various surgical approaches for tumor treatment are only recently being defined.
Anterior Skull Base Tumors: Open and Combined Open and Endoscopic Approaches
There are few studies specifically addressing QOL in patients who have undergone anterior skull base surgery.16,22,28,29 Early studies of QOL in long-term survivors of anterior skull base tumors following craniofacial resection showed that up to 89% had some complaints, particularly regarding cosmesis, and 63% of patients were dissatisfied with their current conditions following surgery.29
Woertgen and colleagues assessed the QOL in 14 patients who underwent open and combined open and endoscopic surgical resections (frontal transdural resection, temporal/transfacial/orbital approach, frontal/transfacial/endonasal approach) and radiation therapy for anterior skull base malignancies.22 About 50% of their cohort reported a QOL score below 50, which translated to “considerable suffering” in their present situation, 45% could return to their careers, and several patients suffered from headache and hemiparesis. Not surprisingly, this was reflected in worse scores for job and health domains. Despite their suffering, the authors reported that all members of the study would again agree to surgery. This incongruence may suggest that a person's will to live may outweigh a painful existence. However, because reliability and responsiveness of this study were likely affected by small sample size, use of a generic instrument, and heterogeneity of skull base pathology and approaches, conclusions from this study are unsubstantiated.
Gil and associates used a validated site-specific multidimensional instrument to assess the postoperative QOL in 40 patients who underwent subcranial approach for resection of anterior skull base tumors.9,16 An improvement in the overall QOL score was seen 6 to 24 months after surgery compared with 3 to 6 months postoperatively. The worst impact on the patients' QOL was seen in the emotional state and financial status domains. Older age resulted in lower scores in physical function. Those with malignancies also reported statistically significant lower scores in performance, physical function, specific symptoms, and emotion, and those who underwent radiation had only significant decreases in specific symptoms and emotion domains. The best mean overall QOL score was 2.81 (score range 1.0 to 5.0) following the subcranial approach to anterior skull base tumors, and this was achieved at 6 to 24 months after surgery. A recent study examining QOL outcomes (anterior skull base questionnaire) in patients who underwent the classical subcranial approach alone and those who underwent subcranial and another approach (midfacial degloving, orbitozygomatic, transfacial, Le Fort I downfracture, or transorbital approach) for complex tumors showed no significant difference in the overall QOL scores. However, there was a significant difference in the disease-specific domain score between the two groups.28
Early data on sinonasal morbidity and QOL following the endonasal approach to the skull base suggest that there may be a greater disruption of normal sinonasal anatomy and function that may be higher compared with standard external approaches. However, this morbidity appears to be temporary. The QOL results are encouraging, showing that the overall QOL is very good and that this is achieved early in the postoperative period compared with external approaches. However, major limitations of this study are that the vast majority of patients underwent surgery for benign skull base lesions and included multiple endonasal skull base modules. Further studies examining the impact of site-, disease-, surgical module-, and reconstruction-specific parameters on the QOL of these patients are warranted.
Limitations of Present Studies and Future Directions
The inherent nature of diseases that involve the skull base and their treatments, along with socioeconomic differences and availability of emotional support, makes an assessment of QOL factors challenging. However, valid data may be obtained that can provide pertinent information regarding the best treatment modalities and surgical approaches that provide the optimum QOL in patients suffering from cranial base tumors. Future studies using validated disease and site-specific multidimensional QOL instruments are essential. With increased patient numbers, prospective study design, and pretreatment evaluation, longitudinal and multicenter studies would enable improved assessment of QOL. Valid QOL data may help to guide the selection of optimal therapy, type of surgical approach, and reconstruction method and to implement measures that improve perioperative care of the patient that enables prompt functional and emotional recovery.
CONCLUSION
Recent awareness of the impact of treatments on the QOL of patients with skull base tumors has led to the development of several surgical approaches that improve tumor extirpation while attempting to reduce morbidity associated with the procedure. An estimate of the QOL following various treatments would help determine its utility, although ultimately, the adoption of a particular form of treatment or reconstruction will depend on patient and physician preference. In some cases, this will involve a trade-off between QOL and the potential for cure. When cure rates are equivalent, QOL issues assume greater importance. More recent studies indicate that the overall QOL is good following surgery and early QOL results following endoscopic approaches to the skull base are promising. Further studies on the impact of reconstruction methods and approach-specific QOL outcomes are in progress.
REFERENCES
- Boyle J O, Shah K C, Shah J P. Craniofacial resection for malignant neoplasms of the skull base: an overview. J Surg Oncol. 1998;69:275–284. doi: 10.1002/(sici)1096-9098(199812)69:4<275::aid-jso13>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Raveh J, Turk J B, Lädrach K, et al. Extended anterior subcranial approach for skull base tumors: long-term results. J Neurosurg. 1995;82:1002–1010. doi: 10.3171/jns.1995.82.6.1002. [DOI] [PubMed] [Google Scholar]
- Terrell J E, Nanavati K A, Esclamado R M, Bishop J K, Bradford C R, Wolf G T. Head and neck cancer-specific quality of life: instrument validation. Arch Otolaryngol Head Neck Surg. 1997;123:1125–1132. doi: 10.1001/archotol.1997.01900100101014. [DOI] [PubMed] [Google Scholar]
- Weymuller E A, Yueh B, Deleyiannis F W, Kuntz A L, Alsarraf R, Coltrera M D. Quality of life in patients with head and neck cancer: lessons learned from 549 prospectively evaluated patients. Arch Otolaryngol Head Neck Surg. 2000;126:329–335. discussion 335–336. doi: 10.1001/archotol.126.3.329. [DOI] [PubMed] [Google Scholar]
- Weymuller E A, Jr, Yueh B, Deleyiannis F W, Kuntz A L, Alsarraf R, Coltrera M D. Quality of life in head and neck cancer. Laryngoscope. 2000;110(3 Pt 3):4–7. doi: 10.1097/00005537-200003002-00002. [DOI] [PubMed] [Google Scholar]
- Karnell L H, Funk G F, Hoffman H T. Assessing head and neck cancer patient outcome domains. Head Neck. 2000;22:6–11. doi: 10.1002/(sici)1097-0347(200001)22:1<6::aid-hed2>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Kalkanis S N, Quiñones-Hinojosa A, Buzney E, Ribaudo H J, Black P M. Quality of life following surgery for intracranial meningiomas at Brigham and Women's Hospital: a study of 164 patients using a modification of the functional assessment of cancer therapy-brain questionnaire. J Neurooncol. 2000;48:233–241. doi: 10.1023/a:1006476604338. [DOI] [PubMed] [Google Scholar]
- Hassan S J, Weymuller E A., Jr Assessment of quality of life in head and neck cancer patients. Head Neck. 1993;15:485–496. doi: 10.1002/hed.2880150603. [DOI] [PubMed] [Google Scholar]
- Gil Z, Abergel A, Spektor S, Shabtai E, Khafif A, Fliss D M. Development of a cancer-specific anterior skull base quality-of-life questionnaire. J Neurosurg. 2004;100:813–819. doi: 10.3171/jns.2004.100.5.0813. [DOI] [PubMed] [Google Scholar]
- Morley A D, Sharp H R. A review of sinonasal outcome scoring systems—which is best? Clin Otolaryngol. 2006;31:103–109. doi: 10.1111/j.1749-4486.2006.01155.x. [DOI] [PubMed] [Google Scholar]
- Morton R P, Izzard M E. Quality-of-life outcomes in head and neck cancer patients. World J Surg. 2003;27:884–889. doi: 10.1007/s00268-003-7117-2. [DOI] [PubMed] [Google Scholar]
- Felce D, Perry J. Quality of life: its definition and measurement. Res Dev Disabil. 1995;16:51–74. doi: 10.1016/0891-4222(94)00028-8. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick R, Fletcher A, Gore S, Jones D, Spiegelhalter D, Cox D. Quality of life measures in health care. I: Applications and issues in assessment. BMJ. 1992;305:1074–1077. doi: 10.1136/bmj.305.6861.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Laliberte L, Morris J N, Wiemann M. The Karnofsky Performance Status Scale. An examination of its reliability and validity in a research setting. Cancer. 1984;53:2002–2007. doi: 10.1002/1097-0142(19840501)53:9<2002::aid-cncr2820530933>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Robinson K, Gatehouse S, Browning G G. Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol. 1996;105:415–422. doi: 10.1177/000348949610500601. [DOI] [PubMed] [Google Scholar]
- Gil Z, Abergel A, Spektor S, et al. Quality of life following surgery for anterior skull base tumors. Arch Otolaryngol Head Neck Surg. 2003;129:1303–1309. doi: 10.1001/archotol.129.12.1303. [DOI] [PubMed] [Google Scholar]
- Gil Z, Abergel A, Spektor S, Khafif A, Fliss D M. Patient, caregiver, and surgeon perceptions of quality of life following anterior skull base surgery. Arch Otolaryngol Head Neck Surg. 2004;130:1276–1281. doi: 10.1001/archotol.130.11.1276. [DOI] [PubMed] [Google Scholar]
- Bjordal K, Freng A, Thorvik J, Kaasa S. Patient self-reported and clinician-rated quality of life in head and neck cancer patients: a cross-sectional study. Eur J Cancer B Oral Oncol. 1995;31B:235–241. doi: 10.1016/0964-1955(95)00010-f. [DOI] [PubMed] [Google Scholar]
- McLachlan S A, Allenby A, Matthews J, et al. Randomized trial of coordinated psychosocial interventions based on patient self-assessments versus standard care to improve the psychosocial functioning of patients with cancer. J Clin Oncol. 2001;19:4117–4125. doi: 10.1200/JCO.2001.19.21.4117. [DOI] [PubMed] [Google Scholar]
- Kwok H C, Morton R P, Chaplin J M, McIvor N P, Sillars H A. Quality of life after parotid and temporal bone surgery for cancer. Laryngoscope. 2002;112:820–833. doi: 10.1097/00005537-200205000-00010. [DOI] [PubMed] [Google Scholar]
- Kelleher M O, Fernandes M F, Sim D W, O'Sullivan M G. Health-related quality of life in patients with skull base tumours. Br J Neurosurg. 2002;16:16–20. doi: 10.1080/02688690120114183. [DOI] [PubMed] [Google Scholar]
- Woertgen C, Rothoerl R D, Hosemann W, Strutz J. Quality of life following surgery for malignancies of the anterior skull base. Skull Base. 2007;17:119–123. doi: 10.1055/s-2006-953513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samii A, Gerganov V, Herold C, Gharabaghi A, Hayashi N, Samii M. Surgical treatment of skull base chondrosarcomas. Neurosurg Rev. 2009;32:67–75. discussion 75. doi: 10.1007/s10143-008-0170-4. [DOI] [PubMed] [Google Scholar]
- Natarajan S K, Sekhar L N, Schessel D, Morita A. Petroclival meningiomas: multimodality treatment and outcomes at long-term follow-up. Neurosurgery. 2007;60:965–979. discussion 979–981. doi: 10.1227/01.NEU.0000255472.52882.D6. [DOI] [PubMed] [Google Scholar]
- Martinez-Devesa P, Barnes M L, Alcock C J, Kerr R S, Milford C A. Evaluation of quality of life and psychiatric morbidity in patients with malignant tumours of the skull base. J Laryngol Otol. 2006;120:1049–1054. doi: 10.1017/S0022215106002477. [DOI] [PubMed] [Google Scholar]
- Mueller D, Oro' J J. Prospective analysis of self-perceived quality of life before and after posterior fossa decompression in 112 patients with Chiari malformation with or without syringomyelia. Neurosurg Focus. 2005;18:ECP2. doi: 10.3171/foc.2005.18.2.11. [DOI] [PubMed] [Google Scholar]
- Baumann I, Polligkeit J, Blumenstock G, Mauz P S, Zalaman I M, Maassen M M. Quality of life after unilateral acoustic neuroma surgery via middle cranial fossa approach. Acta Otolaryngol. 2005;125:585–591. doi: 10.1080/00016480510026935. [DOI] [PubMed] [Google Scholar]
- Fliss D M, Abergel A, Cavel O, Margalit N, Gil Z. Combined subcranial approaches for excision of complex anterior skull base tumors. Arch Otolaryngol Head Neck Surg. 2007;133:888–896. doi: 10.1001/archotol.133.9.888. [DOI] [PubMed] [Google Scholar]
- Fukuda K, Saeki N, Mine S, et al. Evaluation of outcome and QOL in patients with craniofacial resection for malignant tumors involving the anterior skull base. Neurol Res. 2000;22:545–550. doi: 10.1080/01616412.2000.11740716. [DOI] [PubMed] [Google Scholar]
- Brazier J E, Harper R, Jones N M, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter W B, Bobbitt R A, Bergner M, Gilson B S. Validation of an interval scaling: the sickness impact profile. Health Serv Res. 1976;11:516–528. [PMC free article] [PubMed] [Google Scholar]